Abstract
Scrub typhus is a rickettsial disease caused by Orientia tsutsugamushi, one of the most common infectious diseases in the Asia-Pacific region. It has been reported from northern, eastern, and southern India, and its presence has been documented in at least 11 Indian states. However, scrub typhus meningoencephalitis has not been well documented in Kerala. We report two cases of scrub typhus meningoencephalitis from northern Kerala. The diagnosis was made based on the clinical pictures, presence of eschar, and a positive Weil–Felix test with a titer of > 1:320. The first patient succumbed to illness due to respiratory failure and the second patient improved well.
Keywords: Meningoencephalitis, rickettsia, scrub typhus
Introduction
Scrub typhus is an acute febrile illness caused by Orientia tsutsugamushi (rickettsia tsutsugamushi). Scrub typhus is a public health problem in Asia, where about 1 million new cases are identified annually and 1 billion people may be at risk of this disease. In India, the presence of scrub typhus and other rickettsial diseases has been known for several decades. During World War II, scrub typhus produced considerable morbidity and mortality among troops deployed in Southeast Asia.[1] However, there has been a considerable decline in the incidence of scrub typhus in the later decades. Recent reports from several parts of India, including South India, indicate that there is a resurgence of scrub typhus.[2–6] Scrub typhus is grossly underdiagnosed in India due to its nonspecific clinical presentation, limited awareness and low index of suspicion among clinicians, and lack of diagnostic facilities. O. tsutsugamushi is an obligatory intracellular Gram-negative coccobacillus. There are several serotypes of O. tsutsugamushi, and infections with one serotype gives only transient cross-immunity to another. It is a zoonotic disease transmitted by the larval mites (chiggers) of the Leptotrombidium deliense group. These larval mites usually feed on the wild rats of the subgenus Rattus. The infection is acquired through agricultural activities in the oil palm, rubber plantation, rice fields, and recreational activities in the woods or mountainous areas. The infection manifests clinically as a nonspecific febrile illness often accompanied by headache, myalgia, nausea, vomiting, diarrhea, cough, or breathlessness. The pathognomic clinical sign of scrub typhus is “eschar” (40–50%) which may be inconspicuous as it is often present in areas like groin, gluteal folds, breast folds, and external genitalia and may go unnoticed in dark-skinned people. Furthermore, the patients are usually unaware of the bite, as the eschar is painless and does not itch, and the bite may be in a location that is difficult to examine. Severity varies from subclinical illness to severe illness with multiple organ system involvement, which can be serious enough to be fatal, unless diagnosed early and treated.
Case Reports
Case 1
A 45-year-old farmer from north Kerala presented with high-grade fever associated with myalgia and headache and recurrent vomiting of 2-week duration. On examination, there was conjunctival congestion. There was no pallor, jaundice, lymphadenopathy, or edema. Vitals were stable except for sinus tachycardia, and respiratory and cardiovascular system examination was normal. The liver was palpable 2 cm below the right costal margin and the tip of the spleen was palpable. Neurologic examination showed mild neck stiffness with normal optic fundi. Investigations showed a total count of 8700 cell/mm3 with a polymorph predominant differential count, normal hemoglobin, and a platelet count of 78000/mm3 and an erythrocyte sedimentation rate (ESR) of 76 mm/h. Blood urea was 84 mg/dL and serum creatinine was 1.4 mg/dL. Total bilirubin was 0.8 mg/dL and direct 0.4 mg/dL, with albumin 2.8 gm/dL and total protein 6.8 g%. SGOT and SGPT were elevated (160 and 184 U/L, respectively) and serum ALP was 82 U/L. Serum electrolytes and urine routine were normal and the peripheral smear for the malarial parasite was negative. A lumbar puncture revealed opening pressure of 260 mmH2O and a mild lymphocytic pleocytosis (15 cells), high protein (60 mg), and normal glucose. With a 1-week history of high-grade fever, headache hepatosplenomegaly, and slightly elevated liver function test, the initial diagnosis was kept as enteric fever with meningism, but the elevated ESR and abnormal renal function test, thrombocytopenia, and the occupation of the patient were in favor of an equal possibility of leptospirosis even though prolonged fever was against it. Considering this, he was started on inj. ceftriaxone. It was continued for 48 h but fever persisted and headache increased in severity. An abdominal ultrasonogram (USG) showed hepatosplenomegaly only. Serologic tests were negative for hepatitis A, B, and E virus, HIV, dengue, and leptospirosis. The Widal agglutination test was also negative. Ceftriaxone was continued still keeping the possibility of enteric fever with meningism, but on the fourth day, the patient developed altered sensorium, agitated behavior, and recurrent seizure. His electroencephalography (EEG) showed moderate diffuse slowing of the background activity and computed tomography (CT) of the brain was normal. The patient developed respiratory distress on the seventh day of hospitalization. X-ray of the chest showed interstitial pneumonitis. As there was a recent increase in the incidence of scrub typhus in the medical ward, a possibility of rickettsial infection was suspected and he was searched for any eschar which was found on the groin [Figure 1]. Meanwhile, samples were sent for the Weil-Felix reaction, which turned out to be positive for the OXK antigen in titers of 1:5120 [Figure 2]. He was put on doxycycline and ceftriaxone was discontinued. His fever responded on the third day of starting doxycycline but the respiratory status worsened and he required ventilator support. He was also started on chloramphenicol but in spite of the best supportive care and broad-spectrum antibiotic coverage, the patient succumbed to his illness on the 12th day of hospitalization due to respiratory failure. The diagnosis was missed initially because of similarities of clinical features with those of typhoid fever and leptospirosis, which are much more common in north Kerala, and the limited awareness and low index of suspicion.
