Abstract
The intensive care unit at Queen Elizabeth Central Hospital (QECH) has 4 beds and offers level 2 care. A retrospective audit of all admissions to the unit during 2002 was carried out. There were a total of 339 admissions giving a bed occupancy rate of 82 %. Surgical patients made up 81 % of admissions. 45% of all admissions were ventilated. Overall mortality was 38%. Ventilated patients had a mortality of 71% compared with 10% for non-ventilated. Data are also presented for mortality within the surgical and paediatric surgical admissions.
Introduction
The Intensive Care Unit (ICU) is a specialised area where facilities for the critically ill are concentrated and where the level of care and supervision is considerably more sophisticated than in the ordinary ward. The ICU in QECH is multidisciplinary and deals with all types of critically ill patients. The level of care is level 2(+) meaning patients are admitted when they require active system support, e.g. intermittent positive pressure ventilation, have single (2) or multiple (2+) organ failure, airway problems or have conditions which require potent drug infusions. It is a 4-bed unit, comprising 0.4% of the beds in the hospital (USA 7–11%; Europe 3–4%; UK 1–2%). Basic monitoring in the form of ECG, pulse oximetry and blood pressure measurement are available. It is usually possible to ventilate patients in all 4 beds at one time. In the event of one of the ventilators breaking down, a ventilator from the theatre can be borrowed to overcome this shortage.
In general there are usually a minimum of 2 nurses and support staff available for monitoring and nursing care of patients. Anaesthetic clinical officers provide 24-hour medical cover, with anaesthetic consultant support and input from the admitting specialty department. As the QECH is a teaching hospital, student nurses, interns and rotating surgical and medical registrars welcome additional staff. Laboratory facilities are minimal with only FBC and Blood glucose levels regularly available. Serum sodium, potassium urea and creatinine measurements are available occasionally.
Methods
A retrospective audit was carried out of all patients admitted to ICU between 1 January 2002 and 31 December 2002. Data were collected by the ICU nurses and entered into an admissions book. This data was then transferred into a Microsoft Excel worksheet. The following data were collected: demographic data; length of admission; specialty; main diagnosis; secondary diagnosis; number of days (intubated); number of days ventilated; and outcome. The main outcome measure was survival to discharge to the general ward.
Because the documentation of diagnosis was not standardized, surgical patients were further classified under broad diagnostic groups to aid in the analysis of the data. These groups were: trauma surgery; abdominal surgery; thoracic surgery; head and neck surgery; endocrine surgery; burns surgery; and urological surgery. The trauma and abdominal groups were further subdivided: abdominal surgery into bowel obstruction, peritonitis, tumour, miscellaneous; and trauma surgery into head, neck, chest, abdominal, pelvis and extremities. Paediatric surgical patients were defined as patients younger than 16 years of age.
Results
Admissions
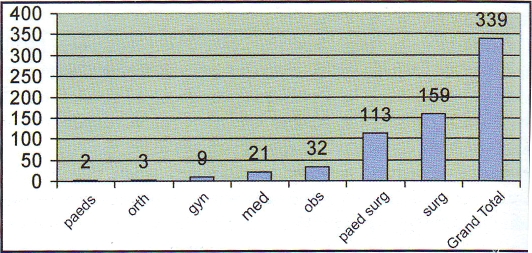
There were 339 patients admitted over 1 year with a total of 1199 days of admission and bed occupancy of 82%. Admissions by specialty are shown in figure 1. Surgical patients included orthopaedic, paediatric and adult patients bringing the total number of surgical patients up to 275 or 81% of all admissions. Of the 339 patients admitted in the ICU, 12 were intubated and not ventilated because they were patients who required airway protection but were able to breath on a T-piece. 154 patients (45%) were intubated and ventilated for a total of 542 days with an average of 3.5 days and maximum length of ventilation of 29 days. Paediatric and adult surgery differed in ventilation rate: 33% of paediatric surgical patients were ventilated compared with 53% of adult surgical patients.
Figure 1.
Number of admissions by specialty
Mortality
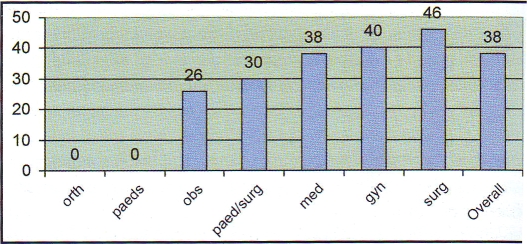
A total of 128 patients died on the ICU giving a case-fatality rate of 38%. No records could be made of those patients who died in the hospital after discharge to the ward. Mortality is given by specialty in figure 2. Ventilated patients had a higher mortality than those who did not need ventilation - figure 4. 110 (71%) of the 154 patients who were ventilated died compared to 18 (10%) deaths in 185 non-ventilated patients — RR 7.34 (95% CI: 4.7–11.5). The maximum duration of ventilation with survival to discharge was 26 days.
Figure 2.
Mortality (%) by specialty
Figure 4.
