Abstract
Objective
The purpose of this study was to assess postoperative complications and patient satisfaction associated with mid-level provision of male circumcision in rural Kenya.
Methods
A prospective cohort study was conducted among children, adolescents, and adult men undergoing male circumcision from September 1, 2008 to December 4, 2008 at Marie Stopes International Kenya mobile outreach sites located in eight districts in the Nyanza and Western Provinces, Kenya. Male circumcision procedures were performed by registered nurses, surgical technicians, or nurse aides. Postoperative follow-up visits took place on the day of the procedure and at postoperative days 3, 7, and 30, with additional visits as necessary. Data on adverse events, healing conditions, satisfaction level, and resumption of activities were assessed at each follow-up visit.
Results
A total of 285 individuals were screened, and 240 underwent male circumcision procedures. All procedures were performed using the guided forceps technique by mid-level providers. At the first follow-up visit (postoperative day 3), 5.8% (n = 14) individuals did not return for post-surgical assessment. Retention rates at the second (day 7) and third (day 30) follow-up visits were 91.3% (n = 219) and 84.6% (n = 203), respectively. The prevalence of complications (moderate and severe adverse events) was 1.3% (3/240). At the first and second follow-up visits, 91.7% of patients (n = 220) were capable of resuming their daily activities, and 100% by day 30. The majority of patients (>99%) were satisfied with the procedure, counseling, and information received.
Conclusion
Male circumcisions can be delivered safely and successfully by mid-level providers in rural settings with high client satisfaction, thereby increasing access to human immunodeficiency virus prevention services in Kenya.
Keywords: male circumcision, human immunodeficiency virus, reproductive health, mid-level providers, Kenya
Introduction
Scaling up male circumcision programs can potentially have a large impact on the human immunodeficiency virus (HIV) epidemic. Three randomized controlled trials have shown that male circumcision reduces the risk of heterosexual transmission of HIV by approximately 50%–60%.1–3 Mathematical modeling estimates that six million new HIV infections and three million deaths could be prevented over the next 20 years if all men in sub-Saharan Africa became circumcised.4
The World Health Organization (WHO) and the Joint United Nations Program on HIV/AIDS (UNAIDS) state that scaling up male circumcision services could provide a rare opportunity to reach adolescent boys and young men with comprehensive reproductive health information and services.5,6 In sub-Saharan Africa, cultural hurdles, financial constraints, and a shortage of skilled practitioners pose tremendous challenges for the implementation of mass circumcision services.7 Nevertheless, there has been growing support for widespread availability and accessibility of male circumcision services.7 In Kenya, the Male Circumcision Consortium together with government and local partners worked closely in the development and implementation of the national male circumcision strategy in 2008.8
As a member of the Male Circumcision Consortium, Marie Stopes International Kenya (MSI Kenya) integrated male circumcision services into its mobile outreach reproductive health program by training mid-level providers to perform male circumcision services in rural settings.8 From June 2007 to November 2008, MSI Kenya mobile outreach program performed a total of 5000 procedures (300 procedures per month) in Nyanza and Western Provinces, Kenya.
However, little has been done to assess adverse events or complications among scaled-up male circumcision programs. In a systematic review of complications of male circumcision in Anglophone Africa, Muula et al noted that the available data were inadequate to obtain a prevalence measurement.9 Serious complications and adverse events following improperly performed male circumcision procedures, including hematoma, penile amputation, and death, have also been documented.10–12 In a study of 1007 males in Western Kenya, Bailey et al found that 25% of circumcised males experienced an adverse event (35% in traditional circumcisions, 18% in clinical settings).10 These serious complications resulted from poor training, lack of appropriate clinical settings, and inadequate patient follow-up.
The primary objective of this study was to assess postoperative complications and satisfaction associated with mid-level provision of male circumcision in Nyanza and Western Provinces, Kenya. The main outcomes of interest were the prevalence of moderate and severe adverse events, the ability of the client to resume normal activities, and client satisfaction level.
