Abstract
'if a man will begin with certainties, he shall end in doubts;
'but if he will be content to begin with doubts he shall end in certainties'.
Sir Francis Bacon, The Advancement of Learning
Summary
In the absence of level one evidence, the treatment of unruptured intracranial aneurysms is grounded on opinions. Results of the largest registry available, ISUIA (the International Study on Unruptured Intraacranial Aneurysms) suggest that surgical or endovascular treatments are rarely justified. Yet the unruptured aneurysm is the most frequent indication for treatment in many endovascular centres. In preparation for the initiation of a randomized trial, we aimed at a better knowledge of endovascular expert opinions on unruptured aneurysms.
We administered a standard questionnaire to 175 endovascular experts gathered at the WFITN meeting in Val d'lsère in 2007. Four paradigm unruptured aneurysms were used to poll opinions on risks of treatment or observation, as well as on their willingness to treat, observe or propose to the patient participation in a randomized trial, using six questions for each aneurysm.
Opinions varied widely among lesions and among participants. Most participants (92.5%) were consistent, as they would offer treatment only if their estimate of the ten-year risk of spontaneous hemorrhage would exceed risks of treatment. Estimates of the natural history were consistently higher than that reported by ISUIA.
Conversely, treatment risks were underestimated compared to those reported in ISUIA, but within the range reported in a recent French registry (ATENA). Participants were more confident in their evaluation of treatment risks and in their skills at treating aneurysms than in their estimates of risks of rupture entailed by the presence of the lesion, the latter being anchored at or close to 1% /year.
The gulf between expert opinions, clinical practices and available data from registries persist. Expert opinions are compatible with the primary hypothesis of a recently initiated randomized trial on unruptured aneurysms (TEAM), which is a benefit of endovascular treatment of 4% compared to observation over ten years. Only data from a randomized trial could provide convincing objective evidence in favour or against preventive treatment of unruptured in- tracranial aneurysms.
Key words: aneurysm, endovascular treatment, randomized studies
Introduction
Since most individuals with unruptured aneurysms (UAs) are asymptomatic and healthy, the question arises: what are we treating exactly, when we treat such a patient? This trivial question becomes troubling when one realizes that no one has ever proven that preventive treatment of UAs is beneficial.
Several answers come to mind, and some appear unsatisfactory. The notion that we could use an invasive and risky procedure to treat what could be considered an irrational fear of the disease, according to the infinitesimal risk reported by some observational studies, is dis- turbing2. Explanations, reassurance, psychotherapy or even anxiolytic pharmacotherapy, would appear more appropriate if this were the case.
However, most physicians who treat UAs prefer to think that UA can rupture, that the outcome following SAH is too often devastating, that the risk is tangible, and this is what they are trying to prevent. On the other hand, treatment also carries risks. Thus most would admit that these factual boundaries, the risks of the disease and the efficacy and risks of treatment, must be confronted and balanced to justify our collective clinical behaviour: we do treat UAs, at least in certain instances. The question is: on what basis are we making this decision?
Many clinicians come up with recommendations based on an individualized calculation tailored to the patient/aneurysm characteristics. The calculus is an approximation: if
[Estimated yearly risks of rupture] × [life expectancy] - [risks of treatment] > 0
then treatment is indicated. If the result of the calculation is < 0, observation is more prudent. The uncertainty is rare by definition, and corresponds to exactly = 0, an intuitively unhappy consequence of the calculus which is hardly compatible with an honest evaluation of current knowledge, or ignorance, regarding the treatment of unruptured aneurysms.
This type of calculus requires accurate numbers otherwise error will be multiplied beyond control. Where would these estimates come from? How do experts assess the likelihood of an uncertain event?
Beliefs and opinions have a strong influence on actions, especially in the absence of reliable knowledge. Psychological studies have shown that people rely on a limited number of heuristic principles which reduces complex tasks to simpler judgmental operations that are subject to error and bias3. These judgements are based on data of limited validity, as in the case with unruptured aneurysms. In fact, the 'natural history' of the disease is controversial, with only registries being available, and these seem to propose that treatment is rarely if ever indicated2,4-5.
Our first goal was to collect information on expert opinions in endovascular treatment of aneurysms: their beliefs on the natural history of the disease, the risks of treatment, and the action they would propose in a few prototypical cases. Other goals were to assess the coherence and uniformity of their opinions as well as compatibility with the most frequently cited reference, the ISUIA registry2.
However this above a priori calculation of risks versus benefits does not suffice to provide a rational and prudent basis for treatment. The history of medicine is replete with examples of allegedly sound treatments, considered 'standard' or beneficial on account of such a priori presumptions, but eventually proven to cause more harm than good. A more rigorous methodology is required to justify the preventive treatment of unruptured aneurysms: a randomized trial6.
At the time of this inquiry we were initiating the TEAM study, a clinical trial on endovascular management of unruptured aneurysms6-8. Opinions shared by a community of experts are pertinent to at least one interpretation of the concept of 'community equipoise' that is central to the ethical requirements of randomiza- tion7,9-10. Polled knowledge of expert opinions could help to define the types of patients in whom uncertainty dominates, in the mind of clinicians, and for whom the research question regarding the benefits of endovascular prevention would be most pertinent. This data could help anticipate patterns of recruitment and physician resistances that could be encountered during implementation of the trial, and impact on the generalizability of results at the end of the trial11-13.
