Summary
Middle meningeal artery pseudo-aneurysms and arteriovenous fistulas are usually post-traumatic, although occasional iatrogenic cases have been reported. The treatment has been obliteration of the fistula by surgical or endovascular means. Spontaneous closure of fistula is uncommon. We report a case of non-traumatic middle meningeal arteriovenous fistula in a patient with alcoholism, which resolved spontaneously without treatment.
Key words: middle meningeal a-v fistula, spontaneous thrombosis, SAH, alcoholism, DSA
Introduction
Middle meningeal artery pseudoaneurysms and arteriovenous fistulas are usually posttraumatic or iatrogenic in origin1-4. They may exhibit multiple draining pathways and are treated either surgically or now, more often by endovascular means5,6. Spontaneous thrombosis is rare. We report a case of middle meningeal arteriovenous fistula in an alcoholic patient without history of trauma and its spontaneous thrombosis before endovascular treatment could be attempted.
Methods and Results
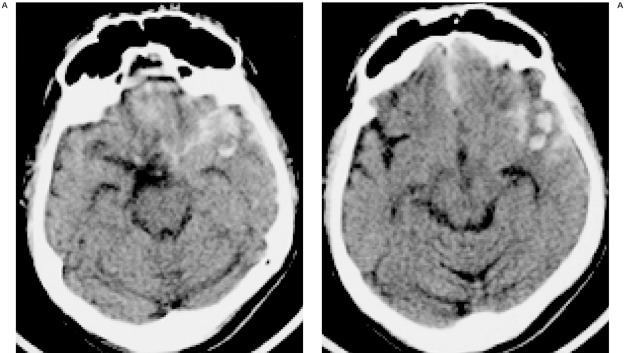
A 42-year-old man presented with one episode of loss of consciousness and generalized tonic-clonic seizures. No history of trauma was present. He was a chronic alcoholic and had been treated for alcohol withdrawal in the past. On examination, there were no focal neurological deficits. CT of the head showed anterior inter-hemispheric and right sylvian fissure subarachnoid hemorrhage with right frontotemporal parenchymal hematoma (figure 1). No skull fracture was seen. Aneurysmal SAH due to rupture of a right middle cerebral artery aneurysm was suspected and a Digital Subtraction Angiography (DSA) was performed.
Figure 1.
Plain CT shows fronto-temporal hematoma with subarachnoid hemorrhage (Patient's right side is on the left side of the image).
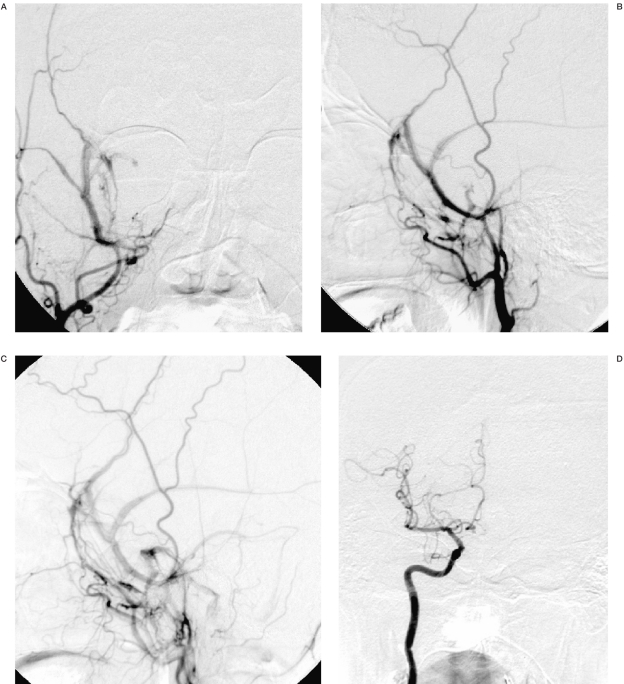
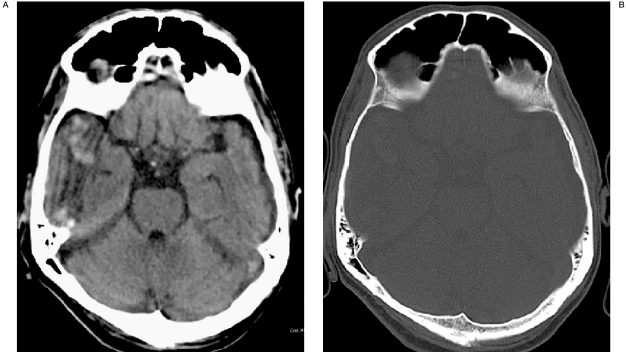
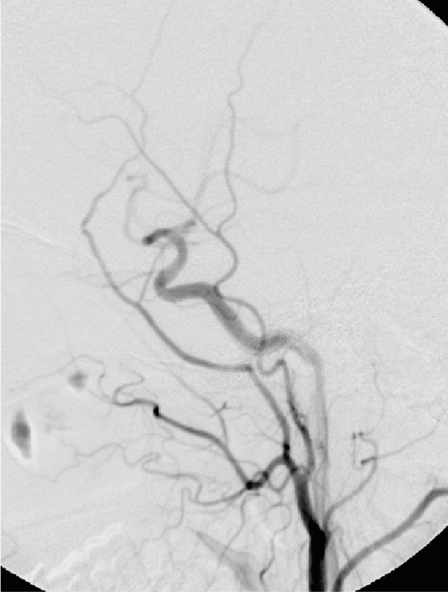
DSA revealed a high flow dural arteriovenous fistula of the right middle meningeal artery branches with drainage into the sphenoidal and parietal portions of the anterior branch of the middle meningeal veins, the posterior and petrosal branches of the middle meningeal veins and retrograde drainage into the cavernous plexus. The ipsilateral sinus of the lesser wing of sphenoid was opacified from the anterior branches of the meningeal veins and drained into the cavernous plexus (sinus). The pterygoid, inferior and superior petrosal sinuses were also visualised. The site of fistula was most likely at the foramen spinosum (figure 2). Bilateral