General introduction
Methodology of this review
We searched for references of published literature about Malawi through Pubmed and obtained full text papers from HINARI, Popline, EBSCO, journals' open access initiatives, local libraries, and - through the gratefully acknowledged help of Dr. Ian Holtby - libraries in the UK. Non peer-reviewed published documents were obtained from the documentation centres of the Ministry of Health, National AIDS Commission, College of Medicine and UN and through Popline. Local researchers were contacted to provide additional grey literature. The Cochrane library was used (through HINARI and the free WHO Reproductive Health Library) for information on the current state of effective interventions for HIV/AIDS.
We made extensive use of Yolande Coombes' review on sexual and reproductive health behaviour in Malawi that was used as input for the national BCI strategy for paragraph 3.2 (behavioural determinants) and 3.3 (structural determinants).1
Virological, immunological and pathogenic aspects of HIVb
Human Immunodeficiency Virus type 1 (HIV-1) is the virus responsible for the global HIV pandemic, whereas the less pathogenic HIV-2 is largely restricted to West Africa. Within the HIV-1 type, subtypes A, C and D are most common in Africa, with subtype C estimated to be responsible for 90% of infections in southern Africa. HIV primarily infects and destroys cells in the immune system, particularly CD4+ T-lymphocytes. The immune system is not able to eliminate the HIV virus, although it may control viral replication to some extent through humoral and cellular immune responses. Because it cannot remove the antigen, the immune system remains highly activated and in the process burns out and falls apart. This degeneration of the immune system over the years results in increased risk of opportunistic infections and malignancies and is the hallmark of Acquired Immune Deficiency Syndrome (AIDS). The rate at which the immune system is destroyed is directly related to the rate of viral replication.
During acute HIV infection, viral load is high because replication occurs in the absence of an immune response. CD4 count drops and about half of recently infected individuals will experience a non-specific viral illness, characterized by fever, sweats, malaise, myalgia, pharyngitis, gastrointestinal disturbance, headache, generalised lymphadenopathy and hepatosplenomegaly. Transmission risk is high during this period. After the immune response has developed, the viral load drops to a plateau and CD4 count increases (but not to pre-HIV levels) and then slowly declines over the years until it reaches such a low level that opportunistic infections and malignancies develop.
About 5–10% of people are rapid progressors, who develop AIDS within one to two years following HIV infection. This is associated with high levels of viral replication and a steep decline in CD4 count. Another 5–10% are able to control HIV very effectively. These long-term non-progressors, who sometimes have been infected for more than 20 years, have very low viral loads and competent immune systems. However, the majority of HIV infected people in developed countries, when not on antiretroviral therapy, progress from HIV infection to AIDS in 8–10 years. There is some evidence that poor socio-economic conditions, including malnutrition and limited access to health care, may contribute to a 1–2 year shorter latent period in developing countries.
The final progression to AIDS is characterised by very low CD4 counts and rising viral load, thus leading to increased transmission risk in this period. The stage of the immune function in HIV infected individuals can be clinically assessed, using the standardised criteria of the WHO Clinical Staging System (table 1).
Table 1.
World Health Organization clinical staging system
WHO Stage 1:
|
WHO Stage 2
|
WHO Stage 3
|
WHO Stage 4 (AIDS)
|
Diagnosis and monitoring of HIV2
Diagnosis
In most contexts, HIV infection is diagnosed by detecting antibodies against HIV, e.g. through enzyme-linked immunosorbent assay (ELISA), Western Blot or rapid test devices. However, antibodies against HIV only become detectable in blood from approximately 4 weeks after infection. Tests for the virus itself reveal infection earlier. The p24 antigen test, which targets one of HIV's core proteins, is positive in the majority of patients a week before an antibody ELISA test becomes reactive. Polymerase Chain Reaction (PCR) testing, which targets a portion of the HIV RNA or DNA, can detect HIV two weeks before ELISA and is best way at the moment to measure viral load. HIV can also be grown in cell culture. The third-generation ELISA-tests have a sensitivity approaching 100% and specificity > 99%. Used correctly, rapid tests have an accuracy closely approaching that of ELISA tests.
The p24 test and culture are mainly used in research, not in routine clinical settings and have been largely superseded by PCR. In resource poor settings none of these tests are routinely available.
Malawi relies on two different rapid tests for diagnosis of HIV in individuals, as per WHO testing recommendations for regions where HIV prevalence exceeds 10% and ELISA for quality control purposes and research. Single ELISA tests are used for ANC sentinel surveillance, in accordance with the recommendations of WHO on HIV testing for surveillance purposes.
Monitoring
To keep track of the progress of HIV disease, CD4 count and viral load are used. Viral load predicts the rate of disease progression and CD4 count indicates the stage of disease the patient has reached. Viral load tests measure the concentration of free virus in the blood plasma, in the form of HIV RNA. A viral load change of more than a 0.5 log10 copies/ml (i.e. a factor 2) is significant. These tests can be used when deciding to start therapy or for monitoring the response to therapy.
CD4 cells are detected using monoclonal antibodies to the CD4 molecule. Adults with normal immune function have a CD4 count of > 1000 cells/µl. Levels of 200–500 cells/µl, < 200 cells/µl and < 50 cells/µl constitute moderate, advanced and severe immune suppression respectively. As of now, CD4 and viral load testing is available only in referral hospitals and research laboratories in Malawi.
Distribution of disease
Incidence of HIV
The first documented case of HIV-1 in Malawi occurred in 1982, as molecular epidemiological analysis of stored blood spot from the Karonga Prevention Study has shown3. From 1982 to 1984 subtypes A, C and D were all present. By 1987 to 1989, subtype C had become the predominant subtype and AC, AD and DC recombinants had emerged. This study supports the general notion that HIV-1 subtype C spread from Central Africa to East and Southern Africa.
Information about incidence of HIV (number of new HIV infection in a given time period) was found in two studies from Malawi.
Pilcher and colleagues found a proportion of 1.8% acute (antibody negative) HIV infection among STD and dermatology clinic attendees, which has high transmission potential because of high viral load and presence of STDs.6 We have no recent incidence data of young people to assess changing incidence following health education behaviour modification campaigns.
Prevalence of HIV
Malawi monitors its HIV prevalence (number of HIV infections existing at a certain point in time) through sentinel surveillance at antenatal clinics (ANC). The most recent ANC sentinel data were collected from February to April 2003 and resulted in the HIV prevalence rates reported in table 2.
Table 2.
HIV prevalence by ANC site, 2003
| Sentinel Site | Locality | Number sampled |
Number HIV + |
% HIV + | (95% CI) |
| Kaporo Health Centre | Rural | 210 | 43 | 20.5 | (15.2–26.6) |
| Mbalachanda Health Centre | Rural | 193 | 28 | 14.5 | (9.9–20.3) |
| Rumphi District Hospital | Semi-urban | 517 | 84 | 16.2 | (13.2–19.8) |
| Nkhata-Bay District Hospital | Semi-urban | 522 | 126 | 24.1 | (20.6–28.1) |
| Mzuzu Health Centre | Urban | 846 | 176 | 20.8 | (18.1–23.7) |
| Kamboni Health Centre | Rural | 238 | 16 | 6.7 | (3.9–10.7) |
| Thonje Health Centre | Rural | 219 | 25 | 11.4 | (7.5–16.4) |
| Kasina Health Centre | Rural | 153 | 11 | 7.2 | (3.6–12.5) |
| Mchinji District Hospital | Semi-Urban | 548 | 99 | 18.1 | (15.0–21.6) |
| St. Anne's Mission Hospital | Semi-Urban | 272 | 27 | 9.9 | (6.6–14.1) |
| Ntcheu District Hospital | Semi-Urban | 500 | 110 | 22.0 | (18.5–25.9) |
| Lilongwe Bottom Hospital | Urban | 810 | 137 | 16.9 | (14.4–19.7) |
| Gawanani Health Centre | Rural | 206 | 35 | 17.0 | (12.1–22.8) |
| Milepa Health centre | Rural | 205 | 31 | 15.1 | (10.5–20.8) |
| Mianga Health centre | Rural | 203 | 47 | 23.2 | (17.5–29.6) |
| Mangochi District Hospital | Semi-Urban | 510 | 74 | 14.5 | (11.6–17.9) |
| Mulanje Mission Hospital | Semi-Urban | 510 | 122 | 23.9 | (20.3–27.9) |
| Nsanje District Hospital | Semi-Urban | 511 | 168 | 32.9 | (28.9–37.2) |
| Limbe Health Centre | Urban | 804 | 222 | 27.6 | (24.6–30.9) |
| Subtotal | Rural Semi-urban Urban |
1,627 3,890 2,460 |
236 810 535 |
14.5 20.8 21.7 |
(12.8–16.3) (19.6–22.1) (20.1–23.4) |
| Total | 7,977 | 1,581 | 19.8 | (19.0–20.7) |
Source: National AIDS Commission. HIV Sentinel Surveillance Report 2003. Lilongwe, 2003.
Women who visit the antenatal clinic do not represent the general population and thus ANC prevalence data do not represent the prevalence in the general population. When compared with community-based samples, ANC data generally overestimate the prevalence in young women (because ANC women are a selection of sexually active women) and underestimate the risk in older women (because ANC women are a selection of women less afflicted by factors like widowhood, divorce and STI associated with fertility and HIV). Overall, in sub-Saharan Africa, ANC data overestimate the risk in men and underestimate the risk in women.7
Crampin and colleagues confirmed that this was indeed the case in Karonga district.8 Directly standardised estimates of men and women from ANC data were 9.4% and 9.2 % versus 11.4% and 13.9% in the community. The prevalence of HIV among sexually active women in Karonga who did not attend ANC was 27%, against 12% in ANC women.12
The differences between ANC and community results in the Karonga study8 were mainly the result of sociodemographic factors like age, area of residence, marital status and moving household, but fertility differences have been important in other studies.7 This underscores the need to carefully adjust ANC data before making extrapolations to the general population, and emphasises that adjustment procedures might need to vary between populations. ANC sentinel surveillance data are used as input into the Estimation and Projection Package (EPP) software of UNAIDS to estimate the prevalence per location and region. These projections take into account the biases associated with over-represented urban ANC sites, but ignore the other biases.
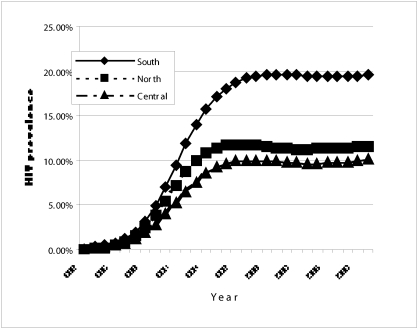
The estimated average adult (15–49 yrs) prevalence in Malawi for 2003 was 14.4% (95% CI: 12%–17%). Estimated prevalence in urban adults (23.0%; 95% CI: 19%–28%) was nearly twice as high as in rural adults (12.4%; 95% CI 10–15%). The estimated prevalence in the South in 2004 was 19.5%, almost double that of the North (11.3%) and Central regions (9.7%) and is projected to stay at that level if HIV prevention programs were to have no impact (figure 1).
Figure 1.
Projected HIV prevalence per region, 1982–2010
Source: Malawi HIV/AIDS estimates 2003. Technical report. Lilongwe, 2004.
Adjusting for the ANC underestimates found in Karonga, the national prevalence of 19.8% found in the ANCs is equivalent to an average national community prevalence of 20.0% and is higher than the NAC estimate of 14.4%.
Other sources of HIV prevalence data are clinical research studies, community based surveys and the data of the Malawi AIDS Counselling and Resource Organisation (MACRO). Their results are tabulated and range from 0% in pregnant women in the early 1980s to 99% in patient populations.