Figure 1.

Eschar on the groin
Figure 2.
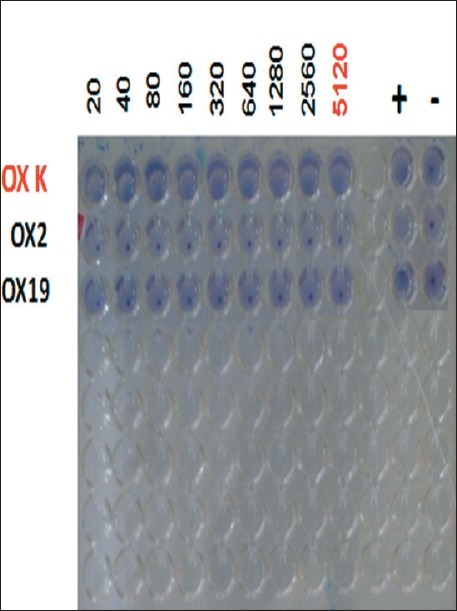
Weil–Felix reaction positivity for the OXK antigen in titers of 1:5120
Case 2
A 30-year-old house wife was admitted with 6 days of fever, headache, vomiting, and cough followed by 1 day of seizure. There was no history of insect bite or rash. Physical examination revealed tachycardia, tachypnea, and a typical eschar on the groin area and below the breast fold [Figure 3]. On neurologic examination, she was drowsy and ocular fundi were normal. The rest of the examination was normal. Investigations revealed a normal WBC count (9500/mm3), thrombocytopenia (72000/ mm3), low serum albumin (3 g%), and elevated liver enzymes (SGOT and SGPT, 176 and 122 IU/mL, respectively). The renal function test was normal. Serologic tests were negative for hepatitis A, B, and E virus, HIV, dengue, and leptospirosis. The Widal agglutination test was also negative. Peripheral smear, blood, and urine culture were normal. Cerebrospinal fluid examination revealed opening pressure of 270 mmH2O and lymphocytic pleocytosis (30 cells) with raised protein (70 mg) and normal glucose. CT of the brain was normal. Abdomen USG and chest X-ray were normal. EEG showed mild diffuse slowing of the background activity. Her Weil–Felix test was positive for the OXK antigen in titers of 1:320. She was started on doxycycline and became afebrile within 48 h.
Figure 3.
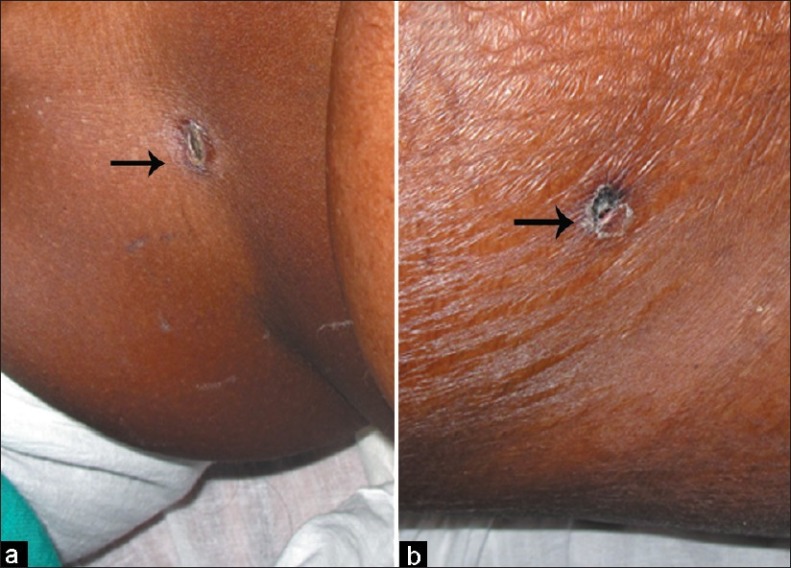
(a) Eschar below the breast fold (black arrow). (b) Eschar on the groin (black arrow)
Based on the clinical picture of fever with eschar, a dramatic therapeutic response to doxycycline and Weil–Felix test positivity, a final diagnosis of scrub typhus with meningoencephalitis was made.