Methods
Thirty-three theoretical and practical questions were presented to an audience of en- dovascular experts at the World Federation of Interventional Neuroradiology meeting in Val d'lsère in January 2007. Responses were given on an anonymous paper report form; there were 175 forms, and 161 were complete.
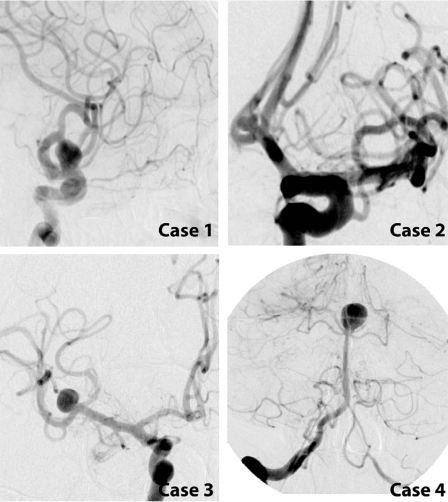
The questionnaire addressed theoretical questions, mixed with a set of six questions for four prototype aneurysm cases (24 questions). The questions were presented randomly to prevent the responders from recalling their previous answers on the same case. The four cases are illustrated in figure 1. These aneurysms were selected to represent a spectrum, with one type that would typically (but questionably), according to available observational studies, call for observation (case 2), one at high risk of rupture (case 4), and two within a presumed grey zones sensitive to diverging opinions (cases 1 and 3).
Figure 1.
Prototype cases. Case 1: 66-year-old female, 10 mm left ophthalmic aneurysm; Case 2: 34-year-old male, 5 mm Acom aneurysm; Case 3:49-year-old male, 8 mm right MCA aneurysm; Case 4: 51-year-old female, 12 mm basilar bifurcation aneurysm.
In designing the questionnaire, we assumed that physicians were rational, used case by case analogical reasoning, but were not impervious to statistical information. Our hypotheses were inspired by Tversky and Kahneman's work on judgment under uncertainty3. We expected physicians to be poorly calibrated, overconfident in their skills, overoptimistic regarding their treatment, and possibly biased in their assessment of risks of the disease, with overweighting of small probabilities6. The questions can be found in the Annex.
Statistics
The proportions are reported with 95% confidence intervals. The difference between groups was analyzed by Mann-Whitney tests. The association between some questions was measured with Spearman's rank correlation coefficients or with the Pearson's chi-square tests. The agreement was studied with Kappa statistics. All analysis was carried out with SPSS version 15.
Results
Demographics
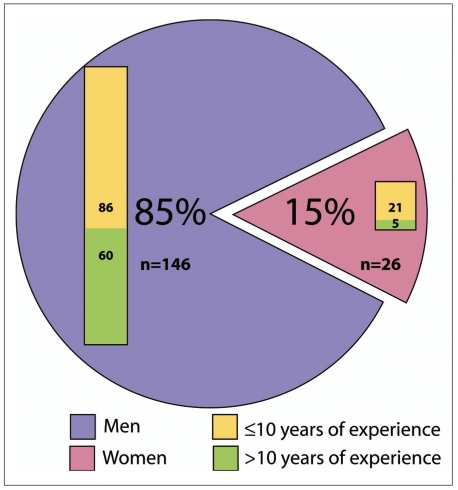
The experience of respondents in years of practice is illustrated in figure 2. Only 15% were women, with 19% of women having more than ten years of experience as compared to 41% of men (P=.001; Mann-Whitney).
Figure 2.
Demographics.
Rationale for treatment decisions
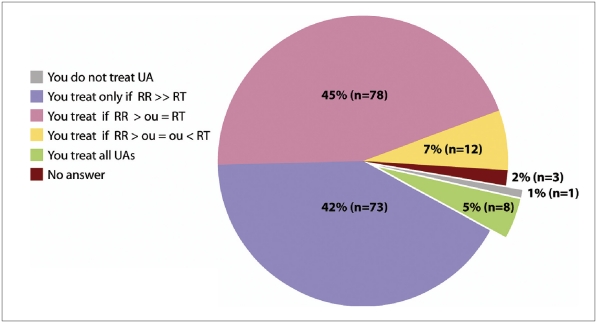
When participants were placed in a context where risks of treatment and risks of rupture for ten years are known for a single patient, most would consider treatment when the ten- year risks of rupture are > (41.7% IC95% [34.4%; 49.4%]) or > or = (44.6% IC95% [37.1%; 52.3%]) to the risks of treatment. Few participants would treat all (5%) or no (1%) patient with unruptured aneurysms, as a rule (figure 3).
Figure 3.
Consideration of treatment when ten-year risks are known.
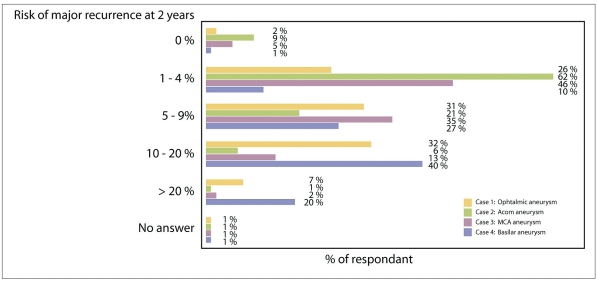
The use of statistical data
If hypothetical knowledge of a single patient is replaced by statistical results on the ten-year outcome of 1000 patients observed versus 1000 patients treated, 12.0% (IC95% [7.8%; 18.0%]) of participants answered that statistics were irrelevant. When other answers form the same participants were examined, all (n=21) would treat, but not observe, all four prototype aneurysms.