The Malawi National Blood Transfusion Service screens the blood of donors who receive prior advice about when not to give blood. The donors are therefore a highly selected group. Of 10246 donations between January and July 2005 342 (3.34%) were HIV positive using a p24 antigen test (personal communication - Dr J Emmanuel, Director of MNBTS).
Number of people living with HIV/AIDS
The EPP software also estimates the absolute number of people living with HIV/AIDS (PLWHA) from the ANC sentinel data (table 3). Although the urban HIV prevalence is double the rural HIV prevalence, in absolute numbers, more than twice as many HIV infected people live in rural areas as compared to cities. Like elsewhere in sub-Saharan Africa, the HIV epidemic has become a ‘women's epidemic’ in Malawi, with almost 1.4 times as many women as men infected. Combinations of the nineteen sentinel sites reported in table 2 were used to represent the 27 districts and 4 urban centres of Malawi. The resulting estimates of rural and urban prevalence were applied to the population structure to come up with estimates of the current number of HIV-infected individuals per district and urban centre (Table 4)
Table 3.
Estimated number of HIV infected persons in Malawi, 2003
| Indicator | Number of PLWHA | 95% Confidence Interval |
| Number of infected adults (15–49 yrs) | 760,000 | (630,000–910,000) |
| Number of infected adult women (15–49 yrs) | 440,000 | (370,000–530,000) |
| Number of infected urban adults (15–49 yrs) | 240,000 | (200,000–290,000) |
| Number of infected rural adults (15–49 yrs) | 530,000 | (440,000–640,000) |
| Number of infected older people (50 yrs and >) | 60,000 | (50,000–70,000) |
Source: National AIDS Commission. HIV/AIDS in Malawi. 2003 estimates and implications. Lilongwe, 2004.
Table 4.
Estimated number of HIV infected persons per district and region
| District | Number of PLWHA | District | Number of PLWHA |
| Chitipa | 7,000 | Mzimba | 22,000 |
| Karonga | 16,000 | Mzuzu City | 13,000 |
| Rumphi | 6,000 | Likoma | 1,000 |
| Nkhata Bay | 10,000 | ||
| Total Northern Region | 75,000 | ||
| Kasungu | 21,000 | Lilongwe Rural | 29,000 |
| Nkhotakota | 10,000 | Lilongwe City | 63,000 |
| Ntchisi | 9,000 | Mchinji | 12,000 |
| Dowa | 21,000 | Dedza | 16,000 |
| Salima | 24,000 | Ntcheu | 12,000 |
| Total Central Region | 216,000 | ||
| Mangochi | 54,000 | Blantyre Rural | 29,000 |
| Machingaw | 32,000 | Blantyre City | 99,000 |
| Balaka | 22,000 | Thyolo | 46,000 |
| Zomba Rural | 41,000 | Mulanje | 42,000 |
| Zomba Municipality | 13,000 | Phalombe | 17,000 |
| Chiradzulu | 18,000 | Chikwawa | 33,000 |
| Mwanza | 12,000 | Nsanje | 17,000 |
| Total Southern Region | 475,000 |
Source: Malawi HIV/AIDS estimates 2003. Technical report. Lilongwe, 2004
Incidence of AIDS-related diseases
A 16 month follow up study of 660 HIV positive people in Ndirande reported the incidence of AIDS and related diseases prior to the availability of ARVsj. The hospitalisation and death rate by CD4 count and WHO staging at enrolment are found in a copy of their table 5. Note TS is an abbreviation of Trimethoprim-Sulfamethoxazole. The most common event was non-specific diarrhoea (37 events per 100 person-years) followed by oral candidiasis, uncomplicated malaria, and fever of unknown origin. Bacterial disease was common (16.2 new events per 100 person-years), but the majority of bacterial isolates were resistant to TS in vitro. The joint Salvation Army/College of Medicine Bangwe home based care project has also enumerated the incidence of common symptoms and diseases during follow-up of home based care patients with stage 3 or 4 AIDS disease. Patients most often complained of cough, chest pain and fever, and like in the Ndirande study, uncomplicated diarrhoea was the most commonly diagnosed disease, followed by oral candidiasis and uncomplicated malaria.
Table 5.
Incidence of hospitalisation and deaths per 100 person-years of observation by CD4 strata and WHO clinical stage, Ndirande (Ref 10)
| CD4 Cells/ mm3 | WHO Clinical stage | |||||||||
| <100 | 100–199 | 200–350 | > 350 | P | I | II | III | IV | P | |
| Number enrolled* |
n=125 | n=159 | n=173 | n=175 | n=289 | n=215 | n=135 | n=21 | ||
| Incidence of hospitalisation# (95% Cl) |
172 (138–212) |
84 (64– 106) |
27 (12–39) |
90 (11–29) |
0.003 | 15 (3–9) |
60 (46–76) |
178 (144–217) |
237 (142–370) |
<0.001 |
| Incident of death## (95% Cl) |
60 (40–86) |
13 (6–23) |
4 (1–11) |
4 (1–11) |
<0.001 | 3 (1–7) |
5 (2–12) |
62 (42–86) |
88 (35–180) |
<0.001 |
Twenty-eight participants did not have a CD4 cell count documented at enrolment
Individuals may have experienced more than one hospitalisation
95% Cl indicates 95% confidence interval based on Poisson distribution
Prevalence of AIDS-related diseases
The joint Salvation Army/College of Medicine Bangwe home based care project also assessed the presence of symptoms at first assessment, severity and duration. Headache was the most common presenting symptom, closely followed by fever, chest pain, shortness of breath and cough. A few studies have reported on specific AIDS related diseases. For TB, please refer to the TB chapter. A study of stroke-like illness in HIV seropositive patients in QECH showed that a cerebral infarct was the cause in nearly half of the patients, followed by cerebral haemorrhage, toxoplasmosis and cryptococcal meningitis.11
Ten percent of women attending ANC in Phalombe had signs of oral lesions, with lesions being 1.6 times more common among HIV positive then HIV negative women; especially oral hairy leukoplakia, that occurred 30 times as often among HIV positive women.12
In a study into ocular findings among TB infected HIV patients with fever, the prevalence of microangiopathy was 17% in patients with AIDS symptoms and 5% in patients without.13 Non-typhoid salmonella infection - a self-limiting diarrhoeal disease in immunocompetent people- caused one-year mortality of 77% and showed a 43% recurrence in a study in QECH. Bacterial resistance was high to cotrimoxazol (73%), ampicillin (79%), gentamycin (43%) and tetracycline (40%).n
In another study in QECH among patients with invasive pneumococcal disease (almost all HIV positive), 42% had bacteraemic pneumonia and 30% confirmed meningitis. In-hospital mortality and total mortality were 39% and 63%. Antibiotic resistance was high for chloramphenicol (24%), tetracycline (50%) and cotrimoxazol (54%). Nearly all pneumococcal isolates were sensitive to erythromycin and 85% were sensitive to penicillin.15
Distribution of risk factors for HIV infection
Biological
STI
In Sub-Saharan Africa, the majority of adult HIV infections are acquired through heterosexual contact. The risk of transmission from one infected person to another is estimated to be 0.0011 (95% CI 0.0008–0.0015) per coital act and increases to 0.0041 if genital ulceration is present16. Many curable STIs enhance HIV transmission by increasing the infectiousness of an HIV-positive person and the susceptibility of the HIV-negative partner, resulting in a 2–10 times increase in HIV transmission per sexual contact, depending on the type and severity of the STD.2 Ulcerative STDs carry a higher risk of HIV transmission than non-ulcerative STDs because they damage the mucosal and skin barrier.
HIV spreads rapidly where STD prevalence is high and prompt access to adequate treatment limited. Several authors have shown increased risk of being infected with HIV (HIV prevalence) in persons with a history of STD, e.g. for urban ANC women (OR 1.9; 1.6–2.3)17, rural ANC women (OR 2.5)12 and men working at a sugar estate (OR 3.1; 1.9–5.0).18 Among men presenting with GUD at an STD clinic, those with a history of STD had an increased risk of being HIV positive (1.9; 1.3–2.9) especially if the history of STD concerned an ulcerative disease (OR 2.4; 1.5–4.0).19 Men who had evidence of previous syphilis infection also had an increased risk for new HIV infection (HR 1.9; 1.1–3.3 in 1994 and HR 2.3; 0.8–6.4 in 1998).5 Refer to the STI chapter for detailed information on the epidemiology of STIs in Malawi.
Nutrition
There is a strong mutual association between nutrition and HIV / AIDS. Any immune impairment that results from HIV / AIDS leads to malnutrition. It is unlikely that malnutrition in itself increases the risk of acquiring HIV, but it does lead to immune impairment and once a person has been infected with HIV, it worsens the effect of HIV and contributes to more rapid progression of AIDS.
Summary: distribution of HIV/AIDS in Malawi.
HIV incidence data are scarce
HIV incidence is 4.2% per year in ANC women and 2.5%–4.2% per year in estate workers
The NAC estimate of HIV prevalence based on ANC surveillance is 14.4% for adult Malawians, but this is an underestimate of true community prevalence
The estimated community prevalence adjusted for ANC underestimation is 20% for adult Malawians
The NAC estimate of number of PLWHA is 760.000, > 60% are in the Southern Region
Diarrhoea, oral thrush and malaria are the most common problems in HIV positive patients
Headache, fever and respiratory complaints are most commonly reported by AIDS patients.
Wasting in AIDS can be caused by increased metabolic demand for nutrients without concomitant increase in dietary intake, diarrhoea and other opportunistic infections, malignancy, malabsorption, or in Africa by starvation secondary to AIDS-related poverty. According to a June 2003 WHO technical consultation, to maintain body weight and physical activity, asymptomatic HIV infected persons have an increased energy need of around 10%. During symptomatic HIV and later AIDS energy requirements increase by 20–30%.20 There is insufficient data to support increased need of protein or fat. Wasting is one of the most frequent manifestations of AIDS in sub-Saharan Africa, especially in food-insecure communities, with about half of all clinically symptomatic AIDS patients being wasted.
Two small clinical trials, one in Tanzania, have reported micronutrients reduce progression of AIDS in the early stages of disease 21,22 Please refer to the Nutrition chapter for more information about the epidemiology of malnutrition in Malawi.
Needlestick accidents & hygiene
Exposure to HIV is a serious occupational hazard among healthcare staff in high prevalence countries. The risk of transmission for a percutaneous needlestick accident is around 0.3 %, less for solid needles, shallow needlesticks or mucosal exposure, and more for deep injury, the needle visibly contaminated with blood directly into an artery or vein23 WHO reported in the World Health Report 2002 that of 35 million health-care workers, 2 million experience percutaneous exposure to bloodborne diseases every year. Two and a half percent of HIV/AIDS in health care workers worldwide is thought to be due to needlestick injuries. In an assessment in 20 countries, health care workers experienced on average 1–9 needlestick injuries per year.24 Some data on the occurrence of needlestick accidents specific for Malawi is found in a recent report on HIV post exposure prophylaxis (PEP) for occupational injuries in Queen Elizabeth Central Hospital 25.
The PEP programme was started in 2003, initially with donated drugs. 29 clients (7 nurses, 10 doctors, 2 clinical officers, 10 others) sought advice after occupational injuries in the first year, of whom 19 started PEP, all with Duovir®. In one case PEP was stopped due to side effects. Few nurses and clinical officers attended as clients. Although the incidence of occupational injuries reported in interviews was high (76%), uptake in the PEP programme was unacceptably low, in particular among nurses, mainly due to poor awareness, but sometimes because they refused an HIV test. By extrapolation 66% of those injured should have used PEP, but did not.
Blood transfusion
Transfusion of HIV infected blood carries a nearly 100% transmission risk. All blood in Malawi is screened before transmission with p24 antigen ELISA test which has a sensitivity of 99.8% and a specificity of 98.9%, but even such a test has a window period of up to 10, but usually 5–7 days. Considering the current prevalence of HIV in blood donations of 3.3%, a number of blood donations that show up negative in the test will nevertheless be infected.
