Abstract
Background:
Little is known regarding the epidemiology of chronic rhinosinusitis (CRS) in racial and ethnic minorities in the United States. This study was designed to comprehensively evaluate the current prevalence of CRS across various treatment settings to identify possible disparities in health care access and use between racial and ethnic populations.
Methods:
The National Health Interview Survey (NHIS), National Ambulatory Medical Care Survey (NAMCS), and National Hospital Ambulatory Medical Care Survey (NHAMCS) database registries were extracted to identify the national prevalence of CRS in race/ethnic populations and resource use in ambulatory care settings. Systematic literature review identified studies reporting treatment outcomes in minority patients electing endoscopic sinus surgery (ESS). Data were supplemented using a multi-institutional cohort of patients undergoing surgical treatment.
Results:
National survey data suggest CRS is a significant health condition for all major race/ethnic groups in the United States, accounting for a sizable portion of office, emergency, and outpatient visits. Differences in insurance status, work absenteeism, and resource use were found between race/ethnic groups. Despite its prevalence, few published studies include information regarding minority patients with CRS. Most (90%) cohort studies did not provide details of race/ethnicity for ESS outcomes. Prospective cohort analysis indicated that minority surgical patients accounted for only 18%, when compared with national census estimates (35%).
Conclusion:
CRS is an important health condition for all major race/ethnic groups in the United States. Significant differences may exist across racial and ethnic categories with regard to CRS health status and health care use. Given current demographic shifts in the United States, specific attention should be given to understanding CRS within the context of racial and ethnic populations. Public clinical trial registration (www.clinicaltrials.gov) I.D. No. NCT00799097.
Keywords: Centers for Disease Control and Prevention, continental population groups, database, ethnology, outcomes research, prevalence, quality of life, registries, sinusitis, United States
Minority racial and ethnic groups make up 35% of the current U.S. population, with African Americans representing 12.6%, Hispanic or Latinos representing 16.3%, and Asian Americans representing 4.8%.1 Although non-Hispanic white Americans accounted for 85% of the population in 1960, the Pew Research Center estimates that by 2050, non-Hispanic white Americans will make up only 47% of the population.2 This dramatic population shift has important implications on health care delivery in the United States. Over the last 30 years, a large body of evidence has documented differences in health outcomes between racial and ethnic groups for a wide range of indices, including infant mortality, overall mortality, cardiovascular disease, and cancer incidence.3,4 The reason for these disparities is complex and is often mediated by socioeconomic inequalities that impact health, health behaviors, and access to health care resources.5
The U.S. Department of Health and Human Services launched Healthy People 2020 with the goal of understanding social determinants of health, eliminating disparities between groups, and improving overall access to care.6 At present, very little is known regarding the epidemiology of chronic rhinosinusitis (CRS) as it relates to racial and ethnic minorities. Most published studies have been limited to case–control series focusing on patients with allergic fungal sinusitis.7–11 Although several studies have reported national statistics detailing CRS prevalence and ambulatory care use, none have focused on minority populations.12,13 Additionally, few primary studies reporting outcomes after CRS treatments have provided data on racial and ethnic subgroups. The result is a large knowledge gap regarding the prevalence and impact of CRS in a substantial segment of the U.S. population. Given that considerable quality-of-life (QOL) declines are seen in patients with CRS, a significant burden of disease may exist in minority populations that remains unappreciated. The primary goal of this study was to evaluate national health registries for the current prevalence of CRS across various treatment settings to identify potential disparities in both access and health care use between racial and ethnic minorities in the United States. The secondary goal was to systematically review published studies reporting outcomes after endoscopic sinus surgery (ESS) in minority patients, supplementing this data with in-depth analysis of a multi-institutional cohort.
MATERIALS AND METHODS
National Health Interview Survey
Data from the National Health Interview Survey (NHIS) were accessed using the Integrated Health Interview Series.14 The NHIS is a yearly cross-sectional household interview survey conducted by the Centers for Disease Control and Prevention (CDC).15 The goal of the NHIS is to monitor the health of the civilian, noninstitutionalized U.S. population, primarily for the purpose of monitoring trends in illness and tracking progress toward achieving national health objectives. Variables extracted from the overall data set for the year 2009 (most recent data release) included adults that were “told they had sinusitis during the past 12 months,” self-reported race (white and African American and Asian), self-reported ethnicity (Hispanic/Latino), insurance status, medical specialist visitation, surgical procedures, inability to work because of health, and delays in medical treatment due to cost.
