Abstract
We evaluated a DNA plasmid-vectored vaccine and a recombinant modified vaccinia virus Ankara vaccine (MVA-mBN32), each encoding cytotoxic and helper T-lymphocyte epitopes of human immunodeficiency virus type 1 (HIV-1) in a randomized, double-blinded, placebo-controlled trial in 36 HIV-1-uninfected adults using a heterologous prime-boost schedule. HIV-1-specific cellular immune responses, measured as interleukin-2 and/or gamma interferon production, were induced in 1 (4%) of 28 subjects after the first MVA-mBN32 immunization and in 3 (12%) of 25 subjects after the second MVA-mBN32 immunization. Among these responders, polyfunctional T-cell responses, including the production of tumor necrosis factor alpha and perforin, were detected. Vaccinia virus-specific antibodies were induced to the MVA vector in 27 (93%) of 29 and 26 (93%) of 28 subjects after the first and second immunizations with MVA-mBN32. These peptide-based vaccines were safe but were ineffective at inducing HIV-1-specific immune responses and induced much weaker responses than MVA vaccines expressing the entire open reading frames of HIV-1 proteins.
INTRODUCTION
A number of nonhuman primate and human studies have shown that DNA plasmid-vectored vaccines administered by themselves elicit broad, but fairly weak, cellular and humoral immune responses (7, 18, 40, 41, 45, 67). When used in combination with other vaccine delivery technologies, such as viral vectors in heterologous prime-boost immunization regimens, they may provide a potent priming response that is restimulated with the following boost by a recombinant viral vector (2–4, 6, 33, 40, 41, 52, 60).
Poxviruses have been extensively studied as human immunodeficiency virus type 1 (HIV-1) vaccine vectors in humans (8, 15, 24, 31). These poxviruses are capable of accommodating large amounts of foreign DNA, and some are attenuated to infect but not replicate in human cells, resulting in expression of a large amount of foreign protein. The use of a single viral vector to prime and boost immune responses to a foreign antigen may not be an efficient regimen. Immune responses to the vector induced after the primary vaccination may interfere with the infection of the virus following a second vaccination, preventing an effective boost of the immune response. Yang et al. (72) showed that DNA priming could overcome the effect of preexisting immunity to viral vectors.
Like other modified vaccinia virus Ankara (MVA) vectors, which were generated as a consequence of deletions in the MVA genome, MVA-BN (Bavarian Nordic A/S GmbH, Martinsried, Germany) exhibits a severely restricted host range and replicates very poorly in most mammalian cell types, including primary human cells and most transformed human cell lines (10, 12, 19, 61). Although MVA-BN exhibits attenuated replication in these cell types, its genes are efficiently transcribed, with the block in viral replication being at the level of virus assembly and egress (12, 61). Recombinant MVA-BN vaccines encoding inserted vaccine transgenes have important characteristics, including a high expression of vaccine antigen in MVA-infected cells (62). They induce both cytotoxic T-lymphocyte (CTL) and antibody responses in humans (35). MVA-BN vaccines at doses ranging from 1 × 106 to 5 × 108 50% tissue culture infectious doses (TCID50) have been administered to over 850 individuals in 12 clinical studies in healthy adults, melanoma patients, patients with atopic dermatitis, and HIV-1-infected patients with no drug-related serious adverse events occurring. No cases of myocarditis or pericarditis have been observed with MVA-BN (35, 65), but the present study was still designed to monitor specifically for cardiac toxicity. In the clinical program with MVA-BN vaccine, the vast majority of participants have received the vaccine via the subcutaneous route of administration. This route of administration has shown satisfactory immune responses and a good safety profile (65). T-cell immune responses by CTL and helper T lymphocytes (HTL) in enzyme-linked immunospot (ELISPOT) assays were highly correlated with the results of the antibody tests (65). In an HIV-1 prophylactic vaccine trial (HIV-NEF-003), Nef-specific cellular and humoral immune responses were induced in subjects. After three vaccinations, 10 of 14 subjects developed T-cell responses that recognized between one and five Nef epitopes (34).
The clinical safety and immunogenicity of a DNA vaccine (EP HIV-1090) encoding the HIV-1-derived CTL epitopes were previously evaluated when delivered alone or simultaneously with HIV-1-derived HTL epitopes in the form of a recombinant protein adsorbed to Alhydrogel as the adjuvant (28, 38). Only low levels of CTL responses were observed in both clinical trials despite the induction of high levels of polyfunctional HTL responses. Our working hypothesis was that delivery of the CTL and HTL epitopes using different vaccine delivery formats did not result in presentation to the immune system in the physically cognate manner required for optimal immunogenicity. This led to the proposal that increased immunogenicity could emanate from use of a heterologous prime-boost vaccine regimen comprised of both the DNA and viral-vectored vaccines, wherein both vaccine components direct the in vivo transcription, translation, processing, and presentation of CTL and HTL epitopes by transfected cells.
Thus, this clinical trial was designed to evaluate the safety of the two vaccines and the ability of the DNA vaccine EP-1233 to prime HIV-1-specific immune responses and the MVA-mBN32 to boost those responses. The heterologous EP-1233 prime and MVA-mBN32 boost regimen was viewed as the most promising approach based on animal studies and had the theoretical advantage of focusing the immune responses to the recombinant MVA on the encoded HIV-1 epitopes.
MATERIALS AND METHODS
Study design.
Our clinical trial evaluated two HIV-1 experimental vaccines: (i) a DNA plasmid-vectored vaccine (EP-1233) and (ii) a modified vaccinia virus Ankara (MVA-mBN32)-vectored vaccine. This multicenter, double-blinded, randomized, placebo-controlled phase 1 clinical trial (HVTN protocol 067) was sponsored by the National Institute of Allergy and Infectious Diseases (NIAID), Division of AIDS (DAIDS) and conducted at three HIV Vaccine Trials Units (HVTU) in the United States. The study protocol was approved by the local site institutional review boards and was carried out in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. Written informed consent was obtained from each subject after the nature and possible consequences of the study were fully explained. Participants were healthy adults, aged 18 to 40 years, who were HIV-1-uninfected and did not have a self-reported history of vaccinia virus vaccinations or clinical evidence of scarification from past vaccinia virus vaccination. Due to a possible association between unattenuated vaccinia virus used for smallpox vaccination, and myopericarditis, specific inclusion and exclusion criteria, along with enhanced cardiac safety monitoring, were included in this protocol to minimize the chances of enrolling anyone with preexisting myopericarditis or cardiovascular disease that could increase their risk from vaccination and to detect potential cardiac effects of the study vaccine.
A total of 36 volunteers were enrolled, 13 at the first site, 12 at the second site, and 11 at the third site, with 30 randomly assigned to receive vaccine and 6 to receive placebo. The DNA plasmid-vectored vaccine (EP1233) was administered first; two study immunizations were given at 0 and 28 days as two 1-ml intramuscular injections in the deltoid muscles of both arms each containing 2 mg of EP-1233, for a total of 4 mg per time point. The third and fourth immunizations were administered at 84 and 168 days as a single subcutaneous injection in the upper arm and consisted of a 0.5-ml injection of the MVA HIV-1 polytope vaccine (MVA-mBN32) containing 108 TCID50/ml. The placebo control recipients received the same volume and number of injections by the same routes as the vaccine recipients. The first 12 subjects were enrolled at no more than one per day with an ongoing evaluation of safety.
During the first 3 days after each study injection, participants reported all systemic and local reactions that had occurred. The severity of a reaction was defined as follows: (i) mild, transient or minimal symptoms; (ii) moderate, notable symptoms requiring modification of activity; and (iii) severe, incapacitating symptoms requiring bed rest and/or resulting in loss of work or social interaction. The clinical and laboratory safety data, including reactogenicity assessments and adverse events reported, were reviewed weekly during the vaccination period; data on adverse events were collected from subjects for all 12 months of study participation.
