Abstract
Background
Asthma comorbidity has been correlated with poor asthma control, increased health services use, and decreased quality of life. Managing it improves these outcomes. Little is known about the amount of different types of comorbidity associated with asthma and how they vary by age.
Methodology/Principal Findings
The authors conducted a population study using health administrative data on all individuals living in Ontario, Canada (population 12 million). Types of asthma comorbidity were quantified by comparing physician health care claims between individuals with and without asthma in each of 14 major disease categories; results were adjusted for demographic factors and other comorbidity and stratified by age. Compared to those without asthma, individuals with asthma had higher rates of comorbidity in most major disease categories. Most notably, they had about fifty percent or more physician health care claims for respiratory disease (other than asthma) in all age groups; psychiatric disorders in individuals age four and under and age 18 to 44; perinatal disorders in individuals 17 years and under, and metabolic and immunity, and hematologic disorders in children four years and under.
Conclusion/Significance
Asthma appears to be associated with significant rates of various types of comorbidity that vary according to age. These results can be used to develop strategies to recognize and address asthma comorbidity to improve the overall health of individuals with asthma.
Introduction
Asthma has been associated with various types of comorbidity, from coronary artery to psychiatric disease, that place significant burden on patients [1]–[3]. Asthma comorbidity has been correlated with poor asthma control, increased health care use, and decreased quality of life, and managing it has been shown to significantly improve these outcomes [4]–[9]. Despite this, there is still little known and relatively little attention paid to diagnosing and treating asthma comorbidity [10]. This is in contrast to other chronic disease comorbidity–such as renal disease among individuals with diabetes and hypercholesterolemia among individuals with coronary artery disease–that have been well studied and are routinely identified and treated accordingly.
Knowledge of the full spectrum of diseases that accompany asthma, the diseases that have the greatest impact and, as asthma can last a lifetime, how they vary by age would help physicians, other health care providers, and policy makers develop strategies to recognize, prioritize, and manage asthma comorbidity effectively. To the best of our knowledge, no previous studies have systematically investigated and measured the impact of different types of comorbidity on individuals with asthma in different life stages. Therefore, we conducted the current study to characterize and quantify different types of asthma comorbidity in individuals of different ages.
Methods
Ethics Statement
The study was approved by the institutional review boards at Sunnybrook Health Sciences Centre and The Hospital for Sick Children, Toronto, Ontario. For the purposes of this research informed consent was not required. The Institute for Clinical Evaluative Sciences (ICES) is named as a prescribed entity in Section 45 of the Personal Health Information Protection Act (PHIPA – Regulation 329/04, Section 18). Under this designation, ICES can receive and use health information without consent for purposes of analysis and compiling statistical information about the Ontario health care system.
Study Design and Setting
We conducted a retrospective population study using universal, health administrative data from Ontario, Canada–the largest province of Canada with a multicultural population of approximately 12 million [11].
Data Sources
Residents of Ontario have universal public health insurance under the Ontario Health Insurance Plan, the single payer for all medically necessary services across the full spectrum of residents, providers and hospitals. Service details are captured in health administrative databases which can be linked on an individual level to provide a complete health services profile for each resident. Three Ontario population-based health administrative databases were used to identify individuals with asthma and measure their comorbidity through their health services use. The Ontario Health Insurance Plan physician services claims database contains information about all services provided by fee-for-service physicians and “shadow-billings” for physicians paid under alternate payment plans. Each physician claim is accompanied by one International Classification of Disease 9th Revision (ICD-9) diagnostic code. The Canadian Institute for Health Information Discharge Abstract Database contains information on all hospitalizations in the province. Finally, the Ontario Registered Persons Database maintains demographic information on all individuals living in Ontario.
Study Population
All individuals living in Ontario on April 1, 2003 (the index date) were followed until March 31, 2008. Those who died or left the province were excluded. Individuals with asthma were identified using a previously validated asthma case definition based on health administrative data [12]. The case-definition of two or more asthma physician visits within two consecutive years and/or one or more asthma hospitalization yielded 89% sensitivity and 72% specificity in children (aged less than17 years) and 84% sensitivity and 76% specificity in adults (aged 18 years or over) when compared to clinical evaluation. More details of the asthma case definition and examples of its use in other studies can be found elsewhere [12]–[14]. Subjects were stratified by age into the following groups: less than four years (preschool), five to 17 years (children and adolescence), 18 to 44 years (younger adults), 45 to 64 years (middle aged adults) and 65 years and older (older adults).
