Summary
Extracranial vertebral artery aneurysm associated with neurofibromatosis (NF1) is very rare. The aneurysm was successfully treated by endovascular trapping of the aneurysm and proximal vertebral artery with coils.
Key words: neurofibromatosis, extracranial aneurysm, vertebral artery
Introduction
Most of the reported extracranial vertebral artery (VA) aneurysms are dissecting aneurysms related to trauma. Since craniocervical vascular lesions associated with NF1 are known to be related to stenosis or occlusion of cerebral arteries, an extracranial VA aneurysm associated with NF1 is very rare. We report the details of the endovascular treatment and review this aneurysm associated with NF1.
Case Presentation
Several months prior to this admission, a 67-year-old male had experienced persistent dizziness, which aggravated while turning the head to the right side. Various kinds of treatment failed to relief his symptom. Multiple fibromas and cafe au lait spots were found on his neck and trunk. Bruit was audible on the left supraclavicular region. No neurological deficits were found. Routine laboratory examinations were normal. Moyamoya disease was found on his son.
Radiological Findings
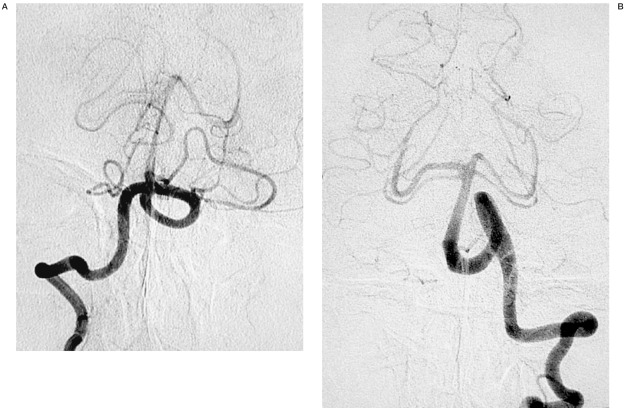
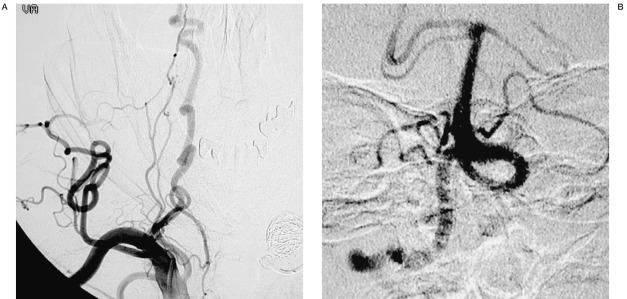
Left subclavian artery angiogram (figure 1A and 1B) revealed a broad based aneurysm of 20 mm x 20 mm without definite neck in the proximal portion of left VA (V1). Left intracranial VA (figure 2B) was elongated but there was neither stenosis nor occlusion. Right VA angiogram (figure 2A) also revealed elongation of intracranial VA. Left vertebral artery was found to be dominant. Left posterior communicating artery was of fetal type. A diagnosis of extracranial VA aneurysm associated with NF1 was made. We postulated that dizziness is secondary to vertebrobasillar artery insufficiency (VBI) due to the aneurysmal blood steal. We decided to treat the aneurysm by endovascular technique.
Figure 1.
A) Left subclavian angiogram and (B) three-dimensional (3D) angiogram, showing a large aneurysm without definite neck in the proximal portion of left vertebral artery.
Figure 2.
A) Right vertebral angiogram, showing severe elongation. B) Left vertebral angiogram, showing no stenosis or occlusion, but severe elongation. Left vertebral artery was found to be dominant.
Treatment
First an occlusion balloon catheter (5F. double lumen) was positioned at the left subclavian artery near the origin of left VA. Occlusion test of the left subclavian and left vertebral artery was performed. The patient tolerated the occlusion well and remained neurologically intact during 20 minutes of occlusion.
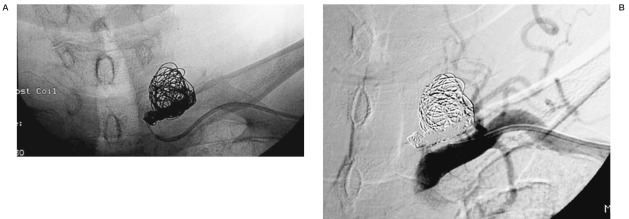
A microcatheter was introduced into the left VA aneurysm and coils (TRUFILL DCS) were deployed into the aneurysm. Following this, proximal part of left VA was also occluded with coils (GDC-US and Fibered GDC). Left subclavian artery angiogram (figure 3A and 3B) didn't demonstrate any anterograde flow into the VA or filling of the aneurysm. An angiogram of the contralateral VA (figure 4A) demonstrated adequate perfusion of the basilar artery and retrograde flow into the left vertebral artery without filling of the aneurysm(figure 4A). The postoperative course was uneventful. His dizziness improved and he was discharged one week later without any neurological deficit.
Figure 3.
A) X-ray film, showing coil occlusion of the aneurysm and left proximal vertebral artery. B) Left subclavian artery angiogram demonstrated no aneurysm and no left VA antegradely.
Figure 4.
A) Right subclavian artery angiogram, showing severe elongation of right vertebral artery cleary B) Right vertebral angiogram, showing adequate flow of the basilar artery, but no retrograde filling of the aneurysm.
