Definition
Undernutrition denotes insufficient intake of energy and nutrients to meet an individual's needs to maintain good health. In most literature, undernutrition is used synonymously with malnutrition. In the strictest sense, malnutrition denotes both undernutrition and overnutrition. To overcome this, terms such as protein energy malnutrition, specific micronutrient deficiencies as well as other descriptive names such as kwashiorkor and marasmus have been used. However, since protein energy malnutrition does not exist in isolation of specific micronutrient deficiencies, neutral terms such as undernutrition are encouraged because they encompass both protein energy undernutrition as well as micronutrient deficiencies. Similarly overnutrition is used when there is excess intake of macronutrients and micronutrients. In the following pages undernutrition and malnutrition will be used interchangeably. Undernutrition will be discussed in terms of protein-energy undernutrition and those specific micronutrient deficiencies which are considered of public health significance in Malawi i.e. vitamin A, iron and iodine deficiency. Overnutrition which is not as prevalent as undernutrition in Malawi will not be addressed.
Undernutrition is defined as insufficient intake of energy and nutrients to meet an individual's needs to maintain good health.
Distribution of Undernutrition
Measures of undernutrition
There are several indicators used to measure nutritional status. These include body composition, clinical signs of deficiency, physical function, biochemical compounds, metabolic processes or dietary intake. The choice of which of these indicators is used is dependent on the question being asked. In clinical settings, it is common to use a combination of qualitative and quantitative descriptions of undernutrition e.g. marasmus and kwashiorkor while in community studies of protein-energy undernutrition, body size is widely used because it is readily measurable and is a sensitive indicator of nutritional status and health. However, for specific nutrient deficiencies other indicators are used. For example serum retinol level, a biochemical measure, can be used to measure vitamin A deficiency and a clinical feature e.g. xerophthalmia can also be used as a measure of vitamin A deficiency.
The commonly used anthropometric measures are weight and length (height)* in combination with age and sex. These measurements are used to construct indices and indicators** that are used to describe nutritional status of individuals or populations. Other measures of body composition that are used include various body circumferences (mid upper arm, head, chest, abdomen etc) and skin folds (biceps, triceps, sub-scapular etc).
Three basic indices are used in childhood: weight for age Z score (WAZ), length / height for age Z score (LAZ / HAZ) and weight for length / height Z score (WLZ / WHZ).
Weight for age: defined as weight of a child relative to the weight of a child of the same age in a reference population, expressed either as a Z score or a percentage relative to the median of the reference population. Qualitatively children who have low weight for age are described as being ‘underweight’.
Height for age (/ length for age): defined as height or length of a child relative to the length or height of a child of the same age in a reference population, expressed either as a Z score or a percentage relative to the median of the reference population. Qualitatively children who have low height for age are described as being ‘stunted’.
Weight for height (/ weight for length): defined as weight of a child relative to the weight of a child of the same height or length in a reference population, expressed either as a Z score*** or a percentage relative to the median of the reference population. Qualitatively children who have low weight for height are described as being ‘wasted’. Wasting is also sometimes called global undernutrition or global acute malnutrition (GAM). Table 1 shows how the indices are used to define undernutrition.
Table 1.
Waterlow classification of undernutrition
| Normal | Mild* | Moderate* | Severe* | ||
| Weight for height (wasting) |
%+ Z score |
90 – 120 2.0 to −0.99 |
80 – 89 −1 to −1.99 |
70 –79 −2.0 to −2.99 |
< 70% <−3.0 |
| Height for age | % | 95 – 110 | 90 – 94 | 85 – 89 | < 85 |
| (stunting) | Z score | 2.0 to −0.99 | −1.0 to −1.99 | −2.0 to −2.99 | < −3.0 |
Without oedema. Presence of oedema denotes severe malnutrition (kwashiorkor) even without severe wasting (Marasmus).
+ Percentage of the median World Health Organization (WHO) / United States National Centre for Health Statistics (NCHS) reference.
In adulthood, since they have stopped attaining height, indices of thinness are more appropriate. The indices used include Body Mass Index which is the weight (in kilograms) divided by the square of height (in meters). Additionally mid upper arm circumference is also used to measure wasting in both children and adults.
Incidence of undernutrition
Primary malnutrition is usually a disease of the dependent and the vulnerable that rely on others for their nutriture while secondary undernutrition accompanies any disease which disturbs appetite, digestion, absorption or utilization of nutrients 2. The vulnerable groups include children in utero and within the first 5 years of life, adolescents, pregnant/lactating women and the elderly. Because children are completely dependent on others for their nutriture they are especially vulnerable.
Within the first 5 years of life there are critical periods during which undernutrition occurs, and evidence suggest that this is different for the various forms of undernutrition. In most developing countries underweight and wasting tend to become evident between 4 and 6 months while stunting tends to appear as early as 2–3 months of age 3–9. The period of highest incidence of undernutrition being between 6 and 20 months, a period Mata 10 has described as' the valley of death', because of the high associated mortality during this period. Because undernutrition is evident at those ages it is logical to think that the problem starts much earlier than it manifests. For height this could be as early as in utero and shorter birth lengths have been documented in population studies from Malawi, but mean birth weights seem comparable to international reference standards 11. The notion that undernutrition starts in utero is also supported by the high incidence of intrauterine growth retardation-low birth weight (IUGR-LBW) estimated at about 15% in Malawi 12.
There is not much literature on population incidence of undernutrition in Malawi because most of the nutrition related data comes from cross sectional studies or hospital based studies. However, in a population based cohort study in a rural community on the eastern shore of Lake Malawi 10, a similar picture has been documented. The incidence of stunting peaked at 3 – 12 months, under-weight between 6–18 months, and wasting at 15–21 months. The incidence did not only vary by age but also by season whereby in the worst months, 8% of all previously normally nourished children developed low weight for age, 10% low height for age and 3% low weight for height. Thus stunting seems to occur earlier followed by underweight before wasting sets in.
Several reasons have been proposed for the observed high incidence of undernutrition during 6 to 18 month age period. The period coincides with the introduction of complementary feeding as breast milk becomes insufficient to meet the metabolic needs of the growing child. However, the complementary feeds in most developing countries such as Malawi are not energy dense or hygienic, resulting in reduced energy and nutrient intake and increased morbidity (especially diarrhoea), which leads to undernutrition 13, 10, 14, 15. Furthermore, during this period children are becoming more mobile and thus exposed to infections while at the same time the protection they had from maternal antibodies has waned and this leads to increased infectious diseases and ultimately to undernutrition. The high incidence of undernutrition in utero can be attributed to maternal undernutrition (see table 3) and low pregnancy weight gain coupled with maternal infections. In the population based cohort described above, mean post mid-pregnancy weight gain was only 259g/week 16.
Table 3.
Regional prevalence of undernutrition in children aged less than 5 years.
| % Underweight | % Stunted | % Wasted | |
| Asia | 42 (154) | 47 (173) | 11 (40) |
| Africa | 27 (32) | 39 (45) | 7 (8) |
| Malawi* | 30 | 49 | 7 |
| Latin America |
12 (7) | 22 (12) | 3 (2) |
| Oceania | 29(0.3) | 42 (0.4) | 6 (0.1) |
Figures in parenthesis represent absolute numbers of children in millions Source de Onis et al. 2000.
Source UNICEF. 2002.
Prevalence of undernutrition
Prevalence of protein-energy undernutrition
Malawi has one of the highest prevalence of protein-energy undernutrition in the world. 30% of under five year old children are underweight, 49% are stunted and 7 are wasted 17. The ages of peak prevalence are usually at 12 months for underweight and stunting while wasting peaks at 18 months. Table 3 shows the prevalence of undernutrition in Malawi compared to other regions of the world and Table 4 shows the prevalence of undernutrition in pre-school children, school children and women.
Table 4.