Discussion
In Kerala, scrub typhus usually does not come out as a differential diagnosis of patients admitted with acute meningoencephalitis. This case reports shows that scrub typhus and other rickettsial infections are emerging threats in Kerala. This febrile illness affects previously healthy active persons and if undiagnosed or diagnosed late may prove to be life threatening as happened in our first case.
Recently, several reports of scrub typhus from various parts of India have been published.[1–5] Most cases of scrub typhus were diagnosed during the rainy months of June to November. However, Mathai et al. reported more cases in the cooler months in southern India.[2] This correlated with the months with a higher number of field rats infected with O. tsutsugamushi and the months with more mites attached to rodents.
In the coming years, scrub typhus may become a major public health problem in Kerala because of the recent increase in number of case reports from various part of Kerala (unpublished). The exact reason for recent outbreaks of scrub typhus in Kerala is not clear. In the last few years, there have been outbreaks of scrub typhus in many areas of south India especially Karnataka and Tamil Nadu.[7–9] So, Kerala being heavily dependent on neighboring states for food grains, fruits, and vegetables, there is an increased chance of transport of mites attached to rodents; moreover, there is a recent increase in tourism as well. It is still not known whether scrub typhus is a newcomer or it was previously undiagnosed because it is possible that it existed in this state but went unnoticed as physicians failed to recognize it. Many physicians might have been treating their patients with scrub typhus without considering it in their differential diagnoses as it responds to commonly used antibiotics like doxycycline and azithromycin.
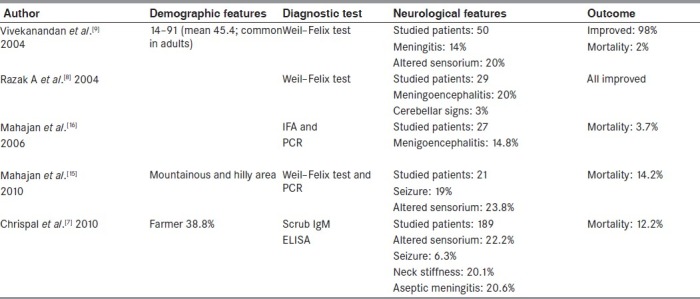
Central nervous system (CNS) involvement is a known complication of scrub typhus which ranges from aseptic meningitis to frank meningoencephalitis.[10] The name “typhus” itself, is derived from the Greek work, “typhos,” which means “stupor.” A recent case series of scrub typhus from Pondicherry reported meningitis as a common CNS complication.[9] Other neurological complications include seizures, delirium, and hearing loss. However, focal CNS damage was rare, and during the encephalitis stage, few complications like cerebellitis,[11] myelitis,[12] and cerebral hemorrhage[13] are reported. We reviewed recent major publications on typhus from India regarding the neurological manifestation [Table 1]. The neurological complications in scrub typhus are attributed to the involvement of the small vessels which occurs throughout the body. The greatest degree of CNS involvement in rickettsial diseases occurs in Rocky Mountain spotted fever and epidemic typhus, followed closely by scrub typhus.
Table 1.
Recent publications on scrub typhus from India
Although rickettsiae can be isolated from or detected in clinical specimens, serological tests still remain an indispensable tool in the diagnosis. Microimmunoflourescence is considered the test of choice. Latexagglutination, indirect hemagglutination, immunoperoxidase assay, ELISA, and polymerase chain reaction are other tests available. But these tests are not available commercially and their complexity limits their use to a small number of centers. The Weil–Felix test using the Proteus OXK strain is a commercially available serodiagnostic test and is in use for many years. A minimum positive titer is 1:80 or a fourfold rise over previous levels is significant. Several studies have shown that the Weil-Felix test has a high specificity. It was found that at a cut-off value of ≥1:320, OXK had a specificity of 97% but it was less sensitive.[9]
Early treatment shows better outcomes and faster resolution than delayed treatment. Tetracycline500 mg, qid, or doxycyclin 200 mg, od, for 7 days is the treatment of choice. Chloramphenicol 500 mg, qid, is an alternative. Rifampicin, 900 mg per day for a week, has been found effective in patients who respond poorly to conventional therapy. Azithromycin has been proven to be more effective than doxycyclin in doxycyclin-susceptible and doxycyclin-resistant strains causing scrub typhus.[14] Rapid defervescence after antibiotics is so characteristic that it is used as a diagnostic test for scrub typhus.