internal carotid angiograms, vertebral angiograms and contralateral external carotid angiogram were normal. There was no arterial aneurysm. After four weeks of conservative management, a repeat CT showed resolution of hematoma (figure 3) and an angiogram was performed prior to endovascular treatment. Selective angiograms of the right external carotid and internal maxillary arteries (figure 4) and superselective angiogram of the right middle meningeal artery (figure 5) showed disappearance of the fistula, probably due to spontaneous thrombosis.
Figure 2.
Right external carotid artery angiogram AP (A), lateral (B) shows middle meningeal arteriovenous fistula with drainage towards sinus of lesser wing of sphenoid, cavernous plexus, pterygoid plexus and visualization of petrosal and meningeal veins in later phase (C). Right Internal Carotid angiogram (D) is normal.
Figure 3.
Repeat CT shows resolution of the hematoma. No fracture is seen.
Figure 4.
Follow-up right ECA angiogram (Lateral) after four weeks shows disappearance of the fistula.
Figure 5.
Superselective middle meningeal angiogram (lateral) also fails to show any fistula.
Discussion
The venous network paralleling the dural arteries of the cranial convexity virtually never develops arteriovenous fistulae (DAVFs), unless arterial disease or direct trauma of the adjacent middle meningeal artery causes arterial rupture into it 1. Middle meningeal AVFs are uncommon lesions, secondary to trauma, surgery or endovascular procedures2-4. The fistula can communicate with the accompanying middle meningeal vein, diploic vein, adjacent cavernous, sphenoparietal, greater petrosal dural venous sinuses, or into a cortical vein7-11.
Traumatic dural arteriovenous fistula of the middle meningeal vessels was first described by Fincher in 19517. In a review of angiograms in 446 patients with head trauma, Freckmann et Al 2 found an arteriovenous fistula of the middle meningeal artery in eight patients (1.8 %).
They classified the arteriovenous fistulae of the middle meningeal artery based on venous drainage in angiography into six types:
-
I.
Drainage via middle meningeal veins to pterygoid plexus, characterized by tramtack appearance of meningeal vessels.
-
II.
Drainage via sphenoparietal sinus or other meningeal veins into the superior sagittal sinus.
-
III.
Drainage via sphenoparietal sinus into cavernous sinus
-
IV.
Drainage via middle meningeal veins and superior petrosal sinus into cavernous sinus/basilar plexus
-
V.
Drainage via diploic veins
-
VI.
Drainage via bridging (cortical) vein into superior sagittal sinus.