Materials and methods
Study design
A prospective cohort study was conducted among children, adolescents, and adult men receiving male circumcision procedures from September 1, 2008 to December 4, 2008 at MSI Kenya mobile outreach sites located in eight districts in the Nyanza and Western Provinces, Kenya. Postoperative follow-up visits took place on the day of the procedure and at postoperative days 3, 7, and 30, with additional visits as necessary. At these follow-up visits, adverse events, healing conditions, client satisfaction, and resumption of activities were assessed. This study was approved by the ethics and research committee of the Kenyatta National Hospital in Nairobi, Kenya, and was conducted with support from Family Health International, the National AIDS and STI Control Program (NASCOP), the Ministry of Health, and the Nyanza Reproductive Health Society.
Study setting and population
The study sites comprised of local communities and health facilities in Nyanza Province (Kisumu West, Kisumu East, Nyando, Siaya, and Bondo) and Western Province (Teso, Butere, and Vihiga) where the MSI Kenya mobile outreach program operates (Figure 1). These sites were selected for the study because they are traditionally noncircumcising communities, and are where MSI Kenya has its mobile outreach operations.
Figure 1.
Study setting: Nyanza and Western Provinces, Kenya.
Notes: Nyanza Province is a noncircumcising region with a human immunodeficiency virus incidence that is 13% above the national average.13 Western Province has a large population living in the rural communities.
Image source: Used with permission by Marie Stopes International.
We recruited males who were 2–60 years of age, capable of signing an informed consent or having a guardian (or parent) willing to sign the document, willing to return for postoperative follow-up visits, willing to undergo physical examination of the penis after circumcision, and capable of answering questions about the male circumcision procedure, sexual activity, and condom use (if applicable). Individuals with known health problems or diseases which might cause adverse events, such as hemophilia and genital ulcer disease, were not included in the study. Study participants were reimbursed for transportation costs.
Study procedures
On the enrolment day, the study participants were asked to provide their consent for surgery, and were given counseling information on the procedure, postoperative wound care, and the need to abstain from sexual intercourse (if applicable) until complete wound healing (examined and certified by medical personnel). Voluntary HIV testing and counseling were offered to all study participants. Information such as demographic and sexual behavioral characteristics (if applicable) and reasons for undergoing circumcision were collected from the study participants or their guardians/parents. Patients were given enrolment cards, and were asked to return to the same mobile outreach site for postoperative follow-up visits.
On the day of surgery, all 240 participants were given lignocaine prior to the procedure, and 238 received paracetamol afterwards. All 240 procedures were performed using the guided forceps technique by mid-level providers (registered nurse, medical technician, and nurse aide). The majority of the procedures (226/240, 94.2%) were performed by registered nurses, five by a surgical technician, and nine by a nurse aide. These mid-level providers received clinical training in male circumcision in accordance with national and international guidelines from the Johns Hopkins Program for International Education in Gynecology and Obstetrics. After the procedure, study participants were evaluated by medical personnel either urgently due to immediate complications or electively in outpatient clinics subsequent to completion of the procedure.
At the time of the procedure and at each of the three follow-up visits, trained medical personnel examined the penis to confirm circumcision status and determine the presence and type of any adverse events. At each visit, a detailed face-to-face interviewer-administered questionnaire was used to obtain data on the perception of circumcision services. Emergency contacts were given to all participants, and care was available for any study participants wishing to see a medical professional between follow-up visits. Loss to follow-up was defined as failure to return for scheduled postoperative appointments.