Specific cardiac assessments were conducted during the study as follows. Participants were questioned at study visits about symptoms and signs suggestive of myopericarditis or other cardiovascular complications, including shortness of breath, chest pain, palpitations, flu-like symptoms, and fatigue. Test results for cardiac troponin I, a biomarker for cardiac tissue injury, were normal at screening. Cardiac troponin I was repeated 2 weeks after each MVA-mBN32/MVA control vaccination. A 12-lead electrocardiogram (ECG) had to be normal at screening, and the test was repeated at 2 weeks after each MVA-mBN32 immunization. If cardiopulmonary symptoms were reported during the trial, the study staff performed a cardiopulmonary examination. After vaccination with MVA-mBN32 or its placebo control, participants who developed signs and symptoms or findings suggestive of a possible new cardiovascular condition, including myopericarditis (such as chest pain, dyspnea, palpitations, congestive heart failure, ECG abnormalities, or an elevated cardiac troponin I), were evaluated with an ECG, cardiac troponin I, and creatine kinase-MB isoenzyme (CK-MB), and an appropriate diagnostic evaluation as medically indicated.
At every clinic visit, HIV-1 risk reduction counseling was provided. Participants were monitored for incidents of social harm related to their participation in the protocol. Three commercially available enzyme-linked immunosorbent assay (ELISA) kits were used to detect HIV-1 infection.
Before the first study injection, 14 days after each study injection, and at months 9 and 12, blood specimens were obtained by venipuncture for safety assessments and to assess immune responses to vaccination. Peripheral blood mononuclear cells (PBMC) were purified from sodium heparin anti-coagulated whole blood within 8 h of venipuncture and cryopreserved (11).
Major histocompatibility complex (MHC) class I HLA molecular typing was done on all study subjects with available samples, as described previously (59). Briefly, the sequence based typing strategy we used queried exon 2 and exon 3 sequences for HLA class I analysis. All results were reported as HLA types according to the nomenclature outlined in the International ImMunoGenetics HLA database (www.ebi.ac.uk/imgt/hla/nomenclature/index.html).
Vaccines. (i) DNA plasmid vaccine EP-1233.
EP-1233 (Pharmexa-Epimmune, Inc.) was a DNA plasmid-vectored vaccine encoding 21 CTL and 18 HTL epitopes from Gag, Pol, Vpr, Nef, Rev, and Env. Epitope selection criteria and vaccine design and construction were described in detail previously (28, 38, 68, 70). Briefly, potential epitopes were identified based on HLA peptide-binding motifs using 128 HIV-1 sequences; approximately half of which were clade B and the remainder from other clades. Potential epitopes were initially selected based on supertype binding properties of the peptides to soluble HLA-A2, HLA-A3, and HLA-B7 HLA superfamily class I or the HLA-DR1,4,7 supertype molecules. Subsequent testing included immunogenicity assessments using HLA transgenic mice and antigenicity measured using PBMC obtained from HIV-1-infected donors. Based on HLA types the vaccines were predicted to induce CD8 and CD4 responses in ca. 85 and 100% of the general population, respectively, and regardless of ethnic background (70). The vaccine also encodes the universal HTL pan-DR epitope (PADRE, amino acid sequence AKFVAAWTLKAA), which has high binding affinity to a wide range of human and murine MHC class II molecules (1). PADRE induces helper-facilitated immunity in mice (1, 16) and lymphoproliferation in human PBMC (1). The PADRE HTL epitope was included as an adjuvant to increase the magnitude and duration of the CTL responses (37).
The EP-1233 DNA vaccine was developed from two sets of HIV-1 epitopes that were fused into a single contiguous reading frame; the N terminus of the gene product was composed of the CTL epitopes while the C terminus was composed of the HTL epitopes. Amino acid spacers were introduced between the epitopes to increase the processing efficiency and correspondingly, the potency of the vaccine. The full-length vaccine insert was assembled from overlapping synthetic oligonucleotides using Pfu DNA polymerase. The 5-prime end of the 843-bp sequence contains a consensus Kozak sequence to support translation of the gene product. A consensus Ig-κ signal sequence was fused to the 5-prime end of the protein coding sequence to facilitate transport of the protein product into the endoplasmic reticulum. A stop codon was included at the 3-prime end of the open reading frame to ensure accurate termination of translation. This construct was cloned into the HindIII and XbaI sites of the pMB75.6 vector backbone. The EP-1233 DNA vaccine plasmid encodes only two open reading frames: the kanamycin resistance gene and the synthetic HIV-1 epitope product.
EP-1233 bulk drug substance was produced in E. coli strain DH5α using high-density fermentation and purified from bacterial lysate material by ethanol precipitation and anion-exchange column chromatography by Althea Technologies, Inc. (San Diego, CA). The DNA vaccine was formulated with a biocompatible adhesive polymer polyvinylpyrrolidone (PVP; Plasdone C-30 [International Specialty Products, Wayne, NJ]). EP-1233 was a clear colorless solution containing 2 mg of DNA vaccine/ml. PVP was present at a concentration of 3.4% in sterile phosphate-buffered saline with vaccine and in the placebo control for the DNA vaccine. The PVP binds to DNA, stabilizes and protects it in vivo, facilitates the dispersion of the DNA through tissues, and augments uptake by skin and muscle cells, thus resulting in increased in vivo gene expression and vaccine immunogenicity (5, 43, 44).
(ii) MVA-mBN32 vaccine.
The modified vaccinia virus Ankara-HIV polyepitope (MVA-mBN32) vaccine encodes the same 21 CTL and 18 HTL HIV-1 epitopes but under separate promoters. The HTL gene was cloned into the intergenic region I4L/I5L of the MVA-BN genome, and the CTL gene was cloned into the deletion II site. Both recombinant inserts are under the control of the vaccinia virus early/late promoter p7.5.
The MVA-mBN32 clinical trial material was manufactured by Bavarian Nordic (Berlin, Germany) on primary chicken embryonic fibroblasts derived from specific pathogen-free eggs in a bioreactor culture using serum-free medium. The virus suspension was harvested and then subjected to ultrasonication, concentration, and purification by serial filtration steps. The purified harvest (bulk drug substance) was formulated in Tris-buffered saline and contained approximately 2 × 108 TCID50/ml. The dose used in the present study was 108 TCID50, corresponding to 0.5 ml as a single subcutaneous injection in the upper arm. A dose of 0.5 ml of Tris-buffered sterile saline was the control preparation for the MVA-mBN32 vaccine.
The vaccine materials were tested individually and using heterologous prime-boost schedules in rabbit studies by SRI (Menlo Park, CA) to determine biodistribution, clearance and general safety to support Phase 1 clinical testing in HIV-1-uninfected volunteers. Release and stability tests on the clinical supplies included appearance, pH, DNA concentration, DNA integrity, and immunogenicity measured using HLA-A2 transgenic mice.
Immunologic assays. (i) ICS assay.
PBMC were thawed and rested overnight, suspended in R10 (RPMI 1640 [Gibco-BRL, NY] containing 10% fetal calf serum [Gemini Bioproducts, CA], 2 mM l-glutamine [Gibco-BRL], 100 U of penicillin G/ml, 100 μg of streptomycin sulfate/ml), and incubated at 37°C in 5% CO2 prior to stimulation. A minimum cell viability of 66% measured after the overnight incubation on the day following the thawing procedure was required for use in the intracellular cytokine staining (ICS) assays. In the presence of brefeldin A (10 μg/ml; Sigma, St. Louis, MO) and 1 μg each of anti-CD28 and anti-CD49d antibodies (BD Biosciences, San Jose, CA)/ml, PBMC were stimulated for 6 h with (i) the HTL peptide pool consisting of the 18 HTL epitopes found in the vaccines, (ii) the CTL peptide pool consisting of the 21 CTL epitopes found in the vaccines, and (iii) the PADRE HTL epitope. For the flow cytometric analysis, the specimens were collected from 96-well plates using a high-throughput sampler (BD Biosciences) device on a BD LSRII flow cytometer and then analyzed using FlowJo software (Treestar, Inc., OR) and LabKey Flow (58).