Paediatric surgical admission and mortality
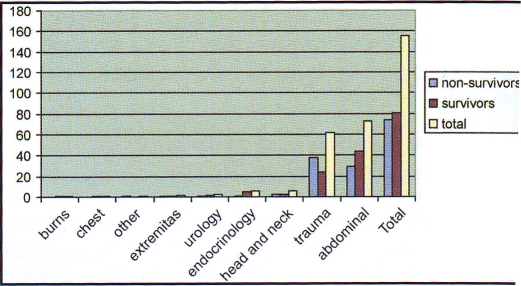
The two main diagnostic groups in adult surgery were abdominal surgery (46% of surgical admissions) and trauma surgery (39% of surgical admissions). 73 of the 159 surgical patients had abdominal pathology. This group was further subdivided. Overall mortality in the group was 40% - figure 3. However analysis of sub groups showed the highest mortality to be in the peritonitis group (51%) with a much lower mortality amongst the bowel obstruction group (29%).
Figure 3.
Mortality among surgical admissions
Trauma
Trauma accounted for 62 of the 159 surgical admissions. The overall mortality in this group was found to be 61%. However, 41 of the 62 trauma admissions had a main diagnosis of head injury. The mortality amongst the head injury group was 70%. 33 of the 41 head injuries were ventilated and mortality in this group was 81%. Only 1 of 8 non-ventilated patients died (12.5%).
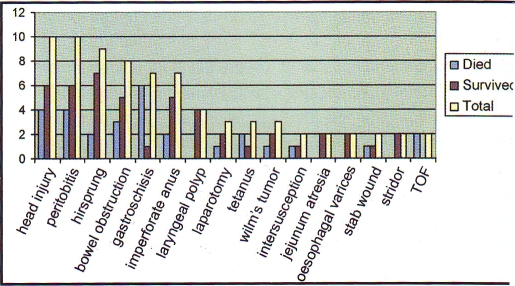
Paediatric Surgery
There were a total of 113 paediatric surgery patients. Mortality in the paediatric surgery group was 30%. 43 of the 113 were under 1 year old (38%). Mortality amongst this group was 39.5% compared with 25% in those aged one to sixteen. Figure 4 shows main diagnoses and mortality. The remaining 37 diagnostic categories had only one patient in each group.
As with the adult surgical data, head injury and abdominal pathology accounted for the largest number of paediatric admissions. Mortality amongst the head injury group was 40%, which is considerably less than the adult head injury mortality (70%). Mortality for the peritonitis was also lower in the paediatric group, 40% compared with 51%.
There was 22% mortality amongst patients admitted with Hirschsprung's disease and 28% mortality amongst those with imperforate anus. Mortality was much higher amongst patients with gastroschisis (85%) and tracheo-oesophageal fistula (100%).
Discussion
The aim of carrying out this audit was to provide a benchmark of ICU outcome with which to compare the results of future audits. It was also to identify problem areas that require further study. Overall mortality was high and this reflects not only the severity of illness of patients at presentation to the ICU but also the limits of the care which can be provided under circumstances of severe resource constraint.
However, the limitations of our data collection were clearly demonstrated and preclude in-depth analysis. In order to improve the quality of the data we need to standardise recording of diagnoses, include more detail on the types of surgical admissions (elective, emergency etc) and introduce a system to score the severity of illness in each patient.
Unfortunately, most validated ICU scoring systems, for example APACHE II (Acute physiology age and chronic health evaluation)(1), use parameters that require arterial blood gas analysis and other variables that we are unable to measure. An alternative would be to use a simplified score such as the clinical sickness score (2), which has been successfully used in the tropics.
The data show that the intensive care unit is working at near maximum capacity and dealing with a large number of critically ill patients. The majority of patients were surgical and the reasons for this are two fold. Firstly the unit is geographically situated within the operating theatre complex and this facilitates surgical input and access to the unit. Secondly, the unit only admits patients with reversible pathology and this applies to a greater proportion of surgical compared to medical patients Recent efforts by the anaesthetic consultants and secondment of medical registrars to the unit have led to the increase of the number of medical and other non-surgical admissions. Despite near maximum capacity use we hope that with improved awareness the ICU facility will increasingly be used by all specialties.
It is clear that we must strive to improve data collection; to impose the recording of diagnoses in a standardized way and to introduce a patient severity score. Until this is done we will not be able to formally audit the performance of our ICU and more importantly to compare it to other units in the region with similar resource problems.
One way in which we may be able to improve the outcome of our patients may be by the implementation of standard treatment protocols. This has now been done in patients with head injuries and since this audit was carried out in 2002 we have implemented a protocol for head injury management, carried out extensive training amongst the ICU staff and encouraged prompt referral to the unit from the surgical teams. As a result our mortality from severe head injury has decreased from 70% to 30% (3). It is our hope that extending this model to other well-defined clinical problems will lead to improved survival in other patient groups.
References
- 1.Wong DT, Knaus WA. Can J Anaesth. 1991;38:374–383. doi: 10.1007/BF03007629. [DOI] [PubMed] [Google Scholar]
- 2.Watters D, Wilson I, Leaver R, Bagshawe A. Care of the Critically ill Patient in the Tropics and Sub-Tropics. Macmillan Education. 1991 [Google Scholar]
- 3.Haisma HJ. An audit into severe head injury mortality on the Intensive care unit Queen Elizabeth Central Hospital 2002–2003. Unpublished audit data. [Google Scholar]