Safety
Adverse events related to surgery were predefined and graded as mild (requiring no treatment), moderate (requiring treatment), or severe complications (requiring surgical intervention, ie, wound exploration for active bleeding, repair of wound dehiscence, hospitalization, or referral for specialized care). Surgery-related adverse events were detected at scheduled postoperative follow-up visits. Grade 1 or mild adverse events required no or minimal treatment, whereas grade 2 (moderate) and grade 3 (severe) adverse events required medical or surgical intervention. Thus, moderate and severe adverse events were most relevant to assessment of safety. The definition of these adverse events followed the guidelines of the WHO and Kenya NASCOP for male circumcision.14–16 Complications were defined as adverse events at grade 2 (moderate) and grade 3 (severe). According to the WHO and Kenya NASCOP guidelines, adverse events graded as mild were defined as side effects because they were not considered to be dangerous or life-threatening, and required no treatment.
Data analysis
Statistical analyses were performed using Intercooled Stata 10.0 (Stata Statistical Software for Professionals: Release 10, StatCorp LP, College Station, TX). The prevalence of adverse events (or complications), patient compliance, resumption of normal activities, and patient satisfaction were described.
Results
Cohort profile
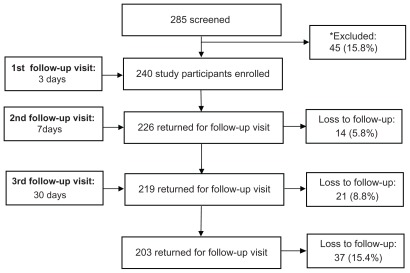
Two-hundred and eighty-five individuals were screened, of whom 240 were enrolled and underwent a circumcision procedure. Of the 45 individuals who were excluded from the study, 27 indicated that they were not able to come back for follow-up visits due to distance or other obligations, seven did not meet the age requirement, three had genital ulcers and were referred for treatment, two were unwilling to give informed consent, and six refused to participate (Figure 2).
Figure 2.
Cohort profile: a total of 240 study participants underwent male circumcision procedures.
Notes: *Among these 45 individuals, 27 were excluded because they indicated that they were not able to return for follow-up visits due to distance or other obligations, seven did not meet the age requirement, three had genital ulcer disease referred for treatment, two were unwilling to provide informed consent, and six refused to participate.
At the first follow-up visit (3 days postoperative), 14 of the 240 (5.8%) individuals did not return for postoperative assessment. The retention rate at the second follow-up visit (7 days) was 91.3% (219/240), and 84.6% (203/240) for the third follow-up visit (30 days). The overall rate of loss to follow-up was 15.4% (37/240, see Figure 2).
Study population characteristics
The 240 study participants came from eight districts in the Nyanza and Western Provinces. Approximately 49% of the study participants came from the Kisumu East and Kisumu West districts, while the other 51% were recruited from Nyando, Bondo, Siaya, Tesco, Busia, and Emuhaya districts.
The median age was 20 ± 8.9 years (interquartile range 17–26); 17.9% (43/240) of the study participants were aged <15 years, 65.8% (158/240) were aged 15–29 years, and 16.3% (39/240) were aged >30 years. The educational level was low among this population, in which only 35.8% (n = 86) had secondary education or higher, and 63.8% had no or primary education only (n = 153). Only 21.8% (n = 43) of the participants were employed, while the rest were unemployed (n = 154) or under the age of 15 years (n = 43). Among those who were older than 15 years of age (n = 197), the majority were single (n = 135, 68.5%) and the rest were currently married (n = 39, 19.8%) or divorced/separated (n = 23, 11.7%, Table 1).
Table 1.
Demographic and behavioral characteristics of 240 study participants
| Characteristics | Overall sample n = 240 |
|---|---|
| n (%) | |
| Age (years) | |
| <15 | 43 (17.9) |
| 15–19 | 68 (28.3) |
| 20–24 | 57 (23.8) |
| 25–29 | 33 (13.8) |
| 30+ | 39 (16.3) |
| Education | |
| None/primary | 153 (63.8) |
| Secondary | 75 (31.2) |
| Post-secondary/tertiary | 12 (5.0) |
| Employment* | |
| Yes | 43 (21.8) |
| No | 154 (78.1) |
| Marital status* | |
| Currently married | 39 (19.8) |
| Separated/divorced | 23 (11.7) |
| Never married | 135 (68.5) |
| Behavioral characteristics | |
| Reasons for circumcision | |
| Partial protection against HIV | 230 (95.8) |
| Others (social/religious; personal hygiene) | 10 (4.2) |
| Sexually active, currently* | |
| Yes | 127 (64.5) |
| No | 70 (35.5) |
| Been tested for HIV in the past | |
| Yes | 62 (25.8) |
| No | 178 (74.2) |
Note:
Study participants <15 years of age were taken out of the analysis for employment, marital status, and current sexual activity.