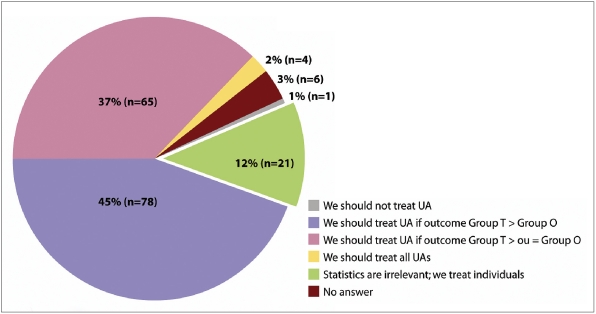
For the other 88% who agreed to base their decision on statistical findings, agreement with the previous question regarding 'knowledge of a single case' was mediocre (n=144; kappa: .43), with some participants opting for a more conservative attitude (they would consider treatment only if the outcome of the treated group was strictly better (44.6% IC95% [37.1%, 52.3%]) or better/equal to observed patients (37.1% (IC95%[30.1%, 44.8%]).
In other words, many participants were more conservative when informed of the statistical results on a population than when placed in an imaginary context of knowing the probabilities for a single patient (figure 4).
Figure 4.
Consideration of treatment and statistics about groups.
Confidence and experience
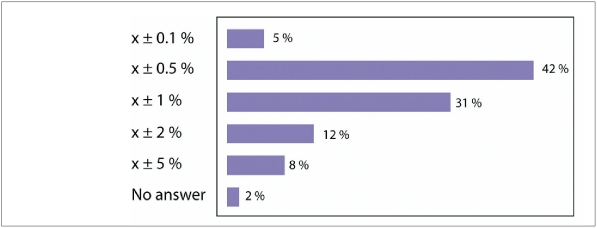
The confidence intervals in estimating rupture risks (rs = -0.157, P<.040) and treatment risks (rs = -0.168, P<.028) were correlated with experience and tended to be narrower for experienced compared to less experienced participants.
There was a significant correlation between experience and auto-evaluation of skills at estimating rupture risks (rs = 0.298, P<.001), as well as between experience and perceived skills at treating aneurysms (rs = 0.435, P<.001).
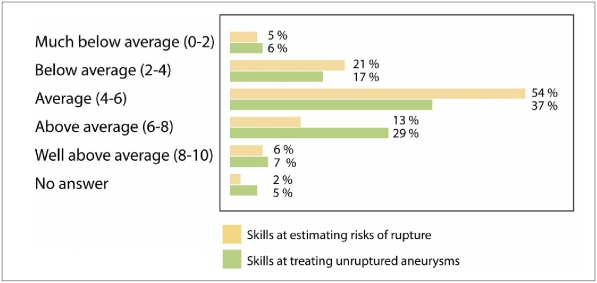
There was a close correlation of auto-evaluations of skills at estimating rupture risks and treatment skills (rs = 0.513, P<.001). However, participants (even experienced participants) were less confident in their skills in estimating rupture risks compared to their estimates of treatment skills (figure 5).
Figure 5.
Skills at estimating risks.
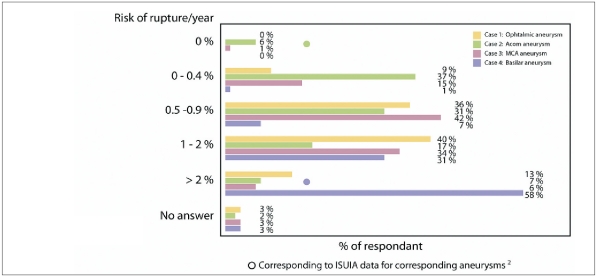
The 'natural history' of unruptured aneurysms
The evaluation of the risks of rupture for the four prototype cases is summarized in figure 6. For three quarters (all but case 4), rupture risks were at least twice those of the corresponding subgroups published in 1. Individual confidence intervals were narrow considering the wide variety of answers (figure 6B).Auto-evaluation of skill at estimating risks is illustrated in figure 5.
Figure 6A.
Risks of rupture of prototype cases.
Figure 6B.
Confidence intervals in estimation of rupture risks.
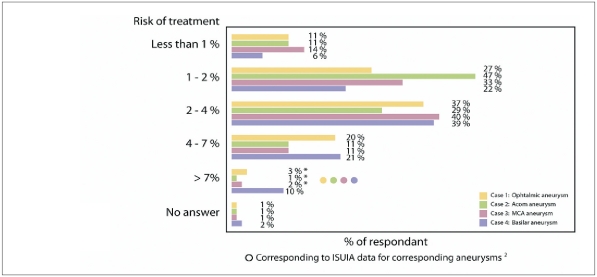
The risks of treatment
The estimates of the risks of treatment for the four prototype aneurysms are summarized in figure 7. For most lesions, risks were less than half those reported in2. Again individuals had narrow confidence intervals, considering the wide variety of answers (figure 7B). Skills at treating aneurysms are illustrated in figure 5.