In summary, we describe the first case of scrub typhus meningoencephalitis from Kerala. Considering the recent increase in scrub typhus in Kerala and other states, a proportionate increase in the neurological complication has to be anticipated. In this context, we hope this report will make physicians aware of this entity which is probably more widespread than considered and emphasize the need for a high degree of clinical suspicion and familiarity with the various clinical manifestations in suspected cases to allow early diagnosis and treatment thereby reducing patient morbidity and mortality.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.Mahajan SK. Scrub Typhus. J Assoc Physicians India. 2005;53:954–8. [PubMed] [Google Scholar]
- 2.Chaudhry D, Garg A, Singh I, Tandon C, Saini R. Rickettsial diseases in Haryana: Not an uncommon entity. J Assoc Physicians India. 2009;57:334–7. [PubMed] [Google Scholar]
- 3.Mathai E, Rolain JM, Verghese GM, Abraham OC, Mathai D, Mathai M, et al. Outbreak of scrub typhus in southern India during the cooler months. Ann N Y Acad Sci. 2003;990:359–64. doi: 10.1111/j.1749-6632.2003.tb07391.x. [DOI] [PubMed] [Google Scholar]
- 4.Prabagaravarthanan R, Harish BN, Parija SC. Typhus fever in Pondicherry. J Commun Dis. 2008;40:159–60. [PubMed] [Google Scholar]
- 5.Ittyachen AM. Emerging infections in Kerala: A case of scrub typhus. Natl Med J India. 2009;22:333–4. [PubMed] [Google Scholar]
- 6.Isaac R, Varghese GM, Mathai E, J M, Joseph I. Scrub Typhus: Prevalence and diagnostic issues in rural Southern India. Clin Infect Dis. 2004;39:1395–6. doi: 10.1086/424748. [DOI] [PubMed] [Google Scholar]
- 7.Chrispal A, Boorugu H, Gopinath KG, Prakash JA, Chandy S, Abraham OC, et al. Scrub typhus: An unrecognized threat in South India - clinical profile and predictors of mortality. Trop Doct. 2010;40:129–33. doi: 10.1258/td.2010.090452. [DOI] [PubMed] [Google Scholar]
- 8.Razak A, Sathyanarayanan V, Prabhu M, Sangar M, Balasubramanian R. Scrub typhus in Southern India: Are we doing enough? Trop Doct. 2010;40:149–51. doi: 10.1258/td.2010.090508. [DOI] [PubMed] [Google Scholar]
- 9.Vivekanandan M, Mani A, Priya YS, Singh AP, Jayakumar S, Purty S. Outbreak of scrub typhus in Pondicherry. J Assoc Physicians India. 2010;58:24–8. [PubMed] [Google Scholar]
- 10.Drevets DA, Leenen PJ, Greenfield RA. Invasion of central nervous system by intracellular bacteria. Clin Microbiol Rev. 2004;17:323–47. doi: 10.1128/CMR.17.2.323-347.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Silpapojakul K, Ukkachoke C, Krisanapan S, Silpapojakul K. Rickettsial meningitis and encephalitis. Arch Intern Med. 1991;151:1753–7. [PubMed] [Google Scholar]
- 12.Kim DE, Lee SH, Park KI, Chang KH, Roh JK. Scrub typhus encephalomyelitis with prominent neurological signs. Arch Neurol. 2000;57:1770–2. doi: 10.1001/archneur.57.12.1770. [DOI] [PubMed] [Google Scholar]
- 13.Yang SH, Wang LS, Liang CC, Ho YH, Chang ET, Cheng CH. Scrub typhus complicated by intracranial hemorrhage - A Case report. Tzu Chi Med J. 2005;17:111–4. [Google Scholar]
- 14.Strickman D, Sheer T, Salata K, Hershey J, Dasch G, Kelly D, et al. in vitro effectiveness ofazithromycin against doxycyclin resistant and –susceptible strains of Rickttsia tsutsugamushi, etiologic agent of scrubtyphus. Antimicrob Agents Chemother. 1995;39:2406–10. doi: 10.1128/aac.39.11.2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mahajan SK, Rolain JM, Kanga A, Raoult D. Scrub typhus involving central nervous system, India, 2004-2006. Emerg Infect Dis. 2010;16:1641–3. doi: 10.3201/eid1610.100456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahajan SK, Rolain JM, Kashyap R, Bakshi D, Sharma V, Prasher BS, et al. Scrub typhus in Himalayas. Emerg Infect Dis. 2006;12:1590–2. doi: 10.3201/eid1210.051697. [DOI] [PMC free article] [PubMed] [Google Scholar]