The eight-color ICS protocol was previously validated (36) for detection of live gamma interferon (IFN-γ)- and interleukin-2 (IL-2)-secreting CD3+ CD8+ and CD3+ CD4+ HIV-1-specific T cells. In addition, both tumor necrosis factor alpha (TNF-α) and IL-4 expression were examined. The cells were first stained with violet live/dead fixable dead cell stain (Invitrogen/Molecular Probes, Eugene, OR) (47) and then fixed, permeabilized, and stained intracellularly with the following antibody reagents: CD3 phycoerythrin-Texas Red (PE-TR), CD4 fluorescein isothiocyanate, CD8 peridinin chlorophyll protein complex-cyanin 5.5 (PerCP-Cy), IFN-γ PE-Cy7, IL-2 PE, TNF-α Alexa 700, and IL-4 allophycocyanin (APC). All antibodies, except the CD3 PE-TR (Beckman-Coulter, Marseille, France) and perforin (Tepnel/Diaclone, Stamford, CT) were obtained from BD Biosciences. For some assays, anti-IL-4 APC was replaced with a perforin antibody that was conjugated to Alexa 647 (Invitrogen Corp., Carlsbad, CA) in the laboratory. At the time of the present study the analyses of IL-4, perforin, and TNF-α were not validated.
Positive responses and criteria for evaluable responses were determined as previously described (36) and were based on background measurements and the number of T cells examined. Since acceptability criteria were applied separately for CD3+ CD4+ and CD3+ CD8+ cells, the total number of specimens included in each ICS analysis could differ between the CD4+ and CD8+ T-cell evaluations.
(ii) IFN-γ ELISPOT assay.
PBMC samples (2 weeks after the fourth vaccination) from the three participants who had positive responses to the CTL peptide pool by ICS were further tested by ELISPOT assay to determine the specific peptides they responded to. ELISPOT assays were performed using a standardized, validated, bulk IFN-γ ELISPOT assay (21, 42) for each of the 21 CTL peptides representing the CTL epitopes in the vaccine.
(iii) Vaccinia virus-specific anti-MVA IgG antibody assay.
Vaccinia virus-specific antibodies were measured by using an automated direct ELISA on a Biomek FX (Beckman Coulter, Krefeld, Germany) on 96-well Maxisorb plates (Nunc, Wiesbaden, Germany) coated with a preparation of MVA-BN-infected CEF cell lysate in coating buffer (200 mM Na2CO3 [pH 9.6]), as described previously (66).
Statistical methods.
As part of the trial design, early evaluation of the immunogenicity response data determined whether the trial would stop after the first group was enrolled and completed follow-up. A determination of fewer than seven immunogenicity responses 2 weeks after the third immunization and 2 weeks after the fourth immunization stopped the trial after participants were enrolled in the first group. The sample size of 30 vaccine and 6 placebo recipients adequately allowed us to evaluate safety. Specifically, a sample size of 30 vaccinees provided a 90% chance of observing at least one serious adverse event, if the true rate of such an event was at least 8%.
To summarize the T-cell response data, positive response rates to any peptide pool were reported. The positivity of the ICS responses was determined by a one-sided Fisher exact test applied to each peptide pool-specific response versus the negative control response with a discrete Bonferroni adjustment for the multiple comparisons. Peptide pools with adjusted P values of < 0.00001 were considered positive (36). Positivity of the individual peptide IFN-γ ELISPOT responses was determined by a one-sided bootstrap test of the null hypothesis that the experimental well responses were twice those of the background (α = 0.05). A Westfall-Young (69) approach was used to adjust for the multiple comparisons across individual peptides. Peptides with adjusted one-sided P values of ≤0.05 were declared positive. In addition, the mean difference in the experimental and negative control wells had to exceed 50 spot-forming cells (SFC) per 106 PBMC for the response to be positive. Vaccinia virus-specific antibody titers were calculated by linear regression and defined as the serum dilution that resulted in an optical density of 0.30 (endpoint titers). A titer of 50 was the lowest reliably detectable antibody level (assay cutoff), and when this titer was reached, the subject was considered seropositive. Antibody titers below the cutoff titer in the assay were assigned an arbitrary value of 25 for the purpose of calculations. Geometric mean titers (GMTs) were calculated using the antilogarithm of the mean of the log10 titer transformation. SAS (version 9.1; SAS Institute) and R were used for all analyses.
Clinical trial registration number.
This study was performed under clinical trial registration number NCT00428337.
RESULTS
Description of study population: demographics, HLA genetic profile, retention.
The 36 study subjects were enrolled between May 2007 and September 2007. Demographics did not differ between study groups (Table 1). The HLA supertype A2, A3, and B7 phenotypes were each present in 40, 51, and 46%, respectively, of the 35 study subjects for whom HLA typing was done (Table 1). Sixteen subjects were phenotyped as positive for only one of these three HLA supertype alleles, 13 subjects were positive for two of the supertypes, two subjects were positive for all three, and 31 (88.6%) of the 35 subjects were positive for one or more of the supertypes.
Table 1.
Demographics, vaccinations, and HLA genetic profile
| Parameter | No. of subjects (%)a |
|
|---|---|---|
| DNA/MVA vaccinees (n = 30) | Placebo controls (n = 6) | |
| Gender | ||
| Male | 17 (57) | 4 (67) |
| Female | 13 (43) | 2 (33) |
| Race/ethnicity | ||
| White, non-Hispanic | 27 (91) | 5 (83) |
| Black/African American, non-Hispanic | 1 (3) | 0 |
| Hispanic | 1 (3) | 0 |
| Asian | 1 (3) | 0 |
| Multiracial | 0 | 1 (17) |
| Median age (yr) | 26 | 28 |
| Age range (yr) | 18-38 | 20-39 |
| Vaccination received by study day | ||
| Day 0 | 30 (100) | 6 (100) |
| Day 28 | 30 (100) | 6 (100) |
| Day 84 | 28 (93) | 6 (100) |
| Day 168 | 26 (87) | 6 (100) |
| MHC class I HLA supertypeb | ||
| A2 | 11 (38) | 3 (50) |
| A3 | 14 (48) | 4 (67) |
| B7 | 12 (41) | 4 (67) |
Except as noted otherwise in column 1.
MHC class I HLA molecular typing was performed for a total of 35 subjects: 29 vaccine and 6 placebo control recipients.
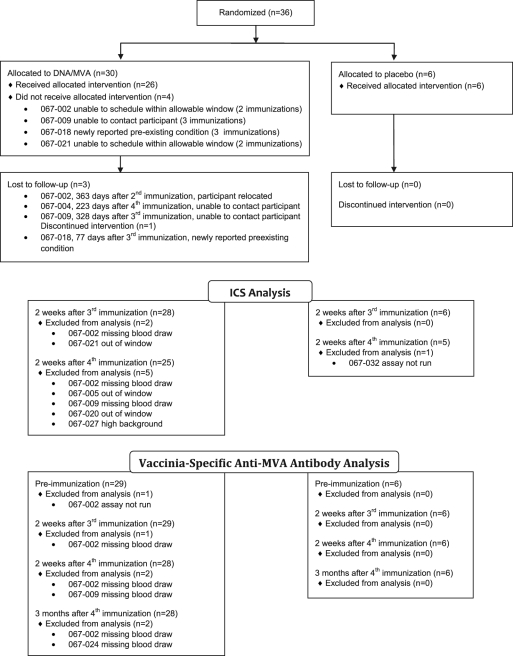
Randomization and follow-up of study subjects is summarized in Fig. 1. All but 4 of the 36 subjects received all study treatment injections; these four subjects, who were all vaccine recipients, included two who did not receive the two MVA-mBN32 injections and two who did not receive the second MVA-mBN32 injection. The reasons were either loss to follow-up or lack of availability to receive the vaccine at the protocol-specified study time in three subjects and identification of a preexisting health condition in the fourth. Two of the four subjects who did not receive all study vaccinations and one subject who received all vaccinations did not complete all study visits.
Fig 1.
Randomization, allocation, follow-up, and immunogenicity testing of enrolled study subjects. The numbers of volunteers screened who did not meet eligibility criteria or chose not to participate was not tracked. ICS is the intracellular cytokine staining assay for cellular immunogenicity assessment. MVA, modified vaccinia virus Ankara.
Safety assessment.
