Recognition of the importance of cough in clinical medicine was the impetus for the original evidence-based consensus panel report on “Managing Cough as a Defense Mechanism and as a Symptom,” published in 1998,1 and this updated revision. Compared to the original cough consensus statement, this revision (1) more narrowly focuses the guidelines on the diagnosis and treatment of cough, the symptom, in adult and pediatric populations, and minimizes the discussion of cough as a defense mechanism; (2) improves on the rigor of the evidence-based review and describes the methodology in a separate section; (3) updates and expands, when appropriate, all previous sections; and (4) adds new sections with topics that were not previously covered. These new sections include nonasthmatic eosinophilic bronchitis (NAEB); acute bronchitis; nonbronchiectatic suppurative airway diseases; cough due to aspiration secondary to oral/pharyngeal dysphagia; environmental/occupational causes of cough; tuberculosis (TB) and other infections; cough in the dialysis patient; uncommon causes of cough; unexplained cough, previously referred to as idiopathic cough; an empiric integrative approach to the management of cough; assessing cough severity and efficacy of therapy in clinical research; potential future therapies; and future directions for research.
To mitigate future diagnostic confusion, two new diagnostic terms have been introduced to replace two older terms that may represent misnomers. The committee unanimously recommends that the term upper airway cough syndrome (UACS) be used in preference to postnasal drip syndrome (PNDS) when discussing cough that is associated with upper airway conditions because it is unclear whether the mechanism of cough is postnasal drip, direct irritation, or inflammation of the cough receptors in the upper airway. The committee also recommends using the term unexplained cough rather than idiopathic cough because it is likely that more than one unknown cause of chronic cough will be discovered. The term idiopathic implies that one is dealing with only one disease.
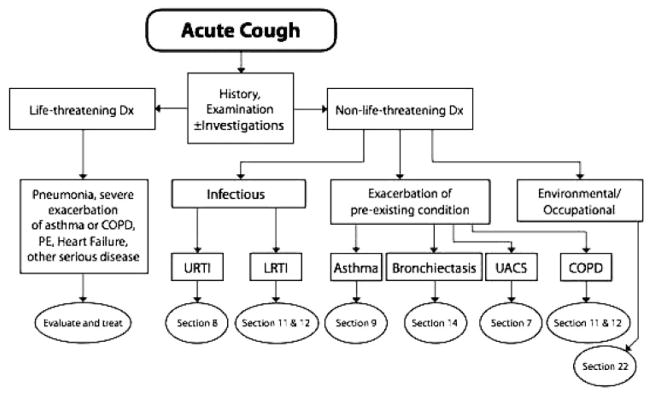
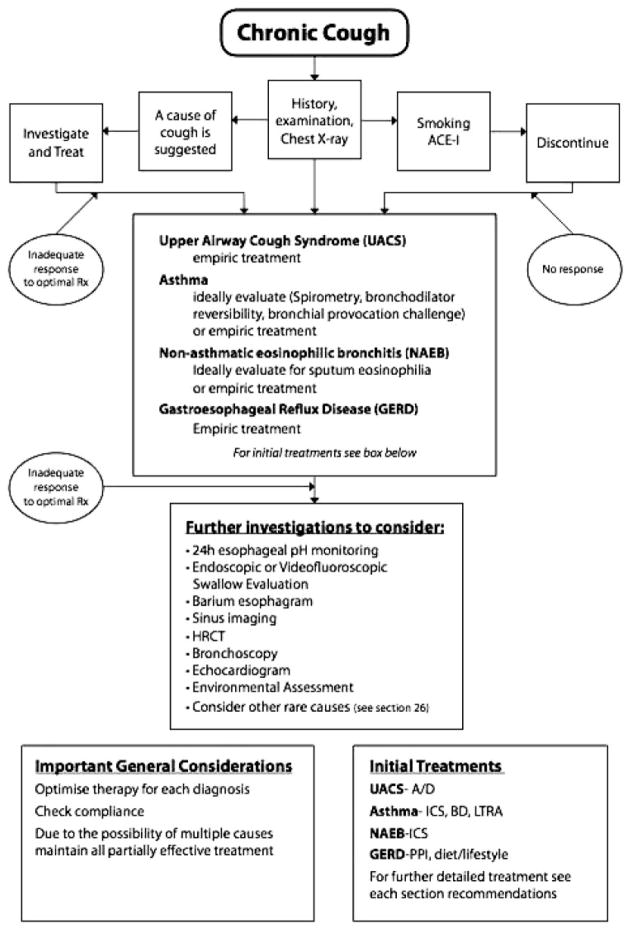
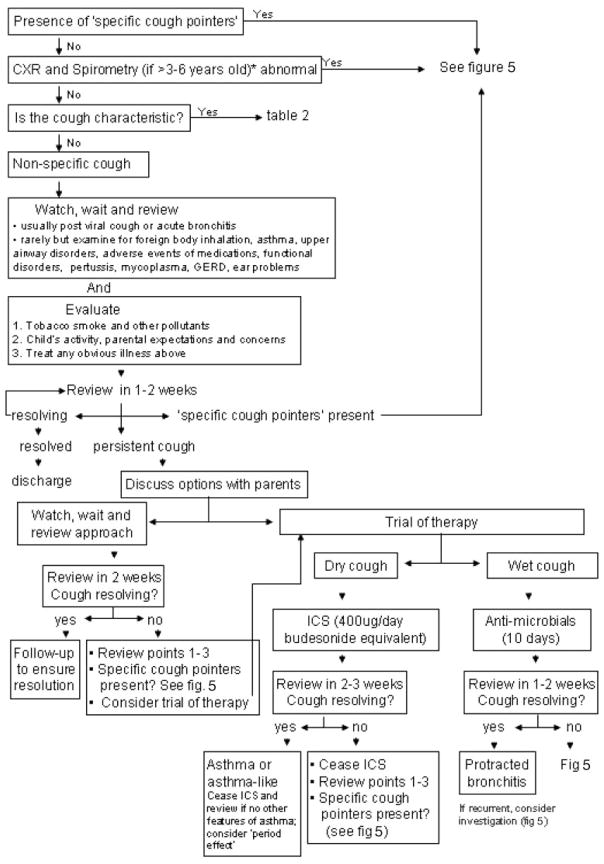
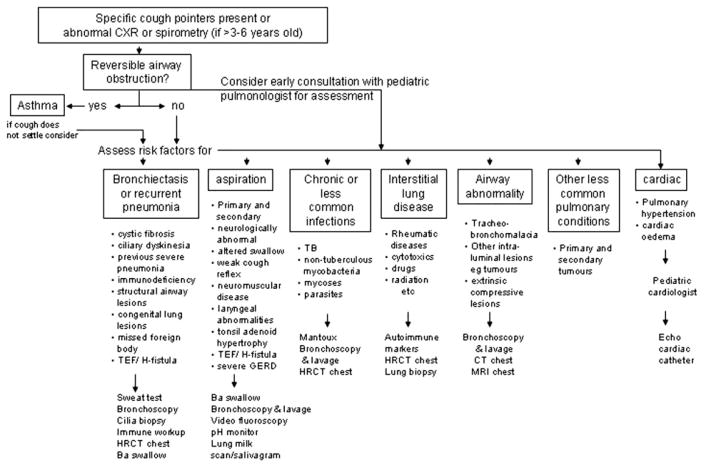
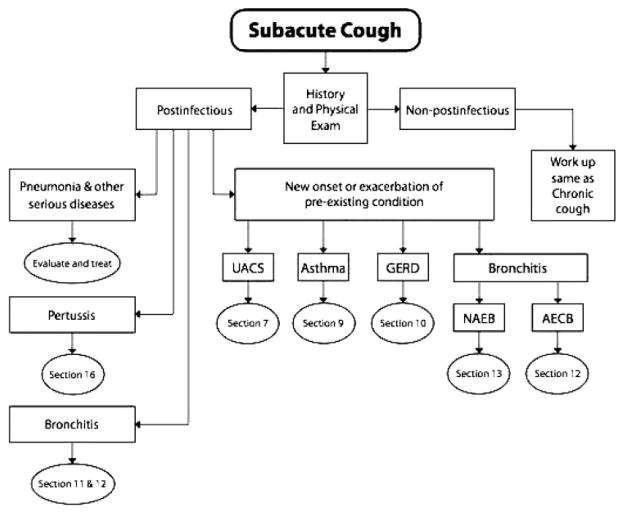
For managing adult patients with cough, the committee recommends an empiric, integrative diagnostic approach, which is presented in the section entitled “An Empiric Integrative Approach to the Management of Cough”.3 Guidelines for managing acute, subacute, and chronic cough are presented in algorithmic form (Fig 1–3). Guidelines with algorithms for evaluating chronic cough in pediatric patients < 15 years of age are presented in the section entitled “Guidelines for Evaluating Chronic Cough in Pediatrics”2,4 [Fig 4, 5]. For a full discussion on how to use the algorithms, please refer to these sections.
Figure 1.
Acute cough algorithm for the management of patients ≥ 15 years of age with cough lasting < 3 weeks. For diagnosis and treatment recommendations refer to the section indicated in the algorithm. PE = pulmonary embolism; Dx = diagnosis; Rx = treatment; URTI = upper respiratory tract infection; LRTI = lower respiratory tract infection. Section 7 = Irwin8; Section 8 = Pratter9; Section 9 = Pratter10; Section 10 = Pratter11; Section 11 = Dicpinigaitis12; Section 12 = Irwin13; Section 13 = Braman14; Section 14 = Braman15; Section 16 = Rosen17; Section 22 = Irwin et al.23
Figure 3.
Chronic cough algorithm for the management of patients ≥ 15 years of age with cough lasting > 8 weeks. ACE-I = ACE inhibitor; BD = bronchodilator; LTRA = leukotriene receptor antagonist; PPI = proton pump inhibitor. See the legend of Figure 1 for abbreviations not used in the text.
Figure 4.