Nutritional status of children and women by demographic factors (Malawi DHS 2000)
| HAZ | WHZ | WAZ | Women | Height | BMI | |||||||
| Age | <−3.0 | <−2.0 | <−3.0 | <−2.0 | <−3.0 | <−2.0 | Mean | % < 145 | % < 18.5 | % > 25.0 | ||
| < 6 months | 3.0 | 11.4 | 1.3 | 5.8 | 1.3 | 5.9 | 15 – 19 | 154.5 | 4.9 | 16.6 | 5.3 | |
| 6 – 9 | 10.2 | 26.4 | 2.0 | 8.9 | 5.0 | 23.9 | 20 – 24 | 155.9 | 2.7 | 6.7 | 9.5 | |
| 10 – 11 | 13.4 | 31.8 | 2.7 | 10.3 | 6.5 | 29.1 | 25 – 29 | 155.9 | 2.6 | 6.0 | 13.2 | |
| 12 – 15 | 21.4 | 46.5 | 1.6 | 13.0 | 11.4 | 38.9 | 30 – 34 | 156.6 | 2.1 | 7.2 | 13.4 | |
| 16 – 23 | 34.0 | 64.0 | 1.9 | 8.2 | 8.4 | 35.3 | 35 – 39 | 156.1 | 2.1 | 5.6 | 19.3 | |
| 24 – 35 | 29.4 | 55.6 | 1.1 | 4.8 | 8.8 | 31.1 | 40 – 44 | 156.2 | 2.6 | 6.1 | 17.8 | |
| 36 – 47 | 30.8 | 59.1 | 0.7 | 2.1 | 3.4 | 21.3 | 45 – 49 | 156.2 | 2.0 | 8.3 | 13.4 | |
| 48 – 59 | 27.6 | 57.4 | 0.6 | 1.5 | 3.5 | 20.5 | ||||||
| Sex | Residence | |||||||||||
| male | 25.8 | 50.5 | 1.2 | 5.1 | 6.0 | 25.7 | Urban | 157.0 | 1.9 | 5.5 | 23.4 | |
| female | 23.0 | 47.6 | 1.3 | 6.0 | 5.7 | 25.1 | Rural | 155.5 | 3.2 | 9.4 | 9.5 | |
| Residence | ||||||||||||
| Urban | 13.5 | 34.2 | 0.9 | 4.9 | 1.4 | 12.8 | Region | |||||
| Rural | 26.1 | 51.2 | 1.3 | 5.6 | 6.5 | 27.3 | Northern | 155.3 | 3.6 | 7.5 | 10.1 | |
| Region | Central | 156.1 | 2.5 | 7.7 | 12.0 | |||||||
| North | 16.2 | 39.0 | 1.0 | 4.7 | 3.4 | 17.4 | Southern | 155.5 | 3.3 | 9.9 | 12.1 | |
| Centre | 30.2 | 55.5 | 1.2 | 5.0 | 6.7 | 27.9 | ||||||
| South | 20.9 | 45.3 | 1.3 | 6.2 | 5.7 | 25.0 | Districts | |||||
| Districts | Blantyre | 157.0 | 1.6 | 6.5 | 22.8 | |||||||
| Blantyre | 13.5 | 38.1 | 1.2 | 6.7 | 3.8 | 18.0 | Karonga | 155.7 | 4.3 | 8.0 | 12.0 | |
| Karonga | 14.6 | 38.8 | 0.4 | 5.2 | 3.1 | 16.0 | Kasungu | 156.2 | 2.8 | 8.2 | 13.2 | |
| Kasungu | 20.9 | 47.4 | 0.6 | 2.7 | 2.8 | 20.7 | Lilongwe | 156.7 | 1.4 | 5.1 | 15.6 | |
| Lilongwe | 31.6 | 54.2 | 1.6 | 5.9 | 7.2 | 27.6 | Mangochi | 154.7 | 4.4 | 9.7 | 11.0 | |
| Mangochi | 24.2 | 47.5 | 1.1 | 5.7 | 8.5 | 28.8 | Mulanje | 154.8 | 3.7 | 12.8 | 9.2 | |
| Mulanje | 26.1 | 49.5 | 1.1 | 4.0 | 5.2 | 27.7 | Mzimba | 155.4 | 2.9 | 7.8 | 9.8 | |
| Mzimba | 17.8 | 43.9 | 1.1 | 4.0 | 3.3 | 18.7 | Salima | 155.4 | 3.4 | 12.3 | 7.8 | |
| Salima | 25.6 | 54.6 | 1.8 | 5.7 | 8.8 | 29.0 | Thyolo | 155.0 | 4.1 | 10.9 | 7.7 | |
| Thyolo | 23.2 | 46.3 | 1.0 | 4.5 | 5.5 | 25.9 | Zomba | 155.5 | 2.9 | 8.4 | 10.4 | |
| Zomba | 21.4 | 45.7 | 2.4 | 7.7 | 7.8 | 24.6 |
Prevalence of Micronutrient deficiencies
Iron deficiency
Iron deficiency is the commonest nutritional deficiency in the world and in Malawi. Four to five billion people may be deficient (66–80% of the world's population) and 2 billion are anaemic (30%) while in developing countries it estimated that 9 in 10 are affected. National estimates from a 2001 micronutrient survey 18 indicated that the prevalence of anaemia by haemoglobin is 80% in preschool children, 27% in pregnant women, 22% in school children, and 17% in men. Iron deficiency as measured by transferrin receptor (TfR) and zinc protoprophyrin (ZP) is also very prevalent (Table 6). Overall, 58% of preschool children have iron deficiency anaemia (IDA) by Hb & ZP and 59% have IDA by Hb & TfR. In school children, IDA is found in 7% by the Hb & ZP indicator and in 10% by the Hb & TfR indicator. In non-pregnant women, IDA is 10% by Hb & ZP and 11% by Hb & TfR. In men, both indicators estimate IDA at around 3%. The prevalence of iron deficiency and anaemia varies by age group, residence and region 18. The WHO classifications of anemia as a public health problem as applied to Malawi show that there is a severe anemia problem (greater than or equal to 40%) in preschool children, a moderate problem (20.0 – 39.9%) in women and school children and a mild problem (5.0 – 19.9%) in men.
Vitamin A
Vitamin A deficiency is the most common cause of blindness in children and leads to increased risk of morbidity and mortality. A 1983 survey in the Lower Shire found that 75% of all monocular blindness and 30% of all bilateral blindness was caused by cornea-related blindness, most likely due to interactions among vitamin A deficiency, measles, malnutrition and trachoma. The prevalence of severe xeropthalmia in the same survey was 3.9%, night blindness five times higher, and corneal scars ten times higher than the WHO cut off indicating that vitamin A deficiency is a public health problem 19. Most recent surveys in the central region indicate high prevalences still and WHO classifies Vitamin A deficiency in Malawi to be a clinical public health problem. The more recent 2001 national micronutrient survey reports almost 60% of preschool children, 38% of school children, 57% of women of child bearing age and 38% of men who have serum retinol values <20microg/dL (WHO criteria states that vitamin A deficiency constitutes a public health problem in countries with a prevalence of >5% of plasma vitamin A of <10 µg/dl (WHO, 1982)).
Iodine status
Summary: Distribution of undernutrition in Malawi.
Incidence:
Population estimates for Malawi not readily available
Stunting tends to occur earlier followed by underweight then wasting
Prevalence:
Highest prevalence found between ages 6 and 20 months
Half of Malawian under five year old children are stunted, one in three are underweight and one in every 14 children are wasted.
Iodine deficiency impairs physical and mental development including intellectual capacity. Goitre (enlargement of the thyroid) reflects significant iodine deficiency in a population. According to WHO classification, all districts in Malawi have some degree of Iodine Deficiency Disorder (IDD). A 1989 survey in 10 districts reported a total goitre rate of 12.7% with widely scattered severely endemic areas. A 1989 review of iodine supplementation surveys showed that 56% of the 177,137 women and children examined in some districts in Malawi from 1983 to 1989 had goitre 20. In the 2001 micronutrient survey, prevalence of iodised salt was also low.
Risk factors for undernutrition
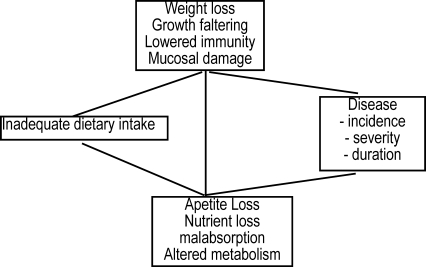
In the development of undernutrition, the starting point is reduction in dietary intake. This can be due to psychiatric illness, anorexia associated with infection, liver disease, neoplasia, drug interaction, nutrient deficiency, famine or starvation, upper intestinal disease, malabsorption or other losses from the body. This reduced dietary intake in turn leads to reduced mass, reduced requirement, reduced work, physiologic and metabolic changes, changes in body composition, and loss of tissue reserve. The defects become self reinforcing in vicious cycles leading to the development of frank undernutrition and ultimately death. An example of such a vicious cycle is illustrated in figure 1.
Figure 1.
Undernutrition - infection vicious cycle.
Source: State of the Worlds Children 1998, UNICEF 1998
Many observational studies on the relationship of undernutrition and infectious disease have been done and have been extensively reviewed (Scrimshaw et al. 1968, Martorell et al. 1975, Tomkins and Watson, 1989, Baqui and Black 2002). Malnourished children are more prone to frequent, long lasting, and severe episodes of disease that result in reduced dietary intakes due to reduction in appetite, nutrient loss, malabsorption, and altered metabolism. The reduced dietary intake leads to further undernutrition thereby completing the cycle which starts again and if unbroken may quickly lead to death 21.
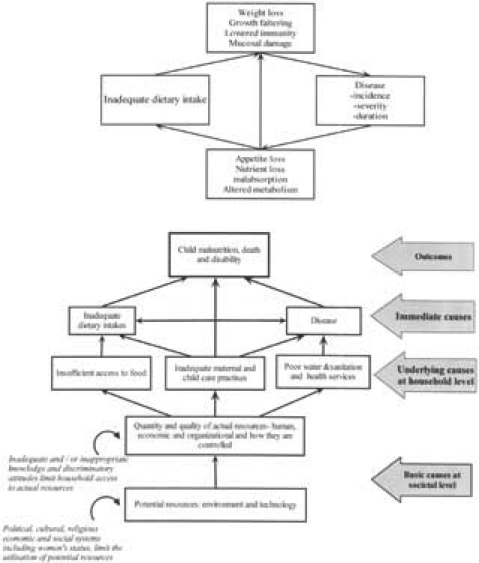
The determinants of malnutrition are multiple, interrelated and operate at different levels. The causes and their relationships can concisely be diagrammatically presented as shown in figure 3.