Data were imported into statistical software (STATA v.11.1; StataCorp, College Station, TX) and cross-referenced with publicly reported records for accuracy. Observations were stratified into groups with and without sinusitis as well as along racial and ethnic categories. Complexities inherent in the initial study design were respected using sampling weights for each observation, ensuring appropriate standard errors. Descriptive statistics were compiled and comparisons among racial/ethnic groups were conducted using chi-square analysis at the 0.05 α-level.
National Ambulatory Medical Care Survey/National Hospital Ambulatory Medical Care Survey
The 2006 National Ambulatory Medical Care Survey (NAMCS) and National Hospital Ambulatory Medical Care Survey (NHAMCS) were accessed via publicly available data from the CDC.16 These surveys collect detailed information regarding patient visits to nonfederal physicians, emergency departments (EDs), and outpatient department (OD) care facilities. A patient visit was considered to be for CRS if the physician used a primary, secondary, or tertiary diagnostic code indicating chronic sinusitis. Information regarding race and ethnicity was captured using classifications similar to those in the NHIS. For each CRS visit, details regarding use of antibiotics, nasal steroids, and decongestants were recorded, as well as the provider's medical specialty where appropriate. To adequately capture comprehensive prescription patterns, drug categories were identified by collapsing the eight medication variables recorded at each visit and using only the first level (broadest category) of the Multum Lexicon therapeutic classification system (Cerner Multum, Inc., Denver, CO) for each medication. Data were analyzed using statistical software and the associated Complex Sampling Modules (SPSS v.19; SPSS, Inc., Chicago, IL) to accurately use patient weighted sampling methods. Differences in all prevalence measures between race/ethnic groups were assessed using chi-square tests at the 0.05 α-level. Prevalence values were compared with national estimates from the U.S. Census.1 Per CDC recommendations, data derived from the NAMCS and NHAMCS were not considered a reliable estimate if the relative standard error was >30% or if the variable had <30 total records. All patient parameters failing to meet those criteria were denoted with an asterisk.
Published Studies Reporting Surgical Outcomes for CRS
A literature review was performed using the U.S. National Library of Medicine to identify studies reporting efficacy outcomes for CRS after ESS.17 The search was conducted using exploded Medical Subject Headings corresponding to “sinusitis,” “endoscopic,” and “surgery.” References from systematic reviews on ESS outcomes were also scanned to ensure all relevant publications were identified. Studies were included if they were performed in the United States and reported either QOL or symptom-related outcomes after ESS on or after 1995. Case–control studies and case series with <20 subjects were excluded, as were recent studies reporting outcomes after balloon dilatation. Studies meeting inclusion/exclusion criteria were reviewed to identify the outcome measure of interest, total study size, sample size of minority patients, and whether a subgroup analysis was performed in minority groups. In those instances where more than one publication used the same underlying cohort, all studies were reviewed and those reporting race/ethnicity were selected for presentation. If none of the studies reported data on race or ethnicity, then data from the largest study were presented.
Subgroup Analysis of Multi-institutional Cohort
We have previously reported overall findings from a multi-institutional cohort of adult patients with CRS enrolled between July 2004 and April 2009.18 All subjects were diagnosed with CRS according to Task Force consensus criteria19 and elected to pursue ESS after failing initial medical management at three participating medical centers (Oregon Health Sciences University, Stanford University, and the Medical College of Wisconsin). Self-reported race and ethnicity were recorded according to the classification system required by the National Institutes of Health. Patients reported a racial classification of African American/black, American Indian/Alaskan Native, Asian, Native Hawaiian/Pacific Islander, or white/Caucasian. In addition to race, each patient was asked to report an ethnicity of either Hispanic/Latino or non-Hispanic/Latino. Additional demographic and socioeconomic characteristics included age, gender, education (years), and household income.
Baseline computed tomography (CT) scans and endoscopic exams were graded according to the Lund-Mackay and Lund-Kennedy scoring systems, respectively.20,21 Disease-specific QOL before and after ESS was evaluated using the Rhinosinusitis Disability Index (RSDI; range, 0–120) and the Chronic Sinusitis Survey (CSS; range, 0–100), with clinicians blinded to all QOL responses throughout the study's duration.22,23 Higher scores indicate worse QOL on the RSDI, and higher scores represent better QOL on the CSS instrument. The study protocol was approved by the Institutional Review Board at each medical center before enrollment. The Institutional Review Board at Oregon Health and Science University provided approval for this human subjects investigation.
