Video abstract
Video
Keywords: chronic heart failure, optic disk, glaucoma, intraocular pressure
Abstract
Purpose
To evaluate the association between chronic heart failure (CHF) and optic nerve head alterations.
Methods
A cross-sectional study was performed. Heart failure patients with recent echocardiograms were subjected to ophthalmologic examinations, including intraocular pressure measurement, optic nerve head, and retinal nerve fiber layer evaluation using stereophotography, Heidelberg retinal tomography, and standard automated perimetry. The ocular findings were correlated with the cardiological evaluation, and compared with a control group without cardiopathy.
Results
A total of 30 patients with CHF and 30 individuals without cardiopathy were enrolled in this study. The mean (standard deviation [SD]) intraocular pressure was 12.3 (2.5) mmHg in the CHF group, and 14.7 (2.9) mmHg in the control group (P < 0.001). The mean (SD) arterial blood pressure was 86.9 (17.1) mmHg in the CHF group, and 103.6 (15.2) mmHg in the control group (P < 0.001). The mean (SD) ocular perfusion pressure was 45.6 (11.1) mmHg in the CHF group, and 54.4 (10.4) mmHg in the control group (P = 0.001). The mean (SD) rim area was 1.41 (0.3) mm2 in the CHF group, and 1.60 (0.26) mm2 in the control group (P = 0.003). The mean (SD) vertical cup/disc ratio was 0.51 (0.17) in the CHF group, and 0.41 (0.18) in the control group (P = 0.02). The Moorfields regression analysis was outside the normal limits in 16 out of 58 (27.6%) eyes of the CHF subjects, and in 4 out of 60 (6.7%) eyes of the control subjects (P = 0.01). The frequency of glaucoma was 10% in the CHF group, whereas none of the control subjects met the criteria for the diagnosis of glaucoma (P = 0.24).
Conclusion
CHF is associated with lower ocular perfusion pressure, and glaucomatous optic nerve head changes.
Introduction
Glaucoma is a progressive optic neuropathy presenting with a distinct appearance of the optic nerve head (ONH) and visual field loss, and is the leading cause of irreversible blindness worldwide.1 The pathophysiological basis of primary open-angle glaucoma (POAG) and the factors contributing to its progression are not fully understood. The elevation of intraocular pressure (IOP) is the most important risk factor, and IOP reduction is currently the only evidence-based treatment. However, some patients develop glaucomatous neuropathy without ocular hypertension.2 Thus, other factors may be involved in the development and progression of glaucoma. The vascular theory describing the mechanism of glaucoma considers optic neuropathy as secondary to insufficient blood perfusion, due to either increased IOP or other risk factors leading to a reduction in the ocular blood flow.3 Several studies have demonstrated that the reduction of ONH perfusion is associated with glaucoma.3
A history of heart disease is already considered to be a risk factor for the development of glaucoma.4 However, the role of heart failure in the reduction of ocular blood flow, and its possible role in the development of glaucoma in these patients has not yet been established. Chronic heart failure (CHF) is a serious and common condition in which an abnormality of cardiac function is responsible for the heart’s failure to pump blood at a rate corresponding to the requirements of the metabolizing tissues.5 A complex neurohormonal system attempts to compensate for heart failure to ensure suitable perfusion of the tissues.6 However, studies indicate that cerebral blood flow may be reduced in these patients.7,8 A recent study with color Doppler imaging reported reduced blood flow velocities and an increased resistance index in the ophthalmic artery of CHF patients.9 The purpose of this study was to evaluate the association between CHF and ONH alterations.
Methods
A cross-sectional study was performed. Patients with CHF symptoms and left ventricle ejection fractions below 55% documented by echocardiography were recruited from the outpatient cardiomyopathy and heart failure clinic of the Federal University of São Paulo, Brazil. Noncardiopathic volunteers were included as a control group. The study was approved by the Institutional Ethics Committee and followed the tenets of the Declaration of Helsinki. Informed consent was obtained from all subjects prior to the study, after full disclosure of the nature and possible consequences of the study.
CHF cases and control subjects under 18 years of age, patients with a prior history of significant ocular disease, ocular trauma or ocular surgery, spherical equivalent greater than ±4.0 D, chronic corticosteroid usage (topical or systemic), angle closure suspect, secondary glaucoma, dense media opacities, retinal disease, heart transplantation, stroke or any other neurological diseases were not included in the study.
Systolic and diastolic blood pressure readings were obtained and used to calculate the mean arterial blood pressure (MAP) according to the following formula: MAP = 2/3 * diastolic blood pressure + 1/3 * systolic blood pressure. The mean ocular perfusion pressure (OPP) was calculated using the following formula: OPP = 2/3 * MAP – IOP.10
The diagnoses of POAG were based on the following criteria:11 (a) a vertical cup/disc ratio (VCDR) of ≥0.7, asymmetry between the right and left VCDRs of ≥0.15 or a remaining neural rim ≤10% of the diameter of the ONH (in upper or lower quadrants), and a visual field defect consistent with glaucoma; (b) VCDR of ≥0.85 in either eye or asymmetry between the right and left VCDRs of ≥0.3 if a reliable field test result could not be obtained. The visual field defect was defined as being consistent with glaucoma if either of the following criteria were present: a cluster of three or more points with a P < 5%, with at least one with a P < 1% in pattern standard deviation, or a glaucoma hemifield test (GHT) outside of normal limits.