Figure 3.
Consequences of undernutrition throughout the life cycle.
(Reproduced with permission from ACC/SCN 2001)
There are three levels of causes of undernutrition. Immediate causes operating at the individual level (biological risk factors), underlying causes operating at the household level (behavioural risk factors), and basic causes which operate at the society level (social risk factors). The immediate causes of malnutrition interrelate with malnutrition in such a way that they form a vicious cycle which if not broken results in death (Figure 1).
The main risk factors for undernutrition can also be considered at the biological, behavioural and societal levels. The biological causes include infectious diseases such as diarrhoea, malaria, HIV, measles and intestinal helminthes, malbsorptive states, and systemic illnesses causing anorexia. Behavioural risk factors include poor water and sanitation, inappropriate maternal and infant feeding practices and insufficient access to food. At the societal level risk factors include political, cultural, religious and social systems including women's status which limit the utilization of potential resources where those are available. Furthermore inadequate and / or inappropriate knowledge may limit household's access to potential resources 22.
Disease risk factors
Diarrhoea disease
Acute diarrhoea is the commonest illness in developing countries. Its prevalence is highest towards the end of the first year and in the second year of life, a period which corresponds to the period of high incidence and prevalence of PEM. Diarrhoea has a consistent harmful effect on weight gain. A review of the effect of diarrhoea on undernutrition reports that between 10 to 80% of the difference between the international growth reference and growth of children in developing countries is associated with diarrhoeal disease. The effect on height gain though reported by some studies, has not been consistent 23. In Malawi there have been few population based studies investigating the role of diarrhoea in undernutrition. However diarrhoea disease is one of the commonest causes of attendance at out patient clinics with about 5 disease episodes per child per year. It is also the third commonest cause for hospital admission and the fourth commonest cause of mortality. In undernutrition, chronic and persistent forms of diarrhoea are the most implicated. Acute episodes are thought to be less implicated since there is usually time for recovery before the next episode. However, in the developing world children tend to have frequent episodes of diarrhoea such that they do not have sufficient time to recover to their pre-illness nutritional status. This puts them on a slippery slope to undernutrition where-by each sub-sequent episode of diarrhoea pushes them down the slope. In Malawi, there are no reported studies of the prevalence of chronic diarrhoea
Intestinal and Urinary Helminths
Intestinal helminthes such as hookworm, round worm and Schistosomiasis are also important risk factors for development of undernutrition especially micronutrient deficiencies. The 2001 micronutrient survey in Malawi reports increased risk of iron deficiency anaemia in school children with infestation. 13.8% of school children had hookworm, 3.7% had roundworm and 2.5% had Schistosoma mansoni. Significantly more male children had hookworm and Schistosoma mansoni. Urban children were significantly more likely to have roundworm. School children in the Northern Region had significantly more roundworm. For urinary schistosomiasis older age children living in a rural area and living in the Southern Region were significantly more likely to have urinary schistosomiasis compared to younger children and those from the other regions.
Malaria
Malaria is not only exacerbated by malnutrition but it also results in growth failure 24. In cohort studies from the Gambia, malaria was significantly associated with lower weight gains in children below 36 months of age. Several clinical trials of chemoprophylaxis and or use of insecticide treated nets show better growth compared to controls 25. In a survey from Malawi 18, malaria parasitemia was associated with twice as much risk of iron deficiency compared to children with no parasitemia. (Prevalence figures of malaria can be found in chapter on malaria). The prevalence of malaria parasitemia in school children was 47.4%. There were no significant differences found in parasite prevalence according to age group, standard, sex, residence or region but rural women were more likely to have malaria parasitemia than their urban counterparts. A total of 12.2% of the men in the survey had malaria parasitemia. Significantly more men in the high SES group had malaria parasitemia in their blood smears.
Malaria has metabolic effects similar to any systemic illness. Rates of whole body protein synthesis and breakdown are increased with breakdown exceeding synthesis. Prolonged infections in endemic areas has effect on placental function and may depress birth weight (refer chapter on malaria in pregnancy). Malaria prophylaxis and effective public health measures against malaria have been documented to improve birth weights in some areas 26. In the bone marrow malaria causes a decrease in haemopoiesis and increases haemolysis of erythrocytes leading to anaemia. Malaria also plays a role as an immune suppressor thereby leading to increased prevalence and severity of infections such as diarrhoea and respiratory disease which also cause malnutrition.
Another important role of malaria in undernutrition is through its effects in pregnancy which leads to low birth weight. The incidence of low birth weight is estimated by the MDHS 2000 to be about 20% and this is likely due to reduced dietary intakes during pregnancy, low pre-pregnancy weight and high incidence of diseases more especially malaria.
HIV
There are several ways how HIV can result in undernutrition. First, there are direct effects on the infected child whereby HIV like other infections increases metabolic demand and because of immunosuppression predisposes to opportunistic infections e.g. diarrhoea, which results in undernutrition. Secondly, there are indirect effects on the child through effects of HIV on mothers irrespective of whether a child is infected or not. Maternal HIV can result in reduced care and disruption of feeding due to maternal morbidity or death. Thirdly, because HIV can be transmitted from mother to child also through breastfeeding, it complicates choices for infant feeding in developing countries. Children who are not breastfed are at increased risk of undernutrition and yet breastfeeding may also increase mother to child transmission of HIV. Recent evidence however suggests that exclusive breast-feeding for six months, followed by abrupt weaning, can be protective against mother to child transmission 27,28.
The distribution of HIV infection in Malawi is presented in the HIV chapter. However in an ongoing study of prevalence of HIV infection in nutrition rehabilitation units in Malawi, HIV prevalence overall was 30.01% (C.I. 22, 37). This was highest in the South 42% (C.I. 30, 54) and lowest in the Central Region, 16% (C.I. 6, 26). Urban and rural prevalence was 50% (C.I. 36, 64) and 19% (C.I. 11, 27) respectively (Thurstans S, personal communication).
Respiratory infections
Infections of the respiratory tract (acute and chronic infections) and middle ear make important contribution to morbidity and mortality particularly in the first year of life. They have an indirect effect on nutritional status through their effect on food intake and appetite. Breathless children can not eat or drink properly and also have increased energy expenditure. In pertusis vomiting after coughing is very common after the acute infection.
Behavioural risk factors
Child caring and feeding practices
Child care is defined as referring to the behaviours and practices of care givers (mothers, siblings, fathers and other child care providers) who provide the food, health care, psychosocial stimulation and emotional support necessary for the healthy growth and development of children.
Inappropriate breastfeeding
It is recommended to exclusively breast feed for at least 6 months before introducing complementary feeds. This is because breast milk is adequate to meet the nutrient requirements of the growing infant and is also protective from infections apart from the other psychological and economic benefits it confers. Failure to exclusively breast feed in developing countries leads to increased morbidity and mortality. Exclusively bottle fed infants in the developing world have a risk ratio of developing undernutrition of between 2 to 50 fold compared to exclusively breast fed infants 29. Breast-feeding has also been shown to reduce the risk of morbidity especially diarrhoeal disease. Recent evidence also suggests that exclusive breast-feeding could reduce mother to child transmission of HIV, which in turn reduces the risk of undernutrition 27, 28.
In Malawi while the prevalence of exclusive breastfeeding has been reported to have increased according to the Demographic Health surveys increased from 3% in 1992 to 67% in 2000, it is still not optimal. Questions have been raised about the prevalence reported in 2000 MDHS and a reanalysis found the prevalence at 44% 18. One of the problems was the way the way exclusive breastfeeding was defined in that survey. The above cited figures of exclusive breastfeeding thus show that complementary feeding is often introduced very early.
Inappropriate complementary feeding practices
In Malawi, the most common complementary food is a thin maize porridge which is not nutrient dense and thus leads to inadequate energy and nutrient intakes among infants. As highlighted above, apart from the quality issues another problem is that these foods are introduced too early in the children's diet. Maize/soy blend (Likuni phala) is promoted as a complementary food and is fortified with micronutrients if commercially provided. However, cost implications means that most poor mothers can not afford such commercial products. Similar reasons also explain why the often given advice of increasing the energy and nutrient content of Likuni phala by adding egg and oil is not followed. When not fortified however, Likuni phala is just slightly better than ordinary maize flour porridge and just replaces the normal porridge from the infant's diet without really complementing it 30.
Another problem with the often used complementary foods in Malawi is their viscosity apart from the low energy and nutrient density. Strategies such as fermentation, soaking, and germination have been successfully used to reduce the viscosity and improve nutrient availability have been practised for a long time in Malawian communities. However, when not done commercially there is a risk of bacterial contamination leading to morbidity but also such processes take a long time. This has implications on increasing the time caregivers have to spend preparing these foods thus compromising their other care giving activities and contribution to household livelihoods.
To overcome the deficiencies in the quality of the complementary feeds, it is necessary to increase the frequency of administration and variety of the food. This is a challenge for the caregiver and family due to time constraints as well as resources such as firewood.
