Abstract
Tuberculous brain abscess and subdural empyema are extremely rare manifestations of central nervous system tuberculosis. Here, we report a case of an 11-year-old immunocompetent child who developed temporal lobe abscess and subdural empyema following chronic otitis media. A right temporal craniotomy was performed and the abscess was excised. The Ziehl Nielsen staining of the aspirated pus from the temporal lobe abscess yielded acid fast bacilli. Prompt administration of antituberculous treatment resulted in complete recovery of the child. Even though the subdural abscess was not drained, we presume that to be of tubercular aetiology. Ours is probably the first case of brain abscess and subdural empyema due to Mycobacterium tuberculosis reported in the same child. This case is being reported because of its rarity and to stress the importance of routine staining for tubercle bacilli in all cases of brain abscess, especially in endemic areas, as it is difficult to differentiate tuberculous from pyogenic abscess clinically as well as histopathologically.
Keywords: Tuberculous brain abscess, subdural empyema, Ziehl Nielsen staining
Introduction
Tuberculosis is still a major health problem in developing countries. With the advent of human immunodeficiency virus (HIV), there is resurgence of tuberculosis. Tuberculous brain abscess and subdural empyema are extremely rare forms of central nervous system (CNS) tuberculosis. A tubercular abscess is characterized by an encapsulated collection of pus containing viable tubercular bacilli without evidence of the classic tuberculoma. Subdural empyema or collection of pus in the subdural space is mostly pyogenic. We are reporting an uncommon case of temporal lobe abscess and subdural empyema following chronic suppurative otits media in an immunocompetent child in whom the aspirated pus from the abscess showed acid fast bacilli.
Case Report
An 11-year-old boy, otherwise healthy (height 136 cm, weight 33 kg), presented with fever and headache of 5 days duration. He had purulent discharge from the right ear for the last 6 months. There was no history of contact with active tuberculosis. He was fully immunized for age and the BCG scar was present. He was gaining weight normally and was free of any significant illness, except for the chronic otitis media.
On examination, the child was drowsy, but comprehending well and verbalizing normally. His BP was 130/90 mm of Hg. The fundus was normal and there were no focal motor/sensory deficits. He had neck stiffness, but Kerning's sign was negative. There was attico antral perforation with purulent discharge from the right ear (unsafe chronic suppurative otitis media). The purulent discharge did not grow any microorganisms on Gram stain or culture (staining for acid fast bacilli was not done at this time). Blood counts showed a polymorphonuclear leucocytosis with an ESR of 100 mm in the first hour. Mantoux test was negative. His liver function and renal function tests were within normal limits, HIV was negative and hepatitis B surface antigen was negative. A provisional diagnosis of pyogenic meningitis/brain abscess was made. Lumbar puncture yielded clear fluid with normal tension, with total cell count of 335/mm, polymorphs 65%, lymphocytes 35%, protein 23 mg% and sugar 50 mg%. The cerebrospinal fluid culture was sterile. Contrast-enhanced computerized tomography (CT) scan of the head showed subdural empyema of 5-mm thickness in the right parafalcine region and evidence of right-sided mastoiditis. The temporal abscess was not evident on CT scan.
The child was given injection ceftriaxone and other symptomatic and supportive measures. After 2 days, weakness of the left lower limb was noticed (power Grade 2) with mild weakness of the left upper limb (grade 4) and left-sided pyramidal signs. Magnetic resonance imaging (MRI) brain with gadolinium contrast showed a peripherally enhancing lesion with thin walls in the right temporal lobe measuring 28 mm x 17 mm x 17 mm with surrounding perilesional edema with restriction of diffusion and a peripherally enhancing multiloculated subdural empyema in the right parafalcine region with a maximum thickness of 9 mm and a smaller collection in the right temporo-occipital region and evidence of right mastoiditis [Figures 1 and 2]. Antibiotics were changed to ceftazidime, vancomycin and metrogyl and a neurosurgical opinion was sought. The surgeon deferred active surgical intervention as the child appeared to improve with antibiotics. He became afebrile after 5 days of treatment and the lower limb weakness improved. The child developed persistent headache and low-grade fever on the 10th day and became drowsy. MRI repeated on the same day showed increase in the size of the temporal lobe abscess (48 mm × 46 mm × 43 mm) with surrounding edema and mass effect compressing the right lateral ventricle. The subdural collection also increased in size (17 mm) with midline shift. An emergency craniotomy was performed and 25 ml of brownish pus was drained and the lateral wall of the abscess was resected and sent for histopathologic study, Gram stain, AFB stain and culture. Aspiration of the subural empyema was not attempted as it was on the medial aspect, and the neurosurgeon opined that it was difficult to approach.