The formation of fistula has been influenced by multiple factors - anatomically the artery runs along the outer surface of the dura accompanied by the paired veins and the dura is firmly adherent to the bone at the bottom of the vascular groove. A tear of the arterial wall by skull fracture or by separation of the dura mater and bone can cause a traumatic MMA fistula2,3. Histologically, medial defects in the meningeal arteries are observed at the points of branching as in other cerebral arteries. Hassler12 observed that while the elastic lamina and adventitia often showed increased thickness over the medial defect, the defects were also thin walled and separated from the subarachnoid space by a thin loose layer of connective tissue. Pathological processes such as atherosclerosis may also decrease the elasticity and predispose to fistula formation. Thus, the fistula is formed probably by the interaction of several influences including vascular injury, anatomical and pathological dispositions.
Intracranial hemorrhage is a specific complication of dural AVFs with retrograde leptomeningeal drainage towards cortical veins 1. In the present study, there was evidence of retrograde drainage into cavernous sinus from the meningeal arterial branches, antegrade opacification of the sinus of the lesser wing of sphenoid from the meningeal veins which further drained into the cavernous sinus and no reflux into cortical veins. Studies have assimilated the sinus of the lesser wing of sphenoid with the sphenoparietal sinus and demonstrated the termination of the superficial middle cerebral vein into the sinus 13,14, although this view is disputed by others15. We hypothesised that the high-flow fistula led to venous hypertension in the superficial middle cerebral vein with resulting cisternal and anterior temporal hemorrhage.
Only few cases of dural AVFs with spontaneous closure have been reported 16,17. Luciani et Al distinguished two types of spontaneously regressing dural AVFs: post-traumatic and spontaneous. According to them, post traumatic fistulae can be distinguished by the following angiographic characteristics: small, involve one or few arteries and drain into atypical veins and sinuses. They hypothesized that the lack of multiple and disseminated feeders which characterize non-traumatic dural fistulae, along with the tendency for scar development in the healing process contribute to spontaneous closure of post-traumatic fistulae16. Satoh et Al18 observed irregularity of the arterial wall on follow-up angiogram and proposed thrombosis of the fistulous site as the likely mechanism of spontaneous closure.
The spontaneous closure of MMA fistula has been observed in elderly patients, who have suffered minor head injury, with a small hematoma or minor symptoms and a good clinical course 18-21 and historical or objective evidence of cranial trauma 16.
Moriya et Al17 reported a spontaneous closure of a non-traumatic dural AVF seven days following a diagnostic angiographic examination, proposing sinus thrombosis secondary to sinus stenosis as the probable etiology for the closure of the fistula. Absence of cortical venous reflex and severe symptoms have been associated with spontaneous closure of the non-traumatic dural fistulae.
The topographic and angioarchitectural characteristics of the present study may suggest a post-traumatic etiology for the fistula. However, in the absence of skull fracture on CT and a negative history for head injury, to assume a traumatic event for separation of dura, arterial injury and a high-flow fistula seems unlikely.
The mechanism for spontaneous closure of this high-flow fistula in our patient is presum-ably secondary to thrombosis at the site of the fistula. Luciani et Al16 proposed an intrinsic compression of the fistula within dural sinuses as a probable mechanism favouring closure. The anatomical disposition of the middle meningeal fistula within the bony grooves on the cranial convexity may support such a closure mechanism. The role of scar tissue is undermined by the indeterminate or non-existent role of trauma in the pathophysiology of the fistula.