Abbreviation: HIV, immune deficiency virus.
The main reason for undergoing circumcision was for partial protection against HIV (n = 230, 95.8%); the rest underwent the procedure for social/religious reasons and to improve personal hygiene. Among the 127 individuals who were currently sexually active, 70 (55.1%) had had a casual sexual partner within the previous 6 months. Among all the study participants, 25.8% (n = 62) had been tested for HIV infection in the past.
Safety
Moderate to severe adverse events
Of the 240 procedures, there were three adverse events that were considered to be complications. These three cases represented an overall complication rate of 1.3% using the WHO and Kenya NASCOP guidelines. Among these complications, one case of severe pain and one case of a moderate anesthetic-related event occurred on the day of the procedure, while one case of moderate infection was observed at the day 7 follow-up visit. These adverse events that occurred on the day of the procedure were fully resolved at the first follow-up visit (day 3 postoperatively). The one case of moderate infection observed at the second follow-up visit (day 7) had been successfully treated by the third follow-up visit (30 days). No study participants sought urgent care through the emergency care service of MSI Kenya mobile outreach team between the preplanned follow-up visits.
Mild adverse events
The prevalence of self-reported side effects was 56.3% on the day of the procedure; 21.1% at the first follow-up visit, 23.2% at the second follow-up visit, and 3.9% at the third follow-up visit. The prevalence of self-reported side effects at day 30 was 63.5%. A wide range of side effects was reported, including 38.5% pain, 21.9% bleeding, 18.1% swelling, 5.0% infection, 1.7% anesthetic-related events, and 0.9% hematoma. Due to the mild nature of these side effects, they were not considered to be dangerous or life-threatening according to the WHO and Kenya NASCOP guidelines.
Postoperative activity and satisfaction
The majority of study patients (99%) were satisfied with the counseling process, the information received, and the outcome of the circumcision procedure at all three follow-up visits. Approximately, 91.7% of the study participants were capable of resuming work/normal activities at the day 3 or 7 follow-up visit. Those who were unable to return to normal activities reported that they were feeling “unwell”. All study participants were able to resume daily activities by day 30.
Discussion
This study demonstrates that male circumcision performed by mid-level providers in rural settings in Nyanza and Western Provinces is safe, with high client satisfaction. The 1.3% complication rate among 240 procedures is comparable with that reported in the three randomized controlled trials1–3 and in a study of 19,478 male infant circumcisions conducted in Israel.17 The majority of the study participants were satisfied with their circumcision procedure, and all were able to resume normal activities by postoperative day 30. To our knowledge, this is the first prospective cohort study conducted in a rural setting outside a controlled clinical environment, with procedures carried out by mid-level providers.
Two factors that might contribute to the low complication rate in our study were use of the guided forceps technique and the competence of the practitioner. Two separate studies in Kenya and Nigeria that evaluated adverse events related to male circumcision showed high complication rates (15% and 43%).18,19 These two studies attributed the high complication rates to their techniques (plastic bell method and traditional method) that were performed by poorly trained performers. Compared with these two studies, the guided forceps method used in our study might have been easier to learn and perform by mid-level providers. All the practitioners in this study were registered nurses, medical technicians, and nurse aides who received adequate training by the Johns Hopkins Program for International Education in Gynecology and Obstetrics, as opposed to traditional surgeons involved in the other two cited studies.18,19
There are several limitations to this study. The overall rate of loss to follow-up was relatively high at 15.4% (n = 37), which may have led to either an underestimation or overestimation of complication rates. However, given that all individuals were given emergency contact information, the 37 individuals who did not return for follow-up visits might not have experienced serious adverse events. However, we were unable to locate these individuals to find out about their experience with the procedure.