Ophthalmologic evaluation
All participants underwent a standardized examination that included best-corrected visual acuity, slit-lamp biomicroscopy, gonioscopy, Goldmann applanation tonometry, fundus biomicroscopy with a 78D lens, standard automated perimetry (SITA 24-2, Humphrey Visual Field Analyzer II; Carl Zeiss Meditec, Dublin, CA), color stereoscopic ONH photography, and confocal scanning laser ophthalmoscopy (Heidelberg retinal tomography, version 3.0; Heidelberg Engineering, Dosenheim, Germany). IOP measurement was performed three times in each eye, and the mean value was considered for the analysis. Visual field reliability criteria included less than 33% fixation losses, false-positive results, and false-negative results. The IOP was measured before pupil dilation, and within 30 minutes of the arterial blood pressure measurement. All of the IOP measurements were performed between 8:00 am and 11:00 am. After pupil dilation, the ONHs were imaged using HRT, a confocal scanning laser ophthalmoscope, which generates a mean topographic image and a stereometric analysis after three consecutive ONH scans. In this study, all of the images must have demonstrated a pixel standard deviation (SD) of <50 μm. In the case of poor centration (more than a quarter of the ONH outside the target circle), empty series, blink or loss of fixation, or insufficient imaging clarity and exposure, the scan was not saved on the hard disk. The assessment of the ONH findings according to the color and thinning of the neural rim and the presence of a hemorrhage and retinal nerve fiber layer (RNFL) defects were based on the evaluation of stereophotographs by an experienced examiner (LASM) blinded to the patients’ clinical data.
Statistical analysis
The correlations between the ONH morphologic parameters, left ventricle ejection fraction and the blood pressure measurements were calculated using the Pearson’s correlation test. The generalized estimating equation with robust standard error was used to take into account the correlation between both eyes of the same individual in the comparisons of the mean values between the groups. It was calculated that 57 eyes in each group were needed, in order to have 80% power to detect a 0.1 difference in the VCDR between the groups, considering an SD of 0.14, an intracluster correlation between both eyes of the same individual of 0.85, a design effect of 1.85, and a significance level of 0.05.
Results
The study population comprised 30 patients with different stages of CHF, and 30 controls (noncardiopathic individuals). The left eye was excluded for one patient in the CHF group due to corneal opacity. Table 1 summarizes the patients’ main characteristics. Age, sex, spherical correction, and ONH size were not significantly different between the two groups.
Table 1.
Demographic and systemic data of the chronic heart failure and control groups
| Variable | CHF group | Control group |
|---|---|---|
| N | 30 | 30 |
| Age, mean (SD), years | 54.8 (12.2) | 54.9 (12) |
| Sex | ||
| Male, N (%) | 19 (63.3) | 15 (50) |
| Female, N (%) | 11 (36.7) | 15 (50) |
| Race | ||
| White, N (%) | 14 (46.7) | 17 (56.7) |
| Black, N (%) | 15 (50) | 13 (43.3) |
| Asian, N (%) | 1 (3.3) | 0.00 |
| Laterality | ||
| Right eye, N (%) | 30 (50.8) | 30 (50) |
| Left eye, N (%) | 29 (49.2) | 30 (50) |
| Visual acuity, median (Q1 to Q3) | 20/20 (20/25 to 20/20) | 20/20 (20/25 to 20/20) |
| Spheric equivalent, mean (SD), D | 0.54 (1.45) | 0.19 (1.47) |
| Cardiopathy etiology | ||
| Chagas, N (%) | 10 (33.3) | NA |
| Ischemic, N (%) | 10 (33.3) | |
| Idiopathic, N (%) | 5 (16.7) | |
| Others, N (%) | 5 (16.7) | |
| Left ventricle ejection fraction, median (Q1 to Q3) | 0.35 (0.30 to 0.42) | NA |
| NYHA functional class of heart failure | ||
| I, N (%) | 16 (53.3) | NA |
| II, N (%) | 10 (33.3) | |
| III, N (%) | 4 (13.3) | |
| Medications | ||
| Diuretics, N (%) | 29 (96.7) | 4 (12.5) |
| β-blockers, N (%) | 28 (93.3) | 1 (3.3) |
| ACE inhibitors, N (%) | 29 (96.7) | 5 (16.7) |
| Digoxin, N (%) | 4 (13.3) | NA |
Abbreviations: ACE, angiotensin-converting enzyme; CHF, chronic heart failure; NYHA, New York Heart Association; SD, standard deviation; NA, not applicable.