Local injection site erythema and induration were more frequent in the 3 days after injection with MVA-mBN32 than with EP-1233 DNA vaccine, and erythema and induration of moderate severity were more common after the second MVA-mBN32 injection than after the first (Table 2). Resolution of the injection site induration after the first MVA-mBN32 injection was delayed past 3 days in six subjects (resolution at days 8, 9, 13, 23, 40, and 57 postvaccination), and resolution after the second MVA-mBN32 injection was delayed past 3 days in seven subjects (resolution at days 5, 6, 7, 9, 10, 10, and 47 postvaccination). Pain and/or tenderness in the first 3 days after injection was least frequent (70%) after the second EP-1233 DNA vaccination and most frequent (96%) after the second MVA-mBN32 vaccination.
Table 2.
Local injection site and systemic symptoms within 3 days of vaccination with either EP-1233 DNA or MVA-mBN32 vaccines
| Symptom or diagnosis | No. of subjects (% of total evaluated) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EP-1233 DNA |
MVA-mBN32 |
|||||||||||
| Day 0 (n = 30) |
Day 28 (n = 30) |
Day 84 (n = 28) |
Day 168 (n = 26) |
|||||||||
| Mild | Moderate | Severe | Mild | Moderate | Severe | Mild | Moderate | Severe | Mild | Moderate | Severe | |
| Local | ||||||||||||
| Pain and/or tenderness | 24 (80) | 2 (7) | 0 | 20 (67) | 1 (3) | 0 | 21 (75) | 3 (11) | 0 | 19 (73) | 6 (23) | 0 |
| Erythema | 0 | 0 | 0 | 1 (3) | 0 | 0 | 12 (43) | 1 (4) | 0 | 11 (42) | 6 (23) | 2 (8) |
| Induration | 0 | 0 | 0 | 1 (3) | 0 | 0 | 11 (39) | 0 | 0 | 11 (42) | 5 (19) | 0 |
| Systemic | ||||||||||||
| Malaise and/or fatigue | 4 (13) | 1 (3) | 0 | 4 (13) | 0 | 0 | 5 (18) | 3 (11) | 0 | 7 (27) | 0 | 0 |
| Myalgia | 4 (13) | 1 (3) | 0 | 3 (10) | 0 | 0 | 7 (25) | 1 (4) | 0 | 3 (12) | 0 | 0 |
| Headache | 7 (23) | 0 | 0 | 5 (17) | 2 (7) | 0 | 6 (21) | 0 | 0 | 5 (19) | 2 (8) | 0 |
| Nausea | 2 (7) | 0 | 0 | 1 (3) | 0 | 0 | 0 | 0 | 0 | 2 (8) | 1 (4) | 0 |
| Vomiting | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 (4) | 0 |
| Chills | 1 (3) | 0 | 0 | 1 (3) | 0 | 0 | 2 (7) | 0 | 0 | 0 | 0 | 0 |
| Arthralgia | 3 (10) | 0 | 0 | 2 (7) | 0 | 0 | 0 | 1 (4) | 0 | 1 (4) | 0 | 0 |
| Maximum of all systemic symptoms overall | 12 (40) | 1 (3) | 0 | 9 (30) | 2 (7) | 0 | 7 (25) | 3 (11) | 0 | 11 (42) | 3 (12) | 0 |
The injection site reactogenicity during the 3 days after the first and second immunizations with the placebo control preparation consisted of mild pain and/or tenderness and was similar to that after immunization with the EP-1233 DNA vaccine. The injection site signs and symptoms during the 3 days after the third and fourth immunizations with placebo control preparation included infrequent mild pain and/or tenderness and erythema.
The proportions of subjects with systemic reactogenicity symptoms during the three day postinjection period did not differ between those observed after EP-1233 DNA vaccine and MVA-mBN32 vaccine injections (Table 2). Only one subject experienced fever during the 3 days postvaccination (grade 1, 37.7 to 38.6°C), which was after the second MVA-mBN32 vaccination. Systemic reactogenicity during the 3 days after control injections was less than after either vaccine preparation.
No adverse events were related to EP-1233 DNA vaccine. From the time of the first MVA-mBN32 vaccine injection, 19 (63.3%) subjects had one or more related adverse events, of which 10 were an injection site nodule (definitely related), six were mild injection site ecchymoses (five definitely and one probably related), four were injection site erythema (two definitely and two probably related), four were injection site induration (three definitely and one probably related), four were injection site pruritus (all definitely related), two were an aspartate aminotransferase elevation (both possibly related), three were injection site exfoliation (one definitely and two probably related), two were injection site swelling (all three definitely related), and one was injection site pain (probably related). From the time of the first placebo control injection for MVA-mBN32, one adverse event was thought to be definitely related (injection site hematoma) and one possibly related (throat irritation).
Cardiac troponin I levels were all within normal range for all participants. Adverse events that could have represented cardiac-related conditions included 32 classified as upper respiratory infection, four as influenza, and one each as musculoskeletal chest pain, cough, dyspepsia, dyspnea, fatigue, and palpitations. All of these were determined to have an etiology other than myopericarditis. The ECG tracings remained normal except in one subject who received the MVA-mBN32 vaccine and had a QTc interval prolongation (435 ms) that was 83 ms over baseline on the ECG done 3 weeks after the fourth vaccination. This adverse event was considered severe, because the interval was at least 60 ms greater than baseline, but was deemed unrelated to the study by the site investigator. The adverse event resolved 9 days later when the QTc interval (407 ms) was 55 ms over the baseline interval. This subject reported use of trazodone and bupropion during this time and may have used methamphetamine. The subject was asymptomatic and had a normal cardiopulmonary evaluation.
Assessment of the injection sites of MVA-mBN32 recipients resulted in reports of unsolicited local injection site adverse reactions that consisted of discrete subcutaneous nodules of mild severity in eight subjects after the first and in six subjects after the second MVA-mBN32 injection and were related to study vaccine. Of the six subjects with a subcutaneous nodule after the second MVA-mBN32 injection, four had the same type of finding after the first MVA-mBN32 injection. Onset was zero to 8 days after vaccination and the range of days to resolution was three to 92 days. None were reported to be painful or tender, and the sizes varied from about 2 mm to 4.5 cm. A uniform method for assessing these nodules was not part of the prospective evaluation of the injection site, so it was not standardized.
Study subjects were assessed for social impact events prospectively throughout the study. Two subjects reported three personal relationship events of minimal impact on quality of life, such as family members expressing concern for their health. Despite staff assistance, two events remained unresolved. There were no reports of problems with employment, education, medical/dental care, health/life insurance, travel/immigration, a military/other government agency, or HIV antibody testing outside of the study.
None of the subjects had a positive diagnostic test for antibodies to HIV-1 by any of the three diagnostic test kits used to test sera obtained at end-of-study participation. The HIV-1 peptides in the vaccine were T-cell, not B-cell epitopes and were not chosen to induce HIV-1-specific antibodies.
Immunogenicity. (i) Cellular immune response.
HIV-1-specific immunogenicity was assessed by ICS assay with PBMC samples obtained on day 98, which was 2 weeks after the third immunization (n = 34), and on day 182, which was 2 weeks after the fourth immunization (n = 30). Cellular immune responses were detected in 3 (12%) of 25 subjects who received vaccine when measured 2 weeks after the fourth immunization (Table 3 and Fig. 2). IFN-γ and IL-2 are the validated cytokines in the ICS assay, and the positivity assessments were based only on these two cytokines. TNF-α and IL-4 were also examined after the third immunization. Figure 2 shows the expression of all four cytokines for the one vaccine recipient with a positive CD4+ T-cell response at this time point. None of the vaccine-induced cells produced IL-4. TNF-α was coproduced by a large proportion of cells, although few cells produced TNF-α without either IFN-γ or IL-2. Because IL-4 was not detected, the ICS assay was modified for the measurements after the fourth immunization to instead examine perforin, a marker of cytotoxic potential. The responder at the earlier time point also had a CD4+ T-cell response at this time point. A similar representation of IFN-γ, IL-2, and TNF-α was observed, without the expression of perforin. Two other vaccine recipients had CD8+ T-cell responses at this later time point. For one subject, a large proportion of the responding cells expressed perforin (Fig. 2C, left), but for the other, few expressed perforin (right). IL-2 was produced by few of the CD8+ T cells for either one. Thus, although only two participants had CD8+ T-cell responses, CD8+ T cells with cytotoxic potential were induced.