Furthermore, the high proportion of self-reported side effects at the first follow-up visits included pain, bleeding, and swelling. These side effects are expected after a surgical procedure, which suggests that the study participants may not have been counseled sufficiently to distinguish between expected and unexpected adverse events. In addition, our prospective cohort study only took place over a 3-month period, so we were not able to provide counseling to the sex partners of the study participants or to continue with long-term follow-up. Further, we were unable to obtain the number of study participants who abstained from sexual activity during each follow-up visit, and our questionnaire had limited ability to obtain detailed sexual behavior, such as postoperative sexual encounters and satisfaction. Lastly, this study was not able to compare postoperative complications and patient satisfaction level with male circumcision provided by mid-level providers or surgeons.
Participants reported a very high satisfaction rate (99%) with regard to the surgical procedure, counseling services, information received, and the final cosmetic outcome of the procedure. All study participants (100%) were capable of resuming daily activities by day 30. These results indicate that male circumcision can be performed safely by mid-level providers with a good level of satisfaction. Cultural hurdles remain one of the biggest challenges to mass implementation of male circumcision in sub-Saharan Africa.6 Our study suggests that provision of male circumcision is feasible in rural Nyanza, a traditionally noncircumcising Luo community with a high HIV prevalence.13 This is attributed to the extensive experience of MSI Kenya in providing sexual and reproductive health services in Nyanza. Furthermore, MSI Kenya worked closely with the local community, government, and other key stakeholders, such as local and international nongovernmental organizations when conducting the study.
Male circumcision for HIV prevention has gained increasing support from researchers, donors, and politicians. However, there are numerous challenges to scaling up, given its status as a biomedical intervention.20 Even in rural settings, our study shows that male circumcision can be provided safely by mid-level providers. It is projected that 60 million new HIV infections will occur by 2015 if the current rates are not reversed.9 In order to halt the epidemic in sub-Saharan Africa, it is time to scale up male circumcision services aggressively. Mass scaling up of male circumcision in countries with a high HIV prevalence would require training a different cadre of mid-level providers, with provision of a comprehensive prevention package, including voluntary counseling and testing services, treatment for sexually transmitted infections, promotion of safer sex, and provision of condoms.
Acknowledgments
The authors extend their appreciation to Heidi Quinn and Tania Boler at Marie Stopes International for their critical review of the manuscript. We would also like to thank all the clinicians and field staff who dedicated a tremendous amount of time and commitment to the study.
Footnotes
Disclosure
The authors work for MSI, an organization that provides male circumcision services in Kenya and also provided funding for this study.
References
- 1.Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med. 2005;2:1112–1122. doi: 10.1371/journal.pmed.0020298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;69:643–656. doi: 10.1016/S0140-6736(07)60312-2. [DOI] [PubMed] [Google Scholar]
- 3.Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369:657–666. doi: 10.1016/S0140-6736(07)60313-4. [DOI] [PubMed] [Google Scholar]
- 4.Williams BG, Lloyd-Smith JO, Gouws E, et al. The potential impact of male circumcision on HIV in sub-Saharan Africa. PLoS Med. 2006;3:1032–1040. doi: 10.1371/journal.pmed.0030262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. WHO and UNAIDS announce recommendations from expert consultation on male circumcision for HIV prevention, 2007. [Accessed February 25, 2012]. Available from: http://www.who.int/mediacentre/news/releases/2007/pr10/en/index.html.
- 6.World Health Organization. Glion consultation on strengthening the linkages between reproductive health and HIV/AIDS: family planning and HIV/AIDS in women and children. 2004. [Accessed February 25, 2012]. Available from: http://www.who.int/reproductive-health/stis/docs/glion_consultationsummary.pdf.