The comparative analyses of IOP, OPP, and blood pressure between the groups are described in Table 2. The IOP ranged from 7 mmHg to 18 mmHg in the CHF group, and from 10 mmHg to 20 mmHg in the control group. The frequency of eyes with a mean OPP of <42 mmHg was 28 out of 59 (47.5%) in the CHF group, and 4 out of 60 (6.7%) in the control group (P = 0.002).
Table 2.
Intraocular pressure, blood pressure, and ocular perfusion pressure measurements
| Variable | CHF group Mean (SD) | Control group Mean (SD) | P* |
|---|---|---|---|
| Intraocular pressure (mmHg) | 12.3 (2.5) | 14.7 (2.9) | <0.001 |
| Systolic blood pressure (mmHg) | 110.4 (24.1) | 130.2 (18) | <0.001 |
| Diastolic blood pressure (mmHg) | 75.2 (14.5) | 90.3 (14.4) | <0.001 |
| Mean blood pressure (mmHg) | 86.9 (17.1) | 103.6 (15.2) | <0.001 |
| Mean ocular perfusion pressure (mmHg) | 45.6 (11.1) | 54.4 (10.4) | 0.001 |
Note:
P values calculated with generalized estimating equations.
Abbreviation: CHF, chronic heart failure.
Of the 59 eyes included in the CHF group, one eye was excluded from the analysis of the HRT structural evaluation due to a topographic SD > 50 μm, and three other eyes were excluded from the stereophotography ONH evaluation due to poor image quality. The ONH evaluation through stereophotography is shown in Table 3. There was no significant difference between the two groups regarding the presence of rim thinning, parapapillary atrophy and RNFL defect. No subject presented with a hemorrhage of the ONH or disc pit.
Table 3.
Optic nerve head evaluation through stereophotography
| Variable | CHF group | Control group | P |
|---|---|---|---|
| N | 28 | 30 | – |
| Vertical cup/disc ratio, Mean (SD) | 0.49 (0.19) | 0.42 (0.15) | 0.06* |
| Horizontal cup/disc ratio, Mean (SD) | 0.47 (0.17) | 0.42 (0.15) | 0.19* |
| Rim pale (focal or difuse) (%) | 7.2 | 3.4 | 0.61† |
| Notch of the neural rim (%) | 10.7 | 0.00 | 0.11† |
| Disc pit (%) | 0.00 | 0.00 | – |
| Disc hemorrhage (%) | 0.00 | 0.00 | – |
| RNFL defect (%) | 7.2 | 0.00 | 0.24† |
Note:
P values calculated with generalized estimating equations;
P values calculated with Fisher’s exact test.
Abbreviations: CHF, chronic heart failure; SD, standard deviation; RNFL, retinal layer fiber layer.
The mean values for the stereometric measures of the ONH measured by HRT are shown in Table 4. The frequency of eyes with a VCDR > 0.7 was 8 out of 59 (13.6%) in the CHF group, and 1 out of 60 (1.7%) in the control group (P = 0.04).
Table 4.
Stereometric measurements of the optic nerve head evaluated by the HRT
| Stereometric measure | CHF group Mean (SD) | Control group Mean (SD) | P* |
|---|---|---|---|
| N (eyes) | 57 | 60 | |
| Disc area, mm2 | 2.04 (0.46) | 2.04 (0.45) | 0.90 |
| Cup area, mm2 | 0.67 (0.50) | 0.45 (0.38) | 0.04 |
| Rim area, mm2 | 1.41 (0.30) | 1.60 (0.26) | 0.003 |
| Rim steepness | −0.24 (0.62) | −0.22 (0.53) | 0.81 |
| Cup/disc area ratio | 0.30 (0.17) | 0.20 (0.14) | 0.004 |
| Cup volume, mm2 | 0.18 (0.21) | 0.09 (0.10) | 0.01 |
| Rim volume, mm2 | 0.36 (0.13) | 0.46 (0.14) | <0.001 |
| Mean cup depth, mm | 0.25 (0.11) | 0.19 (0.09) | 0.02 |
| Maximum cup depth, mm | 0.65 (0.23) | 0.53 (0.25) | 0.04 |
| Height variation contour | 0.39 (0.08) | 0.42 (0.11) | 0.07 |
| Cup shape measure | −0.17 (0.08) | −0.18 (0.08) | 0.75 |
| Mean RNFL thickness, μm | 0.23 (0.08) | 0.26 (0.07) | 0.06 |
| RNFL cross sectional area, mm2 | 1.18 (0.41) | 1.32 (0.39) | 0.08 |
| Horizontal RNFL curvature | −0.004 (0.06) | 0.02 (0.05) | 0.09 |
| Vertical RNFL curvature | −0.10 (0.07) | −0.12 (0.06) | 0.37 |
| Linear cup/disc ratio | 0.51 (0.17) | 0.41 (0.18) | 0.02 |
| Topographic SD | 19.40 (8.74) | 21.20 (7.20) | 0.29 |
Note:
P values calculated with generalized estimating equations.
Abbreviations: RNFL, retinal layer fiber layer; CHF, chronic heart failure.
The frequency of eyes that demonstrated Moorfields regression analyses outside normal limits was 16 out of 58 (27.6%) in the CHF group, and 4 out of 60 (6.7%) in the control group (P = 0.018).