Table 3.
Cellular immune responses measured by ICS for IL-2 and/or IFN-γ
| Study treatment group | Study day | No. of samples tested | No. positivea (%) |
|---|---|---|---|
| Vaccine recipients | 98 | 28 | 1 (3.6) |
| 182 | 25 | 3 (12) | |
| Placebo control recipients | 98 | 6 | 0 (0) |
| 182 | 5 | 0 (0) |
That is, the number of subjects with detectable IL-2 and/or IFN-γ cytokine production by CD3+ CD4+ and/or CD3+ CD8+ T cells.
Fig 2.
T-cell functional profiles for the three vaccine recipients with positive responses as determined by ICS for CD4+ or CD8+ T cells producing IFN-γ and/or IL-2. The MHC class I HLA supertypes were A3, B7 for subject 067-035, A2 for subject 067-007, and A3 for subject 067-025. (A) Expression of IFN-γ, IL-4, and TNF-α is shown for the CD4+ T cells from subject 067-035 2 weeks following the first MVA in response to stimulation with the CTL and HTL peptide pools and the PADRE peptide. (B) Expression is shown for the CD4+ T cells from subject 067-035 2 weeks following the second MVA in response to stimulation with the CTL peptide pool. (C) Expression of cytokines and perforin is shown for CD8+ T cells for two vaccine recipients 2 weeks after the second MVA in response to stimulation with the CTL peptide pool. The four functions—IFN-γ, IL-2, perforin, and TNF-α—were examined for subject 067-025 (left). TNF-α was not stained in the experiment that examined the sample from subject 067-007 (right). For each pie graph, the pie slices show the proportion of the total cytokine-producing cells that are producing 1, 2, or 3 cytokines/functions as noted in the gray-scale key (none produce all four functions). The arcs surrounding the pie graphs show the proportion of the cells producing each of the cytokines as noted in the color key. Overlapping pie arcs indicate multifunctional cells. The percent within each graph shows the background-subtracted percentage of the CD4+ or CD8+ T cells producing IFN-γ and/or IL-2 (the validated cytokine measurement used to determine positivity).
PBMC from all three responders in the ICS assay at day 182 were further tested using the IFN-γ ELISPOT assay to determine the specific peptides among the 21 CTL epitopes in the CTL peptide pool that were responsible for cytokine induction. Only one of the three responders (study subject 067-025) had a positive response measured using the IFN-γ ELISPOT assay, and this was to only one CTL epitope peptide, Gag 271 (single-letter amino acid code sequence MTNNPPIPV), showing a mean of 40.8 background-adjusted mean SFC per 2 × 105 PBMC.
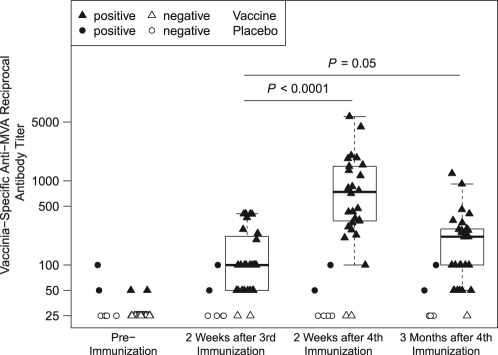
(ii) Vaccinia virus-specific antibodies to MVA.
Four subjects had detectable antibodies to MVA prior to first immunization (2 [33%] of 6 control subjects and 2 [6.9%] of 29 vaccine recipients). Two weeks after the first and second MVA-mBN32 immunizations, 27(93%) of 29 and 26 (93%) of 28 subjects, respectively, had detectable antibodies. Both MVA-mBN32 vaccine recipients with detectable antibodies to MVA prior to the first immunization had a reciprocal antibody titer of 50, and both experienced a 4-fold increase in antibody titer. The anti-MVA antibody GMT was at least 4-fold greater at 14 days after the second MVA-mBN32 immunization (GMT = 694) and statistically higher than the antibody GMT measured 14 days after the first MVA-mBN32 immunization (GMT = 115.5) (P < 0.0001). At 3 months after the second MVA-mBN32 immunization the antibody GMT declined to 167.1 (Fig. 3).
Fig 3.
The vaccinia virus-specific IgG antibody titers measured by ELISA are plotted for individual vaccine and placebo control group study subjects by study time point. Study subjects first received two immunizations with the DNA plasmid-vectored vaccine (EP1233) or placebo control on study days 0 and 28 and then received the recombinant modified vaccinia virus Ankara (MVA)-vectored vaccine (MVA-mBN32) or placebo control, as third and fourth immunizations on study days 84 and 168. Closed symbols represent anti-MVA antibody titers classified as positive for antibody in the assay. Open symbols that represent subjects without detectable anti-MVA antibody in the ELISA are plotted as an antibody titer of 25. The geometric mean titer (GMT) of positive antibody titers is shown as a horizontal line within each box. The boxes represent the interquartile range and the whiskers extend to the data point which is no more than 1.5 times the interquartile range.
DISCUSSION
This phase 1 study tested the safety and immunogenicity of a DNA plasmid and recombinant MVA-vectored vaccines, both encoding defined HIV-1 CTL epitopes within Env, Gag, Nef, Pol, Rev, and Vpr genes that are restricted by the HLA-A2, -A3, and -B7 HLA superfamily allelic products, defined HTL epitopes of HIV-1 within Env, Gag, Pol, and Vpr genes, and the PADRE HTL epitope. This represents the first clinical trial of these second-generation multiepitope vaccines. The prime-boost vaccination design was chosen in part because of the low level of immunogenicity in a previous clinical trial of a DNA plasmid-vectored vaccine, EP HIV-1090, that encoded only the CTL epitopes and PADRE, and was administered alone (28). Another clinical trial that was ongoing at the time our study was planned, included administration of the same HIV-1 HTL epitopes expressed as a recombinant polypeptide protein given alone or in combination with the previously tested EP HIV-1090 DNA plasmid-vectored vaccine (38). The recombinant polypeptide protein induced polyfunctional CD4+ helper T-cell responses in two-thirds of subjects after two immunizations, but the EP HIV-1090 vaccine was minimally immunogenic, failing to reproducibly induce either CD4+ or CD8+ T-cell responses (38).
EP-1233 and MVA-mBN32 in our study were both safe and well tolerated with more local injection site reactogenicity, and more adverse events were observed after administration of the MVA-mBN32 than the EP-1233 DNA plasmid-vectored vaccines. There were no proven episodes of myopericarditis and no cardiotoxicity in association with the MVA-BN vaccine. Although myopericarditis cannot be eliminated as a cause, the QTc interval prolongation after MVA vaccination in one subject may have been related to trazodone, bupropion, or methamphetamine use reported by the subject (17, 49). Amphetamines are associated with acute and chronic cardiotoxicities, but unlike trazodone and bupropion, do not appear on lists of drugs that cause QTc interval prolongation. Myocarditis is a cause of QTc interval prolongation (50); however, this subject did not have other reasons to invoke this as the cause. Systemic reactions were infrequent and mild in the vaccine group, and not different comparing the DNA plasmid-vectored vaccine to the MVA-BN32 vaccine, but were more common than among the placebo control recipients. The subcutaneous nodules at the MVA-mBN32 injection site were a different phenomenon than injection site induration, resolved more slowly, were clinically not very significant and have not been reported in studies employing other MVA vaccines.
A low rate of IL-2- and IFN-γ-secreting CD4+ and CD8+ T-cell responses was detected by ICS in the present study; all four positive specimens from the three vaccine responders had T-cell responses to the CTL peptide pool manifested by IL-2, IFN-γ, and TNF-α production and perforin by the CD8+ T cells. One participant's cells from one time point produced IL-2, IFN-γ, and TNF-α in response to the HTL peptide pool and PADRE. Cells from one subject whose CD8+ T cells produced IFN-γ, TNF-α, and perforin in response to the CTL peptide pool in the ICS assay also produced IFN-γ to one HIV-1 Gag peptide that is a CTL epitope in the ELISPOT assay.