Analyses were conducted using commercially available statistical software (SPSS v.19.0; SPSS, Inc.). For the uniformity of analyses, data were reorganized into non-Hispanic white, non-Hispanic African American, Hispanic, Asian, and Other. Although an “Other” category is not ideal, the small sample size was not conducive to meaningful analysis in the remaining racial groups. Demographic and socioeconomic characteristics among race/ethnicity groups were compared, as were differences in baseline CT and endoscopy scores. Baseline QOL responses were reported by race/ethnic category as well as the change after ESS, using the last available follow-up for analysis. One-way analysis of variance (ANOVA) and independent t-tests were used when continuous measures were normally distributed; Kruskal-Wallis and Mann-Whitney U tests were used for nonparametric distributions. Frequency differences were compared using Pearson's chi-square or exact test where appropriate, with means (SDs) reported throughout. Multivariate linear regression was used to examine whether or not significant differences in descriptive characteristics significantly confound the relationship between race/ethnicity and the changes in QOL outcomes. Confounding was determined to be present if there was a difference of ±10% in the effect estimate for each race/ethnicity variable.
RESULTS
National Health Interview Survey
A total of 27,731 U.S. residents responded to the NHIS in 2009, including 2380 African Americans, 610 Hispanics, 435 Asians, and 24,191 white adults. A diagnosis of sinusitis was reported by 13.8% of African Americans and 13.0% of white respondents, with lower prevalence seen in Hispanics (8.8%) and Asians (7.0%). Across all groups, those reporting sinusitis were more likely to be unable to work due to medical illness than those without sinusitis, with significant differences across race/ethnicity categories (Fig. 1; p < 0.001). The largest impact on work absenteeism for sinusitis patients was seen in African Americans, with just over 23% missing work in the past year. Significant differences in medical insurance status were seen across racial/ethnic groups (Fig. 2). In those with sinusitis, 24.3% of Hispanics were uninsured, compared with 17.6% of African Americans, 11.1% of white adults, and 10.5% of Asians (p < 0.001). Hispanics and African Americans with sinusitis were also more likely to delay medical care because of cost-related concerns than other groups (Fig. 3; both p < 0.001). With regard to treatment, white adults with sinusitis were more likely to have seen a medical specialist in the last 12 months and were more likely to have undergone a surgical procedure than other racial/ethnic groups (Fig. 4; p < 0.001 and p < 0.001, respectively).
Figure 1.
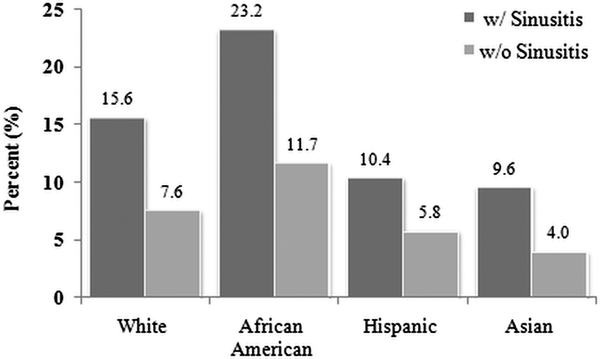
Percentage of U.S. adults unable to work because of medical problem. Data from the 2009 National Health Interview Survey. Respondents indicated whether a physical, mental, or emotional problem currently kept them from working at a job or business.
Figure 2.
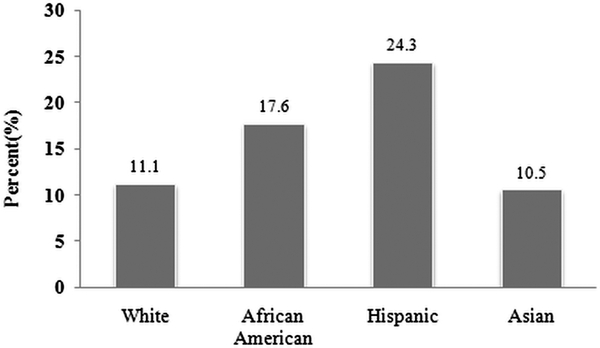
Percentage of sinusitis patients without medical insurance. Data from the 2009 National Health Interview Survey.
Figure 3.
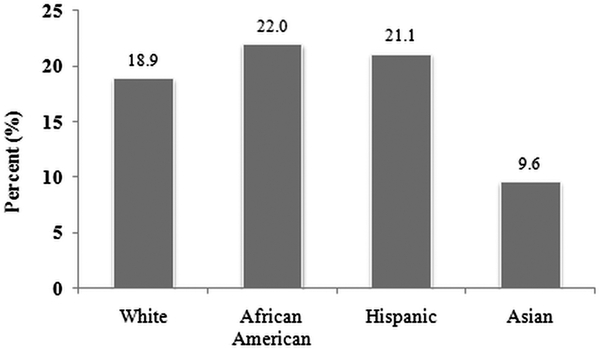
Percentages of adults with sinusitis delaying medical care because of worry about cost. Data from the 2009 National Health Interview Survey.