Figure 1.
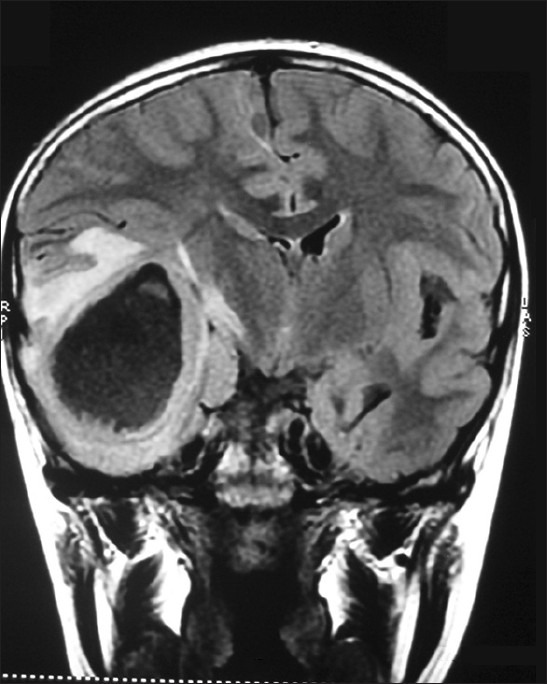
Magnetic resonance imaging brain – FLAIR (fluid attenuated inversion recovery) coronal showing abscess in the right temporal lobe with surrounding edema and squashing of the right lateral ventricle
Figure 2.
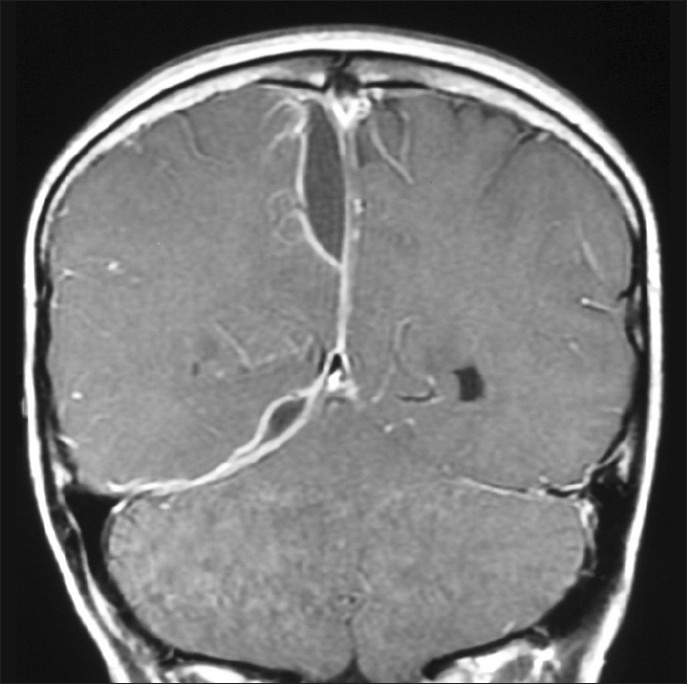
Magnetic resonance imaging brain – T1 coronal (postgadolinium contrast) showing right parafalcine subdural empyema
Gram stain did not show any organism and the bacterial culture was sterile. AFB staining showed 3+++ acid fast bacilli. The quantiferon gold test was found to be negative. The polymerase chain reaction for Mycobacterium tuberculosis could not be carried out due to technical reasons. Histopathology of the abscess wall showed granulation tissue formed by inflammatory cells, predominantly polymorphs with no evidence of granuloma.
The child was put on anti-tubercular treatment with 5 drugs (INH, rifampicin, ethambutol, pyrazinamide and streptomycin) along with steroids. Radical mastoidectomy was performed for the chronic mastoiditis, which showed partial erosion of stapedius. There was no pus and the ear was completely dry. The specimen was sent for AFB stain and culture, but did not show acid fast bacilli. On antituberculous treatment the patient became afebrile after 1 week and is without any neurologic deficits at present. MRI was repeated after 4 weeks, which showed a significant decrease in the size of the abscess [Figure 3]. The subdural abscess also became smaller, but was still visible on MRI [Figure 4].
Figure 3.