Health seeking behaviour
Most of the morbidity associated with undernutrition is from preventable diseases. However one behavioural factor that contributes to undernutrition is the care seeking of caregivers in response to symptoms and signs of that morbidity. There are of course several factors that contribute to whether care is sought including knowledge of the caregivers about the disease, access to care facilities, perceptions of the care givers etc. Care seeking practices related to the commonest morbidity in Malawi, which is also the commonest morbidity associated with undernutrition is less than optimal. The 2000 MDHS report that only 27% of children who had symptoms of acute respiratory infection were taken to a health facility while amongst those reporting diarrhoea disease only 62% were given oral dehydration therapy as first line treatment either at home or by being taken to a health facility. Another aspect of health seeking is to some extent reflected in vaccination coverage rates which indicate that only 70% of 12 to 23 month old children are fully vaccinated, a decline in coverage from 82% in 1982. Furthermore while about 25% of children had a fever in the fortnight prior to the 2000 survey only 27% sought medical care compared to 49% in the 1992. As expected care seeking varied according to literacy and socio-economic status 18.
Summary: Causes and Determinants of undernutrition.
Immediate
Diseases (diarrhoeal disease, Intestinal helminths, malaria, HIV, Acute Respiratory infections, other chronic diseases e.g. tuberculosis)
Inadequate dietary intakes (inappropriate breast feeding and complementary feeding)
Intermediate
Inadequate child caring practices
Poor water and sanitation and health services
Food insecurity
Basic
Gender inequality
Illiteracy
Politics
General poverty
Water supply and sanitation
Although the direct effects of improved water and sanitation on growth are debatable, it is assumed that decreased incidence of diarrhoeal disease can reduce the risk of development of malnutrition by reducing the frequency of infections and time spent being ill. Poor water and sanitation is associated with increased frequency of water and sanitation related morbidity. In the MDHS 2000, 65% of households in Malawi had access to safe clean water, up from 47% 10 years earlier. 79% of households had pit latrines. In rural areas up to 21% of households had no toilet facility. With such poor access to safe water and sanitation, diarrhoeal diseases are more likely to be rampant and lead to poor nutritional status.
Social risk factors
Education
Female education is a major determinant of whether a child becomes malnourished or not. Countries with high female literacy and female status tend to have lower prevalence of malnutrition, independent of differences in the countries' wealth or general standards of living 22. In Malawi, rates of undernutrition also vary by educational status. The literacy rate in Malawi is 48% for women compared to 72% for men. Urban dwellers being more literate than their rural counterparts. In general the northern region has more literacy compared to the southern. The distribution of undernutrition in Malawi also follows a similar pattern. Results from the Integrated Household Survey of suggest that both education and poverty play a part.
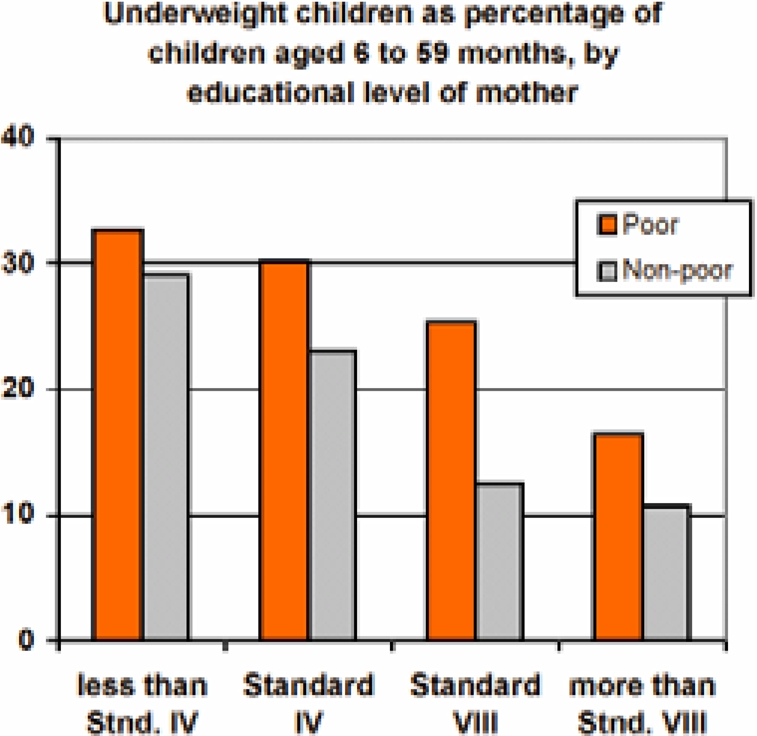
Source: Integrated Household Survey 1998, NSO, Malawi
Household food security
Malawi is one of the poorest countries in the world and the integrated household survey of 1998 approximated that 65% of the population is poor. This population is therefore unlikely to meet their food requirements all year round as well as basic non food needs.
Poverty, encompasses different dimensions of deprivation that relate to human capabilities including consumption and food security, health, education, rights, voice, security, dignity and decent work. In Malawi, poverty is very prevalent in rural communities where over 90% of the population subsists on farming, much of which consist of growing maize. With per capita land holding ranging from 0.18 to 0.26 hectares per household, adoption of improved seed, fertilizer and other soil fertility enhancing technologies is limited such that up to 28% of the rural population are chronically food deficient. This scenario therefore places a substantial portion of the population in food insecurity and at risk of developing undernutrition. 30.
Household food availability is necessary but not always sufficient for improving nutritional status. Actual access to food has to be enhanced with improvements in health status, improvements in maternal and child health to ensure adequate child care practices, access to health services as well as good environmental conditions including safe water and sanitation. All these requirements may be difficult to realize without a change in women's place in society and their role in care giving.
Politics and governance
How well a government controls and utilizes the county's resources for the benefit of its people and for future generations determines the standard of living, distribution of wealth, health conditions, access to opportunities and the country's ability to sustain the institutions of governance and social welfare (National Nutrition Policy, 2000). This has a direct bearing on the nutrition and health of a population. Formulation of appropriate food and nutrition policies is thus expected to improve nutrition status of the population. Since it is usually the very poor in a society that have the worst nutritional problems, deliberate efforts at poverty alleviation specifically targeting the poor are likely to improve nutritional status of the poor.
Consequences of undernutrition
Undernutrition results in both immediate and long-term consequences. Figure 4 succinctly shows the effects of undernutrition throughout the lifecycle. Undernutrition in utero leads to low birth weight babies who are prone to morbidity, have higher risk of cognitive and mental impairment and mortality 31. Low birth weight babies may also end up as undernourished toddlers with reduced mental capacity 32. Childhood undernutrition could also lead to stunted adolescents who may end up as stunted adults if there is no catch up growth.
Childhood undernutrition has been implicated in up to 50% of all childhood deaths in the developing world 33. In a review by Pelletier (Semba 3) 28 community based studies from Asia and sub-Saharan Africa were reviewed and found that mortality was increased not only with severe malnutrition but also mild to moderate forms of malnutrition. The review found that risk of death was 8.4, 4.6, and 2.5 times higher for a child whose weight for age was <60%, 60–69% and 70–79% of the reference median respectively compared to children with normal weight for age. In terms of population attributable risk, this translated to 56% of all childhood deaths being attributable to the potentiating effect of undernutrition 33, 34. Apart from mortality undernutrition also significantly contributes to the burden of morbidity such that the World Bank estimates that about 20 – 25% of total global DALYs are attributed to undernutrition and that is probably an underestimate as well 35. WHO estimates for Malawi suggest that malnutrition accounts for 16.5% of all deaths.
Childhood undernutrition has also been associated with adulthood chronic diseases such as diabetes mellitus, hypertension and coronary heart diseases, the so-called ‘foetal origins’ hypothesis 36,37. Childhood under-nutrition, leading to undernourished adults, can also lead to reduced physical capacity, which may be disadvantageous economically in environments heavily dependent on manual labour as exist in developing countries 38. Furthermore, in women, undernutrition may lead to obstetric complications that can lead to increase in maternal and infant mortality. Additionally, undernourished women are more likely to have low birth weight children, and thus the undernutrition cycle starts again and the effects of undernutrition end up spanning several generations if unchecked 39.
Effective interventions
There are several strategies that have been employed for the prevention of undernutrition and they range from specific interventions aimed at specific determinants to general interventions aimed at a broad range of determinants. As highlighted in the sections on risk factors and consequences, interventions targeting undernutrition are unlikely to work if they are targeting single determinants. Specific nutrition deficiencies are likely to cluster in same individuals and communities such that only when interventions are integrated are they likely to work. The interventions range from specific nutritional or non nutritional interventions targeting a specific deficiency to broad interventions targeting several de- ficiencies. The success of these interventions is debatable as there is a paucity of very good studies examining their efficacy. Below are some interventions which have shown some promise.
Interventions to improve dietary intakes
Dietary supplementation during pregnancy
Current evidence suggests that only supplements that provide more energy rather than more protein improve birth weight significantly. Maternal supplementation can increase maternal weight gain, infant head circumference and when there is a serious energy deficit, the length of the new born infant. In the Gambia 40, locally produced biscuits providing 1, 017 kcal and 22g protein per day from mid pregnancy reduced prevalence of low birth weight by 39% and increased birth weight by 136g and reduced infant mortality by 40%. Such improvement, it is said, can also be achieved by encouraging women to consume more of their normal diet and where possible providing energy supplements. On the other hand there is little evidence that individual nutrient supplementation (including calcium, folic acid, zinc, iron and vitamin A) can improve birth weight other than possibly through reduction in preterm delivery.