Figure 4.
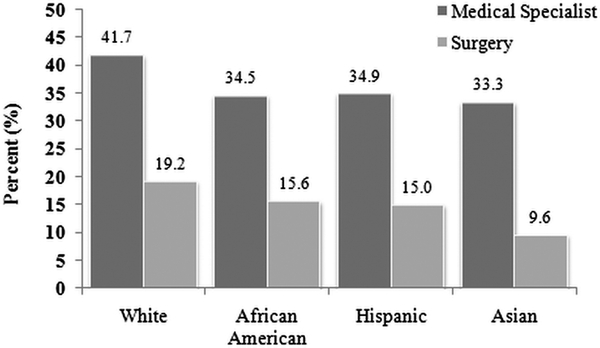
Percentage of adults with sinusitis visiting a medical specialist or undergoing surgery in the last 12 months. Data from the 2009 National Health Interview Survey. Includes both outpatient and inpatient surgical procedures.
National Ambulatory Medical Care Survey/National Hospital Ambulatory Medical Care Survey
CRS accounted for an estimated 20.3 million of 902 million (2.3%) total physician visits represented by the NAMCS in 2006. The frequency of CRS physician visits was similar across race/ethnic classifications: non-Hispanic white (2.3%), African American (2.7%), Hispanic/Latino (2.0%), and Asian (1.4%; (p > 0.050). The NHAMCS ED data estimated 1.2 million visits (1.0%) for CRS out of a total 119.2 million ED visits. The NHAMCS OD data estimated 2.3 million visits (2.3%) for CRS out of 102.2 million total OD visits. Non-Hispanic white patients accounted for a greater percentage of physician and outpatient visits for CRS, compared with population estimates from the 2010 U.S. census (Fig. 5). In comparison, African Americans accounted for ∼34.3% of ED visits, despite comprising only 12.6% of the U.S. population. A total of 47.5% of white patients had private insurance for ED visits, compared with only 29.5% of African Americans and 36.0% of Hispanic/Latinos (p < 0.001). Estimates of physician visits, stratified by provider, and frequencies of medications prescribed across race/ethnicity category were deemed unreliable because of insufficient sample size and/or large standard error.
Figure 5.
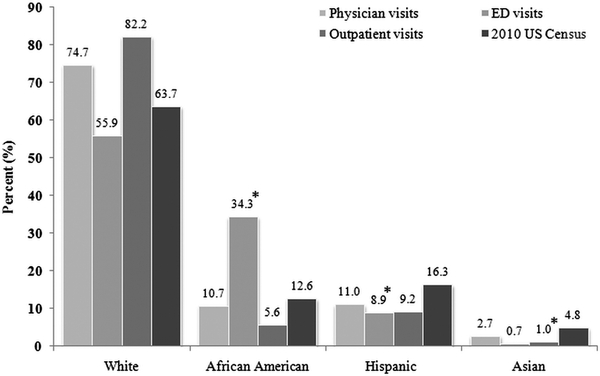
Percentage of patient visits for chronic rhinosinusitis by race/ethnicity. Data from 2006 National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Survey. Asterisk indicates unreliable population estimates because of insufficient sample size or relative standard error >30%.
Published Studies Reporting Surgical Outcomes for CRS
The literature review identified 1784 abstracts reporting surgical outcomes for CRS. After application of the prespecified inclusion/exclusion criteria, publications from 10 research groups were examined in detail and study characteristics were presented in tabular form (Table 1). Together, these studies examined outcomes for 1783 individuals with CRS, with 5 of 10 studies performed in a prospective fashion. Each study took place at a tertiary medical center between 1995 and 2010, with most occurring in large, urban cities. Data describing race and/or ethnicity of the study participants were not presented for 90% of these studies. For those authors with multiple publications, none of the excluded studies reported race or ethnicity data for study participants. The study by Smith et al. in 2010 did report the racial and ethnic makeup of study participants, with 35 of 302 patients from a minority group.18 However, subgroup analysis according to race/ethnicity was done only in a dichotomous fashion (white versus nonwhite), which allowed little inference regarding specific groups. Other prior publications from this same group have not presented detailed subgroup analysis according to specific racial and ethnic categories.
Table 1.