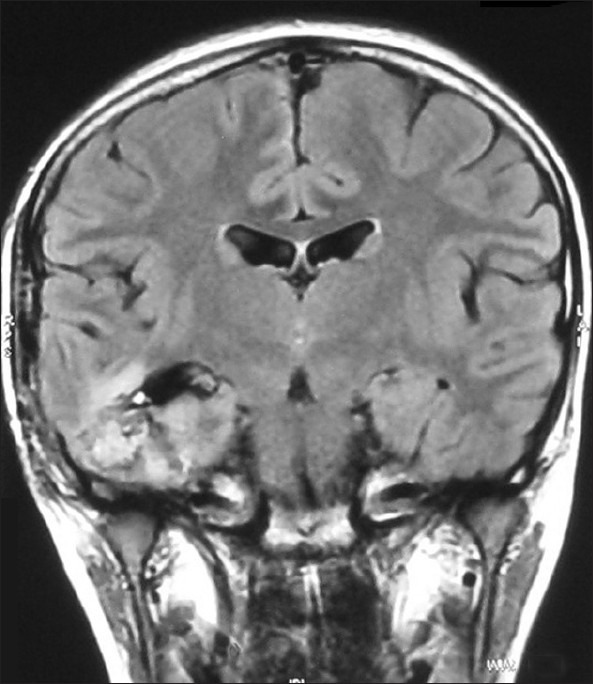
Repeat magnetic resonance imaging (1 month postoperative) FLAIR coronal showing significant reduction in the size of abscess
Figure 4.
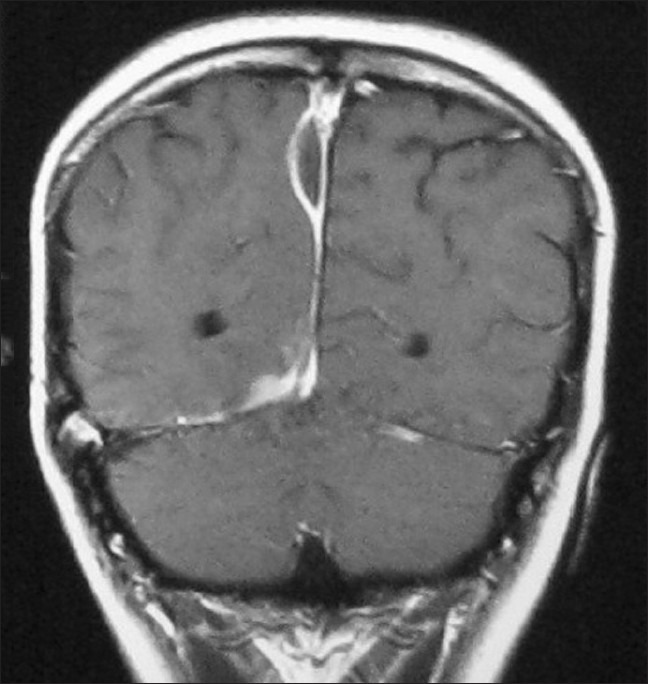
Repeat magnetic resonance imaging T1 coronal – postgadolinium contrast (after 1 month) showing reduction in size of the subdural empyema
Discussion
Although tuberculous meningitis and tuberculomas are frequent manifestations of CNS tuberculosis, the incidence of tuberculous brain abscess is rare. Most of the cases occur by hematogenous spread from extracranial locations; those that occur following otogenic infection involve the temporal lobe and cerebellum.[1] Intracranial subdural tubercular empyema is an extremely rare entity. The co-occurrence of tuberculous brain abscess and subdural empyema has not been reported previously in the literature. This case report highlights the importance of simple investigations like staining for acid fast bacilli in all cases of brain abscess. Although chronic otitis media is commonly seen in children, tuberculous brain abscess of otogenic origin is rare and is often misdiagnosed as pyogenic abscess.[2]
In the aetiologic analysis of 75 cases of brain abscess, tuberculous aetiology was found only in 4% of the cases.[3] Most of the tuberculous abscesses are hematogenous in origin, and spread of infection to the brain could occur due to active tuberculous infection elsewhere in the body.[1] HIV-infected patients and malnourished children are more prone to CNS tuberculosis and abscesses in particular. Our child was well nourished, HIV negative and did not have any evidence of immune deficiency.
A tuberculous abscess is characterized by an encapsulated collection of pus containing viable tubercular bacilli without evidence of the classic tubercular granuloma.[1] The differentiation of tuberculous brain abscess from pyogenic abscess can be difficult clinically and radiologically. It could mimic pyogenic abscess or glioma on imaging studies. The characteristics of the abscess wall on MR spectroscopy can be helpful. Tubercular cerebral abscesses show increased concentrations of lipids and phosphoserine.[4] MR spectroscopy was not done in this case due to technical reasons.