Approach to a child < 15 years of age with chronic cough. There are limitations of the algorithm, which should be read with the accompanying text. Spirometry can usually be reliably performed in children > 6 years of age and in some children > 3 years of age if trained pediatric personnel are present. CXR = chest radiograph.2
Figure 5.
Approach to a child ≤ 14 years of age with chronic specific cough (ie, cough associated with other features suggestive of an underlying pulmonary and/or systemic abnormality). Children > 14 years of age should be managed as outlined in adult guidelines but there is no good evidence where the age cutoff should be. TEF = tracheal esophageal fistula. See the legend of Figure 4 for abbreviation not used in the text.
Summary and Recommendations
Recommendations for each section of these guidelines are listed under their respective section titles. For an in-depth discussion or clarification of each recommendation, readers are encouraged to read the specific section in question in its entirety.
Methodology and Grading of the Evidence for the Diagnosis and Management of Cough5
The recommendations were graded, by consensus by the panel, using the American College of Chest Physicians Health and Science Policy Grading System, which is based on the following two components: quality of evidence; and the net benefit of the diagnostic and therapeutic procedure.
The quality of evidence is rated according to the study design and strength of other methodologies used in the included studies.
The net benefit of the recommendations is based on the estimated benefit to the specific patient population described in each recommendation and not for an individual patient. Usually, the net benefit is a clinical benefit to the population of patients defined in the first phrase of the recommendation, but, in recommendations for future research or other nonclinical recommendations, it may be a societal benefit.
Both the quality of evidence and the net benefit components are listed after each recommendation; their interaction defines the strength of the recommendations.
The recommendations scale is as follows: A, strong; B, moderate; C, weak; D, negative; I, inconclusive (no recommendation possible); E/A, strong recommendation based on expert opinion only; E/B, moderate recommendation based on expert opinion only; E/C, weak recommendation based on expert opinion only; and E/D, negative recommendation based on expert opinion only
Anatomy and Neurophysiology of the Cough Reflex6
There is clear evidence that vagal afferent nerves regulate involuntary coughing.
Coughing, like swallowing, belching, urinating, and defecating, is unique because there is higher cortical control of this visceral reflex.
Cortical control can manifest as cough inhibition or voluntary cough. The implications of this are several-fold: because placebos can have a profound effect on coughing, treatment studies must be placebo-controlled. Because cough can be an affective behavior, psychological issues must be considered as a cause or effect of coughing.
There is a need to study the roles of consciousness and perception in coughing.
Global Physiology and Pathophysiology of Cough7
In patients with endotracheal tubes, tracheostomy need not be performed to improve cough effectiveness. Level of evidence, expert opinion; net benefit, substantial; grade of recommendation, E/A
Individuals with neuromuscular weakness and no concomitant airway obstruction may benefit from mechanical aids to improve cough. Level of evidence, low; net benefit, intermediate; grade of recommendation, C
In patients with ineffective cough, the clinician should be aware of and monitor for possible complications, such as pneumonia, atelectasis, and/or respiratory failure. Level of evidence, low; net benefit, substantial; grade of recommendation, B
Complications of Cough8
In patients complaining of cough, evaluate for a variety of complications associated with coughing (eg, cardiovascular, constitutional, GI, genitourinary, musculoskeletal, neurologic, ophthalmologic, psychosocial, and skin complications), which can lead to a decrease in a patient’s health-related quality of life. Level of evidence, low; benefit, substantial; grade of recommendation, B
Patients with cough should have a thorough diagnostic evaluation, according to the guidelines set forth in this document, to mitigate or prevent these complications. Level of evidence, low; net benefit, substantial; grade of recommendation, B
Overview of Common Causes of Chronic Cough9
In patients with chronic cough and a normal chest roentgenogram finding who are non-smokers and are not receiving therapy with an angiotensin-converting enzyme (ACE) inhibitor, the diagnostic approach should focus on the detection and treatment of UACS (formerly called PNDS), asthma, NAEB, or GERD, alone or in combination. This approach is most likely to result in a high rate of success in achieving cough resolution. Level of evidence, low; benefit, substantial; grade of recommendation, B
In all patients with chronic cough, regardless of clinical signs or symptoms, because UACS (formerly called PNDS), asthma, and GERD each may present only as cough with no other associated clinical findings (ie, “silent PNDS,” “cough variant asthma,” and “silent GERD”), each of these diagnoses must be considered. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with chronic cough, neither the patient’s description of his or her cough in terms of its character or timing, nor the presence or absence of sputum production, should be used to rule in or rule out a diagnosis or to determine the clinical approach. Level of evidence, low; benefit, substantial; grade of recommendation, B
Chronic Upper Airway Cough Syndrome Secondary to Rhinosinus Diseases (Previously Referred to as Postnasal Drip Syndrome)10
In patients with chronic cough that is related to upper airway abnormalities, the committee considers the term UACS to be more accurate, and it should therefore be used instead of the term PNDS. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In patients with chronic cough, the diagnosis of UACS-induced cough should be determined by considering a combination of criteria, including symptoms, physical examination findings, radiographic findings, and, ultimately, the response to specific therapy. Because it is a syndrome, no pathognomonic findings exist. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients in whom the cause of the UACS-induced cough is apparent, specific therapy directed at this condition should be instituted. Level of evidence, low; benefit, substantial; grade of recommendation, B
For patients with chronic cough, an empiric trial of therapy for UACS should be administered because the improvement or resolution of cough in response to specific treatment is the pivotal factor in confirming the diagnosis of UACS as a cause of cough. Level of evidence, low; benefit, substantial; grade of recommendation, B
A patient suspected of having UACS-induced cough who does not respond to empiric antihistamine/decongestant (A/D) therapy with a first-generation antihistamine should next undergo sinus imaging. Although chronic sinusitis may cause a productive cough, it may also be clinically silent, in that the cough can be relatively or even completely nonproductive and none of the typical findings associated with acute sinusitis may be present. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients for whom a specific etiology of chronic cough is not apparent, empiric therapy for UACS in the form of a first-generation A/D preparation should be prescribed before beginning an extensive diagnostic workup. Level of evidence, low; benefit, intermediate; grade of recommendation, C
Cough and the Common Cold11
Patients with acute cough (as well as PND and throat clearing) associated with the common cold can be treated with a first-generation A/D preparation (brompheniramine and sustained-release pseudoephedrine). Naproxen can also be administered to help decrease cough in this setting. Level of evidence, fair; benefit, substantial; grade of recommendation, A
In patients with the common cold, newer generation nonsedating antihistamines are ineffective for reducing cough and should not be used. Level of evidence, fair; benefit, none; grade of recommendation, D
In patients with cough and acute URTI, because symptoms, signs, and even sinus-imaging abnormalities may be indistinguishable from acute bacterial sinusitis, the diagnosis of bacterial sinusitis should not be made during the first week of symptoms. (Clinical judgment is required to decide whether to institute antibiotic therapy.) Level of evidence, fair; benefit, none; grade of recommendation, D
Chronic Cough Due to Asthma12
-
1
In a patient with chronic cough, asthma should always be considered as a potential etiology because asthma is a common condition with which cough is commonly associated. Quality of evidence, fair; net benefit, substantial; grade of recommendation, A
-
2
In a patient suspected of having CVA but in whom physical examination and spirometry findings are nondiagnostic, MIC testing should be performed to confirm the presence of asthma. However, a diagnosis of CVA as the cause of cough is established only after the resolution of cough with specific antiasthmatic therapy. If MIC testing cannot be performed, empiric therapy should be administered; however, a response to steroid therapy will not exclude NAEB as an etiology of the patient’s cough. Quality of evidence, good; net benefit, substantial; grade of recommendation, A
-
3
Patients with cough due to asthma should initially be treated with a standard antiasthmatic regimen of inhaled bronchodilators and inhaled corticosteroids (ICSs). Quality of evidence, fair; net benefit, substantial; grade of recommendation, A
-
4
In patients whose cough is refractory to treatment with ICSs, an assessment of airway inflammation should be performed whenever available and feasible. The demonstration of persistent airway eosinophilia during such an assessment will identify those patients who may benefit from more aggressive antiinflammatory therapy. Quality of evidence, low; net benefit, substantial; grade of recommendation, B
-
5a
For patients with asthmatic cough that is refractory to treatment with ICSs and bronchodilators, in whom poor compliance or another contributing condition has been excluded, a leukotriene receptor antagonist may be added to the therapeutic regimen before the escalation of therapy to systemic corticosteroids. Quality of evidence, fair; net benefit, intermediate; grade of recommendation, B
-
5b
Patients with severe and/or refractory cough due to asthma should receive a short course (1 to 2 weeks) of systemic (oral) corticosteroids followed by ICSs. Quality of evidence, low; net benefit,: substantial; grade of recommendation, B
Chronic Cough Due to Gastroesophageal Reflux Disease13
In patients with chronic cough due to gastroesophageal reflux disease (GERD), the term acid reflux disease, unless it can be definitively shown to apply, should be replaced by the more general term reflux disease so as not to mislead the clinicians into thinking that all patients with cough due to GERD should improve with acid-suppression therapy. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In patients with chronic cough who also complain of typical and frequent GI complaints such as daily heartburn and regurgitation, especially when the findings of chest-imaging studies and/or clinical syndrome are consistent with an aspiration syndrome, the diagnostic evaluation should always include GERD as a possible cause. Level of evidence, low; benefit, substantial; grade of recommendation, B
Patients with chronic cough who have GI symptoms that are consistent with GERD or who fit the clinical profile described in Table 1 in Irwin13, should be considered to have a high likelihood of having GERD and should be prescribed antireflux treatment even when they have no GI symptoms. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with chronic cough, it should not be assumed that GERD has been definitively ruled out as a cause of cough simply because there is a history of antireflux surgery. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with chronic cough, while tests that link GERD with cough suggest a potential cause-effect relationship, a definitive diagnosis of cough due to GERD requires that cough nearly or completely disappear with antireflux treatment. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with chronic cough being evaluated for GERD, the 24-h esophageal pH-monitoring test is the most sensitive and specific test; however, it is recommended that the test results be interpreted as normal only when conventional indices for acid reflux are within the normal range and no reflux-induced coughs appear during the monitoring study. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with cough who are undergoing 24-h monitoring, a low percentage of coughs associated with (or induced by) reflux does not exclude a diagnosis of cough due to GERD. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with cough due to GERD, the degree of abnormality noted in the esophageal pH-monitoring variables, such as the frequency and duration of reflux events, does not directly correlate with the severity of the patients’ cough. Level of evidence, low; benefit, substantial; grade of recommendation, B