Race/ethnicity data in studies reporting efficacy outcomes after surgery in patients with CRS
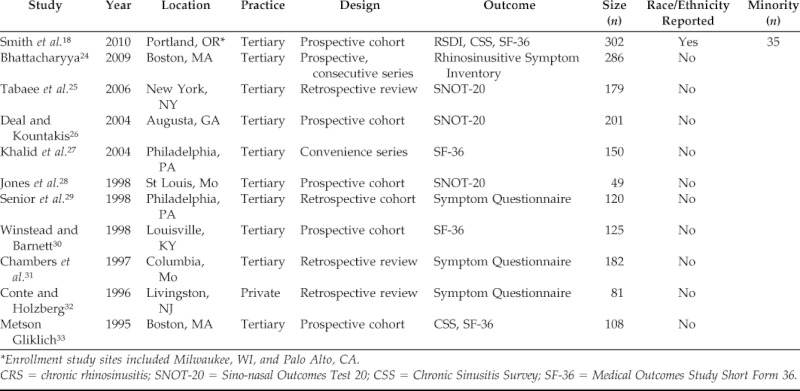
*Enrollment study sites included Milwaukee, WI, and Palo Alto, CA.
CRS = chronic rhinosinusitis; SNOT-20 = Sino-nasal Outcomes Test 20; CSS = Chronic Sinusitis Survey; SF-36 = Medical Outcomes Study Short Form 36.
Subgroup Analysis of Multi-institutional Cohort
A total of 518 adult patients with CRS were enrolled after electing to undergo ESS. Minority race/ethnic groups comprised 18.2% of the cohort, with 23 Asians (4.4%), 20 African Americans (3.9%), 11 Hispanics (2.1%), 4 American Indians (1%), and 4 Native Hawaiians (1%). Baseline demographic findings, clinical characteristics, and socioeconomic factors are shown in Table 2. Significant differences were seen across race/ethnicity classifications for gender distribution, smoking, education, and household income. Regarding objective measures of CRS, no differences were seen among race/ethnicity groups for CT, endoscopy, or olfaction scores (Table 3).
Table 2.
Demographic and clinical characteristics by race/ethnicity categories (n = 518)
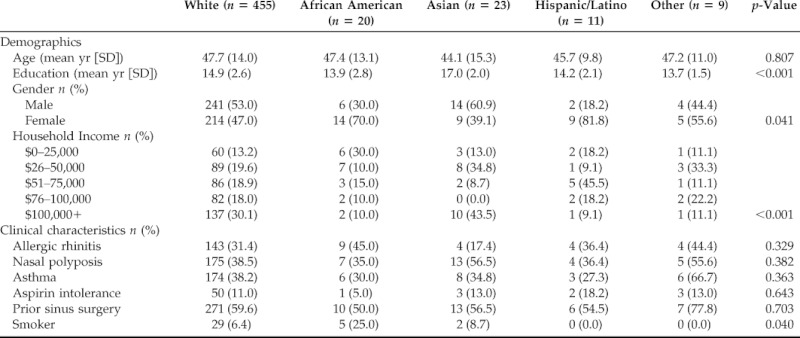
Table 3.
Objective CRS measures by race/ethnicity categories (n = 518)
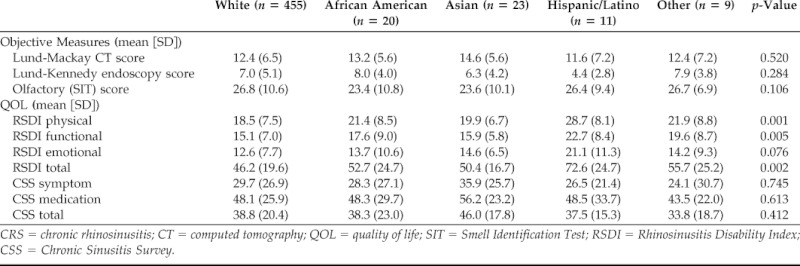
CRS = chronic rhinosinusitis; CT = computed tomography; QOL = quality of life; SIT = Smell Identification Test; RSDI = Rhinosinusitis Disability Index; CSS = Chronic Sinusitis Survey.
A significant difference in baseline QOL was observed among race/ethnicity groups for the total RSDI score as well as the physical and functional subscales (Table 3). These differences were not seen with the CSS instrument. Pairwise testing comparing white patients to minority groups showed a significant difference for RSDI responses from white patients when compared with Hispanic patients. Hispanic patients reported worse RSDI total scores (46.2 [19.6] versus 72.6 [24.7]; p < 0.001), physical subscale scores (18.5 [7.5] versus 28.7 [8.1]; p < 0.001), and functional subscale scores (15.1 [7.0] versus 22.7 [8.4]; p = 0.001). Using linear regression, race/ethnicity remained a significant predictor of total RSDI scores after controlling for demographic factors (age and sex), medical comorbidities (revision surgery, asthma, allergies, depression, and smoking), and socioeconomic (income and years of education) factors (p = 0.001).