Discussion
Neurofibromatosis (NF1) is an autosomal dominant inheritance disorder caused by abnormality of the genes of the 17th chromosome for a frequency of 1 per 3000 to 5000 persons 1,6,7. Most of vascular lesions with NF1 are stenosis and aneurysms of a renal artery or abdominal aorta, but craniocervical vascular lesions are uncommon. The involved craniocervical vessels usually present with stenosis and/or occlusion of intracranial major vessels. Aneurysms and arteriovenous malformations are rarely observed3,4,5,6,7.
A review of the literature revealed that only eight cases of extracranial VA aneurysm associated with NF1 were reported2-8. In previous cases, symptoms include nerve root signs, compression of the brachial nerve plexus, cervical pain, and cervical mass. One of the cases reported rupture of extracranial VA aneurysm developing into vertebral AVF later8. And there was another report of fatal intrathoracic hemorrhage following rupture of extracranial VA aneurysm6. In our case, his main symptom is dizziness. He had no risk factors such as hypertension or arterial sclerosis. We speculated that the mechanism of his dizziness could be due to inadequacy of the posterior circulation. The left VA was dominant and the aneurysm was also located in the left VA. Therefore, his dizziness may be related to steal phenomenon. This hypothesis also explains the aggravation of the dizziness while the patient turning his head to the right. It was similar to the mechanism of bow hunter,s stroke 9,10.Occlusion of left VA and aneurysm by endovascular technique, could result in increased vascular flow in the right VA, thus restoring blood flow of the posterior circulation which consequently will alleviate his symptom. The surgical treatment of an extracranial VA aneurysm with NF is indicated if radiculopathy or myelopathy is present. However, when an aneurysm is diagnosed by an angiography, even if patient is asymptomatic, treatment should be mandatory because risks of AVF formation, fatal hemorrhage, and embolic stroke are high3. Usually treatment modality is surgical trapping and removal of the aneurysm 3,6. In recent years endovascular treatment with detachable balloon was reported 2,6. In our case, endovascular trapping of the aneurysm and proximal VA with coils was performed. Endovascular treatment has advantage of being minimally invasive and of short operation duration, in particular, for ruptured aneurysms. If proximal occlusion of a parent artery alone is done, the aneurysm may not disappear and will be recanalized by blood flow from opposite VA and other collateral vessels. Endovascular trapping of aneurysm and proximal parent artery, is supposed to be a better treatment modality.
Conclusions
When VBI symptom develops with the NF1 patient, it should be taken into consideration about not only intracranial VA-BA lesions but also extracranial VA lesions. Endovascular coiling is feasible, which is a minimally invasive treatment modality for extracranial VA aneurysms.
References
- 1.Greene JF, Jr, Fitzwater JE, et al. Arterial lesion associated with neurofibromatosis. Am J Clin Pathol. 1974;62:481–487. doi: 10.1093/ajcp/62.4.481. [DOI] [PubMed] [Google Scholar]
- 2.Negoro M, Nakaya T, et al. Extracranial vertebral artery aneurysm with neurofibromatosis-Endovascular treatment by detachable balloon. Neuroradiology. 1990;31:533–536. doi: 10.1007/BF00340136. [DOI] [PubMed] [Google Scholar]
- 3.Ohkata N. A Case of Multiple Extracranial Vertebral artery Aneurysms Associated with Neurofibromatosis. No Shinkei Geka. 1994;22(7):637–641. [PubMed] [Google Scholar]
- 4.Ji-Zong Zhao, Xiao-Di Han. Cerebral aneurysm associated with von Reckling hauzen,s Neurofibromatosis: A case report. Surg Neurol. 1998;50:592–596. doi: 10.1016/s0090-3019(97)00376-5. [DOI] [PubMed] [Google Scholar]
- 5.Hoffmann KT, Hosten N, et al. Giant aneurysm of the vertebral artery in neurofibromatosis type 1: report of a case and review of the literature. Neuroradiology. 1998;40:245–248. doi: 10.1007/s002340050576. [DOI] [PubMed] [Google Scholar]
- 6.Miyazaki T, Ohta F, et al. Extracranial vertebral artery ruptured into the thoracic cavity with neurofibromatosis Type 1: Case report. Neurosurgey. 2004;54:1517–1521. doi: 10.1227/01.neu.0000125547.31328.69. [DOI] [PubMed] [Google Scholar]
- 7.Fujimoto M, Nakahara I, et al. Multiple Intracranial Aneurysms and Vascular Abnormalities Associated with Neurofibromatosis Type 1: Case Report. No Shinkei Geka. 2004;32(4):355–359. [PubMed] [Google Scholar]
- 8.Ushikoshi S, Goto K, et al. Vertebral arteriovenous fistula that developed in the same place as a previous ruptured aneurysm: A case report. Surg Neurol. 1999;51:168–173. doi: 10.1016/s0090-3019(98)00011-1. [DOI] [PubMed] [Google Scholar]
- 9.Sakai K, Tsutsui T, et al. Bow Hunter’s Stroke Associated with Atlantooccipital Assimilation-Case Report. Neurol Med Chir (Tokyo) 1999;39:696–700. doi: 10.2176/nmc.39.696. [DOI] [PubMed] [Google Scholar]
- 10.Yamane K, Shima T. Surgical Treatment of a Case with Bow Hunters Stroke caused by C2 Cervical Nerve Traction of the Vertebral Artery. Spinal Surgery. 2003;17(1):35–39. [Google Scholar]