Outcome Variables
The primary outcome was amount of comorbidity in individuals with asthma which was compared to amount of comorbidity in those without asthma. As a direct correlation between amount of comorbidity and health service claims has been previously well validated, amount of comorbidity was examined through physician claims [15], [16]. Physician claims capture health service use in the ambulatory, emergency department and hospitalization setting. Comorbidity was stratified by diagnosis according to 14 ICD-9 disease categories [17]. ICD-9 categories that were vague and/or heterogeneous (such as symptoms, signs and ill-defined conditions and supplementary classification) were not examined. In secondary analysis, a number of specific conditions previously shown to be associated with asthma were also examined [1]. Details of the 14 ICD-9 disease categories and specific conditions, their associated ICD-9 codes, and the populations in which they were studied are presented in Supplemental Table S1.
Potential Confounding Variables
A number of demographic and clinical variables obtained from the health administrative data were adjusted for in multivariable analysis (Table 1). Socioeconomic status was inferred from neighborhood income derived from postal codes and census data [7], [18]. Rural status was based on Statistics Canada's definition of rurality [19]. Because it could potentially be misclassified as asthma, a co-diagnosis of chronic obstructive pulmonary disease (COPD) was also derived from health administrative data and controlled for [20]. Adjustment for other comorbidity as indicated by ICD-9 category was also done.
Table 1. Characteristics of individuals with and without asthma living in Ontario, Canada.
| Characteristic | Individuals with asthma | Individuals without asthma | P-value for equivalence* |
| N | 1,477,575 | 10,143,134 | |
| Age, years (mean (standard deviation)) | 31.8 (22.8) | 38.2 (21.6) | 1.000 |
| Female (%) | 53.2 | 50.6 | 0.985 |
| Socioeconomic Status | |||
| - Quintile 1 (Lowest) | 19.7 | 18.9 | <0.001 |
| - Quintile 2 | 19.9 | 19.7 | |
| - Quintile 3 | 20.2 | 20.1 | |
| - Quintile 4 | 20.4 | 20.5 | |
| - Quintile 5 (Highest) | 19.5 | 20.4 | |
| Rural (versus urban) residence (%) | 11.8 | 13.2 | <0.001 |
| COPD (%) | 16.0 | 4.7 | 1.000 |
COPD, Chronic Obstructive Pulmonary Disease.
Equivalence tests performed. Significant P-values indicate that distributions are ‘practically equivalent’ to within +/− two percentage points for proportions and 0.75 years for age.
Statistical Analyses
Frequencies and proportions were used to report socio-demographic characteristics. Normal approximation (z) tests for equivalence were conducted to determine if groups were statistically equivalent, using a difference margin of two percent absolute difference (i.e. significant p-values (p<0.05) indicated that the true difference in proportions was less than +/− 2%). For each ICD-9 disease category and condition studied absolute counts of physician claims and crude physician claim rates (per 1000 person years) were calculated for individuals with and without asthma. Absolute differences and their gamma-based 95% confidence intervals were also calculated. Adjusted relative risks of comorbidity in individuals with compared to those without asthma (and their 95% confidence intervals) were calculated using multivariable Poisson regression adjusting for age, sex, socioeconomic status, rural/urban place of residence, a co-diagnosis of COPD, and other comorbidity as indicated by ICD-9 categories. An adjusted relative risk more than or equal to one indicated that physician claims for a comorbidity were more common in individuals with compared to those without asthma and a relative risk less than one indicated the opposite. All analyses were stratified by age group and conducted with SAS version 9.2 for UNIX systems (Cary, North Carolina).