References
- 1.Berenstein A, Lasjaunias P, Ter Brugge KG. Surgical Neuroangiography. Clinical and endovascular treatment aspects in adults. 2nd edition. Vol. 2. Berlin Heidelberg: Springer-Verlag; 2002. [Google Scholar]
- 2.Freckmann N, Sartor K, Herrmann HD. Traumatic arteriovenous fistulae of the middle meningeal artery and neighbouring veins or dural sinuses. Acta Neurochir (Wien) 1981;55(3-4):273–281. doi: 10.1007/BF01808443. [DOI] [PubMed] [Google Scholar]
- 3.Terada T, Nakai E, et al. Iatrogenic arteriovenous fistula of the middle meningeal artery caused during embolization for meningioma - case report. Neurol Med Chir (Tokyo) 1997;37(9):677–680. doi: 10.2176/nmc.37.677. [DOI] [PubMed] [Google Scholar]
- 4.Tsutsumi K, Shiokawa Y, et al. Postoperative arteriovenous fistula between the middle meningeal artery and the sphenoparietal sinus. Neurosurgery. 1990;26(5):869–871. doi: 10.1097/00006123-199005000-00023. [DOI] [PubMed] [Google Scholar]
- 5.Tsumoto T, Nakakita K, et al. Bone defect associated with middle meningeal arteriovenous fistula treated by embolization - case report. Neurol Med Chir (Tokyo) 2001;41(1):42–47. doi: 10.2176/nmc.41.42. [DOI] [PubMed] [Google Scholar]
- 6.Komiyama M, Yasui T, et al. Chronic subdural hematoma associated with middle meningeal arteriovenous fistula treated by a combination of embolization and burr hole drainage. Surg Neurol. 1994;42(4):316–319. doi: 10.1016/0090-3019(94)90400-6. [DOI] [PubMed] [Google Scholar]
- 7.Fincher EF. Arteriovenous fistula between the middle meningeal artery and the greater petrosal sinus; case report. Ann Surg. 1951;133(6):886–888. doi: 10.1097/00000658-195106000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Castaigne P, Bories J, et al. Meningeal arterio-venous fistulas with cortical venous drainage. Rev Neurol (Paris) 1976;132(3):169–181. [PubMed] [Google Scholar]
- 9.Smith JE, Epps J, et al. Traumatic arteriovenous fistula between the middle meningeal artery and the sphenoparietal sinus: a case report and review of the world literature. J Natl Med Assoc. 1981;73(3):274–178. [PMC free article] [PubMed] [Google Scholar]
- 10.Betz H. Traumatic arteriovenous fistula between the middle meningeal artery and vein. Spontaneous regression trend during angiographic controls. Radiologe. 1974;14(12):528–531. [PubMed] [Google Scholar]
- 11.Ishii R, Ueki K, Ito J. Traumatic fistula between a lacerated middle meningeal artery and a diploic vein; case report. J Neurosurg. 1976;44(2):241–244. doi: 10.3171/jns.1976.44.2.0241. [DOI] [PubMed] [Google Scholar]
- 12.Hassler O. Medial defects in meningeal arteries. J. Neurosurg. 1962;19:337–340. doi: 10.3171/jns.1962.19.4.0337. [DOI] [PubMed] [Google Scholar]
- 13.Tubbs RS, Salter EG, et al. The sphenoparietal sinus. Neurosurgery. 2007;60(2 Suppl 1):9–12. doi: 10.1227/01.NEU.0000249241.35731.C6. [DOI] [PubMed] [Google Scholar]
- 14.Tanoue S, Kiyosue H, et al. Para-cavernous sinus venous structures: anatomic variations and pathologic conditions evaluated on fat-suppressed 3D fast gradient-echo MR images. Am J Neuroradiol. 2006;27(5):1083–1089. [PMC free article] [PubMed] [Google Scholar]
- 15.San Millan Ruiz D, Fasel JH, et al. The sphenoparietal sinus of Breschet: does it exist? An anatomic study. Am J Neuroradiol. 2004;25(1):112–120. [PMC free article] [PubMed] [Google Scholar]
- 16.Luciani A, Houdart E, et al. Spontaneous Closure of Dural Arteriovenous Fistulas: Report of Three Cases and Review of the Literature. Am J Neuroradiol. 2001;22:992–996. [PMC free article] [PubMed] [Google Scholar]
- 17.Moriya M, Itokawa H, et al. Spontaneous closure of dural arteriovenous fistula after performing diagnostic angiography. No Shinkei Geka. 2007;35(1):65–70. [PubMed] [Google Scholar]
- 18.Satoh T, Sakurai M, et al. Spontaneous closure of a traumatic middle meningeal arterio-venous fistula. Neuroradiology. 1983;25(2):105–109. doi: 10.1007/BF00333301. [DOI] [PubMed] [Google Scholar]
- 19.Golabek R, Szwed M, et al. Traumatic arteriovenous fistula of the middle meningeal artery closed spontaneously. Neurol Neurochir Pol. 1976;10(5):663–665. [PubMed] [Google Scholar]
- 20.Kitahara T, Shirai S, et al. Traumatic middle meningeal arteriovenous fistula. Report of 3 cases and analysis of 32 cases. Eur Neurol. 1977;16(1-6):136–143. doi: 10.1159/000114891. [DOI] [PubMed] [Google Scholar]
- 21.Odake G. Spontaneous closure of a traumatic middle meningeal arterio-venous fistula accompanied by a sagittal epidural hematoma. Neurol Med Chir (Tokyo) 1981;21(12):1267–1273. doi: 10.2176/nmc.21.1267. [DOI] [PubMed] [Google Scholar]