QOL responses after ESS were available for 362 patients with >6 months follow-up. As a whole, the entire cohort showed significant improvements on all QOL measures after surgery (all p < 0.001). Change in QOL after surgery was compared across groups defined by race/ethnicity. No differences by race/ethnicity were seen for total RSDI, total CSS, or any mean subscale score (Table 4).
Table 4.
Postoperative changes in QOL measures across race/ethnicity categories (n = 362)
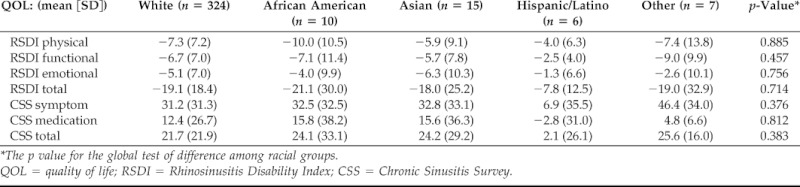
*The p value for the global test of difference among racial groups.
QOL = quality of life; RSDI = Rhinosinusitis Disability Index; CSS = Chronic Sinusitis Survey.
DISCUSSION
This study used several independent data sources to explore CRS in the context of race and ethnicity. The NHIS, NAMCS, and NHAMCS suggest that CRS is a significant health condition for all major race/ethnic groups in the United States and accounts for a substantial portion of physician visits regardless of race or ethnic background. Not surprisingly, these data also suggested that differences in insurance status, specialist visits, and treatment exist across race/ethnic groups with CRS. Specific data regarding race/ethnicity in patients undergoing ESS were sparse, with most studies failing to provide adequate breakdowns along race/ethnicity subgroups. In-depth analysis of a single, large cohort did show baseline differences across race/ethnic groups with regard to socioeconomic factors and QOL. Importantly, QOL did appear to improve significantly in all groups regardless of racial or ethnic background.
Health differences across groups defined by race and ethnicity could be explained by true biological differences or simply by confounding from other socioeconomic variables. Given the rarity of true biological differences defined by race/ethnicity, many researchers prefer to avoid discussion of this patient characteristic altogether. Adjustment for socioeconomic factors such as insurance status, income, and education will often account for a sizable portion of health differences by race.5 However, there remain reasons to study the impact of race and ethnicity on medical conditions. In the clinical research setting, adjustment for a limited set of socioeconomic factors rarely accounts fully for the impact of race or ethnicity. Oftentimes, as in this study, some difference by race/ethnicity will persist, most likely representing some degree of residual confounding.
Disregarding information on race/ethnicity can also obscure inequalities with health care access and/or service use. A major question that remains is whether minority groups with CRS receive appropriate levels of medical and surgical care. The national studies reviewed here are not designed to fully answer this question, especially with regard to surgery, but do suggest that differences may exist. Additionally, results of the literature review from this study highlight the fact that very little published information exists regarding ESS outcomes in minority groups. This may simply represent authors choosing to not include information regarding race/ethnicity, or it might indicate underrepresentation of minorities in surgical cohorts. When reviewing data from our cohort, minority groups accounted for only 18%, when compared with the national average of 35%. African Americans and Hispanics were especially underrepresented. Although some of this disparity might represent geographic distribution of minority groups with regard to study sites, it is equally if not more plausible that differences in income, insurance status, or referral pattern are causal. Further research is needed to quantify rates of ESS in patients with CRS and better qualify possible barriers to health care.
In the cohort analysis, Hispanic patients were found to report worse baseline scores on the RSDI instrument after controlling for socioeconomic factors. The difference in RSDI far exceeded statistical and clinical significance but was not mirrored on the CSS instrument, CT, or endoscopy. One possibility is that Hispanic patients present for surgery when symptoms reach a more severe threshold. Another explanation is that their disease is of equal severity, but Hispanic patients express QOL impacts more forcefully, possibly reflecting differences in language or culture. Although highly significant, this finding could also represent a false positive or be specific to our population. Further research in this group is needed to explore QOL impacts of CRS.