In his excellent review of the subject of tuberculous brain abscess, Whitner gives the following diagnostic criteria[5]:
True abscess formation within the brain substance characterized by cavity formation and central pus.
Vascular granulation tissue containing acute and chronic inflammatory cells, particularly polymorphs histologically.
Proof of tuberculous origin by either a positive pus culture for Mycobacterium tuberculosis or by demonstration of acid fast bacilli in the pus or abscess wall.
Tuberculomas of the brain show a typical granulomatous reaction, comprising of epithelioid cells and giant cells around a central area of necrosis. In contrast, a tubercular abscess shows only chronic, nonspecific inflammatory changes. A giant cell reaction and epithelioid cells are lacking.
A smear with Ziehl Nielsen stain, culture on LJ medium for acid fast bacilli and PCR for Mycobacterium tuberculosis should be carried out on pus from all brain abscesses. In our child, the culture did not yield positive results probably because of prior treatment with Vancomycin. The immunological tests like Mantoux and Quantiferon gold test came as negative probably because the Mycobacteriae were secluded within the thick abscess wall.
There are only two reports of subdural empyema due to tubercle bacilli reported in the pediatric population.[6,7] Subdural empyema is an extra axial collection of pus, often associated with pyogenic abscess. The contrast-enhanced imaging showed a multiloculated subdural empyema in the right parafalcine region and a smaller collection in the right temporo-occipital region in this case. As the subdural collection was not aspirated, we could not demonstrate acid fast bacilli from the lesion.
The surgical treatment of tuberculous brain abscess and subdural empyema needs individualization. Antitubercular therapy is the mainstay of treatment. Surgical evacuation is advocated depending on the size of the abscess and the neurological condition of the patient. Burr hole aspiration of the abscess is usually sufficient. Craniotomy is advisable in nonhealing and multilocular abscesses. In our case, craniotomy and excision of the abscess was performed; the aspiration of subdural empyema was not attempted as it was deep in the medial aspect of the cerebral hemisphere.
This case is reported because of its rarity and to highlight the importance of Ziehl Neilsen stain in all cases of brain abscess and subdural empyema, as the detection of tuberculous etiology might be life-saving to the child.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.Kumar R, Pandey CK, Bose N, Sahay S. Tuberculous brain abscess, clinical presentation, pathophysiology and treatment in children. Childs Nerv Syst. 2002;18:118–23. doi: 10.1007/s00381-002-0575-2. [DOI] [PubMed] [Google Scholar]
- 2.Muzumdar D, Balasubramaniam S, Melkundi S. Tuberculous otogenic brain abscess mimicking pyaemic abscess. Pediatr Neurosurg. 2009;45:220–4. doi: 10.1159/000224619. [DOI] [PubMed] [Google Scholar]
- 3.Menon S, Bharadwaj R, Chowdhary A, Kaundinya DV, Palande DA. Current epidemiology of intracranial abscesses: A prospective 5 year study. J Med Microbiol. 2008;57:1259–68. doi: 10.1099/jmm.0.47814-0. [DOI] [PubMed] [Google Scholar]
- 4.Luthra G, Parihar A, Nath K, Jaiswal S, Prasad KN, Husain N, et al. Comparative evaluation of bacterial, fungal and tubercular brain abscess by MR maging and MR spectroscopy. AJNR Am J Neuroradiol. 2007;28:1332–8. doi: 10.3174/ajnr.A0548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Whitner RD. Tuberculous brain abscess: Report of a case and review of literature. Arch Neurol. 1978;35:148–55. doi: 10.1001/archneur.1978.00500270030007. [DOI] [PubMed] [Google Scholar]
- 6.Banerjee AD, Pandey P, Ambekar S, Chandramouli BA. Pediatric intracranial subdural empyema caused by Mycobacterium tuberculosis: A case report and review of literature. Childs Nerv Syst. 2010;26:1117–20. doi: 10.1007/s00381-010-1157-3. [DOI] [PubMed] [Google Scholar]
- 7.Cayli SR, Onal C, Koçak A, Onmuş SH, Tekiner A. An unusual presentation of neurotuberculosis: Subdural empyema: Case report. J Neurosurg. 2001;94:988–91. doi: 10.3171/jns.2001.94.6.0988. [DOI] [PubMed] [Google Scholar]