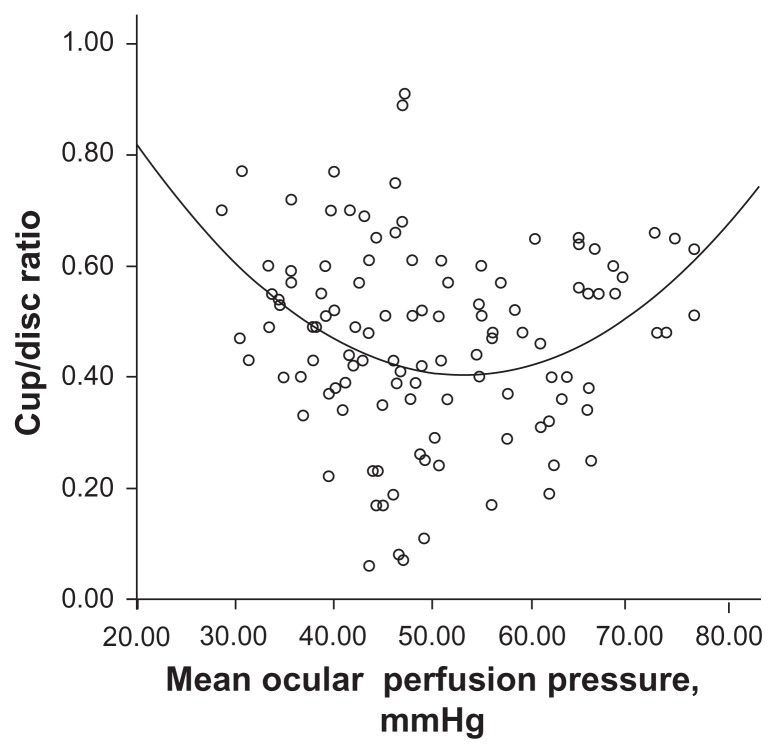
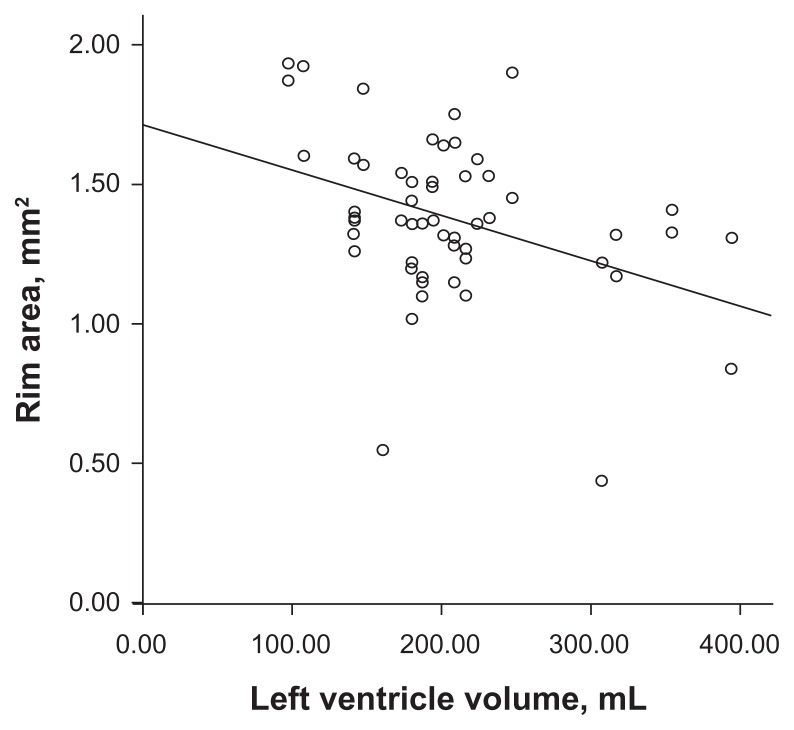
The VCDR exhibited a nonlinear correlation with the mean OPP (R2 = 0.091; P = 0.005) (Figure 1). The rim area showed a negative linear correlation with the volume of the left ventricle among patients with CHF (r = −0.382; P = 0.004) (Figure 2). The tests for a correlation between ONH stereometric measurements and cardiologic parameters of patients with CHF are described in Table 5.
Figure 1.
Scatterplot demonstrating the association between the mean ocular perfusion pressure and the cup:disc ratio. The solid line corresponds to the representation of the quadratic function.
Notes: R2 = 0.091, P = 0.005.
Figure 2.
Scatterplot demonstrating the association between the left ventricle volume and the neural rim area in patients with chronic heart failure.
Notes: r = −0.382; P = 0.01.
Table 5.