Low levels of CTL and HTL responses induced by this prime-boost vaccination regimen were not due to lack of an immune response to MVA. Antibodies to MVA-BN were induced by the MVA-mBN32 vaccine. Also, the historical and clinical assessments to exclude persons who previously had been vaccinated with vaccinia virus were in general successful since only two vaccine recipients and two placebo recipients had detectable antibody at low titer to MVA at day 0. The subjects with detectable anti-MVA antibody before vaccination did not have T-cell cytokine responses in the ICS assay. Antibodies to MVA were boosted to the highest level after the second MVA-mBN32 vaccination compared to after the first and waned to levels similar to those after the first vaccination by 3 months after the second vaccination.
Clinical studies in the literature have reported use of the plasmid DNA/recombinant MVA prime-boost vaccination strategy consisting of other constructs expressing HIV-1 proteins with demonstration of a good safety profile, lack of cases of myopericarditis and various rates of CD4+ and CD8+ T-cell immune responses to the HIV-1 components (13, 27, 29, 30, 32, 48, 53). The dose, route of administration, quality of immune priming achieved with the DNA plasmid vector, sensitivity of the assays used to measure vaccine-induced T-cell responses, and time after booster immunization when peak response is measured all may affect observed response rates to the prime-boost vaccination regimens of between about 10 and 92% (27, 29, 30, 32, 48, 53). Previous immune status to vaccinia virus did not appear to affect responses to HIV-1 proteins expressed by at least one candidate MVA vaccine (29).
The low level of immunogenicity associated with these vaccines is similar to that of others based largely on the use of defined CTL epitopes (13, 27, 32). We included several design features which differentiate the product tested here and which we believed would increase vaccine potency. These features were the selection of the highest affinity HLA-supertype epitopes, the use of spacers to optimize epitope processing and presentation, the inclusion of the universal PADRE HTL epitope as an adjuvant and formulation with PVP to augment cellular uptake of the plasmid DNA. Despite these features the EP-1233 DNA failed to efficiently prime immune responses.
We now believe the observed poor levels of immunogenicity in our study and others using epitope-based vaccines may well reflect a suboptimal match between the vaccine design and the DNA and MVA vectors with respect to how the epitopes are delivered to the immune system. Most recent experimental evidence indicates a dominant role for the cross-presentation pathway following intramuscular vaccine immunogen delivery using DNA plasmid vectors, although some data support a minor role for direct antigen presentation in vivo by transfected myocytes (14, 22, 51, 54, 57). Vaccinia viruses and MVA can infect professional antigen-presenting cells, such as dendritic cells, and thus may be able to mediate vaccine immunogen presentation through the direct priming pathway. However, this infection can impact dendritic cell maturation and function, and evidence points to the dominant use of the cross-presentation pathway for the induction of cellular immune responses to the transgene and viral proteins for vaccinia virus vaccines and MVA-based vectors (20, 23, 39, 56). A recent report of high levels of HIV-1-specific CD4+ (77%) and CD8+ (42%) T-cell responses to other DNA plasmid and recombinant MVA-vectored vaccines that encode noninfectious virus-like particles of HIV-1 and were administered in a heterologous prime-boost regimen as in our study supports the need for emphasis on optimizing the HIV-1 insert to achieve a desirable cellular immune response (26).
Efficient induction of cellular immune responses mediated using cross-presentation appears to require stable protein antigen as the substrate and accumulation of amounts sufficient to induce responses, whereas direct presentation is efficient when unstable or rapidly degraded proteins are presented (46, 55, 63, 71). The EP1233 and the MVA-mBN32 vaccines in our study both encode unnatural genes composed of CTL and HTL epitopes separated by spacer sequences designed to optimize intracellular processing of individual epitopes within transfected or infected cells (5, 28). Although it is feasible that this design could support efficient induction of CTL via the transfer of proteasome substrates (46), the results from our clinical trial indicate otherwise. Overall, our current understanding of the DNA and MVA vaccine vectors and this phase 1 clinical trial result suggest that these vector platforms are not well-suited for use with T-cell epitope-based vaccines (9, 25, 51, 64). Vaccine delivery methods that efficiently deliver epitope-based vaccines to professional antigen presenting cells will need to be investigated to further develop the concept of epitope-based vaccines.
Conclusions.
In summary, our study demonstrated higher reactogenicity and adverse event rates with MVA-mBN32 compared to the DNA plasmid-vectored vaccine, but the MVA was still well-tolerated. These vaccines given in high dose and prime-boost sequence did not elicit adequate HIV-1-specific T-cell immune responses and further optimization of the HIV-1 T-cell epitope-based constructs expressed by DNA plasmids and MVA-vectored vaccines is needed.
ACKNOWLEDGMENTS
This study was supported by grants from the NIAID to Saint Louis University (U01AI-48021), to Pharmexa-Epimmune (contract N01AI-30031), to the HIV Vaccine Trials Network (U01AI-46747), and to the following clinical study sites: University of Rochester, Rochester, NY (U01AI-069511); Vanderbilt University, Nashville, TN (CTSA grant UL1 RR024975 from the NCRR/NIH); and the San Francisco Department of Health, San Francisco, CA (1 U01 AI-069496-01).
We thank all past and present members of the HVTN-067 team whose names have not appeared as coauthors, but whose contributions were nonetheless critical for the success of the study. We thank all sites' staff for recruiting volunteers and administering the vaccinations. We thank all of the volunteers whose participation made this clinical trial possible. We thank Carolyn Novotny and Lin Cowick for manuscript preparation at Saint Louis University. We thank Scharla G. Estep, Pharmacist, Pharmaceutical Affairs Branch of the Office of Policy for Clinical Research Operations, DAIDS, NIAID, and Dale N. Lawrence and Alan Fix, DAIDS for assistance with data safety review and trial conduct. We also thank Danielle Harden for statistical assistance at SCHARP, Cathy Bunce at the University of Rochester, and the study staff at Vanderbilt University and the HIV Research Section at the San Francisco Department of Health, San Francisco, CA.