In diagnosing nonacid GERD as the cause of cough, barium esophagography may be the only available test to reveal GER of potential pathologic significance in this setting (see the “Discussion” section regarding esophageal impedance monitoring). When this is the case, barium esophagography is the test of choice to reveal GER of potential pathologic significance. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with cough due to GERD, a normal esophagoscopy finding does not rule out GERD as the cause of cough. Level of evidence, low; benefit, substantial; grade of recommendation, B
For patients fitting the clinical profile for cough due to GERD, it is recommended that treatment be initially started in lieu of testing. Level of evidence, low; benefit, substantial; grade of recommendation, B
For patients fitting the clinical profile for cough due to GERD, the performance of 24-h esophageal pH monitoring is recommended on therapy when cough does not improve or resolve to assist in determining whether the therapy needs to be intensified or if medical therapy has failed. Level of evidence, low; benefit, substantial; grade of recommendation, B
For patients with chronic cough, the following tests are not routinely recommended to link cough with GERD: (a) assessing for lipid-laden macrophages in BAL fluid and induced sputum, because this test has not been studied in patients with chronic cough and because a positive test result is not specific for aspiration; (b) exhaled nitric oxide measurements, because they do not appear to be helpful in diagnosing cough due to GERD; (c) a Bernstein test, because a negative Bernstein test result cannot be used to exclude the diagnosis of cough due to GERD; and (d) inhaled tussigenic challenges with capsaicin, because they are not specific for coughs due to GERD and because the test result can be positive in patients with GERD without cough. Level of evidence, low; benefit, conflicting; grade of recommendation, I
In patients who meet the clinical profile predicting that silent GERD is the likely cause of chronic cough or in patients with chronic cough who also have prominent upper GI symptoms consistent with GERD, an empiric trial of medical antireflux therapy is recommended. Level of evidence, low; benefit, substantial; grade of recommendation, B
For treating the majority of patients with chronic cough due to GERD, the following medical therapies are recommended: (a) dietary and lifestyle modifications; (b) acid suppression therapy; and (c) the addition of prokinetic therapy either initially or if there is no response to the first two therapies. The response to these therapies should be assessed within 1 to 3 months. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In patients in which this empiric treatment fails, it cannot be assumed that GERD has been ruled out as a cause of chronic cough; rather, the objective investigation for GERD is then recommended because the empiric therapy may not have been intensive enough or medical therapy may have failed. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In some patients, cough due to GERD will favorably respond to acid suppression therapy alone; proton pump inhibition may be effective when H2-antagonism has been ineffective; prokinetic therapy and diet, when added to proton pump inhibition, may be effective when proton pump inhibition alone has been ineffective. Level of evidence, low; benefit, substantial; grade of recommendation, B
Patients requiring an intensive medical treatment regimen should be treated with the following: (a) antireflux diet that includes no > 45 g of fat in 24 h and no coffee, tea, soda, chocolate, mints, citrus products, including tomatoes, or alcohol, no smoking, and limiting vigorous exercise that will increase intraabdominal pressure; (b) acid suppression with a proton pump inhibitor; (c) prokinetic therapy; and (d) efforts to mitigate the influences of comorbid diseases such as obstructive sleep apnea or therapy for comorbid conditions (eg, nitrates, progesterone, and calcium channel blockers) whenever possible. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In patients with chronic cough due to GERD that has failed to improve with the most maximal medical therapy, which includes an intensive antireflux diet and lifestyle modification, maximum acid suppression, and prokinetic therapy, and the rest of the spectrum of treatment options in Table 3 in Irwin,13 cough may only improve or be eliminated with antireflux surgery. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients who meet the following criteria, antireflux surgery is the recommended treatment: (a) findings of a 24-h esophageal pH-monitoring study before treatment is positive, as defined above; (b) patients fit the clinical profile suggesting that GERD is the likely cause of their cough (Table 1 in Irwin13); (c) cough has not improved after a minimum of 3 months of intensive therapy (Table 3 in Irwin13), and serial esophageal pH-monitoring studies or other objective studies (eg, barium esophagography, esophagoscopy, and gastric-emptying study with solids) performed while the patient receives therapy show that intensive medical therapy has failed to control the reflux disease and that GERD is still the likely cause of cough; and (d) patients express the opinion that their persisting cough does not allow them a satisfactory quality of life. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
Chronic Cough Due to Acute Bronchitis14
-
1
In a patient with an acute respiratory infection manifested predominantly by cough, with or without sputum production, lasting no more than 3 weeks, a diagnosis of acute bronchitis should not be made unless there is no clinical or radiographic evidence of pneumonia, and the common cold, acute asthma, or an exacerbation of COPD have been ruled out as the cause of cough. Quality of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
-
2
In patients with the presumed diagnosis of acute bronchitis, viral cultures, serologic assays, and sputum analyses should not be routinely performed because the responsible organism is rarely identified in clinical practice. Quality of evidence, low; benefit, intermediate; grade of recommendation, C
-
3
In patients with acute cough and sputum production suggestive of acute bronchitis, the absence of the following findings reduces the likelihood of pneumonia sufficiently to eliminate the need for a chest radiograph: (1) heart rate > 100 beats/min; (2) respiratory rate > 24 breaths/min; (3) oral body temperature of > 38°C; and (4) chest examination findings of focal consolidation, egophony, or fremitus. Quality of evidence, low; benefit, substantial; grade of recommendation, B
-
4a
For patients with the putative diagnosis of acute bronchitis, routine treatment with antibiotics is not justified and should not be offered. Quality of evidence, good; benefit, none; grade of recommendation, D
-
4b
For these patients, the decision not to use an antibiotic should be addressed individually and explanations should be offered because many patients expect to receive an antibiotic based on previous experiences and public expectation. Quality of evidence, expert opinion; benefit, intermediate; grade of recommendation, E/B
-
5
Children and adult patients with confirmed and probable whooping cough should receive a macrolide antibiotic and should be isolated for 5 days from the start of treatment; early treatment within the first few weeks will diminish the coughing paroxysms and prevent spread of the disease; the patient is unlikely to respond to treatment beyond this period. Level of evidence, good; net benefit, substantial; grade of evidence, A
-
6a
In most patients with a diagnosis of acute bronchitis, β2-agonist bronchodilators should not be routinely used to alleviate cough. Quality of evidence, fair; benefit, none; grade of recommendation, D
-
6b
In select adult patients with a diagnosis of acute bronchitis and wheezing accompanying the cough, treatment with β2-agonist bronchodilators may be useful. Quality of evidence, fair; benefit, small/weak; grade of recommendation, C
-
7
In patients with a diagnosis of acute bronchitis, antitussive agents are occasionally useful and can be offered for short-term symptomatic relief of coughing. Quality of evidence, fair; benefit, small/weak; grade of recommendation, C
-
8
In patients with a diagnosis of acute bronchitis, because there is no consistent favorable effect of mucokinetic agents on cough, they are not recommended. Quality of evidence, fair; benefit, conflicting; grade of recommendation, I
Chronic Cough Due to Chronic Bronchitis15
-
1
Adults who have a history of chronic cough and sputum expectoration occurring on most days for at least 3 months and for at least 2 consecutive years should be given a diagnosis of chronic bronchitis when other respiratory or cardiac causes of chronic productive cough are ruled out. Level of evidence, low; net benefit, substantial; grade of recommendation, B
-
2
The evaluation of patients with chronic cough should include a complete history regarding exposures to respiratory irritants including cigarette, cigar, and pipe smoke; passive smoke exposures; and hazardous environments in the home and workplace. All are predisposing factors of chronic bronchitis. Level of evidence, low; net benefit, substantial; grade of recommendation, B
-
3
Smoke-free workplace and public place laws should be enacted in all communities. Level of evidence, expert opinion; net benefit, substantial; grade of recommendation, E/A
-
4
Stable patients with chronic bronchitis who have a sudden deterioration of symptoms with increased cough, sputum production, sputum purulence, and/or shortness of breath, which are often preceded by symptoms of an upper respiratory tract infection, should be considered to have an acute exacerbation of chronic bronchitis, as long as conditions other than acute tracheobronchitis are ruled out or are considered unlikely. Level of evidence, expert opinion; net benefit, substantial; grade of recommendation, E/A
-
5
In patients with chronic cough who have chronic exposure to respiratory irritants, such as personal tobacco use, passive smoke exposure, and workplace hazards, avoidance should always be recommended. It is the most effective means to improve or eliminate the cough of chronic bronchitis. Ninety percent of patients will have resolution of their cough after smoking cessation. Level of evidence, good; net benefit, substantial; grade of recommendation, A
-
6
In stable patients with chronic bronchitis, there is no role for long-term prophylactic therapy with antibiotics. Level of evidence, low; benefit, none; grade of recommendation, I
-
7
In patients with acute exacerbations of chronic bronchitis, the use of antibiotics is recommended; patients with severe exacerbations and those with more severe airflow obstruction at baseline are the most likely to benefit. Level of evidence, fair; net benefit, substantial; grade of recommendation, A
-
8
In stable patients with chronic bronchitis, the clinical benefits of postural drainage and chest percussion have not been proven, and they are not recommended. Level of evidence, fair; net benefit, conflicting; grade of recommendation, I
-
9
In patients with an acute exacerbation of chronic bronchitis, the clinical benefits of postural drainage and chest percussion have not been proven, and they are not recommended. Level of evidence, fair; net benefit, conflicting; grade of recommendation, I
-
10a
In stable patients with chronic bronchitis, therapy with short-acting β-agonists should be used to control bronchospasm and relieve dyspnea; in some patients, it may also reduce chronic cough. Level of evidence, good; net benefit, substantial; grade of recommendation, A
-
10b
In stable patients with chronic bronchitis, therapy with ipratropium bromide should be offered to improve cough. Level of evidence, fair; net benefit, substantial; grade of recommendation, A