Correlation between the cardiovascular parameters and stereometric measurements of the optic nerve head in patients with chronic heart failure
| Cadiovascular variable | Rim area | Cup area | Cup/disc area ratio | RNFL thickness | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| r | P* | r | P* | r | P* | r | P* | |
| NYHA functional class of heart failure | 0.03 | 0.52 | −0.08 | 0.66 | −0.71 | 0.67 | 0.12 | 0.14 |
| Left ventricle ejection fraction | 0.18 | 0.29 | −0.25 | 0.06 | −0.26 | 0.15 | 0.25 | 0.01 |
| Left ventricle shortening fraction | 0.36 | 0.01 | −0.36 | 0.01 | −0.37 | 0.04 | 0.26 | 0.05 |
| Left ventricle diastolic volume | −0.38 | 0.01 | 0.08 | 0.77 | 0.20 | 0.34 | −0.10 | 0.39 |
| Left ventricle systolic diameter | −0.47 | 0.005 | 0.20 | 0.34 | 0.32 | 0.13 | −0.13 | 0.34 |
| Left ventricle diastolic diameter | −0.36 | 0.03 | 0.11 | 0.71 | 0.22 | 0.30 | −0.02 | 0.84 |
| Left ventricle mass index | −0.34 | 0.08 | 0.25 | 0.07 | 0.34 | 0.02 | 0.05 | 0.71 |
| Systolic blood pressure | −0.16 | 0.23 | −0.06 | 0.67 | −0.04 | 0.80 | 0.05 | 0.60 |
| Diastolic blood pressure | −0.19 | 0.62 | −0.13 | 0.30 | −0.10 | 0.47 | 0.03 | 0.73 |
Notes: r = Pearson’s correlation coefficient.
P values calculated with generalized estimating equations.
Abbreviations: NYHA, New York Heart Association; RNFL, retinal nerve fiber layer.
Three eyes from the CHF group and two eyes of the control group were excluded from the analysis of visual field testing due to the low reliability of the tests. Regarding the frequency of perimetric alterations, 14 out of 56 (25%) eyes in the CHF group and 3 out of 58 (5.2%) eyes in the control group demonstrated a GHT outside normal limits (P = 0.037). The mean deviation was −2.78 (2.89) dB in the CHF group, and −1.52 (1.08) dB in the control group (P = 0.008). The mean PSD was 2.35 (1.66) dB in the CHF group, and 1.91 (0.61) dB in the control group (P = 0.128).
The frequency of glaucoma was 10% (three patients, four eyes) in the CHF group, whereas none of the control subjects met the criteria for the diagnosis of POAG (P = 0.24). None of the individuals who met the diagnostic criteria for glaucoma had a previous diagnosis of glaucoma, or were using ocular hypotensive eye drops. The mean IOP of the subgroup of patients with glaucoma was 12.6 (3.65) mmHg, while the mean of the rest of the CHF group was 12.4 (2.34) mmHg (P = 0.88). The mean OPP was 40.9 (4.09) mmHg in the subgroup with glaucoma, and was 46.3 (11.65) mmHg for the rest of the CHF group (P = 0.17). The mean left ventricle ejection fraction was 0.35 (0.05) in patients with glaucoma, and 0.34 (0.1) for the rest of the CHF group (P = 0.76).
Discussion
The results of this study indicated an association between CHF and glaucomatous ONH alterations. Patients with CHF demonstrated a higher cup/disc ratio and a smaller rim area, compared with those control subjects without heart disease. This type of alteration of the ONH corresponds to the signs classically observed in glaucomatous damage.12 The CHF group also had a higher frequency of results outside of normal limits in the Moorfields regression analysis. This test provides good sensitivity and specificity for the diagnosis of glaucoma.13 Patients with CHF also had a higher frequency of visual field alterations as GHT outside normal limits and a lower mean deviation.
A previous epidemiology study observed a 2.4% prevalence of POAG in the southern region of Brazil among subjects aged over 40 years.14 The results of the present study indicated a 10% frequency of POAG in patients with CHF, which is significantly greater than that described for the Brazilian population. Because patients with glaucoma and heart failure did not display ocular hypertension, vascular causes such as systemic hypotension and low ocular perfusion pressure might be involved in the pathogenesis of glaucoma in these patients.
In this study, several parameters of cardiac injury severity correlated with the ONH stereometric measures, ie, more advanced heart disease was associated with greater damage to the optic nerve. The reduction in cardiac output is associated with compensatory mechanisms that include peripheral vasoconstriction in an attempt to maintain satisfactory blood pressure and perfusion to the essential tissues such as the heart and brain.7 In patients with heart failure, the sympathetic and renin–angiotensin systems are activated as a neurohormonal response to maintain cardiac output and hemodynamic balance. 8 However, excessive neurohormonal activity during CHF causes a reduction in quality of life, increased mortality,15 and increased cerebral vascular resistance, which is often accompanied by symptoms,8 such as cognitive dysfunction, that are present in 35% to 50% of patients with CHF.7,15 Cerebral hypoperfusion is considered to be the main cause of cognitive impairment in patients with heart failure.16 In the retrobulbar circulation, vasoconstriction may cause instability of blood flow in the ONH. Ischemia followed by reperfusion is a known cause of oxidative stress and cell death by apoptosis. According to this pathophysiology, patients with CHF could theoretically be exposed to hemodynamic changes in ocular microcirculation and have an increased risk for developing glaucoma.