In Malawi, protein energy supplementation is practiced but not consistently and micronutrient supplementation with iron, folic acid and vitamin A is also practiced through antenatal clinics. Vitamin supplementation is implemented post partum and on average 29% of post partum women access this 41. 78.5% of women report receiving iron supplementation during their last pregnancy 41.
Promotion of exclusive breast feeding
Promotion of breast-feeding is a strategy that has been encouraged to prevent development of undernutrition. In Malawi exclusive breast-feeding for 6 months is promoted to prevent development of undernutrition. Exclusively bottle fed infants in the developing world have a risk ratio of developing undernutrition of between 2 to 50 fold compared to exclusively breast fed infants 29. Breast-feeding has also been shown to reduce the risk of morbidity especially diarrhoeal disease. Recently, evidence also suggests that exclusive breast-feeding can reduce mother to child transmission of HIV, which in turn reduces the risk of undernutrition 27, 28. Current WHO recommendations are to exclusively breast feed for 6 months. Several initiatives such as the Baby Friendly Initiative and Saving Newborn Lives have been implemented in some districts by NGO's e.g. Save the Children Foundation US (SCF US) to promote early initiation of breastfeeding and exclusively doing so for six months. Their impact on growth has not been rigorously assessed.
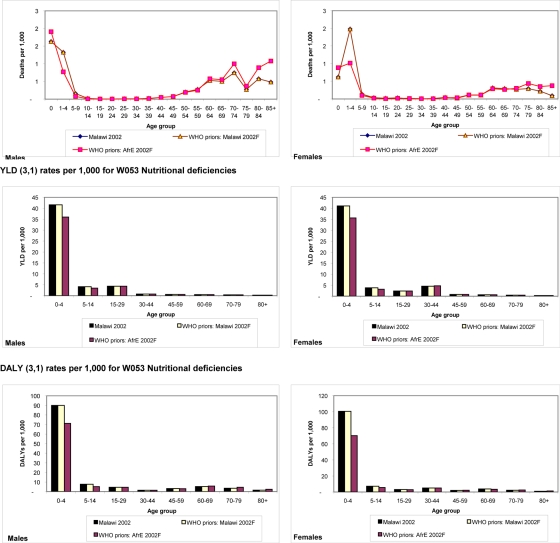
Disease specific comparisons as at 10 Aug 2005
Summary: Impact of undernutrition.
Strongly associated with risk of mortality such that it is directly and indirectly with 50% of all developing country childhood mortality
Contributes about a quarter of total global burden of disease as measured by DALYs.
Significantly affects cognition and development and in turn economic and social development of countries
Implicated in etiology of adult chronic diseases (Foetal Origins Hypothesis)
Improving complementary feeding
Appropriate complementary feeding which should be introduced at optimal time can reduce the incidence of undernutrition. In most developing countries, the energy density of broths and gruels used as complementary feeds is below the recommended 0.6kcal/g. Energy density can be improved by reducing water content and providing additional feedings. At present there is insufficient evidence to support use of amylases to lower the viscosity of cereals and increasing energy through adding sugar and oil can adversely affect the density of protein and micronutrients in the diet 40. This contradicts the often given advice to use fermentation and germination as well as adding oil and sugar to maize porridge in Malawi. Evidence from controlled trials of processed complementary foods such as maize/soy blend (Likuni phala) has shown inconsistent impact on nutritional status as measured by growth 42, 43, 6, 44. Interventions below 12 months are more likely to work better than those after 12 months but in the first 12 months there is always the risk of displacing breast feeding. With regard to micronutrients, it is difficult for infants to consume adequate amounts therefore micronutrient fortification of staples may be very important. Single micronutrient supplementation have shown some benefits: vitamin A prevention of eye lesions, reduction in mortality from measles and diarrhoea and increased haemoglobin synthesis; iron, improved cognitive and motor development of anaemic children; zinc, improved growth of children who are stunted; iodine, reduced mortality, improved mental and motor function and improved growth and cognition 39. More recently novel approaches such as fat based spread which is energy and micronutrient fortified 45–48 and encapsulated sprinkles are being tried for efficacy.
In Malawi complementary feeding is started too early with poor quality complementary feeds. Likuni phala or variations thereof are the commonest complementary food being used. With evidence of good results from ready-to-use-therapeutic foods (RUTF or Chiponde) 30,49, 50, there is a shift towards using these type of foods.
Supplementary feeding
Supplementary feeding is one of the commonest approaches to secondary prevention of undernutrition. It has been used for both prevention and treatment of undernutrition. In controlled research situations supplementary feeding has been shown to improve growth of undernourished children. During pregnancy, dietary supplementation with balanced energy and protein has been shown to improve pregnancy weight gain and birth size 40. Similarly in children, supplementary feeding has been associated with improvements in weight and height gain in controlled situations 51–53. The improvements in growth have however been more pronounced in children less than 2 years and have depended on the severity of undernutrition. This has been attributed to the fact that growth rates and incidence of undernutrition are highest in under-2-year-old children. As such, the often-short dietary supplementation interventions are likely to show effect on growth during such periods of high growth rates. Not all supplementary feeding studies have however, shown improvements in growth 52.
Despite such impressive results in controlled situations, large-scale supplementary feeding programs have not shown much success in improving childhood growth 39,54. Some of the problems associated with large scale feeding programs have been problems in targeting the right groups, ensuring intake of the supplement by intended beneficiaries, spillover to other than intended beneficiaries and replacement of the habitual dietary intakes of the beneficiaries. Another additional important issue is also the choice of food supplements to use. More important than all these caveats the supplementary programmes are usually extremely expensive, unsustainable and short lived.
More specifically, success has been reported with targeted micronutrient supplementation. Implemented usually through the life cycle approach, these strategies have been shown to work in various environments. Examples include vitamin A supplementation coupled with the expanded programme on immunisation and Vitamin A and iron supplementation through antenatal clinics.
Food fortification
Another approach at the societal or national level is fortification of foodstuffs to correct specific micronutrient deficiencies e.g. salt iodisation. In fact, the most effective way to combat iodine deficiency disorders is food fortification and this is mostly salt fortification. However, these approaches have the problems of cost, dependency, sustainability and bioavailability. A cost-benefit analysis is always important in choosing which approach to implement. In Malawi legislation requiring iodination of salt was passed as early as 1985 but only became operational 10 years later. Furthermore, it is not easily enforced as the figures on prevalence of households with salt adequately iodinated is very low. Apart from iodine other food stuffs that could be forti- fied include sugar and cooking oil and margarine for the prevention of vitamin A deficiency. These are currently being done on a voluntary basis by food processors. It would significantly help if there was political will to enforce mandatory fortification.
In Malawi, only 47.1% (95% CI: 40.5, 53.8; DEFF = 2.338) of the households are estimated to have salt with at least 15 ppm . Consistent with the harmonization regulations for iodized salt in Southern Africa the target at the household is for 100% of households to be using salt that contains at least 25 ppm iodine (ICCIDD, 1999). Only 36.7% (95% CI: 30.4, 43.0, DEFF=2.260) of the households in the 2001 national survey met this target 55.
School feeding and health programmes
Schools offer a potentially effective means of providing preventive health services and services to improve nutrition have used this approach. Most national studies do not include data on school age children but a localized study conducted in Northern Malawi revealed that 1.1% were wasted, 19.8% were underweight and 47% were stunted 56. The recent micronutrient survey also showed that 38% of school age children were vitamin A deficient and 22% were anemic 55. Additionally, a large number are infected by parasitic infections including malaria, intestinal helminthes and schistosomes.
A pilot school health package has been developed by the Ministry of Education in conjunction with volunteer organizations and includes a mid morning hot porridge served to both girls and boys in all classes, and in addition, take-home rations are distributed to girls only after attending a minimum of 18 school days a month. The ration includes maize/soy flour blend and a portion of maize. In some school health programmes periodic mass screening and treatment is done for intestinal helminths and urinary schistosomiasis 57.
Interventions to reduce morbidity
Control of Diarrhoea disease
The effect of diarrhoea on short and long-term weight and height gain have been studies in several settings. A recent review 23 reports that while the effect on weight gain is often reported, the effect on linear growth on the other hand has not been consistent. From the review, between 10 to 80% of the difference between the international growth reference and growth of children in developing countries is associated with diarrhoeal disease. The effect on height gain though reported by some studies, has not been consistent 23. Other studies have queried whether the effect of diarrhoea on undernutrition is overemphasized 58,59. The reason for this assertion being that the effect of diarrhoea on dietary intake and growth is transient and thus a child could return to normal diet and growth within a few weeks of an illness episode. However, in the developing world children tend to have frequent episodes of diarrhoea such that they do not have sufficient time to recover to their pre-illness nutritional status. This puts them on a slippery slope to undernutrition where-by each sub-sequent episode of diarrhoea pushes them down the slope. Strategies to prevent diarrhoea through, for example, exclusive breast-feeding, improved water and sanitation, treatment and promotion of oral rehydration therapy are thought to mitigate undernutrition.