-
10c
In stable patients with chronic bronchitis, treatment with theophylline should be considered to control chronic cough; careful monitoring for complications is necessary. Level of evidence, fair; net benefit, substantial; grade of recommendation, A
-
11
For patients with an acute exacerbation of chronic bronchitis, therapy with short-acting β-agonists or anticholinergic bronchodilators should be administered during the acute exacerbation. If the patient does not show a prompt response, the other agent should be added after the first is administered at the maximal dose. Level of evidence, good; net benefit, substantial; grade of recommendation, A
-
12
For patients with an acute exacerbation of chronic bronchitis, theophylline should not be used for treatment. Level of evidence, good; net benefit, none; grade of recommendation, D
-
13
For stable patients with chronic bronchitis, there is no evidence that the currently available expectorants are effective and therefore they should not be used. Level of evidence, low; net benefit, none; grade of recommendation, I
-
14
In stable patients with chronic bronchitis, treatment with a long-acting β-agonist when coupled with an ICS should be offered to control chronic cough. Level of evidence, good; net benefit, substantial; grade of recommendation, A
-
15
For stable patients with chronic bronchitis and an FEV1 of < 50% predicted or for those patients with frequent exacerbations of chronic bronchitis, ICS therapy should be offered. Level of evidence, good; net benefit, substantial; grade of recommendation, A
-
16
For stable patients with chronic bronchitis, long-term maintenance therapy with oral corticosteroids such as prednisone should not be used; there is no evidence that it improves cough and sputum production, and the risks of serious side effects are high. Level of evidence, expert opinion; net benefit, negative; grade of recommendation, E/D
-
17
For patients with an acute exacerbation of chronic bronchitis, there is no evidence that the currently available expectorants are effective, and therefore they should not be used. Level of evidence, low; net benefit, none; grade of recommendation, I
-
18
For patients with an acute exacerbation of chronic bronchitis, a short course (10 to 15 days) of systemic corticosteroid therapy should be given; IV therapy in hospitalized patients and oral therapy for ambulatory patients have both proven to be effective. Level of evidence, good; net benefit, substantial; grade of recommendation, A
-
19
In patients with chronic bronchitis, central cough suppressants such as codeine and dextromethorphan are recommended for short-term symptomatic relief of coughing. Level of evidence, fair; benefit, intermediate; grade of evidence, B
Chronic Cough Due to Nonasthmatic Eosinophilic Bronchitis16
In patients with chronic cough who have normal chest radiograph findings, normal spirometry findings, and no evidence of variable airflow obstruction or airway hyperresponsiveness, the diagnosis of NAEB should be considered. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In patients with chronic cough with normal chest radiograph findings, normal spirometry findings, and no evidence of variable airflow obstruction or airway hyperresponsiveness, the diagnosis of NAEB as the cause of the chronic cough is confirmed by the presence of airway eosinophilia, either by sputum induction or bronchial wash fluid obtained by bronchoscopy, and an improvement in the cough following corticosteroid therapy. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In patients with chronic cough due to NAEB, the possibility of an occupation-related cause needs to be considered. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
For patients with chronic cough due to NAEB, the first-line treatment is ICSs (except when a causal allergen or sensitizer is identified [see recommendation 5]). Level of evidence, low; benefit, substantial; grade of recommendation, B
For patients with chronic cough due to NAEB, when a causal allergen or occupational sensitizer is identified, avoidance is the best treatment. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
For patients with chronic cough due to NAEB, if symptoms are persistently troublesome and/or the natural history of eosinophilic airway inflammation progresses despite treatment with high-dose ICSs, oral corticosteroids should be given. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
Chronic Cough Due to Bronchiectasis17
In patients with suspected bronchiectasis without a characteristic chest radiograph finding, an high-resolution CT (HRCT) scan of the chest should be ordered because it is the diagnostic procedure of choice to confirm the diagnosis. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients for whom there is no obvious cause, a diagnostic evaluation for an underlying disorder causing bronchiectasis should be performed, because the results may lead to treatment that may slow or halt the progression of disease. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with bronchiectasis with airflow obstruction and/or bronchial hyperreactivity, therapy with bronchodilators may be of benefit. Level of evidence, expert opinion; benefit, small; grade of recommendation, E/C
In patients with bronchiectasis caused by cystic fibrosis (CF), rhDNase should be used to improve spirometry. Level of evidence, low; benefit, small; grade of recommendation, C
In patients with CF, prolonged treatment with systemic corticosteroids should not be offered to most patients because of significant side effects. Level of evidence, low; benefit, conflicting; grade of recommendation, I
In patients with CF, prolonged courses of ibuprofen should not be used. Level of evidence, low; benefit, conflicting; grade of recommendation, I
In patients with idiopathic bronchiectasis, the prolonged systemic administration of antibiotics may produce small benefits in reducing sputum volume and purulence, but may also be associated with intolerable side effects. Level of evidence, low; benefit, conflicting, grade of recommendation, I
In patients with CF, therapy with aerosolized antipseudomonal antibiotics are recommended. Level of evidence, low; benefit, intermediate; grade of recommendation, C
In patients with idiopathic bronchiectasis, aerosolized antibiotics should not be used. Level of evidence, low; benefit, negative; recommendation, D
In patients with conditions associated with the hypersecretion of mucus and the inability to expectorate effectively, chest physiotherapy should be used and patients should be monitored for symptom improvement. Level of evidence, expert opinion; benefit, small/weak; grade of recommendation, E/C
In selected patients with localized bronchiectasis that causes intolerable symptoms despite maximal medical therapy, surgery should be offered. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with exacerbations of bronchiectasis, antibiotics should be used, with the selection of agents depending on the likely pathogens. Level of evidence, low; benefit, substantial; grade of recommendation, B
Chronic Cough Due to Nonbronchiectatic Suppurative Airway Disease (Bronchiolitis)18
In patients with cough and incomplete or irreversible airflow limitation, direct or indirect signs of small airways disease seen on HRCT scan, or purulent secretions seen on bronchoscopy, nonbronchiectatic suppurative airways disease (bronchiolitis) should be suspected as the primary cause. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In patients with cough in whom more common causes have been excluded, because bacterial suppurative airways disease may be present and clinically unsuspected, bronchoscopy is required before excluding it as a cause. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients in whom bronchiolitis is suspected, a surgical lung biopsy should be performed when the combination of the clinical syndrome, physiology, and HRCT findings do not provide a confident diagnosis. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In patients with bacterial bronchiolitis, prolonged antibiotic therapy improves cough and is recommended. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with toxic/antigenic exposure or drug-related bronchiolitis, cessation of the exposure or medication plus corticosteroid therapy for those with physiologic impairment is appropriate. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In the inflammatory bowel disease (IBD) patient with cough, bronchiolitis should be suspected as a potential cause. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients in whom IBD-related bronchiolitis is suspected, both adverse drug reaction and infection should be specifically considered. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In patients with IBD, therapy with both oral corticosteroids and ICSs may improve cough, and a trial of therapy is suggested. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with chronic cough who have recently lived in Japan, Korea, or China, diffuse panbronchiolitis (DPB) should be considered in the evaluations of the cause. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with suspected DPB, an appropriate clinical setting and characteristic HRCT scan findings may obviate the need for invasive testing and a trial of macrolide therapy (erythromycin or other 14-member ring macrolides such as clarithromycin and roxithromycin) is appropriate. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In patients with DPB, prolonged treatment (≥ 2 to 6 months) with erythromycin (or other 14-member ring macrolides such as clarithromycin and roxithromycin) is recommended. Level of evidence, low; benefit, substantial; grade of recommendation, B
Postinfectious Cough19
-
1
When a patient complains of cough that has been present following symptoms of an acute respiratory infection for at least 3 weeks, but not more than 8 weeks, consider a diagnosis of postinfectious cough. Quality of evidence, expert opinion; net benefit, intermediate; strength of recommendation, E/B
-
2
In patients with subacute postinfectious cough, because there are multiple pathogenetic factors that may contribute to the cause of cough (including postviral airway inflammation with its attendant complications such as bronchial hyper-responsiveness, mucus hypersecretion and impaired mucociliary clearance, upper airway cough syndrome [UACS], asthma, and gastroesophageal reflux disease), judge which factors are most likely provoking cough before considering therapy. Quality of evidence, expert opinion; net benefit, intermediate; strength of recommendation, E/B
-
3
In children and adult patients with cough following an acute respiratory tract infection, if cough has persisted for > 8 weeks, consider diagnoses other than postinfectious cough. Quality of evidence, low; net benefit, intermediate; strength of recommendation, C
-
4
For adult patients with postinfectious cough, not due to bacterial sinusitis or early on in a Bordetella pertussis infection, while the optimal treatment is not known:
-
4a
Therapy with antibiotics has no role, as the cause is not bacterial infection. Level of evidence, expert opinion; net benefit, none; grade of evidence, I
-
4b
Consider a trial of inhaled ipratropium as it may attenuate the cough. Level of evidence, fair; net benefit, intermediate; grade of evidence, B
-
4c
In patients with postinfectious cough, when the cough adversely affects the patient’s quality of life and when cough persists despite use of inhaled ipratropinin, consider the use of inhaled corticosteroids. Level of evidence, expert opinion; net benefit, intermediate; grade of evidence, E/B
-
4d
For severe paroxysms of postinfectious cough, consider prescribing 30 to 40 mg of prednisone per day for a short, finite period of time when other common causes of cough (eg, UACS due to rhinosinus diseases, asthma, or gastroesophageal reflux disease) have been ruled out. Level of evidence, low; net benefit, intermediate; grade of evidence, C
-
4e
Central acting antitussive agents such as codeine and dextromethorphan should be considered when other measures fail. Level of evidence, expert opinion; net benefit, intermediate; grade of evidence, E/B
-
5
When a patient has a cough lasting for ≥ 2 weeks without another apparent cause and it is accompanied by paroxysms of coughing, post-tussive vomiting, and/or an inspiratory whooping sound, the diagnosis of a B pertussis infection should be made unless another diagnosis is proven. Level of evidence, low; net benefit, substantial; grade of evidence, B
-
6a