Figure 7A.
Risks of treatment of prototype cases.
Figure 7B.
Confidence intervals in estimation of treatment risks.
Decisions about prototype cases
Decisions about individual cases are summarized in table 1. There was an association between experience and the will to treat the Acom aneurysm (□2 (3) = 12.114, p = .007).
Table 1.
Therapeutic choices.
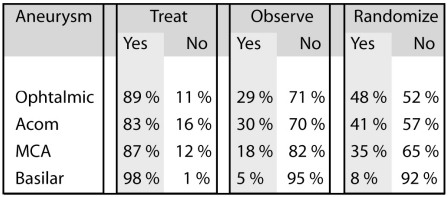 |
Participants' estimates of their skills at treating aneurysms and decision to treat the Acom aneurysm also correlated (P = .013)
There were no such correlation for the other three aneurysms. There was an association between the therapeutic attitude of participants and the willingness to treat the ophthalmic aneurysm (P = .009 and .000). In other words, as a paradigm aneurysm, the 10 mm ophthalmic aneurysm seems to be the best discriminant of the participants' attitude regarding un- ruptured aneurysms.
Consistency
There were strong associations between the estimates of the rupture risks and decision to treat or observe aneurysms for most aneurysms except for the basilar aneurysm, in which the decision was unanimous and thus no association could be studied. The risk of treatment was also correlated but to a lesser degree (see Table 2).
Table 2.
Association between risk estimates and treatment decisions.
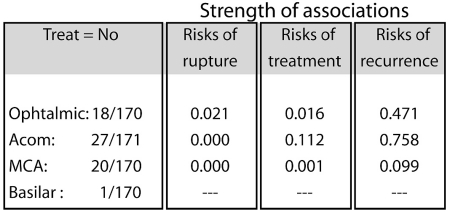 |
If consistency or coherence is judged according to the individual calculus: Consistent answer: Willing to treat if [10 x risks of hemorrhage/year] - [Treatment risks] > or = 0.592 (92.5%) answers were coherent, while 38 (6%) were more conservative and ten (1.5%) could be considered aggressive as compared to the calculus.
Individual equipoise
If the 'equipoise notion' is restricted to cases in whom participants are willing to both treat and observe the aneurysm (when asked on two different occasions), participants considered that they would treat and observe 28/174 for Acom, 7/174 basi- lar bifurcation, 18/174 MCA and ophthalmic 33/174. Yet systematically many more participants were willing to randomize these patients (Acom: 71/171; basilar: 13/174; MCA 60/174; ophthalmic 84/174) (see also table 1). Rather than interpreting these data as a proof of inconsistency, we believe this shows that the uncertainty becomes more 'available' once participants consider changing context from the usual clinical situation where they have to come up with a decision and the context of a trial where they can allow an expression of uncertainty.
Variability in opinions
Diversity and divergence in opinions within the community of experts may be interpreted as an indication of uncertainty in knowledge regarding unruptured aneurysms. Only the 12 mm basilar bifurcation aneurysm evoked constant responses and treatment decisions, while uncertainty was maximal for the 10mm carotid ophthalmic aneurysm.
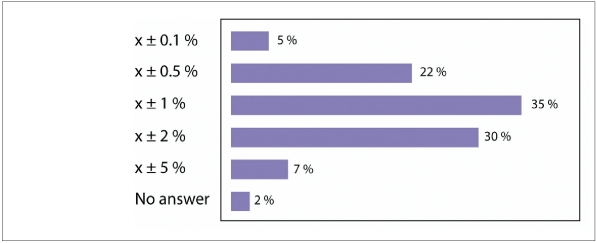
Risks of recurrence
The estimates of the risks of recurrence are illustrated in figure 8. Most answers were optimistic as compared to published reports on the subject14. There was no significant impact of risk of recurrence on decision to treat or observe (Table 2).
Figure 8.
Risk of major recurrences at two years.
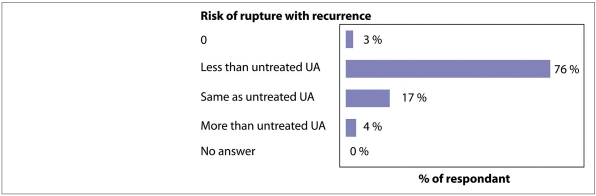
The estimated risk of rupture of a recurring aneurysm according to participants is illustrated in figure 9.
Figure 9.
Risk of rupture with recurrences.
Experience and participation in RCT
Sixty-seven percent of respondents were willing to participate in a randomized trial. No association was found between experience and willingness to participate in RCT [□2 (3) = 1.246, p=.742].
Discussion
This survey shows that endovascular experts are confident in their skills at treating unrup- tured aneurysms, and in estimating treatment risks. They are less confident in their estimates of the risks of rupture entailed by the presence of an unruptured aneurysm. Compared with observational studies, they tend to over-rate rupture risks, but under-rate treatment risks and the frequency of recurrences, resulting in decisions in favour of treatment in more than 80% of instances. They are in general overconfident in all their estimates, since the thousand- patient studies that would be necessary to provide the narrow confidence intervals they claim to possess do not exist and such intervals are way beyond the scope of any individual personal experience. However their individual decisions to treat or observe are frequently consistent with their beliefs on risk of treatment compared to natural history. There is a wide array of opinions among individuals.
a) What are the foundations of expert opinions on the natural history of aneurysms?