Expanded Programme on Immunisations
Of the vaccine preventable diseases, measles is the one most associated with undernutrition. However, its effect on growth has had mixed results. Poor growth outcomes have been reported in some studies 60 and no effect has been reported in others 61. Measles is thought to cause undernutrition through the following mechanisms. First, measles infection is followed by a period of depressed cell mediated immunity, which makes children susceptible to opportunistic infections including diarrhoea and acute respiratory infections. Secondly, during measles infection energy intake is reduced 62. The infections and reduced dietary intake predispose children to undernutrition. Immunization against measles and other vaccine preventable diseases could thus prevent children from developing undernutrition. Additionally the programme has been used as a vehicle for micronutrient supplementation e.g. iron and vitamin A as well as other activities e.g. provision of insecticide treated nets (ITNs) which prevent malaria and thus effectively also target undernutrition especially iron undernutrition.
Micronutrient supplementation
Evidence from clinical trials show that iron supplementation of pregnant women improves Hb and iron status. Efficacy increases with doses up to 60mg/d and daily supplementation is better than weekly and total amount of iron consumed is the most important predictor of maternal Hb response 39. In Malawi this daily supplementation is implemented through the antenatal clinics. Since malaria is endemic in Malawi, anti malarial prophylaxis during pregnancy also helps improve iron status and prevent malaria which is associated with undernutrition and preterm delivery. The above two interventions are also complemented by other non nutritional interventions such as provision of free or subsidized insecticide treated nets through antenatal clinics.
Other strategies include supplementation of low birth weight infants with iron starting at 2 months age. Currently this approach is not being implemented in Malawi. Except for fortification of foods, effectiveness of other food based strategies to improve iron status has not been evaluated properly. Dietary diversification through improved intake of vitamin C rich foods, and supporting of poultry production (chickens, guinea fowls), small livestock (rabbits, goats) and fish has been promoted to improve iron and other micronutrient intakes. Additionally genetic engineering to improve iron content of staple foods may offer an option but the evidence is still not there. Several countries such as Chile, Ghana and Venezuela have recorded improvements in iron status following food fortification.
For iodine, salt iodisation is by far the most effective intervention to combat iodine deficiency and has been shown to be efficacious where salt iodine content was appropriate at the time of consumption.
Vitamin A supplementation through the life cycle approach is another strategy and metaanalysis indicates reduced mortality from diarrhoea and measles by 23 % in ages 6 to 59 months. Just as for iron, there several food based strategies that can also be employed but their effectiveness is also not evaluated properly.
Social interventions
Water supply and sanitation
Reductions in diarrhoeal morbidity and mortality of about 27 % and 30 % respectively have been reported following improvements in water supply and disposal of excreta 63. It is, however, not clear whether this reduction in morbidity does lead to improvements in nutritional status. Studies in Bangladesh 59 and Gambia 61 have shown no reduction in undernutrition following improvements in water and sanitation. However, although the direct effects of improved water and sanitation on growth are debatable, it is still assumed that the decreased incidence of diarrhoeal disease on its own reduces the risk of development of malnutrition by reducing the frequency of infections and time spent being ill.
Child growth monitoring
This strategy is based on the longitudinal charting of a child's growth in order to identify when growth starts faltering and institute action to prevent development of undernutrition. Unlike anthropometric screening for interventions, there is no consensus what constitutes inadequate growth when action has to be taken as the risk from milder forms of growth deficit is not well known 64. In any case, even if the level for taking action were agreed it is still not clear what action to take. Furthermore, since it is the lowest cadres of primary health care providers who usually carry out growth monitoring, it does not necessarily result in proper action. This is because it is difficult to make accurate measurements and interpret them to take necessary action. Compounding this is the fact that the people entrusted with this activity in primary health care programs have many other things to do making the charting of growth an automatic task that does not result in proper action. However, others have argued that when placed in the hands of villagers, growth monitoring becomes a tool for development and community participation 65. In recent years, this has been integrated with other activities such as in integrated management of childhood illness (IMCI). This makes growth monitoring a valuable tool as it is not an isolated activity with questionable scope of success.
Education
Female education is a major determinant of whether a child becomes malnourished or not. Countries with high female literacy and female status tend to have lower prevalence of malnutrition, independent of differences in the countries' wealth or general standards of living 22. It is not clear how this relationship works. Some possible reasons include the fact that educated women are better at organizing their resources and time, making better use of health services, start child bearing later and have longer birth intervals and likely to have an independent source of income 26. However, education per se, if not coupled with improvement in the social status of women may not be effective. Paradoxical improvements in food availability following the green revolution and improvements in female education have not necessarily resulted in improvements in growth status among children on the Indian sub continent 66. A possible reason being the fact that decision-making powers in a community may be vested in men, as such equipping women with knowledge may not necessarily translate into giving them with decision making powers.
Apart from basic literacy, nutritional education programmes have in some settings been shown to improve growth in stature and weight 67. Integrating nutritional education in existing programmes such as IMCI, ANC and out patient care is one effective approach to reduce undernutrition.
Integrated Nutrition programmes
From the foregoing it is quite obvious that single targeted short term interventions are unlikely to succeed in an environment where the causes of malnutrition are not only multiple but also interrelated in a complex way. Integrated approaches combining several strategies are thus the more likely to work in such environments. Several such interventions have been shown to work in different areas especially in south Asia 68. In Malawi a good example is an intervention coordinated by a non governmental organization, World Vision International (Malawi MICAH project) which showed very good impact of this approach 68. Briefly the programs aimed to improve nutritional status by improving micronutrient intake and bioavailability
Summary: Effective interventions.
There are numerous interventions that work directly or indirectly to combat undernutrition.
The evidence for most interventions is not conclusive
Most supplementary feeding interventions have been shown to work in controlled situations but not when implemented in practice.
While scientifically most of the interventions should logically work, the evidence has not been consistent for interventions such as control of diarrhoeal disease, water and sanitation.
Because the etiology is usually multiple and etiologic agents inter-related, integrated approaches are more likely to work but are very expensive to implement.
Micronutrient supplementation of iron / folate and iodine supplementation using community health workers
Dietary diversification and modification (DDM) activities focusing on the raising/production and household consumption of small animals, vegetables and fruits.
Food fortification i.e. iron and micronutrient fortification of corn/soy blend for complementary feeding and advocacy to ensure only iodized salt was imported into project area
Improved infant and child feeding practices through promotion of exclusive breast feeding and nutrient information education and communication.
Additionally the project aimed to reduce prevalence of diseases affecting micronutrient status
Through improved water and sanitation
Control and treatment of common endemic diseases by improving capacity and establishing drug revolving funds etc., mass treatments for schistosomiasis etc.
Promotion of immunisations
When evaluated after four years of implementation, analysis of the survey data indicated that the program had been successful in reducing the prevalence of micronutrient deficiencies and associated diseases. More than 90% of mothers in MICAH areas knew the causes of anaemia and goitre and approximately 85% were using iodized salt in their homes. The prevalence of anaemia in children under five was reduced from 94.3% at baseline to 80.1% in MICAH areas, compared with 90.8% in non-MICAH areas. There was also a significant decrease in the prevalence of severe iodine deficiency (from 15.9% at baseline to 3.2% in the MICAH follow-up area) among school-aged children. There were also significant increase in mothers exclusively breastfeeding (EBF) their infants for 4–6 months, from 45% at baseline to 72% in MICAH follow-up areas and 65% in non-MICAH. The mean duration of EBF was raised from 3 months at baseline to 5 months during the impact survey. In MICAH areas, the prevalence of stunting had also been decreased by 15.3%, from 55.7% at baseline to 40.4% at follow-up. There were further improvements in immunization coverage rates, prevalence of intestinal helminths and access to safe water and sanitation
Other integrated approaches include the IMCI whereby nutrition monitoring and counselling have been incorporated in an approach of treating common childhood illnesses.
Figure 2.
Determinants of undernutrition.
Source: State of the Worlds Children 1998, UNICEF 1998
Table 2.
Classification of undernutrition in using Body Mass Index (BMI) and Mid Upper Arm Circumference (MUAC)
| BMI | MUAC | ||
| Level | Definition | Level (cm) | Definition |
| (Kg/m2) | Males | ||
| >20 | Normal | >22 | Normal |
| 18.5 – 20 | Marginal | <22 | Malnourished |
| 17 – 18.5 | Mild malnutrition | Females | |
| 16 – 17 | Moderate malnutrition | >22 | Normal |
| <16 | Severe malnutrition | <22 | Malnourished |
| Children | |||
| >12.5 | Normal | ||
| 11 – 12.5 | Mild/moderate malnutrition | ||
| < 11 | Severe malnutrition |
Note - MUAC values from MOH Training manual for management of severe acute malnutrition, 2005
Table 11.