For all patients who are suspected of having whooping cough, to make a definitive diagnosis order a nasopharyngeal aspirate or polymer (Dacron; INVISTA; Wichita, KS) swab of the nasopharynx for culture to confirm the presence of B pertussis. Isolation of the bacteria is the only certain way to make the diagnosis. Level of evidence, low; net benefit, substantial; grade of evidence, B
-
6b
PCR confirmation is available but is not recommended as there is no universally accepted, validated technique for routine clinical testing. Level of evidence, low; net benefit, conflicting; grade of evidence, I
-
7
In patients with suspected pertussis infection, to make a presumptive diagnosis of this infection, order paired acute and convalescent sera in a reference laboratory. A fourfold increase in IgG or IgA antibodies to PT or FHA is consistent with the presence of a recent B pertussis infection. Level of evidence, low; net benefit, intermediate; grade of evidence, C
-
8
A confirmed diagnosis of pertussis infection should be made when a patient with cough has B pertussis isolated from a nasopharyngeal culture or has a compatible clinical picture with an epidemiologic linkage to a confirmed case. Level of evidence, low; net benefit, substantial; grade of evidence, B
-
9
Children and adult patients with confirmed or probable whooping cough should receive a macrolide antibiotic and should be isolated for 5 days from the start of treatment because early treatment within the first few weeks will diminish the coughing paroxysms and prevent spread of the disease; treatment beyond this period may be offered but it is unlikely the patient will respond. Level of evidence, good; net benefit, substantial; grade of evidence, A
-
10
Long-acting β-agonists, antihistamines, corticosteroids, and pertussis Ig should not be offered to patients with whooping cough because there is no evidence that they benefit these patients. Level of evidence, good; net benefit, none; grade of evidence, D
-
11
All children should receive prevention against pertussis infection as part of a complete diphtheria, tetanus, acellular pertussis (DTap) primary vaccination series. This should be followed by a single dose DTap booster vaccination early in adolescence. Level of evidence, good; net benefit, substantial; grade of evidence, A
-
12
For all adults up to the age of 65, vaccination with the stronger formulation of TDap vaccine should be administered according to CDC guidelines. Level of evidence, expert opinion; net benefit, substantial; grade of evidence, E/A
Chronic Cough Due to Lung Tumors20
In a patient with cough who has risk factors for lung cancer or a known or suspected cancer in another site that may metastasize to the lungs, a chest radiograph should be obtained. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In patients with a suspicion of airway involvement by a malignancy (eg, smokers with hemoptysis), even when the chest radiograph findings are normal, bronchoscopy is indicated. Level of evidence, low; benefit, substantial; grade of recommendation, B
For patients with stage I and II non-small cell lung cancer (NSCLC), surgery to remove the NSCLC is the treatment of choice. If cough was caused by a NSCLC that can be surgically removed, the cough will typically cease. Level of evidence, low; benefit, substantial; grade of recommendation, B
For patients with more advanced NSCLC (stages III and IV), external beam radiation and/or chemotherapy should usually be offered. Level of evidence, good; benefit, intermediate; grade of recommendation, A
For patients with dyspnea or hemoptysis due to endobronchial tumors, cough may also be present. Endobronchial methods should be considered for the palliation of these symptoms, but cough alone is seldom a reason to offer such treatment. Level of evidence, fair; benefit, small; grade of recommendation, C
For patients with cough and lung cancer, the use of centrally acting cough suppressants such as dihydrocodeine and hydrocodone is recommended. Level of evidence, low; benefit, intermediate; grade of recommendation, C
Cough and Aspiration of Food and Liquids Due to Oral-Pharyngeal Dysphagia21
-
1
In patients with cough, a medical history particularly directed at identifying conditions increasing the likelihood of oral-pharyngeal dysphagia and aspiration (as indicated in Table 1 in Smith Hammond and Goldstein21) should be obtained. Patients with high-risk conditions should be referred for an oral-pharyngeal swallowing evaluation. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
2a
Patients with cough and their caregivers should be questioned regarding perceived swallowing problems, including an association of cough while eating or drinking and a fear of choking while eating and drinking. If a patient with cough reports swallowing problems, further evaluation for oral-pharyngeal dysphagia is indicated. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
2b
Further evaluation, including a chest radiograph and a nutritional assessment, should be considered in patients with cough or conditions associated with aspiration. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
3
Patients with oral-pharyngeal dysphagia and cough should be referred, ideally to a speech-language pathologist (SLP), for an oral-pharyngeal swallow evaluation. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
4
Patients with cough related to pneumonia and bronchitis who have received medical diagnoses and conditions associated with aspiration (Table 1 in Smith Hammond and Goldstein21) should be referred, ideally to an SLP, for an oral-pharyngeal swallow evaluation. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
5
Patients with a reduced level of consciousness are at high risk for aspiration and should not be fed orally until the level of consciousness has improved. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
6
Alert patients with cough who are in high-risk groups for aspiration (Table 1 in Smith Hammond and Goldstein21) should be observed drinking small amounts of water (3 oz). If the patient coughs or shows clinical signs that are associated with aspiration (Tables 2, 3 in Smith Hammond and Goldstein21), the patient should be referred for a detailed swallowing evaluation, preferably to an SLP. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
7
In patients with cough, the value of the subjective assessment of voluntary cough (VC) as the sole predictor of aspiration is uncertain because of poor reliability and an unclear association with evaluation. Level of evidence, low; benefit, conflicting; grade of evidence, I
-
8
The assessment of the reflexive cough response to inhaled irritants as a predictor of aspiration risk and subsequent pneumonia is not recommended due to a lack of adequate supportive studies. Level of evidence, low; benefit, conflicting; grade of evidence, I
-
9
In acute stroke patients, the expulsive phase rise time of VC may predict aspiration. The use of this test has not been validated in other patient groups, and further studies comparing the accuracy of objective measures of VC to the clinical swallow evaluation to identify aspiration risk are needed. Level of evidence, low; benefit, small; grade of recommendation, C
-
10
Patients with dysphagia should undergo videofluoroscopic swallow evaluation (VSE) or fiberoptic endoscopic evaluation of swallowing (FEES) to identify appropriate treatment. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
11
Patients with dysphagia should be managed by organized multidisciplinary teams that may include a physician, a nurse, an SLP, a dietitian, and physical and occupational therapists. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
12
In patients with dysphagia, VSE or FEES can be useful for determining compensatory strategies enabling patients with dysphagia to safely swallow. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
13
In patients with dysphagia, dietary recommendations should be prescribed when indicated, and can be refined by testing with foods and liquids simulating those in a normal diet during the VSE or FEES. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
14
For patients with muscular weakness during swallowing, muscle strength training, with or without electromyographic biofeedback, and electrical stimulation treatment of the swallowing musculature are promising techniques but cannot be recommended at this time until further work in larger populations is performed. Level of evidence, low; benefit, conflicting; grade of evidence, I
-
15
Patients with intractable aspiration may be considered for surgical intervention. Level of evidence, low; benefit, substantial; grade of recommendation, B
Angiotensin-Converting Enzyme Inhibitor-Induced Cough22
In patients presenting with chronic cough, in order to determine that the angiotensin-converting enzyme (ACE) inhibitor is the cause of the cough, therapy with ACE inhibitors should be discontinued regardless of the temporal relation between the onset of cough and the initiation of ACE inhibitor therapy. The diagnosis is confirmed by the resolution of cough, usually within 1 to 4 weeks of the cessation of the offending agent; however, the resolution of cough may be delayed in a subgroup of patients for up to 3 months. Quality of evidence, low; net benefit, substantial; grade of recommendation, B
In patients presenting with chronic ACE inhibitor-induced cough, discontinue therapy with the drug because it is the only uniformly effective treatment. Quality of evidence, low; net benefit, substantial; grade of recommendation, B
In patients whose cough resolves after the cessation of therapy with ACE inhibitors, and for whom there is a compelling reason to treat with these agents, a repeat trial of ACE inhibitor therapy may be attempted. Quality of evidence, fair; net benefit, substantial; grade of recommendation, A
In patients for whom the cessation of ACE inhibitor therapy is not an option, pharmacologic therapy, including that with sodium cromoglycate, theophylline, sulindac, indomethacin, amlodipine, nifedipine, ferrous sulfate, and picotamide that is aimed at suppressing cough should be attempted. Quality of evidence, fair; net benefit, intermediate; grade of recommendation, B
In patients in whom persistent or intolerable ACE inhibitor-induced cough occurs, therapy should be switched, when indicated, to an angiotensin receptor blocker, with which the incidence of associated cough appears to be similar to that for the control drug, or to an appropriate agent of another drug class. Quality of evidence, good; net benefit, substantial; grade of recommendation, A
Habit Cough, Tic Cough, and Psychogenic Cough in Adult and Pediatric Populations23
-
1a
In adult patients with chronic cough, the diagnoses of habit cough or psychogenic cough can only be made after an extensive evaluation has been performed that includes ruling out tic disorders and uncommon causes (as described in the section “Uncommon Causes of Cough”), and cough improves with specific therapy such as behavior modification or psychiatric therapy. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
-
1b
In adult patients with chronic cough that remains persistently troublesome despite an extensive and thorough evidence-based evaluation, and after behavior modification and/or psychiatric therapy have failed, unexplained cough should be diagnosed rather than a habit cough or psychogenic cough. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
-
1c
In children with chronic cough, the diagnoses of habit cough or psychogenic cough can only be made after tic disorders and Tourette syndrome have been evaluated and cough improves with specific therapy such as behavior modification or psychiatric therapy. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
-
2
In adult patients with cough, the diagnosis of habit cough should not be made unless biological and genetic tic disorders associated with coughing such as Tourette syndrome have been ruled out. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
-
3
In adults with chronic cough, the presence or absence of nighttime cough or cough with a barking or honking character should not be used to diagnose or exclude a diagnosis of psychogenic cough. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
4
In children with chronic cough, the characteristics of the cough may be suggestive of, but are not diagnostic of, psychogenic cough. The presence or absence of nighttime cough should not be used to diagnose or exclude psychogenic cough. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
-
5