Sensitivity Analysis
To assess whether it was plausible that misclassification of asthma due to less than perfect specificity of the case definition was responsible for the observed results, an array approach was used [21]. The inclusion of misclassified people could have potentially led to incorrect results if the misclassified people were healthier (or less healthy) than those correctly identified. Therefore, to determine if this influenced the results, we estimated the true relative risks when different assumptions about the health of those who were misclassified relative to those who truly had asthma were made. We were specifically Interested in what assumptions caused the relative risks to be reduced to 1.0 (or no increased risk).
Results
Study Population
There were 11,903,512 individuals living in Ontario in 2003 who were followed for five years. After excluding 282,803 who met at least one exclusion criterion (i.e. developed asthma, left the province, or died in the follow-up period) a study population of 1,477,575 (12.7%) individuals with and 10,143,134 (86.3%) individuals without asthma remained.
On average, individuals with asthma were younger (32 years compared to 38 years), more likely to be female, and more likely to have a co-diagnosis of COPD than those without asthma (Table 1). However, when examined by age group, compared to those without asthma, younger individuals (ages zero to four and five to 17 years) with asthma were more likely to be male and live in an urban region; individuals in the three older age groups (18 to 44, 45 to 64 and 65 years and older) with asthma were more likely to be female and have a co-diagnosis of COPD; and individuals in the two oldest age groups with asthma were more likely to live in a lower income neighborhood (data not shown).
Comorbidity in 14 Disease Categories
Compared to those without asthma, individuals with asthma had higher rates of comorbidity, as indicated by physician claims, in all 14 ICD-9 disease categories (Tables 2 and 3).
Table 2. Rates of health services claims among individuals with and without asthma in 14 disease categories, according to age (Pediatric population).
| Health Services Claims per 1000 person years | |||||||
| 4 years and younger | 5 to 17 years | ||||||
| Individuals with asthma | Individuals without asthma | Absolute rate difference | Individuals with asthma | Individuals without asthma | Absolute rate difference | ||
| Disease Category | (N = 90,387) | (N = 536,432) | (95% confidence interval) | (N = 464,068) | (N = 1,555,638) | (95% confidence interval) | |
| Infectious and parasitic disease | 423.0 | 330.6 | 92.4 (90.6, 94.2) | 256.4 | 208.7 | 47.7 (47.1, 48.4) | |
| Neoplasms | 38.3 | 33.7 | 4.7 (4.1, 5.2) | 43.5 | 39.5 | 4.1 (3.8, 4.3) | |
| Endocrine, nutritional, and metabolic diseases, and immunity disorders | 47.4 | 30.8 | 16.6 (16.0, 17.2) | 76.9 | 56.7 | 20.2 (19.8, 20.6) | |
| Hematologic disorders | 32.0 | 22.7 | 9.3 (8.8, 9.8) | 25.6 | 21.8 | 3.8 (3.6, 4.0) | |
| Psychiatric disorders | 222.1 | 133.5 | 88.6 (87.3, 89.9) | 431.5 | 316.3 | 115.2 (114.3, 116.0) | |
| Nervous system and sense organs | 744.0 | 593.8 | 150.2 (147.7, 152.6) | 333.8 | 254.9 | 78.9 (78.1, 79.6) | |
| Circulatory system | 46.4 | 29.9 | 16.6 (15.9, 17.2) | 71.0 | 54.9 | 16.2 (15.8, 16.5) | |
| Digestive system | 228.2 | 172.2 | 56.0 (54.6, 57.3) | 207.9 | 160.4 | 47.5 (46.9, 48.0) | |
| Genitourinary system | 116.9 | 101.1 | 15.8 (14.8, 16.8) | 161.4 | 152.3 | 9.1 (8.5, 9.6) | |
| Skin and subcutaneous tissue | 337.1 | 260.9 | 76.2 (74.6, 77.9) | 371.1 | 300.3 | 70.8 (70.0, 71.6) | |
| Musculoskeletal system and connective tissue | 74.6 | 54.3 | 20.3 (19.6, 21.1) | 178.9 | 138.4 | 40.4 (39.9, 41.0) | |
| Congenital anomalies | 29.7 | 20.3 | 9.5 (9.0, 9.9) | 16.2 | 10.9 | 5.3 (5.1, 5.5) | |
| Conditions originating in the perinatal period | 7.9 | 3.0 | 4.9 (4.7, 5.2) | 2.3 | 1.1 | 1.2 (1.1, 1.2) | |
| Injury and poisoning | 309.8 | 236.0 | 73.8 (72.3, 75.4) | 444.1 | 344.3 | 99.8 (98.9, 100.7) | |
| Respiratory system other than asthma | 1571.7 | 1058.1 | 513.6 (510.1, 517.1) | 817.6 | 520.5 | 297.1 (296.0, 298.3) | |
Table 3. Rates of health services claims among individuals with and without asthma in 14 disease categories, according to age (Adult population).