Given the scarcity of events that can occur either with or without treatment, it is unbelievable that opinions of experts could be founded on direct personal observations. Confidence intervals can be computed using conventional rules of statistical sciences, using the boundaries given by 95% of values distributed in a normal fashion; for subjects claiming a 0.5% or 1% confidence interval, the number of observations that would warrant such confidence is in the range of multiple thousands of patients, clearly outside the possibility of their experience 15.
Thus it is probable that most rely on publications and conferences at professional meetings. The most widely referred experience is the ISUIA (the meta-analysis by Wermer16 was not available at the time), but participants do not rely on subgroup statistics reported by ISUIA. Ignorance of ISUIA data is unlikely to be an appropriate explanation: it is amongst the most frequently publicized and discussed study within the field, and numerous editorials followed publication of the results. Hence ISUIA subgroup statistics are apparently not accepted as evidence within the field, a happy finding given that these statistics do not pass muster standards of scientific practice 17.
The set up necessary to follow and record so infrequent an event as ruptures has yet to be organized in a non biased context. In the interim, clinicians are repeatedly exposed to sick patients with ruptured aneurysms that are of the same characteristics as those that are not supposed to rupture, an experience that may impact on their beliefs. The nature of 'medical knowledge' and rational justification for action now become a mystery. How can such opinions latch on reality?
A heuristic method commonly used when confronted with uncertain knowledge is anchoring on some reference value and adjustment according to the particular circumstances at hand 3.
Perhaps the opinions of participants are compatible with a process that would use 'anchoring' on an overall mean estimate for all patients, near 1%/year (± 1%), compatible with most series and meta-analyses including ISUIA2,16,18,19, with adjustment of this value in one or the other direction, according to size or location.
b) Competence and confidence
There is abundant evidence that people are generally overconfident in their assignments of probability to their beliefs. Subjects state overly narrow confidence intervals which reflect more certainty than is justified by their knowledge about the assessed quantities 3.
Unrealistic optimism has deep motivational roots 20. For almost every positive trait the majority of individuals believe themselves to be above the median.This was clearly shown when we asked participants to rate their skills at treating aneurysms, or their confidence interval at evaluating treatment risks, as compared to the average interventionist present in the room. Taylor and Brown reached the disturbing conclusion that optimistic self-delusion is both a marker of mental health and well-being, and a factor that contributes to successful coping with the challenges of life 20. The observation that realism may be pathological raises troubling questions for the management of risks. Facing the facts can be disturbing, but given the high cost of mistakes, it might appear judicious that a rational expert should want to base his/her decision on unbiased odds rather than on predictions painted in rosy hues. Conversely, their estimates of their skills in predicting risks of rupture resulted in a 'depressed' curve by comparison to their interventional skills (figure 5), with fewer participants judging themselves 'above average'.
c) The role of statistical data
One crucial premise of this study is that decisions regarding unruptured aneurysms must be rational, otherwise the questionnaire would not make sense.
The first questions of the survey concerned the role of rationality and the use of statistics in decision-making. The majority of participants did commit to the significance of statistics, although they were more conservative when they had to rely on statistics for groups of patients than when they were asked to imagine they knew the exact risks involved in treating or observing a single individual (compare figures 3 and 4). Physicians who claimed that 'statistics were irrelevant' seemed to rely on a strong a priori prejudice in favour of treatment, since they unanimously chose to treat all lesions submitted to their judgement.
Desire is an important actor in decision- making. However, one of the hallmarks of modern medicine is not to confuse desire with reality. We desire to get rid of the problem, but good intentions do not suffice; we may not be willing to pay just any price to eliminate indeterminate risks entailed by the presence of an unruptured aneurysm. One reassuring finding was that most participants subjected their decision to some balance between risks of the disease, efficacy and risks of treatment in order to come up with a rational decision.
During the discussion that followed the disclosure of the results, many participants avowed they had felt a strong irritation upon answering the questions. Many were uncomfortable and would have preferred to be given detailed medical histories, to know more about each individual; some would have tested the patients for asymptomatic conditions, such as silent coronary disease or an occult colon carcinoma. This could be interpreted as an attempt to evade the dilemma by searching for local extraneous factors that could help with decision- making.
d) Between casuistry and statistics
Case by case reasoning (or casuistry) is as old as ancient medicine. Casuistry is deeply entrenched and more intuitive than statistics that have by comparison appeared only recently in medical history. Its emphasis on the individual history and the particular circumstances of the case at hand corresponds more closely to many human values and to personalized care. However medical knowledge in this context faces many difficulties. If it is true that no two patients are alike, how can we learn from the previous individual to the next one? And tragically, if two patients are always irreducibly different, how can we evaluate the outcome of medical actions? Casuistry was the predominant form of moral reasoning in medieval Europe, and its abuses were denounced by Pascal in the Lettres Provinciales21. It has since fallen into disrepute.