There are several important limitations that may affect study conclusions. The NHIS reported prevalence of physician-diagnosed “sinusitis” over the preceding year. This estimate was assumed to represent CRS, but in some instances patients may have been diagnosed with acute sinusitis. Additionally, estimates regarding specialist visits and surgery may not represent care for sinusitis specifically and thus should be considered hypothesis generating as opposed to firm estimates. It should also be kept in mind that the present study used national survey data from 2006 (NAMCS/NHAMCS) and 2009 (NHIS). Although this represents the latest data made publicly available, recent trends over the last several years would not be identified. The NAMCS/NHAMCS sampling scheme uses patient-weighted estimates from participating centers/physicians and thus may not fully capture the true national prevalence of ambulatory patients with CRS. The incorporated literature review was limited to surgical cohort studies because of the paucity of QOL outcomes research involving continued medical therapy for CRS. Potential misclassification bias of multiracial patients may also exist within the surgical cohort analysis, because patients with CRS were prompted to select a single race or ethnic group.
CONCLUSION
National survey data suggest that CRS is a significant health condition for all major race/ethnic groups in the United States, accounting for a sizable portion of office, ED, and OD visits. Differences were seen in insurance status, work absenteeism, and resource use across all race/ethnic groups with CRS. Despite its prevalence, few published studies include information regarding minority patients with CRS. When considering ESS specifically, most large studies do not provide details of race/ethnicity. Analysis of available cohort data did show underrepresentation of minority patients in surgical outcomes studies. Given the demographic shift underway in the United States, specific attention should be given to understanding CRS within the context of racial and ethnic minority populations.
Footnotes
Funded by a grant from the National Institute on Deafness and Other Communication Disorders, one of the National Institutes of Health (DC005805; PI: T. Smith)
TL Smith is a consultant for Intersect ENT, Inc., Palo Alto, CA, which provided no financial support for this investigation. TL Smith and JC Mace also received grant funding (DC005805) from the National Institute on Deafness and Other Communication Disorders, one of the National Institutes of Health, Bethesda, MD, for data collection associated with this investigation. The remaining author had no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Humes KR, Jones NA, Ramirez RR. Overview of race and Hispanic origin: 2010. 2010 Census Briefs. Available online at www.census.gov/prod/cen2010/briefs/c2010br-02.pdf; last accessed May 10, 2011.
- 2. Passel JS, Cohn D. US Population Projections: 2005–2050. Pew ResearchCenter February 11, 2008. Available online at www.pewsocialtrends.org/files/2010/10/85.pdf; last accessed May 10, 2011.
- 3. Williams DR. The health of US racial and ethnic populations. J Gerontol B Psychol Sci Soc 60:53–62, 2005. [DOI] [PubMed] [Google Scholar]
- 4. Kramer MR, Hogue CR. What causes racial disparities in very preterm birth? A biosocial perspective. Epidemiol Rev 31:84–98, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and heath: complexities, ongoing challenges, and research opportunities. Ann N Y Acad Sci 1186:69–101, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. US Department of Health and Human Services. Healthy People 2020: 2011. Washington, D.C.: US Department of Health and Human Services, Available online at www.healthypeople.gov/2020/default.aspx; last accessed September, 2011. [Google Scholar]
- 7. Champagne JP, Antisdel JL, Woodard TD, Koutakis SE. Epidemiologic factors affect surgical outcomes in allergic fungal sinusitis. Laryngoscope 120:2322–2324, 2010. [DOI] [PubMed] [Google Scholar]
- 8. Wise SK, Ghegan MD, Gorham E, Schlosser RJ. Socioeconomic factors in the diagnosis of allergic fungal rhinosinusitis. Otolaryngol Head Neck Surg 138:38–40, 2008. [DOI] [PubMed] [Google Scholar]
- 9. Ghegan MD, Wise SK, Gorham E, Schlosser RJ. Socioeconomic factors in allergic fungal rhinosinusitis with bone erosion. Am J Rhinol 21:560–563, 2007. [DOI] [PubMed] [Google Scholar]
- 10. Ghegan MD, Lee F, Schlosser RJ. Incidence of skull base and orbital erosion in allergic fungal rhinosinusitis (AFRS) and non-AFRS. Otolaryngol Head Neck Surg 134:592–595, 2006. [DOI] [PubMed] [Google Scholar]
- 11. Wise SK, Venkatraman G, Wise JC, DelGaudio JM. Ethnic and gender differences in bone erosion in allergic fungal sinusitis. Am J Rhinol 18:397–404, 2004. [PubMed] [Google Scholar]
- 12. Smith WM, Davidson TM, Murphy C. Regional variations in chronic rhinosinusitis, 2003–2006. Otolaryngol Head Neck Surg 141:347–352, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bhattacharyya N. Contemporary assessment of the disease burden of sinusitis. Am J Rhinol Allergy 23:392–395, 2009. [DOI] [PubMed] [Google Scholar]
- 14. Minnesota Population Center and State Health Access Data Assistance Center, Integrated Health Interview Series, Version 3.0. Minneapolis, MN: University of Minnesota, Available online at www.ihis.us/ihis/; last accessed September, 2011. [Google Scholar]
- 15. Centers for Disease Control and Prevention. National Health Interview Survey. Available online at www.cdc.gov/nhcs/nhis.htm; last accessed May 10, 2011.