Helminth infections
Helminth infections have been postulated to modulate HIV infection. No such evidence was found in a cohort of 389 patients in Lilongwe. Helminth infections were less common among HIV positive patients than among HIV negative patients. HIV positive patients were more likely to report watery stool, abdominal pain and rectal itching but these were not associated with helminth infection. CD4 counts of HIV positive individuals with and without helminth infection were similar and treatment of identified infections did not alter HIV RNA levels.26
Malaria
Acute malaria episodes were associated with transient increases in HIV viral load in a recent study among PLWHA in Thyolo, especially in those with fever, high density parasitaemia and higher CD4 counts.27 Although the average increase was modest (0.25 log copies / ml), the impact in terms of enhanced disease progression and transmission on population level may be important because of the ubiquitous nature of both diseases. Modelling work would have to confirm this.
Behavioural
Age at first sexual contact
Because condom use is very low among adolescents (paragraph 3.2.2), an earlier sexual debut places adolescents at higher risk of contracting HIV or any other STD.
Although Malawi's traditions dictate that young girls abstain from engaging in sexual activities until being initiated by a traditional advisor following the onset of menses, there is increasing evidence that early sexual debut is the norm among most adolescents.
Many studies have shown that over 50 percent of adolescents report to have had sexual intercourse before the age of fifteen.28,29,30,31,32 Some adolescents start having sex as early as aged 8 to 13.33,34,35
However, the MDHS 2000 reports that the median age of first sex is 17.1 years for adolescent girls, and 17.7 for boys. For girls this age at first sex remained the same over; for boys it declined from 19.6 years. Preliminary results from the DHS2004 show a recent increase in age of first sexual intercourse (Table 6).
Table 6.
Number of sexual partners, condom use and age of first sex
| Baseline DHS 2000 | DHS 2004 | |||||||
| Male | Confidence | Female | Confidence | Male | Female | |||
| (a) Proportion of sexually active respondants who had sex with a non-regular partner within the previous 12 months |
0.33 | 0.44 | 0.25 | 0.08 | 0.09 | 0.07 | 0.26 | 0.08 |
| (b) Propotion of people reporting the consistent use of a condom during sexual intercourse with a non-regular partner |
0.39 | 0.32 | 0.46 | 0.29 | 0.03 | 0.28 | 0.47 | 0.3 |
| (c) Median age at first sex amoung 15–24 year olds with a non-regular partner |
17.7 yr | 17.1 yr | 18.1 yr | 17.4 yr | ||||
Source: Malawi Demographic and Health Surveys 2000 and 2004
Number of sexual partners and abstinence
The risk for HIV transmission increases with a higher number of sexual partners, especially when these partners are from a high risk group, e.g. bargirls. Societal norms enable Malawian men to engage in multiple sexual relationships either formally in polygamist unions or tolerated informally through extramarital sex.36 However, women are presented as being ideally faithful38.
Extramarital sex was not an important risk factor in 1994 and 1998 cohorts of male estate workers.5,37 Dallabetta in the late eighties found a slightly increased HIV risk associated with promiscuity (OR 1.6; 1.4–1.8) in antenatal women, but good recent data about the magnitude of HIV risk associated with number of sexual partners were not found for Malawi.
The Malawi Diffusion and Ideational Change project (MDICP) used worry about HIV transmission (perceived risk) as a proxy for actual HIV infection. They examined the association between sexual behaviour and worry about HIV risk among married couples in rural communities in Balaka, Mchinji and Rumphi, in two waves in 1998 and 2001.
Women who knew or suspected their spouse was unfaithful perceived their risk for HIV twice as high as women who reported their husbands to be ‘probably faithful’. Men were not worried about their spouses' unfaithfulness, possibly because they are expected to divorce an adulterous wife. Also moving from a monogamous to a polygamous marriage increased the first wife's worry, by three times. Again, men did not worry: after all, they themselves selected the second wife. Both men's and women's worries about AIDS decreased between 1998 and 2001 and this was associated with changes in behaviour. For women these preventive strategies were discussing with their spouse the importance of avoiding infection and, increasingly, divorcing their unfaithful husbands. Men reported having sex with fewer partners and more careful partner selection, based on demographic characteristics (e.g. village girls, school girls, older married women) or on information obtained through their social networks about the sexual biography of their prospective partner.38,39,40
Self-reports of sexual partnerships are subject to social desirability bias and therefore, face-to-face interviews may not give valid results. Qualitative data show that village residents are extremely aware of the sexual behaviour of others, especially their own spouses. Respondents' reports about others might therefore be closer to the truth than self-reported sexual partnerships.38 In the MDHS 2000, less than 1% of married women and 17.5% of married men said they had had extramarital sex in the past year.41 In the 2001 MDICP study, these figures were 2.5% for women and 11% for men. But in comparison, a probably more realistic 18% of women and 26% of men said their best friends had committed adultery in the past year. Half of all married women and about eighty percent of married men believed their spouse to be faithful.38
According to the 2000 MDHS, unmarried women were slightly more likely to have had more than one sex partner than married women, i.e. 1.7% versus 0.9 %. Unmarried men however were less likely to have had more than one sexual partner, i.e. 14.5% (versus 17.5% of married men).41
Transactional sex
Often, gifts or money are exchanged in casual or extramarital sex. Sometimes this transactional sex involves ‘sugar daddies’, generally older men who obtain sexual favours from young women or girls in exchange for money, clothes or other gifts, but also adult single women often have a man friend who helps them financially or in kind.1 Maluwa-Banda described that these ‘sugar daddies’ do not use condoms to protect themselves from HIV infection and that some ‘sugar daddies’ specifically opt for girls because they are thought not to be infected with HIV.42 Many low income women will end the relationship if the financial report they receive from their partner is not good enough, and many men will leave low income women if they become pregnant. Thus, although -unlike men- most women may not have many partners at the same time, their serial monogamy and their partner's promiscuity places them at risk of HIV.1
In the 2000 MDHS, one fifth of men, either married or not, reported having paid for sex in the previous 12 months. In the 1996 national KAP survey, 1% of married women compared to 19% of unmarried women reported receiving money or gifts for sex43. Other studies reported 24% and 66% of respondents being engaged in transactional sex.1
Commercial sex
Apart from the high percentage women and men engaged in occasional transactional sex, some women depend mainly on sex for their livelihood. Commercial sex workers often are economically disadvantaged and socially stigmatised. This, together with their high sexual partner turnover, renders them at high risk of HIV and other STIs and thus also makes them an important group in the spread of HIV. Prostitution is illegal in Malawi. However, commercial sex is widespread in the form of food handlers, bargirls and cleaners offering sex in rest houses and bars. The National Aids Strategy Planning Unit (1998) reported that sometimes widows who have been dispossessed of all belongings after death of a husband take to commercial sex to make money.
No data were found from Malawi which quantify the risk of HIV transmission through commercial sex, but evidence exists that risk behaviour among commercial sex workers is high. Zacharia et al in Thyolo district showed that one quarter of CSW had an active sexually transmitted disease (STD), 5% had genital ulcer disease (GUD). The majority with an STD engaged in sex while symptomatic and most did not use condoms consistently. Disturbingly, having a GUD was associated with no condom use. Client pressure was the most commonly reported reason for unprotected sex.ar
Marital status
In the Karonga community study, compared to married people, divorced or widowed persons had an increased risk of being HIV positive (OR 3.3, 1.9–5.8) and never having married was only slightly protective (OR 0.9; 0.3–2.2).8 In the 2003–2004 data of MACRO VCT centres (but not in the 2002–2003 data), HIV rates were 4 to 7 times higher in separated, divorced or widowed people. as,at The increased prevalence in widowed people can likely be explained by the fact that their husband or wife had probably died of AIDS. From the MDIC project it appeared that divorcing an unfaithful husband was one of the coping strategies that women used to reduce their risk of HIV, but for many this may have been too late.38
Condom use
A Cochrane review indicates that consistent use of condoms results in 80% reduction in HIV incidence. Consistent use was defined as using a condom for all acts of penetrative vaginal intercourse. Whether condoms were used correctly and perfectly for each and every act of intercourse was unknown, thus the 80% is the effectiveness and not efficacy of condoms for prevention of HIV.47
Self-reports about condom use suffer from the same social desirability bias as reports on number of sexual partners, especially when the use of condoms is targeted or encouraged by government or NGO behaviour change campaigns. Indeed, a study among antenatal women found no relation between reported condom use and frequency of STIs.48 The following data therefore have to be interpreted with caution.
According to the MDHS 2000, only 6% of men and 3% of women report use of condoms within marriage. Condoms were more often used outside of marriage, i.e. by 39% of men and 29% of women. Compared to the 1996 KAPH results, this represents a 50% increase for women (from 20% to 29%) but a stable percentage for men. For women, being younger, never married, living in the Northern Region, having a higher education, having been drunk and urban residence were all associated with condom use outside of marriage. In general the same associations existed for men, but less pronounced and with the exception of age and marital status: both the youngest (15–19 yrs) and oldest (40–54 yrs) age groups used condoms less often, and married men were more likely to have used a condom with a non-cohabiting partner than unmarried men. Disturbingly, condom use during paid sex (which probably carries a higher risk) was even lower than during sex with general non-cohabiting partners: 35% versus 39%.41 Qualitative data from MDICP show that among rural Malawians, acceptability of condom use for sexual relationships outside of marriage had increased between 1998 and 2001, but not within marriage. Quantitative survey data showed that reported condom use for family planning, for extramarital affairs, by best friends and by network partners all approximately doubled within those four years.38
Youth between 15 and 19 years is the group believed to have the highest rate of new HIV infections in Malawi. In an extensive survey among secondary school students by PSI, 34 % of sexually active girls and 55% of sexually active boys had ever used a condom. This is much higher than the reported percentages in the MDHS 2000, possibly because secondary school students are a selected group. Main reasons for not using condoms were: condoms not at hand when they needed them and moral objections.
In a 2000 study among VCT clients in rural Thyolo, 7% used condoms always, 44% intermittently and 49% never. The reasons for no condom use were: having sex with regular partner (37%); having no prior knowledge about usefulness of condoms (34%); condoms not available (21%); reduction of pleasure (5%); partner refusal (2%) and religious reasons (1%).117
In a KAP study among sex-workers in 1990 in Dedza, Mponjela and Mchinji, correct condom use was 19% and the proportion ever condom use was 67%. Although nearly all participants knew that HIV+ people can look healthy, in focus group discussions it emerged that necessity of condom use was judged from the appearance of the partner.49
Sociocultural
Poverty
Analysis of the DHS2000 survey by wealth quintiles50 (with the lowest quintile being the poorest fifth of households in Malawi and the highest quintile being the richest) shows little inequality in relation to knowledge, attitudes and behaviour about HIV/AIDS between the rich and poor. The concentration index is a measure of inequality, with 0 being total equality and −1 and +1 being complete inequality51. There is equality for self reported genital ulcer, unsafe sexual practice in women, and attitudes towards people with HIV. There is however increase use of VCT and condoms and unsafe sexual practices in the rich. Nearly twice as many rich males had sex with an irregular partner in the previous twelve months as poor males, suggesting money buys sex.
Cultural practices
In many communities in Malawi, sex is seen as a cleansing agent which has the power to absolve sins and combat evil spirits. Examples are the practice of a man having sex with young girls after initiation (kutchotsa fumbi, wiping away the dust), widow cleansing (kupita kufa), or girls who tried to induce an abortion being obliged to have sex thrice: once for the sin of sex before marriage; once for becoming pregnant; once for ending the pregnancy. The risk of becoming HIV infected does not only exist during the initiation: according to a study in Mulanje, girls were often encouraged to practice sex afterwards to make sure they will be good wives. However, some respondents indicated that this practice has diminished since the advent of AIDS.1
At the same time many communities believe in the ‘equilibrium theory’ of health, whereby a hot/cold balance has to be maintained in the body. Sex is seen as a heating agent and has to be avoided by pregnant women, to prevent death to the husband, his wife and the unborn foetus. The resulting required abstinence period may be up to a year long and may result in male partners turning elsewhere for sex.