In adult and pediatric patients with chronic unexplained cough, common psychosocial problems such as anxiety, depression, domestic violence, and child abuse/neglect that are often associated with somatization disorders should be evaluated. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
-
6
In adult and pediatric patients with chronic cough associated with troublesome psychological manifestations, psychological counseling or psychiatric intervention should be encouraged, after other causes have been ruled out. Level of evidence, expert opinion; benefit, small/weak; grade of recommendation, E/C
Chronic Cough Due to Chronic Interstitial Pulmonary Diseases24
In patients with chronic cough, before diagnosing interstitial lung disease (ILD) as the sole cause, common etiologies such as UACS, which was previously referred to as PNDS, asthma, and GERD should be considered. As these common causes may also share clinical features with specific ILDs, a diagnosis of ILD as the cause of cough should be considered a diagnosis of exclusion. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In patients with cough secondary to an ILD, because of the prognostic implications, primary treatment should be dictated by the specific disorder. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with cough secondary to idiopathic pulmonary fibrosis, corticosteroids may lead to symptomatic improvement; however, as they have been shown to neither prolong survival nor improve quality of life and may be associated with significant side effects, their use requires an individualized analysis of the overall benefits and risks. Level of evidence, expert opinion; benefit, intermediate; grade of recommendation, E/B
In patients with cough and characteristic clinical and radiographic features, sarcoidosis should be considered as a cause. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In patients with cough secondary to sarcoidosis, although therapy with oral corticosteroids may lead to symptomatic improvement, as they have not been proven to have a durable benefit and are associated with significant side effects, an individualized analysis of the overall benefit and risk is necessary. Level of evidence, fair; benefit, intermediate; grade of recommendation, B
In patients with cough secondary to sarcoidosis, therapy with oral corticosteroids followed by ICSs may improve symptoms. Level of evidence, fair; benefit, conflicting; grade of recommendation, I
In patients with cough, ILD, and a concerning environmental, occupational, or avocational exposure, hypersensitivity pneumonitis should be considered as a potential cause. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In patients with cough due to hypersensitivity pneumonitis, treatment should include the removal of the offending exposure and systemic corticosteroid therapy in those with evidence of physiologic impairment. Level of evidence, low; benefit, substantial; grade of recommendation, B
Cough: Occupational and Environmental Considerations25
In every patient with cough, when taking a medical history, ask about occupational and environmental causes. Level of evidence, expert opinion; benefit, substantial; grade of recommendations, E/A
In every patient with cough who has potentially significant exposures to suspicious environmental or occupational causes, determine the relationship of these occupational and environmental factors to confirm or refute their role in cough and to modify or eliminate exposure to the relevant agents. Level of evidence, expert opinion; benefit, substantial; grade of recommendations, E/A
Because outdoor environmental pollution and occupational exposures can be important factors in causing cough, physicians should play a role in developing and supporting enforceable standards for safe workplace and outdoor air pollution exposure limits. Level of evidence, expert opinion; benefit, substantial; grade of recommendations, E/A
In patients with a high suspicion of cough due to environmental or occupational exposures, consider referring the patient to a specialist in this area or consult evidence-based guidelines. Level of evidence, expert opinion; net benefit, substantial; grade of recommendation, E/A
Chronic Cough Due to Tuberculosis and Other Infections26
In areas where there is a high prevalence of TB, chronic cough should be defined as it is in the World Health Organization Practical Approach to Lung Health program as being 2 to 3 weeks in duration. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with chronic cough who live in areas with a high prevalence of TB, this diagnosis should be considered, but not to the exclusion of the more common etiologies. Sputum smears and cultures for acid-fast bacilli and a chest radiograph should be obtained whenever possible. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with suspected TB, future investigations are needed to refine the criteria for suspecting TB and initiating a diagnostic evaluation, to utilize resources in a cost-effective manner and to improve patient and caregiver adherence to diagnostic recommendations. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In populations at increased risk of becoming infected with TB and transmitting it to others by cough (eg, those persons in prisons and nursing homes), special measures to prevent outbreaks must be made by public health agencies to screen for new cases, maintain surveillance of existing populations, and establish effective diagnostic and treatment programs early in the evaluation. Level of evidence, good; benefit, substantial; grade of recommendation, A
In patients with unexplained chronic cough who have resided in areas of endemic infection with fungi or parasites, a diagnostic evaluation for these pathogens should be undertaken when more common causes of cough have been ruled out. Level of evidence, low; benefit, substantial; grade of recommendation, B
Peritoneal Dialysis and Cough27
In patients receiving long-term peritoneal dialysis with cough, evaluate the patient for the potential causes with increased prevalence in this population such as GERD, ACE inhibitors, pulmonary edema, asthma that may be exacerbated by β-adrenergic-blocking medications, and infection. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
Cough in the Immunocompromised Host28
In patients with immune deficiency, the initial diagnostic algorithm for patients with acute, subacute, and chronic cough is the same as that for immunocompetent persons, taking into account an expanded list of differential diagnoses that considers the type and severity of immune defect and geographic factors. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In HIV-infected patients, CD4+ lymphocyte counts should be used in constructing the list of differential diagnostic possibilities potentially causing cough. Level of evidence, low; benefit, substantial; grade of recommendation, B
HIV-infected patients with CD4+ lymphocyte counts of < 200 cells/μL or those patients with counts of > 200 cells/μL with unexplained fever, weight loss, or thrush who have unexplained cough should be suspected of having Pneumocystis pneumonia, tuberculosis, and other opportunistic infections, and should be evaluated accordingly. Level of evidence, low; benefit, substantial; grade of recommendation, B
Uncommon Causes of Cough29
In patients with chronic cough, uncommon causes should be considered when cough persists after evaluation for common causes and when the diagnostic evaluation suggests that an uncommon cause, pulmonary as well as extrapulmonary (see Table 1 in section 28), may be contributing. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with chronic cough, until uncommon causes that potentially may be contributing to the patient’s cough have been ruled out, the diagnosis of unexplained cough should not be made. Level of evidence, low; benefit, substantial; grade of recommendation, B
If cough persists after consideration of the most common causes, perform a chest CT scan and, if necessary, a bronchoscopic evaluation. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients who present with abrupt onset of cough, consider the possibility of an airway foreign body. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with unexplained cough, evaluate the possibility of drug-induced cough. Level of evidence, low; benefit, substantial; grade of recommendation, B
In patients with unexplained cough, consider a therapeutic trial of withdrawing the drug that is suspected to cause the cough. Level of evidence, low; benefit, substantial; grade of recommendation, B
Unexplained (Idiopathic) Cough30
The diagnosis of unexplained (idiopathic) cough is a diagnosis of exclusion. It should not be made until a thorough diagnostic evaluation is performed, specific and appropriate treatment (according to the management protocols that have performed the best in the literature) has been tried and has failed, and uncommon causes have been ruled out. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
An Empiric Integrative Approach to the Management of Cough3
-
1
In patients with cough, the starting point is the medical history and physical examination. Although the timing and characteristics of the cough are of little diagnostic value, the medical history is important to determine whether the patient is receiving an ACE inhibitor, is a smoker, or has evidence of a serious life-threatening or systemic disease. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
-
2
In patients with an acute cough, first determine whether the acute cough is a reflection of a serious illness such as pneumonia or pulmonary embolism, or, as is usually the case, a manifestation of a non-life-threatening disease such as a respiratory tract infection (eg, common cold or lower respiratory tract infection), an exacerbation of a preexisting condition (eg, COPD, UACS, asthma, or bronchiectasis), or an environmental or occupational exposure to some noxious or irritating agent (eg, allergic or irritant-induced rhinitis). Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
-
3
In patients with a subacute cough, first determine whether it is a postinfectious cough or not. If it is postinfectious, determine whether it is a result of UACS, transient bronchial hyperresponsiveness, asthma, pertussis, or an acute exacerbation of chronic bronchitis. If it is noninfectious, manage the cough the same way as chronic cough. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
-
4a
In patients with chronic cough, systematically direct empiric treatment at the most common causes of cough (ie, UACS, asthma, NAEB, and GERD). Level of evidence, low; benefit, substantial; grade of recommendation, B
-
4b
In patients with chronic cough, therapy should be given in sequential and additive steps because more than one cause of cough may be present. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
5
Patients with a chronic cough who smoke should be counseled and assisted with smoking cessation. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
6
In a patient with cough who is receiving an ACE inhibitor, therapy with the drug should be stopped and the drug should be replaced. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
7
In patients with chronic cough, initial empiric treatment should begin with an oral first-generation A/D. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
8a
In patients whose chronic cough persists after treatment for UACS, the possibility that asthma is the cause of cough should be worked up next. The medical history is sometimes suggestive, but is not reliable in either ruling in or ruling out asthma. Therefore, ideally, broncho-provocation challenge (BPC), if spirometry does not indicate reversible airflow obstruction, should be performed in the evaluation for asthma as a cause of cough. In the absence of the availability of BPC, an empiric trial of antiasthma therapy should be administered (see section on the treatment of asthma in this guideline). Level of evidence, low; benefit, substantial; grade of recommendation, B
-
8b
In patients with chronic cough, in whom the diagnoses of UACS and asthma have been eliminated or treated without the elimination of cough, NAEB should be considered next with a properly performed induced sputum test for eosinophils. If a properly performed induced sputum test to determine whether eosinophilic bronchitis is present cannot be performed, an empiric trial of corticosteroids should be the next step. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
9
In the majority of patients with suspected cough due to asthma, ideally, before starting an oral corticosteroid regimen, a BPC should be performed and, if the result is positive, some combination therapy of ICSs, inhaled β-agonists, or oral leukotriene inhibitors should be administered. A limited trial of oral corticosteroids, however, should be administered in some patients who are suspected of having asthma-induced cough before eliminating the diagnosis from further consideration. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