- 16. Centers for Disease Control and Prevention. Ambulatory Health Care Data. Available online at www.cdc.gov/nhcs/ahcd.htm; last accessed May 10, 2011.
- 17. US National Library of Medicine. National Institutes of Health. Available online at www.ncbi.nlm.nih.gov/pubmed; last accessed April 15, 2011.
- 18. Smith TL, Litvack JR, Hwang PH, et al. Determinants of outcomes of sinus surgery: A multi-institutional prospective cohort study. Otolarygol Head Neck Surg 142:55–63, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Benninger MS, Ferguson BJ, Hadley JA, et al. Adult chronic rhinosinusitis: Definitions, diagnosis, epidemiology, and pathophysiology. Otolaryngol Head Neck Surg 129(suppl):S1–S32, 2003. [DOI] [PubMed] [Google Scholar]
- 20. Lund VJ, Mackay IS. Staging in rhinosinusitis. Rhinology 31:183–184, 1993. [PubMed] [Google Scholar]
- 21. Lund VJ, Kennedy DW. Staging for rhinosinusitis. Otolaryngol Head Neck Surg 117:S35–S40, 1997. [DOI] [PubMed] [Google Scholar]
- 22. Benninger MS, Senior BA. The development of the rhinosinusitis disability index. Arch Otolaryngol Head Neck Surg 123:1175–1179, 1997. [DOI] [PubMed] [Google Scholar]
- 23. Gliklich RE, Metson R. Techniques for outcomes research in chronic rhinosinusitis. Laryngoscope 105:387–390, 1995. [DOI] [PubMed] [Google Scholar]
- 24. Bhattacharyya N. Assessing the additional disease burden of polyps in chronic rhinosinusitis. Ann Otol Rhinol Laryngol 118:185–189, 2009. [DOI] [PubMed] [Google Scholar]
- 25. Tabaee A, Hsu AK, Shrime MG, et al. Quality of life and complications following image-guided sinus surgery. Otolarygol Head Neck Surg 135:76–80, 2006. [DOI] [PubMed] [Google Scholar]
- 26. Deal RT, Kountakis SE. Significance of nasal polyps in chronic rhinosinusitis: Symptoms and surgical outcomes. Laryngoscope 114:1932–1935, 2004. [DOI] [PubMed] [Google Scholar]
- 27. Khalid AN, Quraishi SA, Kennedy DW. Long-term quality of life measures after functional endoscopic sinus surgery. Am J Rhinol 18:131–136, 2004. [PubMed] [Google Scholar]
- 28. Jones ML, Piccirillo JF, Haiduk A, Thawley SE. Functional endoscopic sinus surgery: Do ratings of appropriateness predict patient outcomes? Am J Rhinol 12:249–255, 1998. [DOI] [PubMed] [Google Scholar]
- 29. Senior BA, Kennedy DW, Tanabodee J, Kroger H, Hassab M, Lanza D. Long-term results of functional endoscopic sinus surgery. Laryngoscope 108:151–157, 1998. [DOI] [PubMed] [Google Scholar]
- 30. Winstead W, Barnett SN. Impact of endoscopic sinus surgery on global health perception: An outcomes study. Otolaryngol Head Neck Surg 119:486–491, 1998. [DOI] [PubMed] [Google Scholar]
- 31. Chambers DW, Davis WE, Cook PR, et al. Long-term outcomes analysis of functional endoscopic sinus surgery: Correlation of symptoms with endoscopic examination findings and potential prognostic variables. Laryngoscope 107:504–510, 1997. [DOI] [PubMed] [Google Scholar]
- 32. Conte LJ, Holzberg N. Functional endoscopic sinus surgery, symptom relief: A patient perspective. Am J Rhinol 10:135–140, 1996. [Google Scholar]
- 33. Metson R, Gliklich RE. Effect of sinus surgery on quality of life. Otolaryngol Head Neck Surg 117:12–17, 1997. [DOI] [PubMed] [Google Scholar]