The degree to which harmful sexual practices still persist is not well known. Two studies estimated that around half of girls and of boys expected to undergo sexual cleansing after initiations and another found that over 80% or women and 60% of men had been involved in initiation ceremonies.1
Commercial sex centres
All workers in public locations offering food, drinks or accommodation (i.e. including those who work as commercial sex workers) are required by law to present to the community police a medical certificate once a month. The police regularly conduct patrols to enforce this.44 Valid data about the number and distribution of commercial sex centres do not exist, but many bars and resthouses have commercial sex workers.
Economic environment (trade centres, transport routes)
AIDS is believed to have spread along the major trading and transport routes from Central to Southern Africa and also within countries. Shorter distance to a commercial centre (see previous graph) was a strong predictor of increased HIV risk in the incidence study at Nchalo sugar estate.5 Travelling was also among the strongest risk factors in the Karonga community studies, with odds ratios ranging from 1.7 to 5.3 depending on the sex and region of residence of the respondent. Whereas a detailed analysis of HIV prevalence along Malawi's major transport routes has not been done, it is obvious that the major trade centres (the cities) and economically most active region (the Southern region) have the highest HIV prevalence.
Education
In the late eighties, early nineties, higher education was associated with an increased risk of HIV.8,52,53 Later on, this association disappeared, possibly because the most educated may be responding more readily to health education programmes.54 The same trend was seen in Malawi.8
Impact of HIV/AIDS
Life expectancy and burden of disease
Life expectancy
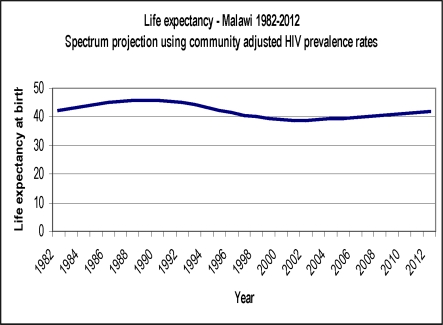
Figure 2 is a projection of life expectancy, using estimated community prevalence data adjusted for the underestimation in ANC prevalence estimates. It shows that life expectancy decreased by 6 years (or 13 %), i.e. from the pre-AIDS level of 45 years for Malawians born in 1989 to 39 years for those born in 2002, after which it is projected to rise again.
Figure 2.
Projected life expectancy
In Karonga district median survival of HIV positive patients was 8 years, 36% were alive at 10 years post seroconversion. Ninety-one percent of deaths were attributable to HIV.55
Summary: Malawian determinants for HIV/AIDS.
Sexually transmitted diseases are common
Adolescents start sex at a median age of 17 years
The degree to which harmful sexual practices such as kutchotsa fumbi and kupita kufa still exist is not known
A quarter of men have multiple partners and half report not using a condom with a non-regular partner
Transactional and commercial sex are common - up to a fifth of men report having paid for sex in the last twelve months
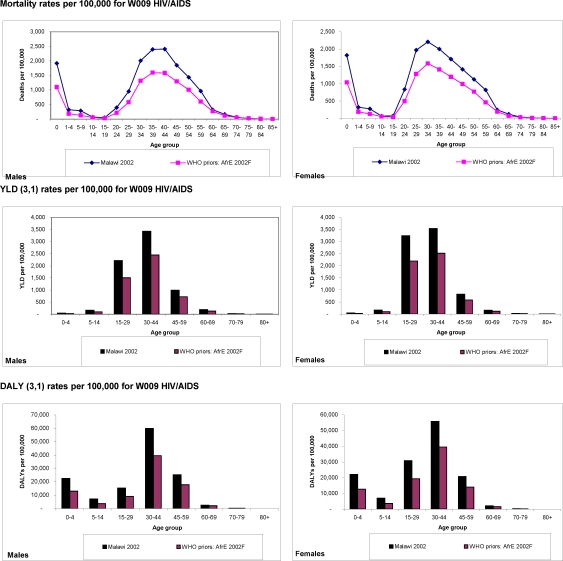
Burden of disease
HIV/AIDS is the dominant cause of disease burden in Malawi. An analysis of the burden attributable to HIV/AIDS is presented using WHO's Global Burden of Disease analysis which uses Disability Adjusted Life Years (DALYs)56. The burden in Malawi is compared to the burden caused by these preventable diseases in other southern African countries (labelled WHO AfrE in Figures 3). The WHO Burden of Disease Unit publishes estimates of DALYs which are a combination of Years of Life Lost (YLLs) and Years Lived with Disability (YLDs). These are used to measure the burden of disease for each country and region. HIV/AIDS accounts for 31% of the total burden of disease measured in DALYs, followed by respiratory diseases (11%) and malaria (9%).
Figure 3.
Orphans
Hunter and Williamson, estimated the number of orphans (defined as loss of one parent) in Malawi in 2005 to be one million, or one fifth of all children under 15 years (table 7). Maternal (mother dead) or double orphans (both parents dead) constituted about half of these and paternal orphans (father dead) the other half. Almost eighty percent of maternal / double orphans were estimated to be due to AIDS.57
Table 7.
Estimated number of orphans, per type and as a percentage of total; number of orphans, 1990–2010
| Population <15 | Maternal /double orphans all causes |
Maternal /double orphans as % of children < 15 |
% of maternal /double orphans from AIDS |
Paternal orphans all causes |
Paternal orphans (% of all children < 15) |
Total orphans all causes |
Total orphans (% of children < 15) |
|
| 1990 | 4,340,904 | 255,502 | 5.9% | 37,9% | 383,253 | 8.8% | 638,755 | 14.7% |
| 1995 | 4,450,393 | 352,934 | 7.9% | 51.8% | 529,401 | 11.9% | 882,335 | 19.8% |
| 2000 | 4,659,452 | 426,421 | 9.2% | 64.1% | 521,181 | 11.2% | 947,602 | 20,3% |
| 2005 | 4,734,313 | 499,935 | 10.6% | 72.9% | 499,935 | 10.6% | 999,870 | 21.1% |
| 2010 | 4,674,103 | 553,003 | 11.8% | 78.4% | 452,457 | 9.7% | 1,005,460 | 21.5% |
Infant and child morbidity and mortality in HIV affected households
Crampin et al found that infants in Karonga district who were born to HIV infected mothers were 3.3 times more likely to die than children of HIV infected women, for children aged 1–5 years the risk was five-fold. Child mortality was associated with death of HIV infected mothers, but not of HIV infected fathers or HIV uninfected mothers. No association was found between maternal HIV status or orphanhood and stunting, wasting and reported ill-health. Cumulative mortality at 10 years was 49% among children of HIV infected mothers. Most of excess deaths were due to vertical transmission.58
Economic
The economic effects of AIDS are first felt by individuals and their families and then by firms and businesses and the macro-economy. The two major economic effects of the HIV epidemic are reduction in labour supply and increased direct and indirect costs associated with medical care, funerals, lost time due to illness, recruitments and training costs to replace workers, and care of orphans.59
Formal evaluations of the costs for households have not been found, but results of focus group discussions and case histories suggest that the normal redistribution and reciprocity arrangements that enable households to share resources during periods of food shortage are severely threatened by HIV/AIDS.60 Individuals report doing ganyu (casual labour) as a coping mechanism. Although this supplements the income, the labour supply available for the household decreases.61 The impact of AIDS on firms consists of increased expenditures (for health care, funerals and replacement of employees) and reduced revenues (absenteeism due to illness, funeral attendance or training). A national survey among 74,858 micro- and small enterprises was conducted in Malawi in 2000. These enterprises are predominantly located in rural areas, employ 38% of the total workforce, contribute income to 25% of households and contribute about 15.6% to the GDP. The survey showed that 12.4% of firms were conscious of being affected by HIV/AIDS. But 37%, i.e. double the HIV infection rate, were likely to have been affected as measured through proxy questions like having additional dependants, increased absenteeism and health and funeral expenses. The sectors most affected were construction, services and forestry, while crops, livestock and fishery were least affected. The type of impact was different for the different sectors: while 38% of crop-producing firms had to downsize their businesses, possibly because of reduced labour to work on the farms, most of the other firms felt the impact on their market with fewer customers. The transport sector mainly suffered through reduced profit levels.62
Three reports estimated HIV/AIDS associated costs incurred on larger firms, i.e. a tea estate, Brown and Clapperton Limited (a now closed Blantyre-based industry) and Lonrho Companies, all in the mid 1990s. These costs accounted for 3.4%, 1.5%–6% and 3.4% of gross profit, respectively.63,64,65
The economic effects on the public sector are enormous. In July 2001, the Malawi Institute of Management asessed the effect of HIV/AIDS on five public sector organizations, i.e. the Ministries of Health (MOH), Education, Science and Technology (MoEST), Agriculture and Irrigation (MoAI), Water Development (MoWD) and the Malawi Police Service.66 The average annual attrition rate was 2.3%, of which 50% was due to death. The age and gender profile of these deaths suggests that much of this mortality is AIDS related.
All ministries except MoEST experienced higher death rates than what was expected based on age-sex specific death rates in the general population. All ministries have a high number of vacancies (e.g. MoEST 58%) and vacancy levels have increased considerably over the past five to ten years. Data on absenteeism are generally not recorded, except for staff working in the Police Hospital. Absenteeism due to morbidity had tripled in the last 7 years. Available data from the MoEST suggest that training costs alone for replacing teachers deceased in the period 1990–1999 amounted to MK 635 million (5.5 million US $). Replacement costs for agricultural professionals were estimated at US $ 9 million and 290 paramedical deaths cost 13 million MK (113,000 US $). The estimated direct costs to the whole public sector associated with death benefits, absenteeism due to morbidity, funeral costs and attendance to funerals of government employees was between MK 6.6 million and MK 9.6 million per annum (US $57,000–83,000).
Where HIV-AIDS associated costs are financed from savings, the reduction in investment could lead to a reduction in economic growth. However, some studies have found that the macro-economic impacts may be small, especially if there is a plentiful supply of labor and worker benefits are small.59
Health services
The government of Malawi and the World Bank reported in 1998 that the annual death rate among health personnel was 6 times the expected rate (3% versus 0.5%). Harries et al in a nationwide survey among health care workers found that 2% of them had died during 1999, the majority from TB and chronic illnesses, believed to be mainly AIDS-related. They projected that around one quarter of all health staff working in 1999 would have died by 2009.67
Effective interventions
Biological interventions
Circumcision
Quite a few observational studies show a lower prevalence of HIV in circumcised men, but confounding in these studies (for example by religion) has not been adequately addressed. A Cochrane review found insufficient evidence to support an interventional effect of male circumcision on HIV acquisition in heterosexual men.68 Three RCT are currently being done in Kenya, Uganda and South Africa and scheduled for completion in 2005–2006. Preliminary encouraging results are available from one such trial in Johannesburg69. The trial of over 1500 men circumcised and a similar number followed up as controls has the results shown in the figure.
Summary : impact of HIV/AIDS in Malawi.
Life expectancy has fallen to 39 years
HIV causes a third of the total burden of disease
20% of children have lost one parent; 10% have lost their mother or both parents
The major economic costs are associated with health care, funerals, time lost due to illness, recruitment and training costs to replace workers and orphan care
The results of these trials will need to be carefully considered before circumcision is implemented as a public health intervention for prevention of sexually transmitted HIV.