10
In patients whose cough responds only partially or not at all to interventions for UACS and asthma or NAEB, treatment for GERD should be instituted next. Level of evidence, low; benefit, substantial; grade of recommendation, B
-
11
In patients with cough whose condition remains undiagnosed after all of the above has been done, referral to a cough specialist is indicated. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
Assessing Cough Severity and Efficacy of Therapy in Clinical Research31
In patients with chronic cough, to optimally evaluate the efficacy of cough-modifying agents, investigators should use both subjective and objective methods because they have the potential to measure different things. A patient’s subjective response is likely to be the only one that measures the impact of the intensity of cough. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In patients with chronic cough, with respect to subjective methods, it is recommended that a valid and reliable cough-specific health-related quality-of-life instrument be utilized. Level of evidence, fair; benefit, substantial; grade of recommendation, A
When assessing patients with chronic cough, even though visual analog scales have not been psychometrically tested, they are recommended because they are commonly used and valid, and they are likely to yield different but complementary results to cough-specific health-related quality-of-life instruments. Level of evidence, low; benefit, intermediate; grade of recommendation, C
When assessing patients with chronic cough, because health-related quality-of-life instruments have been psychometrically tested and visual analog scales have not, the cough-specific health-related quality-of-life instruments are recommended as the primary subjective outcome measure. Level of evidence, fair; benefit, intermediate; grade of recommendation, B
In patients with chronic cough, with respect to objective methods, tussigenic challenges should be used before and after the intervention to assess the effect of therapy on cough sensitivity only in disease states in which cough reflex sensitivity is known to be heightened. Level of evidence, low; benefit, small/weak; grade of recommendation, C
In patients with chronic cough, because the act of coughing has the potential to traumatize the upper airway (eg, the vocal cords), assessing the presence of upper airway edema before and after therapy with flow-volume loops is useful. Level of evidence, low; benefit, intermediate; grade of recommendation, C
In patients undergoing treatment for chronic cough, cough counting over 24 h is recommended with a computerized methodology that is reliable and accurate, noninvasive and portable, and easy to use in unattended, ambulatory, real-life settings within a patient’s home environment. Level of evidence, low; benefit, intermediate; grade of recommendation, C
Cough Suppressant and Pharmacologic Protussive Therapy32
In patients with chronic bronchitis, agents that have been shown to alter mucus characteristics are not recommended for cough suppression. Level of evidence, good; benefit, none; grade of recommendation, D
In patients with cough due to upper respiratory infection (URI) or chronic bronchitis, the only inhaled anticholinergic agent that is recommended for cough suppression is ipratropium bromide. Level of evidence, fair; benefit, substantial; grade of recommendation, A
In patients with chronic or acute bronchitis, peripheral cough suppressants, such as levodropropizine and moguisteine, are recommended for the short-term symptomatic relief of coughing. Level of evidence, good; benefit, substantial; grade of recommendation, A
In patients with cough due to URI, peripheral cough suppressants have limited efficacy and are not recommended for this use. Level of evidence, good; benefit, none; grade of recommendation, D
In patients with chronic bronchitis, central cough suppressants, such as codeine and dextromethorphan, are recommended for the short-term symptomatic relief of coughing. Level of evidence, fair; benefit, intermediate; grade of recommendation, B
In patients with cough due to URI, central cough suppressants have limited efficacy for symptomatic relief and are not recommended for this use. Level of evidence, good; benefit, none; grade of recommendation, D
In patients with chronic or acute cough requiring symptomatic relief, drugs that affect the efferent limb of the cough reflex are not recommended. Level of evidence, low; benefit, none; grade of recommendation, D
In patients requiring intubation during general anesthesia, the use of neuromuscular blocking agents is recommended to suppress coughing. Level of evidence, good; benefit, substantial; grade of recommendation, A
In patients with acute cough due to the common cold, preparations containing zinc are not recommended. Level of evidence, good; benefit, none; grade of recommendation, D
In patients with acute cough due to the common cold, over the counter combination cold medications, with the exception of an older antihistamine-decongestant, are not recommended until randomized controlled trials prove they are effective cough suppressants. Level of evidence, fair; benefit, none; grade of recommendation, D
In patients with acute or chronic cough not due to asthma, albuterol is not recommended. Level of evidence, good; benefit, none; grade of recommendation, D
In patients with neuromuscular impairment, protussive pharmacologic agents are ineffective and should not be prescribed. Level of evidence, good; benefit, none; grade of recommendation, D
In patients with bronchitis, hypertonic saline solution and erdosteine are recommended on a short-term basis to increase cough clearance. Level of evidence, good; benefit, substantial; grade of recommendation, A
In adult patients with CF, amiloride is recommended to increase cough clearance. Level of evidence, good; benefit, substantial; grade of recommendation, A
In adult patients with CF, while recombinant DNase does improve spirometry it is not recommended to increase cough clearance. Level of evidence, good; benefit, none; grade of recommendation, D
Nonpharmacologic Airway Clearance Therapies33
In patients with CF, chest physiotherapy is recommended as an effective technique to increase mucus clearance, but the effects of each treatment are relatively modest and the long-term benefits unproven. Level of evidence, fair; benefit, small; grade of recommendation, C
In patients with expiratory muscle weakness, manually assisted cough should be considered to reduce the incidence of respiratory complications. Level of evidence, low; benefit, small; grade of recommendation, C
In persons with airflow obstruction caused by disorders like COPD, manually assisted cough may be detrimental and should not be used. Level of evidence, low; benefit, negative; grade of recommendation, D
In patients with COPD and CF, huffing should be taught as an adjunct to other methods of sputum clearance. Level of evidence, low; benefit, small; grade of recommendation, C
In patients with CF, autogenic drainage should be taught as an adjunct to postural drainage as a method to clear sputum because it has the advantage of being performed without assistance and in one position. Level of evidence, low; benefit, small; grade of recommendation, C
In patients with neuromuscular weakness and impaired cough, expiratory muscle training is recommended to improve peak expiratory pressure, which may have a beneficial effect on cough. Level of evidence, expert opinion; benefit, small; grade of recommendation, E/C
In patients with CF, positive expiratory pressure is recommended over conventional chest physiotherapy because it is approximately as effective as chest physiotherapy, and is inexpensive, safe, and can be self-administered. Level of evidence, fair; benefit, intermediate; grade of recommendation, B
In patients with CF, devices designed to oscillate gas in the airway, either directly or by compressing the chest wall, can be considered as an alternative to chest physiotherapy. Level of evidence, low; benefit, conflicting; grade of recommendation, I
In patients with neuromuscular disease with impaired cough, mechanical cough assist devices are recommended to prevent respiratory complications. Level of evidence, low; benefit, intermediate; grade of recommendation, C
The effect of nonpharmacologic airway clearance techniques on long-term outcomes such as health-related quality of life and rates of exacerbations, hospitalizations, and mortality is not known at this time. The committee recommends that future investigations measure these outcomes in patients with CF, and in other populations with bronchiectasis, COPD, and neuromuscular diseases. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
Guidelines for Evaluating Cough in Pediatrics4
Children with chronic cough require careful and systematic evaluation for the presence of specific diagnostic indicators. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
Children with chronic cough should undergo, as a minimum, a chest radiograph and spirometry (if age appropriate). Level of evidence, expert opinion; benefit, intermediate; grade of recommendation, E/B
In children with specific cough, further investigations may be warranted, except when asthma is the etiologic factor. Level of evidence, expert opinion; benefit, intermediate; grade of recommendation, E/B
Children with chronic productive purulent cough should always be investigated to document the presence or absence of bronchiectasis and to identify underlying and treatable causes such as cystic fibrosis and immune deficiency. Level of evidence, low; benefit, substantial; grade of recommendation, B
In children with chronic cough, the etiology should be defined and treatment should be etiologically based. Level of evidence, expert opinion; benefit, substantial; grade of recommendation, E/A
In children with nonspecific cough, cough may spontaneously resolve, but children should be reevaluated for the emergence of specific etiologic pointers (see Table 1 in Chang and Glomb4). Level of evidence, low; benefit, substantial; grade of recommendation, B
In children with nonspecific cough and risk factors for asthma, a short trial (ie, 2 to 4 weeks) of beclomethasone, 400 μg/d, or the equivalent dosage with budesonide may be warranted. However, most children with nonspecific cough do not have asthma. In any case, these children should always be reevaluated in 2 to 4 weeks. Level of evidence, fair; benefit, intermediate; grade of recommendation, B
In children who have started therapy with a medication, if the cough does not resolve during the medication trial within the expected response time, the medication should be withdrawn and other diagnoses considered. Level of evidence, low; benefit, intermediate; grade of recommendation, C
In children with cough, cough suppressants and other over-the-counter cough medicines should not be used as patients, especially young children, may experience significant morbidity and mortality. Level of evidence, good; benefit, none; grade of recommendation, D
In children with nonspecific cough, parental expectations should be determined, and the specific concerns of the parents should be sought and addressed. Level of evidence, low; benefit, intermediate; grade of recommendation, E/B
In all children with cough, exacerbating factors such as exposure to tobacco smoke should be determined and interventional options for the cessation of exposure advised or initiated. Level of evidence, low; benefit, substantial; grade of recommendation, B
Children should be managed according to the studies and guidelines for children (when available), because etiologic factors and treatments in children are sometimes different from those in adults. Level of evidence, low; benefit, substantial; grade of recommendation, B
In children ≤ 14 years of age with chronic cough, when pediatric-specific cough recommendations are unavailable, adult recommendations should be used with caution. Level of evidence, expert opinion; benefit, intermediate; grade of recommendation, E/B
Potential Future Therapies for the Management of Cough34
Currently available cough-suppressant therapy is severely limited by a dearth of effective agents and their unacceptable side affects. Several classes of pharmacologic agents are currently under investigation in an attempt to develop clinically useful cough suppression.