Shows the burden of Protein -energy malnutrition and selected micronutrient deficiencies in Malawi. (WHO Afro rates)
| Total | Total | |||||
| Nutritional deficiencies |
YLL | Male | Female | YLD | Male | Female |
| 61 | 31 | 30 | 50 | 23 | 27 | |
| Protein-energy malnutrition |
43 | 23 | 20 | 23 | 11 | 12 |
| Iodine deficiency | 2 | 1 | 1 | 10 | 5 | 5 |
| Vitamin A deficiency | 6 | 3 | 3 | 0 | 0 | 0 |
| Iron-deficiency anaemia |
10 | 4 | 6 | 16 | 6 | 10 |
| Other nutritional disorders |
1 | 0 | 0 | 0 | 0 | 0 |
YLL: Years of life lost due to premature death
YDL: Years of life lived with disability
WHO estimates for Malawi can be compared to the Afro region
Footnotes
Supine length is measured until 24 months and erect height thereafter because children are able to stand on their own. The MOH Training manual for management of severe acute malnutrition (2005) recommends that children less than 85 cm are measured supine and more then 85cm standing.
Indices are defined as combinations of measurements, which have a biological meaning, e.g. weight for height while indicators are derived from indices to form a social concept taking on a value system e.g. proportion of children below a certain level of weight for height which can be used to describe nutritional status of a community 1
A Z score is a measure of how far an observation is from the population mean as measured in standard deviation units. A standard deviation score of a nutritional indicator for an individual = (individual's value − median value of reference population)/standard deviation value of reference population.
References
- 1.Waterlow JC. Classification and definition of protein energy malnutrition. WHO Monograph Series no 68. Geneva: World Health Organisation; 1976. [PubMed] [Google Scholar]
- 2.Golden MHN. Severe malnutrition. In: Weatherall DJ, Ledington JGG, Warell DA, editors. Oxford textbook of Medicine. 3rd ed. Vol. 1. Oxford: Oxford University Press; 1995. pp. 1278–1296. [Google Scholar]
- 3.Habicht JP, Martorell R, Yarbrough C, Malina RM, Klein RE. Height and weight standards of pre-school children. How relevant are ethnic differences in growth potential? Lancet. 1974;1:611–615. doi: 10.1016/s0140-6736(74)92663-4. [DOI] [PubMed] [Google Scholar]
- 4.Whitehead RG, Paul AA. Growth charts and the assessment of infant feeding practices in the western world and in developing countries. Early Hum Dev. 1984;3:187–207. doi: 10.1016/0378-3782(84)90031-8. [DOI] [PubMed] [Google Scholar]
- 5.Martorell R, Kettle Khan L, Schroeder D. Reversibility of stunting: epidemiological findings in children from developing countries. Eur J Clin Nutr. 1994;48(suppl 1):S45–S57. [PubMed] [Google Scholar]
- 6.Martorell R. Child growth retardation: A discussion of its causes and of its relationship to health. In: Blaxter KL, Waterlow JC, editors. Nutritional adaptation in man. London: John Libbey; 1985. pp. 13–30. [Google Scholar]
- 7.Neumann CG, Harrison GG. Onset and evolution of stunting in infants and children. Examples from the Human Nutrition Collaborative Research Support Program. Kenya and Egypt studies. Eur J Clin Nutr. 1994;48(suppl 1):S90–S102. [PubMed] [Google Scholar]
- 8.Rivera J, Ruel MT. Growth faltering starts in the first three months of life among rural Guatemalan children. Eur J Clin Nutr. 1997;51:92–96. doi: 10.1038/sj.ejcn.1600371. [DOI] [PubMed] [Google Scholar]
- 9.Shrimpton R, Victora CG, de Onis M, Lima RC, Blossner M, Clugston G. Worldwide timing of growth faltering: Implications for nutritional interventions. Paediatrics. 2001;107(5):E75. doi: 10.1542/peds.107.5.e75. [DOI] [PubMed] [Google Scholar]
- 10.Mata LJ, editor. A prospective field study of health and growth. Massachusetts: MIT press; 1981. The children of Santa Maria Caque. [Google Scholar]
- 11.Maleta K, Virtanen SM, Espo M, Kulmala T, Ashorn P. Timing of growth faltering in rural Malawi. Arch Dis Child. 2003;88:574–578. doi: 10.1136/adc.88.7.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.WHO UNICEF, author. Low birth weight. A tabulation of available information. Geneva: Maternal Health and Safe Motherhood Programme. WHO and UNICEF; 1992. [Google Scholar]
- 13.Morley D, Bricknell J, Woodland M. Factors influencing the growth and nutritional status of infants and young children in a Nigerian village. Trans R Soc Trop Med Hyg. 1968;62:165–195. doi: 10.1016/0035-9203(68)90155-7. [DOI] [PubMed] [Google Scholar]
- 14.Scrimshaw NS, Taylor CE, Gordon JE, editors. Interaction of nutrition and infection. WHO monograph series no 57. Geneva: World health Organisation; 1968. Nutrition Policy Discussion Paper No 15. [PubMed] [Google Scholar]
- 15.Martorell R, Habicht JP, Yarbrough C, Lechtig A, Klein E, Western KA. Acute morbidity and physical growth in rural Guatemalan children. Am J Dis Child. 1975;129:1296–1301. doi: 10.1001/archpedi.1975.02120480022007. [DOI] [PubMed] [Google Scholar]
- 16.Ulmala T, Vaahtera M, Rannikko J, Ndekha M, Cullinan T, Salin M-L, Ashorn P. The relationship between antenatal risk characteristics, place of delivery and adverse delivery outcome in rural Malawi. Acta Obstet Gynecol Scand. 2000;79:984–990. [PubMed] [Google Scholar]
- 17.National Statistical Office (Malawi) and OCR Macro, author. Malawi Demographic and Health Survey 2000. Calverton, Maryland, USA: National Statistical Office, Zomba, Malawi and OCR macro; 2001. [Google Scholar]
- 18.Ministry of Health and Population, UNICEF, CDC, author. National Micronutrient Survey Report, Lilongwe, Malawi. 2003
- 19.OMNI Micronutrient fact sheet.
- 20.Ministry of Health and Population, author. IDD Review Report. Malawi: 1998. [Google Scholar]
- 21.Tomkins AM, Watson F. Malnutrition and infection. A review. Geneva: Advisory Committee on Co-ordination/Subcommittee on Nutrition, World Health Organisation; 1989. [Google Scholar]
- 22.UNICEF, author. The state of the world's children 1998. Oxford: Oxford University Press; 1998. [Google Scholar]
- 23.Baqui AH, Black RE. Childhood infectious diseases and their contribution to undernutrition. In: Black RE, Michaelsen KF, editors. Public health issues in infant and child nutrition. Philadephia: Nestle Nutrition Workshop Series, Nestec Ltd, Vevey/Lippincott Williams & Wilkins; 2002. pp. 20–57. [Google Scholar]
- 24.Garnham PCC. Malarial immunity in Africans: effects in infancy and early childhood. Am J Trop Med Hyg. 1949;43:47–61. doi: 10.1080/00034983.1949.11685394. [DOI] [PubMed] [Google Scholar]
- 25.Bruce-Chwatt LJ. Malaria in African infants and effect on growth and development in children in southern Nigeria. Ann Trop Med Parasitol. 1952;46:173–200. doi: 10.1080/00034983.1952.11685522. [DOI] [PubMed] [Google Scholar]
- 26.Waterlow JC. Protein energy malnutrition. London: Edward Arnold; 1992. [Google Scholar]
- 27.Coutsoudis A, Pillay K, Spooner E, Kuhn L, Coovadia HM. Influence of infant feeding patterns on early mother to-child transmission of HIV -1 in Durban, South Africa: a prospective cohort study. Lancet. 1999;354:471–476. doi: 10.1016/s0140-6736(99)01101-0. [DOI] [PubMed] [Google Scholar]
- 28.Coutsoudis A, Pillay K, Kuhn L, Spooner E, Tsai WY, Coovadia HM. Method of feeding and transmission of HIV-1 from mothers to children by 15 months of age: prospective cohort study from Durban, South Africa. AIDS. 2001;15:379–387. doi: 10.1097/00002030-200102160-00011. [DOI] [PubMed] [Google Scholar]
- 29.Jason JM, Nieberg P, Marks JS. Mortality and infectious disease associated with infant feeding practices in developing countries. Paediatrics. 1984;74(Suppl):702–727. [PubMed] [Google Scholar]
- 30.Maleta K, Duggan MB, Briend A, Manary M, Wales J, Espo M, Kulmala T, Ashorn P. Some based nutritional rehabilitation of stunted, mildly wasted children with a peanut based spread in rural Malawi. J Paed Gastr Nutr. 2004;38:152–158. [Google Scholar]
- 31.GOM, author. Food and Nutrition Policy Paper.