Treatment for STIs
There is limited evidence from randomised controlled trials for STI control as an effective HIV prevention strategy. In Rakai, Uganda, after 3 rounds of treatment of all community members for STIs the rate ratio of incident HIV infection was 0.97 (95%CI 0.81 to 1.16), indicating no effect of the intervention. In Mwanza, Tanzania however, a more targeted approach of strengthened syndromic management of STIs in primary care clinics led to a 38% reduction (95%CI 15% to 55%) in HIV incidence in the intervention group.70 Refer to the STI chapter for information about treatment of STIs in Malawi.
Prevention of needlestick accidents
MOH in cooperation with JHPIEGO started training staff in infection prevention and in the quality improvement process in 2001 in the four central hospitals and in Chiradzulu District Hospital, St. Johns hospital and Likuni Hospital, resulting in steady progress in achievement of performance standards in all hospitals and three sites achieving standards for external recognition. This program was extended to Chitipa, Rumphi, Nkhata Bay, Mzimba, Karonga, Salima and Mulanje District Hospitals in 2004 and will be further expanded to include more hospitals and NGOs in the near future.
Screening of blood
All blood is screened by the Malawi National Blood Transfusion Service.
Nutrient supplementation
A typical World Food Programme food supplementation scheme for community home based care patients in urban Bangwe, Blantyre had no effect on survival, nutritional status or symptom relief71. Food supplementation to HIV/AIDS home based care patients and their families does not seem to work well, possibly because the intervention is too late to affect the course of disease or insufficiently targeted perhaps due to problems of distribution in an urban setting.
Ready To Use Food (RTUF) has successfully been used in therapeutic feeding of malnourished children (also in Malawi, in both hospital settings and the community) and in emergency relief situations (refer to nutrition chapter). Its effectiveness in management of HIV in Malawi is currently being investigated.
In a recently reported RCT from Tanzania, HIV infected women taking multivitamins (B, C and E) had a 27% reduced risk of dying and a 50% reduced risk of progressing to WHO stage 4. The effect of vitamin A alone was smaller and adding vitamin A to the multivitamin regimen reduced the efficacy of multivitamins72. As of now, no micronutrient interventions have been implemented in Malawi.
Vaginal microbicides
Microbicides are products that are applied vaginally to reduce transmission of HIV during sexual intercourse. They work by killing or immobilizing the virus, by forming a barrier between the virus and vaginal tissue, by boosting the vagina's natural defences against HIV or by preventing replication of HIV. Modeling work has shown that if a 60% effective vaginal microbicide would be used by 20% of women in half of unprotected sexual acts, 2.5 million infections would be averted globally in 3 years.73 The most extensively researched product has been nonoxynol-9, a spermicide. A Cochrane review found no evidence that nonoxynol-9 protects against vaginal acquisition of HIV infection by women from men. There is evidence that it may do harm by increasing the frequency of genital lesions.74 However, many other products with different mechanisms of action have passed safety tests and the efficacy of four products is currrently being tested in trials Africa and Asia. Among these is Buffergel, a product that maintains the protective acidity of the vagina. Buffergel was proved to be safe and acceptable in Malawi75 and is currently in efficacy testing in Lilongwe and Blantyre and in several other African countries.
Cotrimoxazole prophylaxis
Opportunistic infections are an important cause for the increased morbidity and mortality in patients with HIV, and two randomised trials in Côte d'Ivoire show that prophylaxis using cotrimoxazole (which is effective against many of those infections) reduces morbidity and mortality in HIV infected smear positive TB patients76 and morbidity in patients with early symptomatic HIV.77 Following these studies, WHO/UNAIDS issued provisional recommendations that cotrimoxazole be given to all patients living with AIDS.78 Unlike Côte d'Ivoire, in Malawi - at least in the Southern region - resistance to cotrimoxazole is widespread.10, 14, 79,80 Operational research to assess the feasibility and effectiveness in the Malawian setting was therefore carried out in Thyolo and Karonga districts.
From 1 July 1999 onwards, TB patients registered with the NTP in Thyolo District were offered VCT and when tested HIV positive, cotrimoxazole prophylaxis 480 mg twice daily for the duration of their TB treatment and indefinitely thereafter. Following this intervention, all-cause end-of-treatment mortality decreased from 36% to 28% for all TB patients (p<0.001), from 49% to 37% for smear-negative pulmonary TB patients (p<0.01), from 40% to 33% for extrapulmonary TB patients (p=0.05) and from 22% to 20% for smear positive pulmonary TB patients (p=0.5). Because no HIV test results were available for the pre-intervention period, no distinction could be made between HIV positive and HIV negative individuals.115 Compliance was high (94%) and simpler methods like verbal verification and pill counts showed high sensitivity and positive predictive values when compared with the urine testing.81 Ninety-three percent of patients were still taking the free cotrimoxazole tablets 3–6 months after completing the TB treatment and wished to do so indefinitely. Two thirds said they would not be able to afford to buy the drug themselves.82
In Karonga district a similar intervention was started in 2000, with similar reductions in overall mortality.114 Because this study also had HIV test results available for some of the patients in the pre-intervention period, it was found that the reduction in mortality was confined to HIV positive patients and that the observed reduction in mortality could be attributed to the cotrimoxazole prophylaxis. The Karonga study did show a strong reduction in mortality among HIV positive smear positive TB patients.
Cotrimoxazole prophylaxis for HIV positive TB patients as part of a VCT/CTX package has been implemented in July 2003 in 15 hospitals in Malawi. Of all TB patients who accepted VCT and tested HIV positive, 97% accepted cotrimoxazole prophylaxis.82
In Thyolo, resistance of faecal E. coli to cotrimoxazole was higher (89%) in those on cotrimoxazole prophylaxis compared to those not receiving cotrimoxazole prophylaxis (77%), indicating that the benefits of cotrimoxazole prophylaxis in preventing non-typhoid Salmonella bacteraemia and enteritis might become limited in the future.84
The Ndirande study found a high probable or confirmed bacterial infection rate of 78 new events per 100 person-years in HIV patients (of whom 15.3% developed TB) but also a high cotrimoxazole resistance rate of 76%10. The authors discuss the problems of cross-resistance to SP particularly when the incidence of malaria was found to be 34.1 per 100 person-years.
Anti-retroviral therapy
According to the Malawian treatment guidelines for AIDS, adult patients are eligible for ARVs if they are known to be HIV-seropositive and understand the implications of ARV therapy, plus they must be in WHO stage 3 or 4, or have a CD4 count below 200 cells/µl or be in WHO stage 2 with TLC < 1200 cells/µl. The exception are patients in WHO class 3 who only have minor manifestations of oral hairy leukoplakia or vulvo-vaginal candidiasis.85 See table 1 for WHO staging.
First line regimen is currently (2006) stavudine (d4T) + lamivudine (3TC) + nevirapine (NVP). In case of adverse reactions to these drugs the stavudine component may be substituted by zidovudine (AZT) and the nevirapine component by efavirenz (EFV). If patients fail the first line regimen, the recommended second line regimen is zidovudine (AZT) + didanosine (ddI) + Nelfinavir (NFV).
Data about the clinical effectiveness of ARV in Malawi are available from the programs in the Lighthouse Clinic in Lilongwe that offers ARV at a cost of $US 20–25 per month and from the free ARV program provided by Medicins Sans Frontieres (MSF) in Thyolo. The results, based on their most recently published data are tabulated (Table 9).
Table 9.
Effectiveness of ARV program, the Lighthouse Lilongwe and MSF Thyolo
| Indicator | Lighthouse, Lilongwe | Thyolo DH |
| Hosseinipour et al86 | ||
| References | Neuhann et al87 | Harries et al89 |
| Hosseinipour et al88 | ||
| Description of cohort | ||
| Jan–Jun 2003 (ref 86) | ||
| Period | Jul–Dec 2003 (ref 87) | April–Sep 2003 |
| Jan–Jul 2003 (ref 88) | ||
| 179 (ref 86) | ||
| Number of patients | 753 (ref 87) | 220 |
| 141 (ref 88) | ||
| WHO stage 3 or 4 | 62% (ref 88) | Not reported |
| Women | 52% (ref 88) | Not reported |
| CD4 before ART (cells/µl) | 50 (ref 88) | Not reported |
| Fee | For medication | Free |
| Process | ||
| Alive and on ARV | 64% at 6 months (ref 88) | 90% after 3–6 months |
| Lost to follow-up | 7% at 6 months(ref 88) | 0% after 3–6 months |
| Stopped therapy | 3% at 6 months (ref 88) | 4% after 3–6 months |
| On alternative 1st line therapy | 1% (ref 88) | 4% |
| On 2nd line therapy | 0% (ref 88) | 0% |
| Adherent ≥ 95% | 95% (ref 88) | 99% |
| Outcome | ||
| Median change in bodyweight (kg) | 5.7 (ref 88) | Not reported |
| Median change in CD4 count (cells/µl) | 92 (ref 88) | Not reported |
| HIV RNA below 400 copies | 79% (ref 88) | Not reported |
| Resumed normal daily activity | 72% (ref 87) | 88% |
| Early mortality (≤3 months) | 25% (ref 86) | Not reported |
| Total mortality | 27% (ref 88) | 6% |
| Side effects reported | 32% (ref 87)* | 14% |
Study only reported on neuropathic pain
Early mortality (in the period between seeking treatment and 3 months after starting ARVs) was high, i.e. 25% and was the leading cause of loss to follow-up in clients at the paying ARV programme of the Lighthouse Clinic in Lilongwe. Lighthouse uses a fast track system in which patients are seen by a nurse who uses an algorithm to decide if patients need to be referred to clinicians, which occurred in 11% of visits. Adherence of ≥95% was report for 95% of clinic visits. Three quarters of patients had resumed their previous daily activities, one third reported neuropathic pain. The non-paying programme at Thyolo district hospital had a much lower mortality, and less side effects, possibly as a result of broader inclusion criteria (WHO 3 or 4 or CD4 count under 350). Loss to follow-up was zero. The other indicators were similar to those of the Lighthouse.
More recent experience is now available from a study at QECH90. A total of 422 (59%) of the patients who started ART since 2000 were lost to follow-up. The 176 patients enrolled in the study had good virological and excellent clinical treatment results. The most common side effect was peripheral neuropathy. Nevirapine plasma levels were remarkably high and associated with successful virological treatment results. Two simple adherence questions pertaining to the use of medication in the previous 8 days corresponded well with nevirapine levels. The most important reasons for non-adherence were shortage of drugs in the hospital pharmacy and personal financial constraints.
Behavioural interventions
Voluntary Counselling and Testing (VCT)
VCT for HIV has been shown to be a cost effective intervention to reduce HIV transmission in Africa.91,92 The benefits are numerous: people who find out they are HIV-negative can take actions to remain uninfected, e.g. persuading their partner to go for testing or using condoms. Individuals who test positive can protect their partner from becoming infected, can protect themselves from becoming re-infected and mothers can take steps to avoid mother to child transmission. Access to preventive and life prolonging therapy such as cotrimoxazole prophylaxis and antiretroviral therapy are added benefits of VCT. The family of a HIV positive person may better plan for the future, both financially and in terms of child care and division of property. Knowing that someone is HIV positive may reduce the family's spending on health care and traditional healer services to find out what is wrong with the person. Finally, people living with HIV can help relatives, neighbours and policy makers to acknowledge the reality of the epidemic and decrease stigma, denial and fear.
In 2000, Zachariah and colleagues investigated the motives for going for VCT at the district hospital based VCT centre in Thyolo district.93 The most common reason for seeking VCT was recent knowledge about HIV/AIDS and the wish to know their HIV status (50%), repeated illness and suspicion of AIDS (18%) and suspicion that a partner had practiced unprotected sex outside the current relationship (11%). Seventy-seven percent of people coming for VCT had been encouraged by others who had undergone VCT.