Several studies have demonstrated an association between glaucoma and cardiovascular disease. Some studies suggest that ischemic heart disease is more prevalent among patients with POAG, particularly in normal tension glaucoma.17,18 An echocardiographic study observed a trend toward a higher prevalence of myocardial relaxation dysfunction in patients with glaucoma.19 In a series of 10 cases of normal tension glaucoma, it was reported that there was a well-defined history of clinical shock secondary to various causes, including intestinal bleeding, cardiac arrest, and acute myocardial infarction.20 Some studies in glaucoma patients observed an increased prevalence of vascular diseases such as ischemic heart disease, migraines, and peripheral vascular disease21 and an increased cardiovascular risk.22 No studies were found in the literature concerning the investigation of glaucomatous ONH alterations in patients with heart failure.
The pathogenesis of ONH alteration in these patients was probably related to a reduction in ocular perfusion secondary to heart failure. However, we cannot rule out a possible thromboembolic etiology for the changes of the optic nerve found in patients with CHF because cardiovascular disease is an important risk factor for thrombotic events. However, this etiology is improbable because the patients did not report any history of sudden decreased vision. Moreover, fundoscopic signs of anterior ischemic optic neuropathy such as neural rim pallor were uncommon (two patients), and did not correlate with the glaucoma diagnosis.
The CHF group demonstrated a lower mean IOP than the control group, and no patients with heart failure had an IOP ≥ 21 mmHg. This may be because patients with CHF had significantly lower blood pressure. A positive correlation between blood pressure and IOP has been well documented.23 For each 10 mmHg rise in systolic and diastolic blood pressure, there is an increase in IOP ranging from 0.20 mmHg to 0.44 mmHg and 0.40 mmHg to 0.85 mmHg, respectively.23 It has been speculated that blood pressure plays a role in maintaining the hydrostatic pressure necessary for the production of aqueous humor by the ciliary body.24 Blood pressure may also influence the episcleral pressure, and thus modify the aqueous humor drainage.25 Some of the medications used to treat heart failure, such as angiotensin-converting enzyme inhibitors,26 angiotensin receptor antagonists,27 beta-blockers, 28 and digoxin,29 may also directly influence IOP by inhibiting aqueous humor production.
The mean OPP was approximately 15% lower in CHF patients compared with that of control patients. This difference was due to the lower blood pressure found in patients with CHF. Hypotension in these patients may be caused by heart failure, or by the excessive vasodilatory effect of medications used to treat the disease. There was a nonlinear correlation between the OPP and the VCDR. The patients with a lower ocular perfusion pressure had higher VCDRs. This finding is consistent with previous studies that indicate low OPP is a risk factor for glaucomatous optic neuropathy.30 However, according to the correlation described in this study, patients with high values for the OPP also showed high VCDRs. A curve representing the relationship between OPP and the VCDR (Figure 1) is similar to that described for the relationship between OPP and the prevalence of glaucoma in Latinos.31 This increased prevalence of excavation and glaucoma associated with higher levels of ocular perfusion pressure is probably related to the systemic arterial hypertension in this population group.
This study, however, does present a few limitations, such as the cross-sectional design, which impairs the ability to determine with certainty whether the heart failure preceded the changes of the ONH, and whether the low OPP in patients with CHF would be a natural consequence of the pathogenesis of cardiovascular disease, or due to the use of medications. Regarding the sample, the evaluated patients with CHF may not be representative of all cases of this disease, especially because they were outpatients. The presence of heart disease of different etiologies, different stages, and different risks for ocular microvasculature alterations may have attenuated the differences between the cases and controls. Our sample consisted of outpatients (mainly functional classes I and II). However, the occurrence of glaucomatous changes in patients with mild-to-moderate CHF, and thus a longer life expectancy suggests that these patients might suffer some impact on their quality of life. Despite the similarity between the cases and controls regarding age and sex, other potential confounders were not controlled, such as carotid atherosclerosis and the use of medications. As to the diagnostic ability of the Moorfields regression analysis, one major drawback is the great structural variability of the ONH in the normal population. Race is an important factor associated with this variability.32 Although the latest version of HRT contains data from normal individuals of white and black races,33 no data from Latinos were included in this version.
The presence of glaucoma in patients with heart failure may be related to low cerebral blood flow and may be a poor prognostic factor for heart disease. The prevalence of heart failure is increasing in western countries, and the evolution of treatment and increased survival in turn increases the likelihood that more patients with heart failure may suffer the impact of glaucoma on their quality of life.
The treatment of normal tension glaucoma is a major challenge for specialists, because the disease continues to progress in many patients despite a reduction in IOP.2 POAG management in patients with heart failure is complicated by contraindication to the use of beta blockers and potential intolerance to alpha2-agonists. Further studies are needed to identify which glaucoma medications demonstrate real efficacy and tolerability at this end of the disease spectrum, in which the change to ocular blood flow seems to be involved in the pathogenesis of glaucoma to a greater extent than the IOP. Because glaucoma is a slowly progressive disease and low perfusion pressure is not commonly observed in the general population, advanced heart failure may serve as an excellent clinical model to test the relationship between a low level of blood perfusion to the ocular tissues and the incidence of glaucomatous damage.