- 7.Pincock S. Workforce biggest barrier to roll-out of male circumcision. Lancet. 2007;370:1817–1818. doi: 10.1016/S0140-6736(07)61759-0. [DOI] [PubMed] [Google Scholar]
- 8.Kaiser Daily HIV/AIDS report. Global challenges: Kenya launches male circumcision program. 2008. [Accessed February 25, 2012]. Available from: http://www.kaisernetwork.org/Daily_reports/rep_index.cfm?DR_ID=55734.
- 9.Muula AS, Prozesky HW, Mataya RH, Ikechebelu JI. Prevalence of complications of male circumcision in Anglophone Africa: a systematic review. BMC Urol. 2007;7:4. doi: 10.1186/1471-2490-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bailey RC, Egesah O, Rosenberg S. Male circumcision for HIV prevention: a prospective study of complications in clinical and traditional settings in Bungoma, Kenya. Bull World Health Organ. 2008;86:669–677. doi: 10.2471/BLT.08.051482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krieger JN, Bailey RC, Opeya J, et al. Adult male circumcision: Results of a standardized procedure in Kisumu District, Kenya. BJU Int. 2005;96:1109–1113. doi: 10.1111/j.1464-410X.2005.05810.x. [DOI] [PubMed] [Google Scholar]
- 12.Opeya CJ, Ayieko BO, Kawango A, et al. Adult male circumcision in Kenya: safety and patient satisfaction (Abstract TuPeB4648). International AIDS Conference; Bangkok, Thailand. July 11–16 2004. [Google Scholar]
- 13.National AIDS and STI Control Programme, Ministry of Health, Kenya. Kenya AIDS Indicator Survey 2007: preliminary report. Nairobi, Kenya: 2008. [Accessed February 25, 2012]. Available from: http://www.aidskenya.org/public_site/webroot/cache/article/file/KAIS__Preliminary_Report.pdf. [Google Scholar]
- 14.World Health Organization/Joint United Nations Program on HIV/AIDS. Operational guidance for scaling up male circumcision services for HIV prevention. 2008. [Accessed February 25, 2012]. Available from: http://www.malecircumcision.org/programs/documents/MC_OpGuideFINAL_web.pdf.
- 15.World Health Organization. Joint United Nations Program on HIV/AIDS and Johns Hopkins Program for International Education in Gynecology and Obstetrics. Manual for male circumcision under local anaesthesia, Version 2.5C. 2008. [Accessed February 25, 2012]. Available from: http://www.malecircumcision.org/programs/documents/WHO_MC_Manual_Local_Anaesthesia_v2-5C_Jan08.pdf.
- 16.National AIDS and STD Control Programme (NASCOP) Guidelines for safe, voluntary medical male circumcision in Kenya. Ministry of Health; 2008. [Accessed March 22, 2012]. Available from: http://www.malecircumcision.org/programs/documents/Kenya_VMMC_Report_01.2012.pdf. [Google Scholar]
- 17.Ben Chaim J, Livne PM, Binyamini J, Hardak B, Ben-Meir D, Mor Y. Complications of circumcision in Israel: a one year multicenter survey. Isr Med Assoc J. 2005;7:368–370. [PubMed] [Google Scholar]
- 18.Magoha GA. Circumcision in various Nigerian and Kenyan hospitals. East Afr Med J. 1999;76:583–586. [PubMed] [Google Scholar]
- 19.Osuigwe AN. Circumcision-related complications in the male: experience amongst the Igbo’s of Southeast Nigeria. Afr J Urol. 2004;10:246–251. [Google Scholar]
- 20.Katz IT, Wright AA. Circumcision-a surgical strategy for HIV prevention in Africa. N Engl J Med. 2008;359:2412–2415. doi: 10.1056/NEJMp0805791. [DOI] [PMC free article] [PubMed] [Google Scholar]