According to the NAC annual HIV/AIDS M&E report, VCT services were available at 70 sites throughout the country, which provided VCT to 86,631 clients in 2003. However, none of the districts had VCT available as per national guidelines (every 8 kms in rural areas, and 1 site for every 10,000 people in urban areas).94 These data are still incomplete, because only 34% of all institutions trained on using the NAC M&E system had submitted reports from 2003. More detailed data on VCT are available from MACRO, which offers VCT in stand-alone centres in Blantyre, Lilongwe and Mzuzu. From Oct 2002 – Sep 2003 51,178 clients came for VCT and from Oct 2003–Sep 2004 the uptake dropped to 46,286. This group going for VCT was a highly selected one. Sixty-six percent of clients were between 15 and 29 years old, less than one third were women, one quarter had at least secondary school education and 64% were either never married or were separated, divorced or widowed. The majority had paid jobs.
Peer education programmes
In 1990 peer educator training was done among sex workers in Dedza town. The peer educators were trained for 4 days to give information about HIV/AIDS, to promote and distribute condoms and to teach safe sex negotiation skills. After 4 months, correct condom use had increased from 19% to 68% and ever condom use from 67% to 100%. The intervention was then upscaled to most districts in Malawi and involved training of 1183 sex workers and 458 truck drivers (their potential clients) as peer educators by end 1992. An evaluation years later showed that the presence of active peer educators among CSW had led to an increase in condom use with paying partners (90% compared to 76%). The truck driver peer educators were generally inactive, but companies where training had occurred were more likely to encourage and distribute condoms.49
Social interventions
Social marketing of condoms
PSI is the main social marketing organisation that supplies condoms in Malawi, called Chisango. Recently also BLM launched a new condom brand, Manyuchi. Apart from the approximately 9 million condoms sold through social marketing in 2004, another 28 million were distributed through the public sector.95
Summary : Interventions for HIV/AIDS in Malawi.
Biological
Circumcision may reduce risk of transmission
Treatment of STIs, which are common, will reduce transmission
Prevention of needlestick injuries should be universal for health sector staff
Cotrimoxazole is effective at reducing mortality and probably is cost-effective
ART has huge potential and pitfalls
Vaginal microbicides are not yet on the market but are being tested in Malawi
Behaviour and social
Changing behaviour and cultural practices remains the long term solution
Accessibility to VCT is not yet sufficient
Social marketing of behaviour change
Behaviour change to prevent STIs, including HIV, and unwanted pregnancy is marketed through PSI's Youth Alert! Programme. It teaches young people between 10 and 20 life skills to enable them to make informed choices about how to protect their health and achieve their goals in life. The main components are secondary school visits and a radio show (Youth Alert Mix!) with listeners' clubs. Until mid 2004 all secondary schools were visited at least once, reaching 62,000 students and 1,500 teachers. Youth Alert! Mix has quickly become the top-rated radio program among the youth in Malawi.95
Special clinics for prostitutes
All workers at public locations offering food, drinks or accommodation are required to produce a valid medical clearance certificate monthly at the communal police or on request. However, special outreach or mobile clinics do not exist countrywide.
Training for traditional healers
A one day course for Malawian traditional healers encouraged them to counsel STD patients about HIV/AIDS risks, conduct community education activities, talk with other healers regarding HIV/AIDS and distribute condoms to clients.96
Workplace policy and implementation of HIV interventions
Some evidence exists that HIV interventions such as treatment for STIs, condom distribution and VCT services can be effectively implemented in the context of a workplace programme.97 A survey among 20 companies in Malawi, ranging in size from 20 – 22,500 employees, showed that the majority provided core packages of prevention services with some basic care and support elements. However, there was a lack of established coordination mechanisms, existing workplace policies and involvement of senior management outside of the traditional human resource and health portfolios. None provided ARV treatment.98 This is now changing with active participation of the private and public sector encouraged by the NAC.
Table 8.
New HIV Infections
| Months | 0 – 3 | 4 – 12 | 13 – 21 | Total |
| Intervention (circumcised) |
2 | 7 | 9 | 18 |
| Control (uncircumcised) |
9 | 15 | 27 | 51 |
| Total | 11 | 22 | 36 | 69 |
References
- 1.Coombes Y. A literature review to support the Situational Analysis for the National Behaviour Change Interventions Strategy on HIV/AIDS and Sexual and Reproductive Health. Lilongwe: 2001. Sexual and reproductive health behaviours in Malawi. [Google Scholar]
- 2.Wilson D, Naidoo S, Bekker L, Cotton M, Maartens G, editors. Handbook of HIV medicine. Oxford: Oxford University Press Southern Africa; 2002. [Google Scholar]
- 3.McCormack GP, Glynn JR, Crampin AC, et al. Early evolution of the human immunodeficiency virus type 1 subtype C epidemic in rural Malawi. J Vir. 2002;76:12890–12899. doi: 10.1128/JVI.76.24.12890-12899.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taha TE, Dallabetta GA, Hoover DR, et al. Trends of HIV-1 and STD among pregnant and postpartum women in urban Malawi. AIDS. 1998;12:197–203. doi: 10.1097/00002030-199802000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Kumwenda NI, Taha TE, Hoover DR, et al. HIV-1 incidence among male workers at a sugar estate in rural Malawi. JAIDS. 2001;27:202–208. doi: 10.1097/00126334-200106010-00016. [DOI] [PubMed] [Google Scholar]
- 6.Pilcher CD, Price MA, Hoffman IF, et al. Frequent detection of acute primary HIV infection in men in Malawi. AIDS. 2004;18:517–524. doi: 10.1097/00002030-200402200-00019. [DOI] [PubMed] [Google Scholar]
- 7.Glynn JR, Buvé A, Caraël M, et al. Factors influencing the difference in HIV prevalence between antenatal clinic and general population in sub-Saharan Africa. AIDS. 2001;15:1717–1725. doi: 10.1097/00002030-200109070-00016. [DOI] [PubMed] [Google Scholar]
- 8.Crampin AC, Glynn JR, Ngwira BMM, et al. Trends and measurement of HIV prevalence in northern Malawi. AIDS. 2003;17:1817–1825. doi: 10.1097/00002030-200308150-00011. [DOI] [PubMed] [Google Scholar]
- 9.Jahn A, Ngwira L, Chisambo V, Crampin A. HIV prevalence and risks in women who do not attend antenatal clinic; National HIV/AIDS Research Dissemination Meeting; May 2004; Lilongwe, Malawi. [Google Scholar]
- 10.van Oosterhout JJ, Laufer MK, Graham SM, et al. A Community-Based Study of the Incidence of Trimethoprim-Sulfamethoxazole-Preventable Infections in Malawian Adults Living With HIV. J Acquir Immune Defic Syndr. 2005;39:626–631. [PubMed] [Google Scholar]
- 11.Kumwenda JJ, Mateyu G, Kampondeni S, van Dam AP, van Lieshout L, Zijlstra EE. Differential Diagnosis of Stroke in a Setting of High HIV Prevalence in Blantyre, Malawi. Stroke. 2005;36:960–964. doi: 10.1161/01.STR.0000162585.97216.ef. [DOI] [PubMed] [Google Scholar]
- 12.Muzyka BC, Kamwendo L, Mbweza E, et al. Prevalence of HIV-1 and oral lesions in pregnant women in rural Malawi. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:56–61. doi: 10.1067/moe.2001.112542. [DOI] [PubMed] [Google Scholar]
- 13.Beare NAV, Kublin JG, Lewis DK, et al. Ocular disease in patients with tuberculosis and HIV presenting with fever in Africa. Br J Ophtalmol. 2002;86:1076–1079. doi: 10.1136/bjo.86.10.1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gordon MA, Banda HT, Gondwe M, et al. Non-typhoidal salmonella bacteraemia among HIV-infected Malawian adults: high mortality and frequent recrudescence. AIDS. 2002;6:1633–1641. doi: 10.1097/00002030-200208160-00009. [DOI] [PubMed] [Google Scholar]
- 15.Gordon SB, Chaponda M, Walsh AL, et al. Pneumococcal disease in HIV infected Malawian adults: acute mortality and long-term survival. AIDS. 2002;16:1409–1417. doi: 10.1097/00002030-200207050-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gray RH, Wawer MJ, Brookmeyer R, et al. Probability of HIV-1 transmission per coital act in monogamous, heterosexual, HIV-1-discordant couples in Rakai, Uganda. Lancet. 2001;357:1149–1153. doi: 10.1016/S0140-6736(00)04331-2. [DOI] [PubMed] [Google Scholar]
- 17.Dallabetta GA, Miotti PG, Chiphangwi JD, et al. High socioeconomic status is a risk factor for human immunodeficiency virus type 1 (HIV-1) infection but not for sexually transmitted diseases in women in Malawi: implications for HIV-1 control. JID. 1993;167:36–42. doi: 10.1093/infdis/167.1.36. [DOI] [PubMed] [Google Scholar]
- 18.Sutcliffe S, Taha TE, Kumwenda NI, Taylor E, Liomba G. HIV-1 prevalence and herpes simplex virus 2, hepatitis C virus, and hepatitis B virus infections among male workers at a sugar estate in Malawi. JAIDS. 2002;31:90–97. doi: 10.1097/00126334-200209010-00012. [DOI] [PubMed] [Google Scholar]
- 19.Behets FMT, Liomba G, Lule G, et al. Sexually transmitted diseases and HIV control in Malawi: a field study of genital ulcer disease. JID. 1995;171:451–455. doi: 10.1093/infdis/171.2.451. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization, author. Nutrient requirements for people living with HIV / AIDS. Report of a technical consultation. Geneva: World Health Organization; 2003. [Google Scholar]
- 21.Fawzi WW, Msamanga GI, Spiegelman D, et al. A randomized trial of multivitamin supplements and HIV disease progression and mortality. N Engl J Med. 2004;351(1):23–32. doi: 10.1056/NEJMoa040541. [DOI] [PubMed] [Google Scholar]
- 22.Jiamton S, Pepin J, Suttent R, et al. A randomized trial of the impact of multiple micronutrient supplementation on mortality among HIV-infected individuals living in Bangkok. AIDS. 2003;17:2461–2469. doi: 10.1097/00002030-200311210-00008. [DOI] [PubMed] [Google Scholar]
- 23.Cardo DM, Culver DH, Ciesielski CA, et al. A case-control study of HIV seroconversion in health care workers after percutaneous exposure. N Engl J Med. 1997;337:1485–1490. doi: 10.1056/NEJM199711203372101. [DOI] [PubMed] [Google Scholar]
- 24. http://www.who.int/occupational_health/topics/needinjuries/en/index.html.