Conclusion
CHF is associated with glaucomatous alterations of the ONH. The low cardiac output, the decreased systemic blood pressure, and the low OPP might be related to the vascular pathogenesis of the ONH alterations.
Acknowledgments
The project number and institution responsible for the approval of the Research Ethics Committee is 0812/07 – UNIFESP. The authors are grateful for the financial support provided by CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior) for PhD student scholarship.
Footnotes
Disclosure
The authors have no conflicts of interest in this work.
References
- 1.Weinreb RN, Khaw PT. Primary open-angle glaucoma. Lancet. 2004;363(9422):1711–1720. doi: 10.1016/S0140-6736(04)16257-0. [DOI] [PubMed] [Google Scholar]
- 2.Collaborative Normal-Tension Glaucoma Study Group. The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. Am J Ophthalmol. 1998;126(4):498–505. doi: 10.1016/s0002-9394(98)00272-4. [DOI] [PubMed] [Google Scholar]
- 3.Flammer J, Orgul S, Costa VP, et al. The impact of ocular blood flow in glaucoma. Prog Retin Eye Res. 2002;21(4):359–393. doi: 10.1016/s1350-9462(02)00008-3. [DOI] [PubMed] [Google Scholar]
- 4.Gordon MO, Beiser JA, Brandt JD, et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):714–720. doi: 10.1001/archopht.120.6.714. discussion 829–830. [DOI] [PubMed] [Google Scholar]
- 5.Remme WJ, Swedberg K Task Force for the Diagnosis and Treatment of chronic Heart Failure, European Society of Cardiology. Guidelines for the diagnosis and treatment of chronic heart failure. Eur Heart J. 2001;22(17):1527–1560. doi: 10.1053/euhj.2001.2783. [DOI] [PubMed] [Google Scholar]
- 6.Saxena PR, Schoemaker RG. Organ blood flow protection in hypertension and congestive heart failure. Am J Med. 1993;94(4A):4S–12S. [PubMed] [Google Scholar]
- 7.Almeida OP, Flicker L. The mind of a failing heart: a systematic review of the association between congestive heart failure and cognitive functioning. Intern Med J. 2001;31(5):290–295. doi: 10.1046/j.1445-5994.2001.00067.x. [DOI] [PubMed] [Google Scholar]
- 8.Choi BR, Kim JS, Yang YJ, et al. Factors associated with decreased cerebral blood flow in congestive heart failure secondary to idiopathic dilated cardiomyopathy. Am J Cardiol. 2006;97(9):1365–1369. doi: 10.1016/j.amjcard.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 9.Almeida-Freitas DB, Meira-Freitas D, Melo LA, Jr, Paranhos A, Jr, Iared W, Ajzen S. Color Doppler imaging of the ophthalmic artery in patients with chronic heart failure. Arq Bras Oftalmol. 2011;74(5):326–329. doi: 10.1590/s0004-27492011000500003. [DOI] [PubMed] [Google Scholar]
- 10.Gherghel D, Orgul S, Gugleta K, Gekkieva M, Flammer J. Relationship between ocular perfusion pressure and retrobulbar blood flow in patients with glaucoma with progressive damage. Am J Ophthalmol. 2000;130(5):597–605. doi: 10.1016/s0002-9394(00)00766-2. [DOI] [PubMed] [Google Scholar]
- 11.Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002;86(2):238–242. doi: 10.1136/bjo.86.2.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uchida H, Brigatti L, Caprioli J. Detection of structural damage from glaucoma with confocal laser image analysis. Invest Ophthalmol Vis Sci. 1996;37(12):2393–2401. [PubMed] [Google Scholar]
- 13.Miglior S, Guareschi M, Albe E, Gomarasca S, Vavassori M, Orzalesi N. Detection of glaucomatous visual field changes using the Moorfields regression analysis of the Heidelberg retina tomograph. Am J Ophthalmol. 2003;136(1):26–33. doi: 10.1016/s0002-9394(03)00084-9. [DOI] [PubMed] [Google Scholar]
- 14.Sakata K, Sakata LM, Sakata VM, et al. Prevalence of glaucoma in a South Brazilian population: Projeto Glaucoma. Invest Ophthalmol Vis Sci. 2007;48(11):4974–4979. doi: 10.1167/iovs.07-0342. [DOI] [PubMed] [Google Scholar]
- 15.Zuccala G, Pedone C, Cesari M, et al. The effects of cognitive impairment on mortality among hospitalized patients with heart failure. Am J Med. 2003;115(2):97–103. doi: 10.1016/s0002-9343(03)00264-x. [DOI] [PubMed] [Google Scholar]
- 16.Roman GC. Brain hypoperfusion: a critical factor in vascular dementia. Neurol Res. 2004;26(5):454–458. doi: 10.1179/016164104225017686. [DOI] [PubMed] [Google Scholar]