The casuist must classify cases into reference classes typified by prototype cases. Typical and unusual circumstances are then defined to determine exceptions and attenuating factors. Ambiguities and conflicts between paradigm cases abound, and the particular details of the individual stories serve to sort out and match current difficulties with recognized presumptions of the reference classes. Once confronted with an individual, the casuist must decide which paradigmatic cases are directly relevant to the case at hand. The cognitive categories that casuists must share in order to be able to group cases, derive maxims and find analogies are 'thickets of bias that can skew decisions' 22. This bias causes us to hold unwarranted and untested beliefs, but since they are 'so deeply rooted in our culture, we do not see them as needing to be tested, or we may not even recognize that we are making assumptions' 22. These implicit beliefs can affect each step of the above mentioned process for coming to resolution of cases. 'Since there are no universals in casuistry against which we can measure either our outcome or the process by which we came to the result, there is little protection against minor, or worse, snowballing effects of bias that lay hidden in the shared understandings of the community of casuists who make important decisions'22.
This is where the science of clinical trials finds its crucial role. But resorting to the machinery of the clinical trial to collect reliable knowledge from multiple institutions, and to analyze results in such a fashion as to minimize bias and error, does not mean that clinicians must abandon their clinical judgement, which will remain essential at both ends of the clinical trial process. First the decision to propose participation in a trial remains their prerogative, and patients, society as well as trial investigators trust the clinical judgement of clinicians that the inclusion of the particular patient is appropriate and in his/her interest. Finally, at the end of the trial, once analysis provides a general answer to the clinical dilemma, it will be up to the clinicians to decide, using their judgemental expertise, to whom the answer applies and what particular circumstances and features of the case should be taken into account to tailor the new medical knowledge to the individual so that s/he can be offered the best possible option.
e) The opinions of the expert community and the truth about aneurysms
For empiricists of the Hellenistic period, medicine was a collection of personal observations of whatever proved beneficial or harmful not just once, but repeatedly. But events such as aneurysmal ruptures in patients followed for UAs are too infrequent to be reliably monitored by single individuals or centres. The ancient empiricists recognized this common problem, and proposed that the accumulated experience of numerous individuals over the course of time constituted medical knowledge23. The reliability of these accounts was problematic, a difficulty that was partially countered using the criterion of agreement23. Thus 'medical knowledge' could mean the opinions that are shared by a community of 'knowledgeable' experts. In the absence of reliable knowledge from scientific studies, expert opinions do have some authority. This type of authority is subject to disagreements, rhetorical arguments, motivational biases, as well as pressures from the market and from peers, from custom and fashion. Nevertheless it is commonly recognized as valuable in medical conferences, in the clinical field, by healthcare systems, and in courts of law. After all, 'we do well to trust collective judgement of experts, since in the absence of objective criteria to dictate the choice of each individual, what better criteria could there be than the decision of the expert group?'24.
The notion of expert groups as a threat to democracy or to the 'common good' is a subject beyond the scope of this article, but we still need to remind ourselves of the controversies that can arise from the authority bestowed on opinions and values shared by a group of individuals trained and licensed in a peculiar fashion25. There are a number of characteristics that experts share by virtue of training which licenses their membership in one community24. Certain theories and propositions are believed by nearly all members of the group. It is actually quite difficult for individuals to resist accepting dominant beliefs of a group of which they form part, though of course dissidents and hereticsdo occur 26.
A new recruit is trained to know and to accept these beliefs as a condition for entry to the group. Many of the same considerations apply to religious sects, political parties and so on. According to Pierce's pragmatism, 'truth is the opinion which is fated to be ultimately agreed to by all who investigate', but this may sever the relation between beliefs and facts which would be said to verify them 27. Could we simply agree and act without evidence? With this concept it would seem that truth could be determined by voting, clearly an unsatisfactory result. We could just vote that we should treat unruptured aneurysms, and forget about any proof of potential benefits.
This won't do.
There must be some relation between opinions and 'truths' regarding unruptured aneur- ysms. Modern physicians submit their beliefs to the test of reality and require positive results of a clinical trial before recommending a therapeutic regimen on a regular basis. However, before such results become available, a tension arises between their beliefs and their determination to confront them with reality. Relying on beliefs to act on an everyday basis is such a habit for clinicians that the sceptical stance necessarily involved in participation in a trial is not natural at Al11-13.
The tension between beliefs and 'suspension of judgment' may thus hamper the progress of the clinical trial designed to solve the clinical dilemma. There are two ways out of this tension. One is external, authoritative, and appeals to a legal enforcement: One can impose laws prohibiting the clinical use of drugs or devices without the approval of some regulatory agency that in turn requires clinical trials prior to commercialization. This procedure may endanger the privileged doctor-patient relationship, open the door to bureaucratic or third- party control of medicine, threaten autonomy and perhaps slow progress. Alternatively one can appeal to an ethical imperative, self-imposed by the expert community, an autonomous determination to recommend a treatment and act only once action has proved beneficial, using the prudent and rational apparatus of the clinical trial.
f) The uncertainty and community equipoise
Many physicians feel they cannot enrol a patient into a trial because in such or other circumstance they have a 'therapeutic obligation' 9. A review of the historical context in which the confrontation between the notions of 'therapeutic obligation' and 'scientific methods in clinical research' has been introduced reveals a fallacy behind this apparent controver- sy9. Commissioners confronted with historical scandals regarding the use of human subjects in research were asked to review and propose ways to regulate clinical research, assuming a mature, solid state, static medical practice 28. But such an opposition between scientific progress and ethics of practice is ill-advised, as candidly claimed by J. Dewey: 'As my study and thinking progressed, I became more and more troubled by the intellectual scandal involved in the current dualism between something called 'science' on the one hand and something called 'morals' on the other... ' 29. What could be the meaning of an ethical principle such as a 'therapeutic obligation', forcing physicians to offer the 'best possible care' but prohibiting the only means of determining reliably what the 'best treatment' could be?