Footnotes
Published ahead of print 8 March 2012
REFERENCES
- 1. Alexander J, et al. 1994. Development of high potency universal DR-restricted helper epitopes by modification of high-affinity DR-blocking peptides. Immunity 1:751–761 [DOI] [PubMed] [Google Scholar]
- 2. Allen TM, et al. 2000. Induction of AIDS virus-specific CTL activity in fresh, unstimulated peripheral blood lymphocytes from rhesus macaques vaccinated with a DNA prime/modified vaccinia virus Ankara boost regimen. J. Immunol. 164:4968–4978 [DOI] [PubMed] [Google Scholar]
- 3. Amara RR, et al. 2002. Critical role for Env as well as Gag-Pol in control of a simian-human immunodeficiency virus 89.6P challenge by a DNA prime/recombinant modified vaccinia virus Ankara Vaccine J. Virol. 76:6138–6146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Amara RR, et al. 2001. Control of a mucosal challenge and prevention of AIDS by a multiprotein DNA/MVA vaccine. Science 292:69–74 [DOI] [PubMed] [Google Scholar]
- 5. Anwer K, et al. 1999. Synergistic effect of formulated plasmid and needle-free injection for genetic vaccines. Pharm. Res. 16:889–895 [DOI] [PubMed] [Google Scholar]
- 6. Barouch DH, et al. 2001. Reduction of simian-human immunodeficiency virus 89.6P viremia in rhesus monkeys by recombinant modified vaccinia virus Ankara vaccination. J. Virol. 75:5151–5158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Barouch DH, et al. 2000. Control of viremia and prevention of clinical AIDS in rhesus monkeys by cytokine-augmented DNA vaccination. Science 290:486–492 [DOI] [PubMed] [Google Scholar]
- 8. Belshe RB, et al. 2001. Safety and immunogenicity of a canarypox-vectored human immunodeficiency virus type 1 vaccine with or without gp120: a phase 2 study in higher- and lower-risk volunteers. J. Infect. Dis. 183:1343–1352 [DOI] [PubMed] [Google Scholar]
- 9. Bins AD, Wolders MC, van den Boom MD, Haanen JB, Schumacher TN. 2007. In vivo antigen stability affects DNA vaccine immunogenicity. J. Immunol. 179:2126–2133 [DOI] [PubMed] [Google Scholar]
- 10. Blanchard TJ, Alcami A, Andrea P, Smith GL. 1998. Modified vaccinia virus Ankara undergoes limited replication in human cells and lacks several immunomodulatory proteins: implications for use as a human vaccine. J. Gen. Virol. 79:1159–1167 [DOI] [PubMed] [Google Scholar]
- 11. Bull M, et al. 2007. Defining blood processing parameters for optimal detection of cryopreserved antigen-specific responses for HIV vaccine trials. J. Immunol. Methods 322:57–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Carroll MW, Moss B. 1997. Host range and cytopathogenicity of the highly attenuated MVA strain of vaccinia virus: propagation and generation of recombinant viruses in a nonhuman mammalian cell line. Virology 238:198–211 [DOI] [PubMed] [Google Scholar]
- 13. Cebere I, et al. 2006. Phase I clinical trial safety of DNA- and modified virus Ankara-vectored human immunodeficiency virus type 1 (HIV-1) vaccines administered alone and in a prime-boost regime to healthy HIV-1-uninfected volunteers. Vaccine 24:417–425 [DOI] [PubMed] [Google Scholar]
- 14. Cho JH, Youn JW, Sung YC. 2001. Cross-priming as a predominant mechanism for inducing CD8+ T cell responses in gene gun DNA immunization. J. Immunol. 167:5549–5557 [DOI] [PubMed] [Google Scholar]
- 15. de Bruyn G, et al. 2004. Safety profile of recombinant canarypox HIV vaccines. Vaccine 22:704–713 [DOI] [PubMed] [Google Scholar]
- 16. del Guercio MF, et al. 1997. Potent immunogenic short linear peptide constructs composed of B cell epitopes and Pan DR T helper epitopes (PADRE) for antibody responses in vivo. Vaccine 15:441–448 [DOI] [PubMed] [Google Scholar]
- 17. DePonti F, Poluzzi E, Cavalli A, Recanatini M, Montanaro N. 2002. Safety of non-antiarrhythmic drugs that prolong the QT interval or induce torsade de pointes. Drug Safety 25:263–286 [DOI] [PubMed] [Google Scholar]
- 18. Doria-Rose NA, et al. 2003. Multigene DNA priming-boosting vaccines protect macaques from acute CD4+-T-cell depletion after simian-human immunodeficiency virus SHIV89.6P mucosal challenge. J. Virol. 77:11563–11577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Drexler I, Heller K, Wahren B, Erfle V, Sutter G. 1998. Highly attenuated modified vaccinia virus Ankara replicates in baby hamster kidney cells, a potential host for virus propagation, but not in various human transformed and primary cells. J. Gen. Virol. 79:347–352 [DOI] [PubMed] [Google Scholar]
- 20. Drexler I, et al. 2003. Identification of vaccinia virus epitope-specific HLA-A*0201-restricted T cells and comparative analysis of smallpox vaccine. Proc. Natl. Acad. Sci. U. S. A. 100:217–222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dubey S, et al. 2007. Detection of HIV vaccine-induced cell-mediated immunity in HIV-seronegative clinical trial participants using an optimized and validated enzyme-linked immunospot assay. J. Acquir. Immune Defic. Syndr. 45:20–27 [DOI] [PubMed] [Google Scholar]
- 22. Fu T-M, et al. 1997. Priming of cytotoxic T lymphocytes by DNA vaccines: requirement for professional antigen-presenting cells and evidence for antigen transfer from myocytes. Mol. Med. 3:362–371 [PMC free article] [PubMed] [Google Scholar]
- 23. Gasteiger G, Kastenműller W, Ljapoci R, Sutter G, Drexler I. 2007. Cross-priming of cytotoxic cells dictates antigen requisites for Modified vaccinia virus Ankara vector vaccines. J. Virol. 81:11925–11936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gilbert PB, et al. 2003. Long-term safety analysis of preventive HIV-1 vaccines evaluated in AIDS vaccine evaluation group NIAID-sponsored phase I and II clinical trials. Vaccine 21:2933–2947 [DOI] [PubMed] [Google Scholar]
- 25. Giri M, Ugen KE, Weiner DB. 2004. DNA vaccines against human immunodeficiency virus type 1 in the past decade. Clin. Microbiol. Rev. 17:370–389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Goepfert PA, et al. 2011. Phase 1 safety and immunogenicity testing of DNA and recombinant modified vaccinia Ankara vaccines expressing HIV-1 viruslike particles. J. Infect. Dis. 203:610–619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Goonetilleke N, et al. 2006. Induction of multifunctional human immunodeficiency virus type 1 (HIV-1)-specific T cells capable of proliferation in healthy subjects by using a prime-boost regimen of DNA- and modified vaccinia virus Ankara-vectored vaccines expressing HIV-1 Gag coupled to CD8+ T-cell epitopes. J. Virol. 80:4717–4728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gorse GJ, et al. 2008. Safety and immunogenicity of cytotoxic T-lymphocyte poly-epitope, DNA plasmid (EP HIV-1090) vaccine in healthy, human immunodeficiency virus type 1 (HIV-1)-uninfected adults. Vaccine 26:215–223 [DOI] [PubMed] [Google Scholar]
- 29. Gudmundsdotter L, et al. 2009. Recombinant modified vaccinia Ankara (MVA) effectively boosts DNA-primed HIV-specific immune responses in humans despite preexisting vaccinia immunity. Vaccine 27:4468–4474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Guimarães-Walker A, et al. 2008. Lessons from IAVI-006, a phase I clinical trial to evaluate the safety and immunogenicity of the pTHr.HIVA DNA and MVA.HIVA vaccines in a prime-boost strategy to induce HIV-1 specific T-cell responses in healthy volunteers. Vaccine 26:6671–6677 [DOI] [PubMed] [Google Scholar]
- 31. Gupta K, et al. 2002. Safety and immunogenicity of a high-titered canarypox vaccine in combination with rgp120 in a diverse population of HIV-1-uninfected adults: AIDS Vaccine Evaluation Group Protocol 022A. J. Acquir. Immune Defic. Syndr. 29:254–261 [DOI] [PubMed] [Google Scholar]
- 32. Hanke T, McMichael AJ, Dorrell L. 2007. Clinical experience with plasmid DNA- and modified vaccinia virus Ankara-vectored human immunodeficiency virus type 1 clade A vaccine focusing on T-cell induction. J. Gen. Virol. 88:1–12 [DOI] [PubMed] [Google Scholar]
- 33. Hanke T, et al. 1999. Effective induction of simian immunodeficiency virus-specific cytotoxic T lymphocytes in macaques by using a multiepitope gene and DNA prime-modified vaccinia virus Ankara boost vaccination regimen. J. Virol. 73:7524–7532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hain J, et al. 2005. MVA-Nef, the prophylactic vaccination phase I trial: immunization with MVA-Nef is safe and immunogenic in HIV-1 negative volunteers. AIDS Vaccine 2005, Montreal, Quebec, Canada [Google Scholar]