- 17.Hayreh SS. The role of age and cardiovascular disease in glaucomatous optic neuropathy. Surv Ophthalmol. 1999;43(Suppl 1):S27–S42. doi: 10.1016/s0039-6257(99)00018-1. [DOI] [PubMed] [Google Scholar]
- 18.Waldmann E, Gasser P, Dubler B, Huber C, Flammer J. Silent myocardial ischemia in glaucoma and cataract patients. Graefes Arch Clin Exp Ophthalmol. 1996;234(10):595–598. doi: 10.1007/BF00185290. [DOI] [PubMed] [Google Scholar]
- 19.Bojic L, Ermacora R, Karelovic D, Hozo I. Should we screen for asymptomatic left ventricular dysfunction in glaucoma patients? Ann Saudi Med. 2001;21(1–2):35–37. doi: 10.5144/0256-4947.2001.35. [DOI] [PubMed] [Google Scholar]
- 20.Drance SM, Morgan RW, Sweeney VP. Shock-induced optic neuropathy: a cause of nonprogressive glaucoma. N Engl J Med. 1973;288(8):392–395. doi: 10.1056/NEJM197302222880804. [DOI] [PubMed] [Google Scholar]
- 21.Jeganathan VS, Wong TY, Foster PJ, et al. Peripheral artery disease and glaucoma: the Singapore Malay Eye Study. Arch Ophthalmol. 2009;127(7):888–893. doi: 10.1001/archophthalmol.2009.136. [DOI] [PubMed] [Google Scholar]
- 22.Orzalesi N, Rossetti L, Omboni S OPTIME Study Group, CONPROSO Collegio Nazionale dei Professori Ordinari di Scienze Oftalmologiche. Vascular risk factors in glaucoma: the results of a national survey. Graefes Arch Clin Exp Ophthalmol. 2007;245(6):795–802. doi: 10.1007/s00417-006-0457-5. [DOI] [PubMed] [Google Scholar]
- 23.Costa VP, Arcieri ES, Harris A. Blood pressure and glaucoma. Br J Ophthalmol. 2009;93(10):1276–1282. doi: 10.1136/bjo.2008.149047. [DOI] [PubMed] [Google Scholar]
- 24.Bill A. The role of ciliary blood flow and ultrafiltration in aqueous humor formation. Exp Eye Res. 1973;16(4):287–298. doi: 10.1016/0014-4835(73)90094-8. [DOI] [PubMed] [Google Scholar]
- 25.Xu L, Wang H, Wang Y, Jonas JB. Intraocular pressure correlated with arterial blood pressure: the Beijing Eye Study. Am J Ophthalmol. 2007;144(3):461–462. doi: 10.1016/j.ajo.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 26.Shah GB, Sharma S, Mehta AA, Goyal RK. Oculohypotensive effect of angiotensin-converting enzyme inhibitors in acute and chronic models of glaucoma. J Cardiovasc Pharmacol. 2000;36(2):169–175. doi: 10.1097/00005344-200008000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Costagliola C, Verolino M, De Rosa ML, Iaccarino G, Ciancaglini M, Mastropasqua L. Effect of oral losartan potassium administration on intraocular pressure in normotensive and glaucomatous human subjects. Exp Eye Res. 2000;71(2):167–171. doi: 10.1006/exer.2000.0866. [DOI] [PubMed] [Google Scholar]
- 28.Chauhan JK, Mishra YC, Khilnani K. A clinical study of effect of oral atenolol on normal intraocular pressure and systemic blood pressure. Indian J Ophthalmol. 1989;37(4):179–181. [PubMed] [Google Scholar]
- 29.Ferraiolo BL, Pace DG. Digoxin-induced decrease in intraocular pressure in the cat. Eur J Pharmacol. 1979;55(1):19–22. doi: 10.1016/0014-2999(79)90143-2. [DOI] [PubMed] [Google Scholar]
- 30.Leske MC, Wu SY, Hennis A, Honkanen R, Nemesure B BESs Study Group. Risk factors for incident open-angle glaucoma: the Barbados Eye Studies. Ophthalmology. 2008;115(1):85–93. doi: 10.1016/j.ophtha.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 31.Memarzadeh F, Ying-Lai M, Chung J, Azen SP, Varma R Los Angeles Latino Eye Study Group. Blood pressure, perfusion pressure, and open-angle glaucoma: the Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci. 2010;51(6):2872–2877. doi: 10.1167/iovs.08-2956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chi T, Ritch R, Stickler D, Pitman B, Tsai C, Hsieh FY. Racial differences in optic nerve head parameters. Arch Ophthalmol. 1989;107(6):836–839. doi: 10.1001/archopht.1989.01070010858029. [DOI] [PubMed] [Google Scholar]
- 33.Zelefsky JR, Harizman N, Mora R, et al. Assessment of a race-specific normative HRT-III database to differentiate glaucomatous from normal eyes. J Glaucoma. 2006;15(6):548–551. doi: 10.1097/01.ijg.0000212289.00917.a8. [DOI] [PubMed] [Google Scholar]