Clearly any modern account of an ethics of medical practice should accommodate the need for clinical trials, our only means to achieve reliable knowledge of the consequences of our actions. Trials are difficult to realize, partly because unwarranted beliefs are deeply entrenched in the expert community. The opinions of expert clinicians who will be asked to enrol patients into the trial may influence the types of cases that will be included and hence impact on trial results.
Many clinicians rely on an individual calculus of risks based on a priori estimates multiplied by years of life expectancy. This procedure is a natural extension of the analogical type of reasoning that remains the only available option in routine individual clinical decisions, but it is applied at the wrong end of the inquiry. How can reliable knowledge precede verification? Far from providing evidential proof to guide clinical actions, this procedure can only support provisional, fallible hypotheses that must be subjected to the inquiry. Nevertheless a realistic anticipation of the behaviour of clinical investigators must take into consideration the possibility that for some types of cases, beliefs are so entrenched that the clinical prejudices in favour of treatment may not be overcome. If expert opinions can set the stage for a frequent interpretation of the notion of equipoise (community equipoise rather than individual equipoise) 9, then we may have to accept that the 12 mm basilar aneurysm, which enjoyed a nearly unanimous verdict, lies outside the scope of the current community equipoise. We have seen above that the uncertainty becomes more available within the clinical trial context.
We can also hope for further loosening of clinical pseudo-certainties as enrolment progresses. We believe there is currently no scientific proof to support the treatment of any type of lesion. However, if experts cannot be convinced that in this particular case of a large basilar aneurysm, in which treatment risks are higher, chances of success lower, risks of recurrences higher, and consequently treatment benefits for this aneurysm as uncertain as for others, we may have to accept that they will not enrol a sufficient sample of this type of aneurysms to provide clear evidential support that the general conclusions of the trial apply to this particular group. This must be considered an unfortunate consequence of our human nature however, and the results of this survey should not be used as an authoritative prescription of who should legitimately be included in the trial. We believe that leaders of the field should emphasize that the uncertainty, no matter how uncomfortable, can only be lifted by proof established by using rigorous methodology, and that judgement should be suspended until concrete facts are compelling enough to justify the adoption of a treatment recommendation. The scientific method remains instrumental to autonomous and reliable knowledge; it is a crucial tool in our quest for freedom and truth, essential to protect both patients and physicians from the tyranny of unjustified beliefs, motivational biases and extraneous pressures.
Conclusions
Endovascular experts are in general in favour of treatment of unruptured aneurysms, even for lesions that do not justify treatments, at least according to available registries. Their beliefs vary widely but they are coherent, probably optimistic and remain unsupported by evidential proof.
A randomized trial is required to justify preventive treatment of unruptured aneurysm; the suspension of judgement that is necessary to enrol patients may become more prevalent once physicians switch from a traditional 'Doctor knows best' context, in which they are forced to come up with a decision, albeit unwarranted, to the clinical trial context, in which they can acknowledge the current medical uncertainty and work to provide a reliable answer to the present clinical dilemma.
Acknowledgement
The authors gratefully acknowledge the participation of the ABC WIN meeting attendees who took part in the survey; without your help and your patience this would not have been possible. Thank you.
References
- 1.Bacon F. First book: Of the proficience and advancement of learning, divine and human. Part V, section 8. 1605. 2004. Apr, The advancement of Learning. Available from the Gutenberg project: Release #5500. URL: http://www.gutenberg.org/wiki/Main_Page . Acessed June 29th, 2007. [Google Scholar]
- 2.Wiebers DO, Whisnant JP, et al. Unruptured intracranial aneurysms: Natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003;362:103–110. doi: 10.1016/s0140-6736(03)13860-3. [DOI] [PubMed] [Google Scholar]
- 3.Tversky A, Kahneman D. Judgment under uncertainty: Heuristics and biaises. Science. 1974:1124–1131. doi: 10.1126/science.185.4157.1124. [DOI] [PubMed] [Google Scholar]
- 4.Rasmussen P, Mayberg M. Defining the natural history of unruptured aneurysms. Stroke. 2004;35:232–233. doi: 10.1161/01.STR.0000107769.23095.FE. [DOI] [PubMed] [Google Scholar]