- 32.Ashworth A. Effects of intrauterine growth retardation on mortality and morbidity in infants and young children. Eur J Clin Nutr. 1998;52(suppl 1):S34–S42. [PubMed] [Google Scholar]
- 33.Grantham-McGregor S. A review of studies of the effect of severe malnutrition on mental development. J Nutr. 1995;125(suppl):2233S–2238S. doi: 10.1093/jn/125.suppl_8.2233S. [DOI] [PubMed] [Google Scholar]
- 34.Pelletier D, Frongillo EA, Schroeder D, Habicht JP. A methodology for estimating the contribution of malnutrition to child mortality in developing countries. J Nutr. 1994;124:2106S–2122S. doi: 10.1093/jn/124.suppl_10.2106S. [DOI] [PubMed] [Google Scholar]
- 35.Pelletier D, Frongillo EA, Schroeder D, Habicht JP. The effects of malnutrition on child mortality in developing countries. Bull WHO. 1994;7(4):443–448. 1995. [PMC free article] [PubMed] [Google Scholar]
- 36.Murray CJL, Lopez AD. The Global Burdenof Disease. Cambridge MA: Harvard University Press; 1996. p. 312. [Google Scholar]
- 37.Barker DJP. Fetal origins of coronary heart disease. BMJ. 1995;311:171–174. doi: 10.1136/bmj.311.6998.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Joseph KS. Validating the fetal origins hypothesis: An epidemiologic challenge. In: Black RE, Michaelsen KF, editors. Public health issues in infant and child nutrition. Philadephia: Nestle Nutrition Workshop Series, Nestec Ltd, Vevey/Lippincott Williams & Wilkins; 2002. pp. 199–216. [Google Scholar]
- 39.Branca FG, Pastore T, Demissie A, Ferro-Luzzi A. The nutritional impact of seasonality in children and adults of rural Ethiopia. Eur J Clin Nutr. 1993;47:840–850. [PubMed] [Google Scholar]
- 40.Allen LH, Gillespie SR, editors. ACC/SCN, author. What works? A review of the efficacy and effectiveness of nutrition interventions. Manila: ACC-/SCN Geneva in collaboration with the Asian Development Bank; 2001. [Google Scholar]
- 41.Ceesay SM, Prentice AM, Cole TJ, Foord F, Weaver LT, Poskitt EM, Whitehead RG. Effects on birth weight and perinatal mortality of maternal dietary supplements in rural Gambia: 5-year randomised controlled trial. BMJ. 1997;315:786–790. doi: 10.1136/bmj.315.7111.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chilima DM, Kalimbiria AA, Mtimuni BM, Mvula N. Surveillance of Micronutrient Programmes in Malawi. Lilongwe, Malawi: Likuni Press and Publishing House; [Google Scholar]
- 43.Brown KH, Dewey K, Allen L. Complementary feeding of young children in developing countries: A review of current scientific knowledge. Geneva: WHO/NUT/98.1; 1998. [Google Scholar]
- 44.Dewey KG. Success of intervention programs to promote complementary feeding. In: Black RE, Michaelsen KF, editors. Public health issues in infant and child nutrition. Philadephia: Nestle Nutrition Workshop Series, Nestec Ltd, Vevey/Lippincott Williams & Wilkins; 2002. pp. 199–216. [Google Scholar]
- 45.Schroeder DG, Martorell R, Rivera JA, Ruel MT, Habicht J-P. Age differences in the impact of nutritional supplementation on growth. J Nutr. 1995;125(suppl):1051–1059. doi: 10.1093/jn/125.suppl_4.1051S. [DOI] [PubMed] [Google Scholar]
- 46.Briend A, Lacsala R, Prudhon C, Mounier B, Grellety Y, Golden MH. Ready to use therapeutic food for treatment of marasmus. Lancet. 1999;353:1767–1768. doi: 10.1016/S0140-6736(99)01078-8. [DOI] [PubMed] [Google Scholar]
- 47.Stubbs J, Ferres S, Horgan G. Energy density of foods: effects on energy intake. Crit Rev Food Sci Nutr. 2000;40(6):481–515. doi: 10.1080/10408690091189248. [DOI] [PubMed] [Google Scholar]
- 48.Yao M, Roberts SB. Dietary energy density and weight regulation. Nutr Rev. 2001;59(8):247–258. doi: 10.1111/j.1753-4887.2001.tb05509.x. [DOI] [PubMed] [Google Scholar]
- 49.Collins S. Changing the way we address severe malnutrition during famine. Lancet. 2001;358:498–501. doi: 10.1016/S0140-6736(01)05630-6. [DOI] [PubMed] [Google Scholar]
- 50.Diop EI, Dossou NI, Ndour MM, et al. Comparison of the efficacy of a solid ready to use food and a liquid milk-based diet for the rehabilitation of severely malnourished children: a randomized trial. Am J Clin Nutr. 2003;78:302–307. doi: 10.1093/ajcn/78.2.302. [DOI] [PubMed] [Google Scholar]
- 51.Manary MJ, Ndekha MJ, Ashorn P, Maleta K, Briend A. Some-based therapy for severe malnutrition with ready-to-use food. Arch Dis Child. 2004;89(6):557–561. doi: 10.1136/adc.2003.034306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lutter CK, Mora JO, Habicht J-P, Rasmussen KM, Robson DS, Guillermo Herrera M. Age specific responsiveness of weight and length to nutritional supplementation. Am J Clin Nutr. 1990;51:359–364. doi: 10.1093/ajcn/51.3.359. [DOI] [PubMed] [Google Scholar]
- 53.Simondon KB, Gartner A, Berger J, Cornu A, Massamba JP, San Miguel JL, Ly C, Missotte I, Simmondon F, Traisac P, Delpeuch F, Maire B. Effect of early, short term supplementation on weight and linear growth of 4-7mo-old infants in developing countries: a four-country randomized trial. Am J Clin Nutr. 1996;64:537–545. doi: 10.1093/ajcn/64.4.537. [DOI] [PubMed] [Google Scholar]
- 54.Lartey A, Manu A, Brown KH, Pearson JM, Dewey KG. A randomised community based trial of the effects of improved, centrally processed complementary foods on growth and micronutrient status of Ghanaian infants from 6 to 12 mo of age. Am J Clin Nutr. 1999;70:391–404. doi: 10.1093/ajcn/70.3.391. [DOI] [PubMed] [Google Scholar]
- 55.Beaton GH, Ghassemi H. Supplementary feeding programs for young children in developing countries. Am J Clin Nutr. 1982;35:864–916. doi: 10.1093/ajcn/35.4.864. [DOI] [PubMed] [Google Scholar]
- 56.MICAH, author. World Vision Malawi. 1998. Survey report. [Google Scholar]
- 57.Chilima DM, Kalimbira A, Chanje DI. Enukweni and Engucwini Nutrition Survey 2002. 2002 Consultancy report: Christian Children's Fund of Great Britain.
- 58.Chilima D. School Health and Nutrition Programme in Malawi
- 59.Briend A. Is diarrhoea a major cause of malnutrition among under-five year old children in developing countries? Eur J Clin Nutr. 1990;44:611–628. [PubMed] [Google Scholar]
- 60.Briend A, Hasan KHZ, Aziz KMA, Hoque BA. Are diarrhoea control programmes likely to reduce childhood malnutrition? Observations from rural Bangladesh. Lancet. 1989;2:319–322. doi: 10.1016/s0140-6736(89)90498-4. [DOI] [PubMed] [Google Scholar]
- 61.Reddy V, Bhashkaram P, Raghuramulu N, Milton RC, Rao V, Madhusudan J, Krishna KV. Relationship between measles, malnutrition, and blindness: a prospective study in Indian children. Am J Clin Nutr. 1986;50:924–930. doi: 10.1093/ajcn/44.6.924. [DOI] [PubMed] [Google Scholar]
- 62.Rowland MGM, Cole TJ, Whitehead RG. A quantitative study into the role of infection in determining nutritional status in Gambian village children. Br J Nutr. 1977;37:441–450. doi: 10.1079/bjn19770047. [DOI] [PubMed] [Google Scholar]
- 63.Duggan MB, Alwar J, Milner RDG. The nutritional cost of measles in Africa. Arch Dis Child. 1986;61:61–66. doi: 10.1136/adc.61.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Esrey SA, Feachem RG, Hughes JM. Interventions for the control of diarrhoeal diseases among young children: improving water supplies and excreta disposal facilities. Bull World Health Organ. 1985;63:757–772. [PMC free article] [PubMed] [Google Scholar]
- 65.Jelliffe EFP, Jelliffe DB. Algorithms, growth monitoring and nutritional interventions. J Trop Paediatr. 1987;33:290–295. doi: 10.1093/tropej/33.6.290. [DOI] [PubMed] [Google Scholar]
- 66.Hendratta L, Rohde JE. Ten pitfalls of growth monitoring promotion. Indian Journal of Paediatrics. 1988;55(suppl):S9–S15. doi: 10.1007/BF02810384. [DOI] [PubMed] [Google Scholar]
- 67.Ramalingaswami V, Johnsson U, Rohde J. Progress of Nations. New York: UNICEF; 1996. The Asian Enigma. [Google Scholar]
- 68.Penny ME, Creed-Kanashiro HM, Robert RC, Narro MR, Caulfield ME, Black RE. Effectiveness of an educational intervention delivered through the health services to improve nutrition in young children: a cluster-randomised comtrolled trial. Lancet. 2005:365–370. doi: 10.1016/S0140-6736(05)66426-4. [DOI] [PubMed] [Google Scholar]
- 69.Brown KH, Dewey KG, Allen LH. Complementary feeding of young children in developing countries: A review of current scientific knowledge. Geneva: WHO; 1998. [Google Scholar]