- 35. Harrer E, et al. 2005. Therapeutic vaccination of HIV-1-infected patients on HAART with a recombinant HIV-1 nef-expressing MVA: safety, immunogenicity, and influence on viral load during treatment interruption. Antivir. Ther. 10:285–300 [PubMed] [Google Scholar]
- 36. Horton H, et al. 2007. Optimization and validation of an 8-color intracellular cytokine staining (ICS) assay to quantify antigen-specific T cells induced by vaccination. J. Immunol. Methods 323:39–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ishioka GY, et al. 1999. Utilization of MHC class I transgenic mice for development of minigene DNA vaccines encoding multiple HLA-restricted CTL epitopes. J. Immunol. 162:3915–3925 [PubMed] [Google Scholar]
- 38. Jin X, et al. 2009. A novel HIV T helper epitope-based vaccine elicits cytokine-secreting HIV-specific CD4+ T cells in a phase I clinical trial in HIV-uninfected adults. Vaccine 27:7080–7086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kastenműller W, et al. 2006. Infection of human dendritic cells with recombinant vaccine virus MVA reveals general persistence of viral transcription but distinct maturation-dependent cytopathogenicity. Virology 350:276–288 [DOI] [PubMed] [Google Scholar]
- 40. Kent SJ, et al. 1998. Enhanced T-cell immunogenicity and protective efficacy of a human immunodeficiency virus type 1 vaccine regimen consisting of consecutive priming with DNA and boosting with recombinant fowlpox virus. J. Virol. 72:10180–10188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. McConkey SJ, et al. 2003. Enhanced T-cell immunogenicity of plasmid DNA vaccines boosted by recombinant modified vaccinia virus Ankara in humans. Nat. Med. 9:729–735 [DOI] [PubMed] [Google Scholar]
- 42. McElrath MJ, et al. 2008. HIV-1 vaccine-induced immunity in the test-of-concept step study: a case–cohort analysis. Lancet 372:1894–1905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Mumper RJ, et al. 1996. Polyvinyl derivatives as novel interactive polymers for controlled gene delivery to muscle. Pharm. Res. 13:701–709 [DOI] [PubMed] [Google Scholar]
- 44. Mumper RJ, et al. 1998. Protective interactive noncondensing (PINC) polymers for enhanced plasmid distribution and expression in rat skeletal muscle. J. Control Release. 52:191–203 [DOI] [PubMed] [Google Scholar]
- 45. Mwau M, et al. 2004. A human immunodeficiency virus 1 (HIV-1) clade A vaccine in clinical trials: stimulation of HIV-specific T-cell responses by DNA and recombinant modified vaccinia virus Ankara (MVA) vaccines in humans. J. Gen. Virol. 85:911–919 [DOI] [PubMed] [Google Scholar]
- 46. Norbury CC, et al. 2004. CD8+ T cell cross-priming via a transfer of proteasome substrates. Science 304:1318–1321 [DOI] [PubMed] [Google Scholar]
- 47. Perfetto SP, et al. 2006. Amine reactive dyes: an effective tool to discriminate live and dead cells in polychromatic flow cytometry. J. Immunol. Methods 313:199–208 [DOI] [PubMed] [Google Scholar]
- 48. Peters BS, et al. 2007. Studies of a prophylactic HIV-1 vaccine candidate based on modified vaccinia virus Ankara (MVA) with and without DNA priming: effects of dosage and route on safety and immunogenicity. Vaccine 25:2120–2127 [DOI] [PubMed] [Google Scholar]
- 49. Pilgrim JL, Gerostamoulos D, Drummer OH, Bollmann M. 2009. Involvement of amphetamines in sudden and unexpected death. J. Forensic Sci. 54:478–485 [DOI] [PubMed] [Google Scholar]
- 50. Pinney SP, Mancini DM. 2004. Myocarditis and specific cardiomyopathies: endocrine disease and alcohol, p 1949–1974 In Fuster V, Alexander RW, O'Rourke RW. (ed), Hurst's the heart, 11th ed. McGraw-Hill Book Co, New York, NY [Google Scholar]
- 51. Radcliffe JN, Roddick JS, Friedmann PS, Stevenson FK, Thridborough SM. 2006. Prime-boost with alternating DNA vaccines designed to engage different antigen presentation pathways generates high frequencies of peptide-specific CD8+ T cells. J. Immunol. 177:6626–6633 [DOI] [PubMed] [Google Scholar]
- 52. Robinson HL, et al. 1999. Neutralizing antibody-independent containment of immunodeficiency virus challenges by DNA priming and recombinant pox virus booster immunizations. Nat. Med. 5:526–534 [DOI] [PubMed] [Google Scholar]
- 53. Sandström E, et al. 2008. Broad immunogenicity of a multigene, multiclade HIV-1 DNA vaccine boosted with heterologous HIV-1 recombinant modified vaccinia virus Ankara. J. Infect. Dis. 198:1482–1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Shedlock DJ, Weiner DB. 2000. DNA vaccination: antigen presentation and the induction of immunity. J. Leukoc. Biol. 68:793–806 [PubMed] [Google Scholar]
- 55. Shen L, Rock KL. 2004. Cellular protein is the source of cross-priming antigen in vivo. Proc. Natl. Acad. Sci. U. S. A. 101:3035–3040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Shen X, Wong SBJ, Buck CB, Zhang J, Siliciano RF. 2002. Direct priming and cross-priming contribute differentially to the induction of CD8+ CTL following exposure to vaccinia virus via different routes. J. Immunol. 169:4222–4229 [DOI] [PubMed] [Google Scholar]
- 57. Shirota H, Petrenko L, Hong C, Klinman DM. 2007. Potential of transfected muscle cells to contribute to DNA vaccine immunogenicity. J. Immunol. 179:329–336 [DOI] [PubMed] [Google Scholar]
- 58. Shulman N, et al. 2008. Development of an automated analysis system for data from flow cytometric intracellular cytokine staining assays from clinical vaccine trials. Cytometry A 73:847–856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Smith WP, et al. 2006. Toward understanding MHC disease associations: partial resequencing of 46 distinct HLA haplotypes. Genomics 87:561–571 [DOI] [PubMed] [Google Scholar]
- 60. Subbramanian RA, et al. 2003. Magnitude and diversity of cytotoxic-T-lymphocyte responses elicited by multiepitope DNA vaccination in rhesus monkeys. J. Virol. 77:10113–10118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Sutter G, Moss B. 1992. Nonreplicating vaccinia vector efficiently expresses recombinant genes. Proc. Natl. Acad. Sci. U. S. A. 89:10847–10851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Sutter G, Wyatt LS, Foley PL, Bennink JR, Moss B. 1994. A recombinant vector derived from the host range-restricted and highly attenuated MVA strain of vaccinia virus stimulates protective immunity in mice to influenza virus. Vaccine 12:1032–1040 [DOI] [PubMed] [Google Scholar]
- 63. Tobery TW, Silicano RF. 1997. Targeting of HIV-1 antigens for rapid intracellular degradation enhances cytotoxic T lymphocyte (CTL) recognition and the induction of de novo CTL responses in vivo after immunization. J. Exp. Med. 185:909–920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Truckenmiller ME, Norbury C. 2004. Viral vectors for inducing CD8+ T cell responses. Expert Opin. Biol. Ther. 4:861–868 [DOI] [PubMed] [Google Scholar]
- 65. Vollmar J, et al. 2006. Safety and immunogenicity of Imvamune, a promising candidate as a third generation smallpox vaccine. Vaccine 24:2065–2070 [DOI] [PubMed] [Google Scholar]
- 66. Von Krempelhuber A, et al. 2010. A randomized, double-blind, dose-finding phase II study to evaluate immunogenicity and safety of the third generation smallpox vaccine candidate IMVAMUNE®. Vaccine 28:1209–1216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Vuola JM, et al. 2005. Differential immunogenicity of various heterologous prime-boost vaccine regimens using DNA and viral vectors in healthy volunteers. J. Immunol. 174:449–455 [DOI] [PubMed] [Google Scholar]
- 68. Walker LE, et al. 2009. Design and preclinical development of a recombinant protein and DNA plasmid mixed format vaccine to deliver HIV-derived T-lymphocyte epitopes. Vaccine 27:7087–7095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Westfall PH, Young SS. 1993. Resampling-based multiple testing: examples and methods for P-value adjustment. John Wiley & Sons, Inc, New York, NY [Google Scholar]
- 70. Wilson CC, et al. 2003. Development of a DNA vaccine designed to induce cytotoxic T lymphocyte responses to multiple conserved epitopes in HIV-1. J. Immunol. 171:5611–5623 [DOI] [PubMed] [Google Scholar]
- 71. Wolkers MC, Brouwenstijn N, Bakker AH, Toebes M, Schumacher TNM. 2004. Antigen bias in T cell cross-priming. Science 304:1314–1317 [DOI] [PubMed] [Google Scholar]
- 72. Yang ZY, et al. 2003. Overcoming immunity to a viral vaccine by DNA priming before vector boosting. J. Virol. 77:799–803 [DOI] [PMC free article] [PubMed] [Google Scholar]