- 5.Vindlacheruvu RR, Mendelow AD, Mitchell P. Risk- benefit analysis of the treatment of unruptured intracranial aneurysms. J Neurol Neurosurg Psychiatry. 2005;76(2):234–239. doi: 10.1136/jnnp.2003.031930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raymond J, Meder JF, et al. The Trial On Endovascular Aneurysm Management Team Collaborative Group. Unruptured intracranial aneurysms: the unreliability of clinical judgment, the necessity for evidence, and reasons to participate in a randomized trial. J Neuroradiol. 2006;33(4):211–219. doi: 10.1016/s0150-9861(06)77266-2. [DOI] [PubMed] [Google Scholar]
- 7.Raymond J, Meder JF, et al. Trial on Endovascular Aneurysm Management (TEAM) collaborative group. Trial on endovascular treatment of unruptured aneurysms (TEAM): study monitoring and rationale for trial interruption or continuation. J Neuroradiol. 2007;34(1):33–41. doi: 10.1016/j.neurad.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 8.Raymond J, Chagnon M, et al. A randomized trial on the safety and efficacy of endovascular treatment of unruptured intracranial aneurysms is feasible. Interventional Neuroradiology. 2004;10:103–112. doi: 10.1177/159101990401000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gifford F. Community-equipoise and the ethics of randomized clinical trials. Bioethics. 1995;9(2):127–148. doi: 10.1111/j.1467-8519.1995.tb00306.x. [DOI] [PubMed] [Google Scholar]
- 10.Miller PB, Weijer C. Rehabilitating equipoise. Kennedy Inst Ethics J. 2003;13(2):93–118. doi: 10.1353/ken.2003.0014. [DOI] [PubMed] [Google Scholar]
- 11.McCulloch P, Kaul A, et al. Tolerance of uncertainty, extroversion, neuroticism and attitudes to randomized controlled trials among surgeons and physicians. Br J Surg. 2005;92(10):1293–1297. doi: 10.1002/bjs.4930. [DOI] [PubMed] [Google Scholar]
- 12.Young J, Harrison J, et al. Developing measures of surgeons’ equipoise to assess the feasibility of randomized controlled trials in vascular surgery. Surgery. 2004;136(5):1070–1076. doi: 10.1016/j.surg.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 13.Fung EK, Lore JM., Jr Randomized controlled trials for evaluating surgical questions. Arch Otolaryngol Head Neck Surg. 2002;128(6):631–634. doi: 10.1001/archotol.128.6.631. [DOI] [PubMed] [Google Scholar]
- 14.Raymond J, Guilbert F, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke. 2003;34:1398–1403. doi: 10.1161/01.STR.0000073841.88563.E9. [DOI] [PubMed] [Google Scholar]
- 15.Kahneman D, Lovallo D. Timid choices and bold forecasts: A cognitive perspective on risk taking. Management Science. 1993;39:17–31. [Google Scholar]
- 16.Wermer MJ, van der Schaaf IC, et al. Risk of rupture of unruptured intracranial aneurysms in relation to patient and aneurysm characteristics: an updated metaanalysis. Stroke. 2007;38(4):1404–1410. doi: 10.1161/01.STR.0000260955.51401.cd. [DOI] [PubMed] [Google Scholar]
- 17.Mills JL. Data torturing. N Engl J Med. 1993;329(16):1196–1199. doi: 10.1056/NEJM199310143291613. [DOI] [PubMed] [Google Scholar]
- 18.Rinkel GJE, Djibuti M, et al. Prevalence and Risk of Rupture of Intracranial Aneurysms. Stroke. 1998;29(1):251–256. doi: 10.1161/01.str.29.1.251. [DOI] [PubMed] [Google Scholar]
- 19.Juvela S, Porras M, Heiskanen O. Natural history of unruptured intracranial aneurysms: a long-term follow-up study. J Neurosurg. 1993;79(2):174–182. doi: 10.3171/jns.1993.79.2.0174. [DOI] [PubMed] [Google Scholar]
- 20.Taylor SE, Brown JD. Illusion and well-being: A social psychological perspective on mental health. Psychological Bulletin. 1988;103:193–210. [PubMed] [Google Scholar]
- 21.Pascal B. Les Provinciales, ou, Les Lettres écrites par Louis de Montalte à un provincial de ses amis et aux révérends pères Jésuites sur le sujet de la morale et de la politique de ces pères. Paris: Librairie de Firmin Didot Frères, fils et cie; 1853. p. 455. [Google Scholar]
- 22.Jonsen AR, Toulmin SE. The Abuse of Casuistry a History of Moral Reasoning. Los Angeles, CA, USA: University of California Press; 1988. Casuistry confounded: Pascal’s critique; pp. 231–249. [Google Scholar]
- 23.Cambiano G. Philosophy, Science and Medicine. In: Algra K, Barnes J, Mansfeld J, Schofield M, editors. The Cambridge History of Hellenistic Philosophy. New York, NY, USA: Cambridge University Press; 2000. pp. 586–616. [Google Scholar]
- 24.Khun TS. The Essential Tension: Selected Studies in Scientific Tradition and Change. Chicago, USA: The University of Chicago Press; 1977. Objectivity, value, judgement and theory choice; pp. 320–339. [Google Scholar]
- 25.Goldman AI. Experts: which ones should you trust? In: Selinger E, Crease RP, editors. The Philosophy of Expertise. New York, NY: Columbia University Press; 2006. p. 1438. [Google Scholar]
- 26.Gillies D. Keynes and Probability. In: Bateman , editor. The Cambridge Companion to Keynes, Backhouse. Cambridge: Cambridge University Press; 2006. [Google Scholar]
- 27.Russell B. History of Western Philosophy. New York, NY, USA: Simon & Schuster Inc., publishers; 1972. p. 736. [Google Scholar]
- 28.National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. The Belmont Report: Ethical Principles and Guidelines for Research Involving Human Subjects. Washington DC: US Govt Printing Office (DHEW); 1978. [US DHHS Publication GPO 887-809] [Google Scholar]
- 29.Dewey J. Contemporary American Philosophers. Volume II. New York, NY: The Macmillan Company; 1930. From absolutism to experimentalism; pp. 13–27. [Google Scholar]