- 25.van Oosterhout JJ, Nyirenda M. Post exposure prophylaxis (PEP) for HIV in Queen Elizabeth Central Hospital, Blantyre; National HIV and AIDS Dissemination Conference (Abstract); 2005. [Google Scholar]
- 26.Hosseinipour MC, Joaki G, Gama S, et al. The effect of treating helminth infections on HIV; National HIV/AIDS Research Dissemination Meeting; May 2004; Lilongwe, Malawi. [Google Scholar]
- 27.Kublin JG, Patnaik P, Jere CS, et al. Effect of Plasmodium falciparum malaria on concentration of HIV-1-RNA in the blood of adults in rural Malawi: a prospective cohort study. Lancet. 2005;365:233–240. doi: 10.1016/S0140-6736(05)17743-5. [DOI] [PubMed] [Google Scholar]
- 28.McAuliffe E, Ntata P. Baseline survey in Lilongwe and Blantyre Districts for HIV/AIDS prevention through information and education for youth in Malawi. Zomba: Centre for Social Research; 1994. [Google Scholar]
- 29.Bisika T, Ntata P. Youth and AIDS: follow-up mini-KAPB survey in Blantyre, Lilongwe and Mzuzu. Zomba: Centre for Social Research; 1997. [Google Scholar]
- 30.Ekridge P, Gombar A, Nazombe J. Baseline Survey: Youth AIDS project in Salima. Salima: Care and Concern Youth Network; 1997. [Google Scholar]
- 31.Hickey C. Factors Explaining Observed Patterns of Sexual Behaviours, Phase I: Mchinji District Profile Social Research. 1997 [Google Scholar]
- 32.Kachingwe SI, Umar E, Madalazi P, Jere D, Chizimba E. Voluntary counselling and confidential testing. Lilongwe: Ministry of Health and Population; 2001. [Google Scholar]
- 33.Bisika T, Kakhongwe P. Research on HIV/AIDS, STDs and skin disease in Malawi. A literature review. Zomba: Centre for Social Research; 1995. [Google Scholar]
- 34.Ministry of Education, Sports and Culture (MOESC), author Sexuality and Reproductive Health Education for primary schools in Malawi. Lilongwe: Ministry of Education, Science and Technology; 2000. [Google Scholar]
- 35.Save the Children. A situation analysis of young peoples' access to utilization of and need for reproductive health services in Traditional Authority Zulu, Mchinji district. 2000
- 36.Tsoka MG. Analysis of the HIV/AIDS epidemic and the high population growth in Malawi. Zomba: Centre for Social Research; 1999. [Google Scholar]
- 37.Kumwenda NI, Taha TE, Hoover DR, et al. Three surveys of HIV-1 prevalence and risk factors among men working at a sugar estate in Malawi. Sex Transm Dis. 2002;29:366–371. doi: 10.1097/00007435-200206000-00010. [DOI] [PubMed] [Google Scholar]
- 38.Smith KP, Watkins SC. Perceptions of risk and strategies for prevention: responses to HIV/AIDS in rural Malawi. Soc Science Med. 2005;60(3):649–660. doi: 10.1016/j.socscimed.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 39.Watkins SC. Navigating the AIDS Epidemic in Rural Malawi. Population and Development Review. 2004;30:673. [Google Scholar]
- 40.Kaler A. AIDS talk in everyday life: the presence of HIV/AIDS in men's informal conversation in Southern Malawi. Soc Science Med. 2004;59:285–297. doi: 10.1016/j.socscimed.2003.10.023. [DOI] [PubMed] [Google Scholar]
- 41.National Statistical Office [Malawi] and ORC Macro, author. Malawi Demographic and Health Survey 2000. Zomba, Malawi and Calverton, Maryland, USA: National Statistical Office and ORC Macro; 2001. [Google Scholar]
- 42.Maluwa-Banda D. Baseline survey report on the sexual and reproductive health programme for out-of-school young people. Lilongwe: Department of Youth, National Youth Council of Malawi and UNFPA; 2001. [Google Scholar]
- 43.National Statistics Office, Zomba, Malawi, author. 1996 Malawi Knowledge, Attitudes and Practices in Health Survey (MKAPH) Zomba: NSO; 1997. Macro International. [Google Scholar]
- 44.Zachariah R, Spielmann MP, Harries AD, Nkhoma W, Chantulo A, Arendt V. Sexually transmitted infections and sexual behaviour among commercial sex workers in a rural district of Malawi. Int J STD AIDS. 2003;14:185–188. doi: 10.1258/095646203762869197. [DOI] [PubMed] [Google Scholar]
- 45.Malawi AIDS Counseling and Resource Organization, author. USAID Oct 2002–Sep 2003 Report. Lilongwe: 2004. [Google Scholar]
- 46.Malawi AIDS Counseling and Resource Organization, author. USAID Oct 2003–Sep 2004 Report. Lilongwe: 2004. [Google Scholar]
- 47.Weller S, Davis K. The Cochrane Library. 4. Chichester, UK: John Wiley & Sons, Ltd.; 2003. Condom effectiveness in reducing heterosexual HIV transmission (Cochrane Review) p. CD003255. [DOI] [PubMed] [Google Scholar]
- 48.Taha TE, Canner JK, Chiphangwi JP, et al. Reported condom use is not associated with incidence of sexually transmitted diseases in Malawi. AIDS. 1996;10:207–212. doi: 10.1097/00002030-199602000-00012. [DOI] [PubMed] [Google Scholar]
- 49.Walden VM, Mwaungulu K, Makhumula-Nkhoma P. Measuring the impact of a behaviour change intervention for commercial sex workers and their potential clients in Malawi. Health Educ Research. 1999;14:545–554. doi: 10.1093/her/14.4.545. [DOI] [PubMed] [Google Scholar]
- 50.Shea RO, Johnson K. DHS Comparative Reports No. 6, 2004. Calverton, Maryland: ORC Macro; The DHS Wealth Index. [Google Scholar]
- 51. http://siteresources.worldbank.org?INTPAH/Resources/Publications/Quantitative-Techniques/health_eq_tn07.pdf.
- 52.Hargreaves JR, Glynn JR. Educational attainment and HIV-1 infection in developing countries: a systematic review. Trop Med Int Health. 2002;7:489–498. doi: 10.1046/j.1365-3156.2002.00889.x. [DOI] [PubMed] [Google Scholar]
- 53.Slutsker L, Cabeza J, Wirima JJ, Steketee RW. HIV-1 infection among women of reproductive age in a rural district in Malawi. AIDS. 1994;8:1337–1340. doi: 10.1097/00002030-199409000-00019. [DOI] [PubMed] [Google Scholar]
- 54.Glynn JR, Carael M, Buve A, et al. Does increased general schooling protect against HIV infection? A study in four African cities. Trop Med Int Health. 2004;9:4–14. doi: 10.1046/j.1365-3156.2003.01168.x. [DOI] [PubMed] [Google Scholar]
- 55.Crampin AC, Floyd S, Glynn JR, et al. Long-term follow-up of HIV-positive and HIV-negative individuals in rural Malawi. AIDS. 2002;16:1545–1550. doi: 10.1097/00002030-200207260-00012. [DOI] [PubMed] [Google Scholar]
- 56.Mathers CD, Bernard C, Moesgaard Iburg C, et al. Global Programme on Evidence for Health Policy Discussion Paper No. 54. World Health Organization; 2003. Dec, Global Burden of Disease in 2002: data sources, methods and results. (revised February 2004) [Google Scholar]
- 57.Hunter S, Williamson J. Children on the brink. Executive summary. Updated estimates and recommendations for intrevention. Washington, DC: USAID; 1997. [Google Scholar]
- 58.Crampin AC, Floyd S, Glynn JR, et al. The long-term impact of HIV and orphanhood on the mortality and physical well-being of children in rural Malawi. AIDS. 2003;17:389–397. doi: 10.1097/00002030-200302140-00013. [DOI] [PubMed] [Google Scholar]
- 59.Bollinger L, Palamuleni ME. The economic impact of AIDS in Malawi. The Futures Group International; 2000. Aug, place of publication not indicated. [Google Scholar]
- 60.Mtika M. Illness, deaths and social obligations: peasant food security in the context of AIDS in Malawi. Int Conf AIDS. 1998;12:472. (abstract no. 24159). Cited in Bollinger L & Palamuleni ME, August 2000. [Google Scholar]
- 61.Munthali SM. Socio/economic impact of HIV-AIDS in Malawi: Focus Group Discussions on community impacts and coping strategies. OATUU Health Safety and Environment Programme. 1998 Cited in Bollinger L & Palamuleni ME, August 2000. [Google Scholar]
- 62.Grant W. Effects of HIV/AIDS on micro-and small enterprises: lessons from Malawi. AIDS Analysis Africa. 2002;12:10–11. [Google Scholar]
- 63.Jones C. What HIV cost a tea estate in Malawi. AIDS Analysis Africa. 1997;7:5–7. [PubMed] [Google Scholar]
- 64.Jones C. Brown and Clapperton Limited: the cost implications of HIV/AIDS. JSI-STAFF Project, Lilongwe, Malawi. 1996 Cited in Bollinger L & Palamuleni ME, August 2000. [Google Scholar]
- 65.Ntirenda C, Zimba D. The impact of HIV/AIDS on production: the experience with Lonrho Companies, Malawi. Int Conf AIDS. 1998 Cited in Bollinger L & Palamuleni ME, August 2000. [Google Scholar]
- 66.UNDP and Government of Malawi, author. The impact of HIV/AIDS on human resources in the Malawi Public Sector. Lilongwe: 2002. Feb, [Google Scholar]
- 67.Harries AD, Hargreaves NJ, Gausi F, Kwanjana JH, Salaniponi FM. High death rates in health care workers and teachers in Malawi. Trans Roy Soc Trop Med Hyg. 1996:34–37. doi: 10.1016/s0035-9203(02)90231-2. [DOI] [PubMed] [Google Scholar]
- 68.Siegfried N, Muller M, Volmink J, et al. The Cochrane Library. 4. Chichester, UK: John Wiley & Sons, Ltd; 2003. Male circumcision for prevention of heterosexual acquisition of HIV in men (Cochrane Review) p. CD003362. [DOI] [PubMed] [Google Scholar]
- 69.Cohen J. AIDS research. Male circumcision thwarts HIV infection. Science. 2005;309(5736):860. doi: 10.1126/science.309.5736.860. [DOI] [PubMed] [Google Scholar]
- 70.Wilkinson D, Rutherford G. The Cochrane Library. 4. Chichester, UK: John Wiley & Sons, Ltd.; 2003. Population-based interventions for reducing sexually transmitted infections, including HIV infection (Cochrane Review) p. CD001220. [DOI] [PubMed] [Google Scholar]
- 71.Bowie C, Alinafe L, Marsh R, Misiri H, Cleary P, Bowie CT. An assessment of food supplementation to chronically sick patients receiving home based care in Bangwe, Malawi: a descriptive study. Nutr J. 2005;4:12. doi: 10.1186/1475-2891-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fawzie WW, Msamanga GI, Spiegelman D, et al. A randomized trial of multivitamin supplements and HIV disease progression and mortality. N Engl J Med. 2004;351:23–32. doi: 10.1056/NEJMoa040541. [DOI] [PubMed] [Google Scholar]
- 73.The Public Health Working Group of the Microbicide Initaitive, author. The public health benefits of microbicides in lower-income countries. Model Projections. New York, year not specified. Available from: http://www.global-campaign.org/clientfiles/rep7_publichealth.pdf.