Future Directions in the Clinical Management of Cough35
As suggested in the various sections of this guideline, further research should be conducted to elucidate the mechanisms of the production of cough in various diseases and conditions, the optimal methods of assessment, and treatment, specific to the suspected cause. Level of evidence, expert opinion; benefit, substantial; strength of recommendation, E/A
Research is particularly needed in areas such as the treatment of postinfectious cough, the characterization of psychogenic cough, the methods of assessment of cough, and pharmacotherapy. Level of evidence, expert opinion; benefit, substantial; strength of recommendation, E/A
Figure 2.
Subacute cough algorithm for the management of patients ≥ 15 years of age with cough lasting 3 to 8 weeks. For diagnosis and treatment recommendations refer to the section indicated in the algorithm. AECB = acute exacerbation of chronic bronchitis. See the legend of Figure 1 for abbreviations not used in the text. See Figure 1 for references to Sections.
Acknowledgments
This clinical practice guideline received the endorsements of the ATS and the CTS.
Abbreviations
- ACE
angiotensin-converting enzyme
- ACP
American College of Physicians
- A/D
antihistamine/decongestant
- ATS
American Thoracic Society
- BPC
bronchoprovocation challenge
- CTS
Canadian Thoracic Society
- DPB
diffuse panbronchiolitis
- dTap
acellular pertussis
- FEES
fiberoptic endoscopic evaluation of swallowing
- GERD
gastroesophageal reflux disease
- HRCT
high-resolution CT
- HSP
Health and Science Policy Committee
- IBD
inflammatory bowel disease
- ICS
inhaled corticosteroid
- ILD
interstitial lung disease
- NAEB
nonasthmatic eosinophilic bronchitis
- NSCLC
non-small cell lung cancer
- SLP
speech-language pathologist
- TB
tuberculosis
- UACS
upper airway cough syndrome
- URI
upper respiratory infection
- VC
voluntary cough
- VSE
videofluoroscopic swallow evaluation
References
- 1.Irwin RS, Boulet LP, Cloutier MM, et al. Managing cough as a defense mechanism and as a symptom: a consensus panel report of the American College of Chest Physicians. Chest. 1998;114(suppl):133S–181S. doi: 10.1378/chest.114.2_supplement.133s. [DOI] [PubMed] [Google Scholar]
- 2.Rudolph C, Mazur L, Liptak G, et al. Guidelines for evaluation and treatment of gastroesophageal reflux in infants and children: recommendations of the North American Society for Pediatric Gastroenterology and Nutrition. J Pediatr Gastroenterol Nutr. 2001;32(suppl):S1–S31. doi: 10.1097/00005176-200100002-00001. [DOI] [PubMed] [Google Scholar]
- 3.Pratter MR, Brightling CE, Boulet LP, et al. An empiric integrative approach to the management of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):222S–231S. doi: 10.1378/chest.129.1_suppl.222S. [DOI] [PubMed] [Google Scholar]
- 4.Chang AB, Glomb WB. Guidelines for evaluating cough in pediatrics: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):260S–283S. doi: 10.1378/chest.129.1_suppl.260S. [DOI] [PubMed] [Google Scholar]
- 5.McCrory DC, Zelman Lewis S. Methodology and grading of the evidence for the diagnosis and management of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):28S–32S. doi: 10.1378/chest.129.1_suppl.28S. [DOI] [PubMed] [Google Scholar]
- 6.Canning BJ. Anatomy and neurophysiology of the cough reflex: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):33S–47S. doi: 10.1378/chest.129.1_suppl.33S. [DOI] [PubMed] [Google Scholar]
- 7.McCool FD. Global physiology and pathophysiology of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):48S–53S. doi: 10.1378/chest.129.1_suppl.48S. [DOI] [PubMed] [Google Scholar]
- 8.Irwin RS. Complications of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):54S–58S. doi: 10.1378/chest.129.1_suppl.54S. [DOI] [PubMed] [Google Scholar]
- 9.Pratter MR. Overview of common causes of chronic cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):59S–62S. doi: 10.1378/chest.129.1_suppl.59S. [DOI] [PubMed] [Google Scholar]
- 10.Pratter MR. Chronic upper airway cough syndrome secondary to rhinosinus diseases (previously referred to as postnasal drip syndrome): ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):63S–71S. doi: 10.1378/chest.129.1_suppl.63S. [DOI] [PubMed] [Google Scholar]
- 11.Pratter MR. Cough and the common cold: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):72S–74S. doi: 10.1378/chest.129.1_suppl.72S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dicpinigaitis PV. Chronic cough due to asthma: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):75S–79S. doi: 10.1378/chest.129.1_suppl.75S. [DOI] [PubMed] [Google Scholar]
- 13.Irwin RS. Chronic cough due to gastroesophageal reflux disease: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):80S–94S. doi: 10.1378/chest.129.1_suppl.80S. [DOI] [PubMed] [Google Scholar]
- 14.Braman SS. Chronic cough due to acute bronchitis: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):95S–103S. doi: 10.1378/chest.129.1_suppl.95S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Braman SS. Chronic cough due to chronic bronchitis: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):104S–115S. doi: 10.1378/chest.129.1_suppl.104S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brightling CE. Chronic cough due to nonasthmatic eosinophilic bronchitis: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):116S–121S. doi: 10.1378/chest.129.1_suppl.116S. [DOI] [PubMed] [Google Scholar]
- 17.Rosen MJ. Chronic cough due to bronchiectasis: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):122S–131S. doi: 10.1378/chest.129.1_suppl.122S. [DOI] [PubMed] [Google Scholar]
- 18.Brown KK. Chronic cough due to nonbronchiectatic suppurative airway disease (bronchiolitis): ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):132S–137S. doi: 10.1378/chest.129.1_suppl.132S. [DOI] [PubMed] [Google Scholar]
- 19.Braman SS. Postinfectious cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):138S–146S. doi: 10.1378/chest.129.1_suppl.138S. [DOI] [PubMed] [Google Scholar]
- 20.Kvale PA. Chronic cough due to lung tumors: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):147S–153S. doi: 10.1378/chest.129.1_suppl.147S. [DOI] [PubMed] [Google Scholar]
- 21.Smith Hammond CA, Goldstein LB. Cough and aspiration of food and liquids due to oral-pharyngeal dysphagia: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):154S–168S. doi: 10.1378/chest.129.1_suppl.154S. [DOI] [PubMed] [Google Scholar]
- 22.Dicpinigaitis PV. Angiotensin-converting enzyme inhibitor-induced cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):169S–173S. doi: 10.1378/chest.129.1_suppl.169S. [DOI] [PubMed] [Google Scholar]
- 23.Irwin RS, Glomb WB, Chang AB. Habit cough, tic cough, and psychogenic cough in adult and pediatric populations: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):174S–179S. doi: 10.1378/chest.129.1_suppl.174S. [DOI] [PubMed] [Google Scholar]
- 24.Brown KK. Chronic cough due to chronic interstitial pulmonary diseases: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):180S–185S. doi: 10.1378/chest.129.1_suppl.180S. [DOI] [PubMed] [Google Scholar]
- 25.Tarlo SM. Cough: occupational and environmental considerations: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):186S–196S. doi: 10.1378/chest.129.1_suppl.186S. [DOI] [PubMed] [Google Scholar]
- 26.Rosen MJ. Chronic cough due to tuberculosis and other infections: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):197S–201S. doi: 10.1378/chest.129.1_suppl.197S. [DOI] [PubMed] [Google Scholar]
- 27.Tarlo SM. Peritoneal dialysis and cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):202S–203S. doi: 10.1378/chest.129.1_suppl.202S. [DOI] [PubMed] [Google Scholar]
- 28.Rosen MJ. Cough in the immunocompromised host: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):204S–205S. doi: 10.1378/chest.129.1_suppl.204S. [DOI] [PubMed] [Google Scholar]
- 29.Prakash UBS. Uncommon causes of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):206S–219S. doi: 10.1378/chest.129.1_suppl.206S. [DOI] [PubMed] [Google Scholar]
- 30.Pratter MR. Unexplained (idiopathic) cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):220S–221S. doi: 10.1378/chest.129.1_suppl.220S. [DOI] [PubMed] [Google Scholar]
- 31.Irwin RS. Assessing cough severity and efficacy of therapy in clinical research: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):232S–237S. doi: 10.1378/chest.129.1_suppl.232S. [DOI] [PubMed] [Google Scholar]
- 32.Bolser DC. Cough suppressant and pharmacologic protussive therapy: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):238S–249S. doi: 10.1378/chest.129.1_suppl.238S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCool FD, Rosen MJ. Nonpharmacologic airway clearance therapies: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):250S–259S. doi: 10.1378/chest.129.1_suppl.250S. [DOI] [PubMed] [Google Scholar]
- 34.Dicpinigaitis PV. Potential future therapies for the management of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):284S–286S. doi: 10.1378/chest.129.1_suppl.284S. [DOI] [PubMed] [Google Scholar]
- 35.Boulet LP. Future directions in the clinical management of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):287S–292S. doi: 10.1378/chest.129.1_suppl.287S. [DOI] [PubMed] [Google Scholar]