- 74.Wilkinson D, Ramjee G, Tholandi M, Rutherford G. The Cochrane Library. 4. 2003. Nonoxynol-9 for preventing vaginal acquisition of HIV infection by women from men (Cochrane Review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.van De Wijgert J, Fullem A, Kelly C, et al. Phase 1 trial of the topical microbicide BufferGel: safety results from four international sites. J Acquir Immune Defic Syndr. 2001;26:21–27. doi: 10.1097/00126334-200101010-00003. [DOI] [PubMed] [Google Scholar]
- 76.Wiktor SZ, Sassan-Morokro M, Grant AD, et al. Efficacy of trimethoprim-sulfamethoxazole profylaxis to decrease morbidity and mortality in HIV-1-infected patients with tuberculosis in Abidjan, Côte d'Ivoire: a randomised controlled trial. Lancet. 1999;353:1469–1475. doi: 10.1016/s0140-6736(99)03465-0. [DOI] [PubMed] [Google Scholar]
- 77.Anglaret X, Chene G, Attia A, et al. Early chemoprofylaxis with trimethoprim-sulfamethoxazole for HIV-1-infected adlts in Abidjan, Côte d'Ivoire: a randomised trial. Cotrimo-C1 Study Group. Lancet. 1999;353:1463–1468. doi: 10.1016/s0140-6736(98)07399-1. [DOI] [PubMed] [Google Scholar]
- 78.WHO/UNAIDS, author. Provisional WHO/UNAIDS recommendations on the use of cotrimoxazole prophylaxis in adults and children living with HIV/AIDS in Africa. Geneva: UNAIDS; 2000. [Google Scholar]
- 79.Pitman C, Amali R, Kanyerere H, et al. Bloody diarrhoea of adults in Malawi: clinical features, infectious agents, and antimicrobial sensitivities. Trans R Soc Trop Med Hyg. 1996;90:284–287. doi: 10.1016/s0035-9203(96)90251-5. [DOI] [PubMed] [Google Scholar]
- 80.Walsh AM, Phiri AJ, Graham SM, Molyneux EM, Molyneux ME. Bacteraemia in febrile Malawian children: clinical and microbiological features. Pediatr Inf Dis. 2000;19:312–318. doi: 10.1097/00006454-200004000-00010. [DOI] [PubMed] [Google Scholar]
- 81.Zachariah R, Harries AD, Arendt V, et al. Compliance with cotrimoxazole prophylaxis for the prevention of opportunistic infections in HIV-positive tuberculosis patients in Thyolo district, Malawi. Int J Tuberc Lung Dis. 2001;5:843–846. [PubMed] [Google Scholar]
- 82.Zachariah R, Spielmann MP, Harries AD, Gomani P, Bakali E. Cotrimoxazole prophylaxis in HIV-infected individuals after completing anti-tuberculosis treatment in Thyolo, Malawi. Int J Tuberc Lung Dis. 2002;6:1046–1050. [PubMed] [Google Scholar]
- 83.Chimzizi RB, Harries AD, Manda E, Khonyongwa A, Salaniponi FM. Counselling HIV testing and adjunctive cotrimoxazole for TB patients in Malawi: from research to routine implementation. Int J Tuberc Lung Dis. 2004;8:938–944. [PubMed] [Google Scholar]
- 84.Zachariah R, Harries AD, Spielmann MP, et al. Changes in Escherichia coli resistance to co-trimoxazole in tuberculosis patients and in relation to co-trimoxazole prophylaxis in Thyolo, Malawi. Trans R Soc Trop Med Hyg. 2002;96:202–204. doi: 10.1016/s0035-9203(02)90306-8. [DOI] [PubMed] [Google Scholar]
- 85.Ministry of Health and National Aids Commission, author. Guidelines for the use of antiretroviral therapy in Malawi. Lilongwe: 2003. Oct, Treatment of AIDS. [Google Scholar]
- 86.Hosseinipour M, Neuhann F, Kanyama C, et al. Early mortality is the leading cause of loss to follow-up among antiretroviral clinic patients in Lilongwe, Malawi; National HIV/AIDS Research Dissemination Meeting; May 2004; Lilongwe, Malawi. [Google Scholar]
- 87.Neuhann F, Hosseinipour M, Nyireda J, et al. Fast track review of patients on ARV using a checklist in Lilongwe, Malawi; National HIV/AIDS Research Dissemination Meeting; 5–6 May 2004; Lilongwe, Malawi. [Google Scholar]
- 88.Hosseinipour M, Kanyama C, Nkhalamba T, et al. Safety and efficacy of D4T/3TC/NVP among HIV/AIDS positive adults in Lilongwe Malawi; National HIV/AIDS Research Dissemination Meeting; May 2004; Lilongwe, Malawi. [Google Scholar]
- 89.Harries AD, Gomani P, Teck R, et al. Monitoring the response to antiretroviral therapy in resource-poor settings: the Malawi model. Trans R Soc Trop Med Hyg. 2004;98:695–701. doi: 10.1016/j.trstmh.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 90.van Oosterhout JJ, Bodasing N, Kumwenda JJ, et al. Evaluation of antiretroviral therapy results in a resource-poor setting in Blantyre, Malawi. Trop Med Int Health. 2005;10:464–470. doi: 10.1111/j.1365-3156.2005.01409.x. [DOI] [PubMed] [Google Scholar]
- 91.The voluntary HIV-1 Counselling and Testing Efficacy Study Group, author. Efficacy of voluntary HIV-1 counselling and testing in individuals and couples in Kenya, Tanzania and Trinidad: a randomised trial. Lancet. 2000;356:103–112. [PubMed] [Google Scholar]
- 92.Sweat M, Gregorich S, Sangiwa G, et al. Cost-effectiveness of voluntary HIV-1 counseling and testing in reducing sexual transmission of HIV-1 in Kenya and Tanzania. Lancet. 2000;356:113–121. doi: 10.1016/S0140-6736(00)02447-8. [DOI] [PubMed] [Google Scholar]
- 93.Zachariah R, Spielmann MP, Harries AD, Salaniponi FL. Voluntary counselling, HIV testing and sexual behaviour among patients with tuberculosis in a rural district of Malawi. Int J Tuberc Lung Dis. 2003;7:65–71. [PubMed] [Google Scholar]
- 94.Malawi National AIDS Commission, author. Annual HIV and AIDS monitoring and Evaluation Report 2003. Lilongwe: 2004. [Google Scholar]
- 95.Danart A, Mackie W, Cisek C, Kondoole N, Chizani N. Midterm evaluation of Population Services International's improving health hrough social marketing project. LTG Associates, Inc. and Social & Scientific Systems, Inc.; 2004. [No place specified] [Google Scholar]
- 96.Berger RA, Porter L, Mekisini G, Courtright P. Traditional healers in AIDS control. AIDS. 1994;8:1511–1512. doi: 10.1097/00002030-199410000-00028. [DOI] [PubMed] [Google Scholar]
- 97.Rosen S, Simon JL, Thea DM, Vincent JR. Care and treatment te extend the working lives of HIV positive employees: calculating the benefits to business. South Afr J Science. 2000;96:6. [Google Scholar]
- 98.Morris CN. Workplace HIV policy and interventions in Malawi: results of a nationwide survey. AIDS Analysis Africa. 2003;13:14–15. [Google Scholar]
- 99.Chiphangwi J, Liomba G, Ntaba HM, et al. Human immunodeficiency virus infection is prevalent in Malawi. Infection. 1987;15:363. doi: 10.1007/BF01647741. [DOI] [PubMed] [Google Scholar]
- 100.Miotti PG, Dallabetta G, Ndovi E, Liomba G, Saah AJ, Chiphangwi J. HIV-1 and pregnant women: associated factors, prevalence, estimate of incidence and role in fetal wastage in central Africa. AIDS. 1990;4:733–736. [PubMed] [Google Scholar]
- 101.Lan Y, Kumwenda N, Taha TE, et al. Carotenoid status of pregnant women with and without HIV infection in Malawi. East Afr Med J. 1999;76:133–137. [PubMed] [Google Scholar]
- 102.Ahmed SD, Cuevas LE, Brabin BJ, et al. Seroprevalence of hepatitis B and C and HIV in Malawian pregnant women. J Inf. 1998;37:248–251. doi: 10.1016/s0163-4453(98)91983-1. [DOI] [PubMed] [Google Scholar]
- 103.Glynn JR, Ponnighaus J, Crampin AC, et al. The development of the HIV epidemic in Karonga District, Malawi. AIDS. 2001;15:2025–2029. doi: 10.1097/00002030-200110190-00016. [DOI] [PubMed] [Google Scholar]
- 104.Candotti D, Mundy C, Kadewele G, Nkhoma W, Bates I, Allain JP. Serological and molecular screening for viruses in blood donors from Ntcheu, Malawi: high prevalence of HI-1 subtype C and of markers of hepatitis B and C viruses. J Med Vir. 2001;65:1–5. [PubMed] [Google Scholar]
- 105.Medecins Sans Frontieres France, author. Chiradzulu District HIV/AIDS program, year 2001. Blantyre: 2002. Feb, [Google Scholar]
- 106.Kristensen JK. The prevalence of symptomatic sexually transmitted diseases and human immunodeficiency virus infection in outpatients in Lilongwe, Malawi. Genitourin Med. 1990;66:244–246. doi: 10.1136/sti.66.4.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Waddell KM, Lewallen S, Lucas SB, Atenyi-Agaba C, Herrington CS, Liomba G. Carcinoma of the conjunctiva and HIV infection in Uganda and Malawi. Br J Ophtalmol. 1996;80:503–508. doi: 10.1136/bjo.80.6.503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Archibald LK, McDonald LC, Nwanyanwu O, et al. A hospital-based prevalence survey of bloodstream infections in febrile patients in Malawi: implications for diagnosis and therapy. JID. 2000;181:1414–1420. doi: 10.1086/315367. [DOI] [PubMed] [Google Scholar]
- 109.James J, Hofland HWC, Borgstein ES, Kumiponjera D, Komolafe OO, Zijlstra EE. The prevalence of HIV infection among burn patients in a burns unit in Malawi and its influence on outcome. Burns. 2003;29:55–60. doi: 10.1016/s0305-4179(02)00236-x. [DOI] [PubMed] [Google Scholar]
- 110.Kelly PM, Cumming RG, Kaldor JM, Irwig LM. A new, clinically based algorithm for the doagnosis of HIV in African tuberculosis patients: cross-sectional analysis from Mzuzu, Malawi. Int J STD AIDS. 1999;10:231–236. doi: 10.1258/0956462991913998. [DOI] [PubMed] [Google Scholar]
- 111.Harries AD, Maher D, Mvula B, Nyangulu D. An audit of HIV testing and HIV serostatus in tuberculosis patients, Blantyre, Malawi. Tuber Lung Dis. 1995;76:413–417. doi: 10.1016/0962-8479(95)90007-1. [DOI] [PubMed] [Google Scholar]
- 112.Harries AD, Nyangulu DS, Kangombe C, Ndalama D, Wirima JJ, Salaniponi FM, Liomba G, Maher D, Nunn P. The scourge of HIV-related tuberculosis: a cohort study in a district general hospital in Malawi. Ann Trop Med Parasitol. 1997;91:771–776. doi: 10.1080/00034989760527. [DOI] [PubMed] [Google Scholar]
- 113.Hargreaves NJ, Kadzakumanja O, Phiri S, et al. What causes smear-negative pulmonary tuberculosis in Malawi, an area of high HIV seroprevalence? Int J Tuberc Lung Dis. 2001;5:113–122. [PubMed] [Google Scholar]
- 114.Mwaungulu FBD, Floyd S, Crampin AC, et al. Cotrimoxazole prophylaxis reduces mortality in human immunodeficiency virus-positive tuberculosis patients in Karonga District, Malawi. Bull WHO. 2004;82:354–363. [PMC free article] [PubMed] [Google Scholar]
- 115.Zachariah R, Spielmann MPL, Chinji C, et al. Voluntary counselling, HIV testing and adjunctive cotrimoxazole reduces mortality in tuberculosis patients in Thyolo, Malawi. AIDS. 2003;17:1053–1061. doi: 10.1097/00002030-200305020-00015. [DOI] [PubMed] [Google Scholar]
- 116.Kwanjana JH, Harries AD, Salaniponi FML, Nyangulu DS, Gausi F. TB-HIV seroprevalence in patients with tuberculosis in Malawi; National HIV/AIDS Research Dissemination Meeting; 5–6 May 2004; Lilongwe, Malawi. [Google Scholar]
- 117.Zachariah R, Spielmann MP, Harries AD, Buhendwa L, Chingi C. Motives, sexual behaviour and risk factors associated with HIV in individuals seeking voluntary counselling and testing in a rural district in Malawi. Trop Doct. 2003;33:88–91. doi: 10.1177/004947550303300211. [DOI] [PubMed] [Google Scholar]
- 118.Bisika T, Konyani S, Chamangwana I, Khanyiriza G. The epidemiology of HIV among drug abusers in Thyolo district; National HIV/AIDS Research Dissemination Meeting; 5–6 May 2004; Lilongwe, Malawi. [Google Scholar]
- 119.Banerjee A, Harries AD, Mphasa N, Yadid AE, Nyirenda T, Salaniponi FM. Prevalence of HIV, sexually transmitted disease and tuberculosis amongst new prisoners in a district prison, Malawi. Trop Doct. 2000;30:49–50. doi: 10.1177/004947550003000124. [DOI] [PubMed] [Google Scholar]