| Health Services Claims per 1000 person years | |||||||||
| 18 to 44 years | 45 to 64 years | 65 years and older | |||||||
| Individuals with asthma | Individuals without asthma | Absolute rate difference | Individuals with asthma | Individuals without asthma | Absolute rate difference | Individuals with asthma | Individuals without asthma | Absolute rate difference | |
| Disease Category | (N = 492,044) | (N = 4,154,792) | (95% confidence interval) | (N = 264,150) | (N = 2,583,341) | (95% confidence interval) | (N = 166,926) | (N = 1,312,931) | (95% confidence interval) |
| Infectious and parasitic disease | 239.1 | 171.9 | 67.3 (66.7, 67.8) | 220.2 | 137.3 | 82.9 (82.2, 83.7) | 290.7 | 199.1 | 91.7 (90.5, 92.8) |
| Neoplasms | 148.1 | 128.0 | 20.1 (19.7, 20.6) | 535.4 | 458.5 | 76.9 (75.7, 78.1) | 1111.6 | 1027.5 | 84.0 (81.7, 86.4) |
| Endocrine, nutritional, and metabolic diseases, and immunity disorders | 329.0 | 243.2 | 85.9 (85.2, 86.6) | 930.0 | 667.7 | 262.3 (260.7, 263.8) | 1093.0 | 966.1 | 126.9 (124.6, 129.2) |
| Hematologic disorders | 57.2 | 42.5 | 14.7 (14.4, 15.0) | 114.2 | 72.0 | 42.2 (41.7, 42.8) | 317.8 | 246.2 | 71.6 (70.3, 72.8) |
| Psychiatric disorders | 1273.2 | 723.2 | 550.0 (548.7, 551.3) | 1428.7 | 783.1 | 645.6 (643.6, 647.5) | 1408.0 | 1257.0 | 150.9 (148.3, 153.6) |
| Nervous system and sense organs | 443.4 | 300.7 | 142.7 (141.9, 143.5) | 820.1 | 564.2 | 255.8 (254.4, 257.3) | 1684.8 | 1426.1 | 258.7 (255.8, 261.6) |
| Circulatory system | 382.9 | 281.5 | 101.4 (100.7, 102.2) | 1661.3 | 1199.3 | 462.0 (459.9, 464.1) | 4342.6 | 3573.0 | 769.6 (765.0, 774.3) |
| Digestive system | 509.7 | 324.9 | 184.8 (183.9, 185.7) | 829.5 | 529.6 | 299.9 (298.4, 301.3) | 1236.9 | 882.3 | 354.6 (352.1, 357.1) |
| Genitourinary system | 627.5 | 458.7 | 168.8 (167.8, 169.7) | 734.6 | 509.4 | 225.3 (223.9, 226.7) | 1099.8 | 885.1 | 214.7 (212.4, 217.0) |
| Pregnancy, childbirth and the puerperium | 310.2 | 241.6 | 68.6 (68.0, 69.3) | 2.1 | 1.4 | 0.7 (0.6, 0.7) | na | na | na |
| Skin and subcutaneous tissue | 365.3 | 270.8 | 94.5 (93.7, 95.2) | 443.8 | 302.0 | 141.8 (140.7, 142.8) | 598.4 | 479.3 | 119.1 (117.3, 120.8) |
| Musculoskeletal system and connective tissue | 618.4 | 398.1 | 220.3 (219.3, 221.2) | 1383.6 | 807.8 | 575.8 (573.9, 577.7) | 1732.3 | 1267.2 | 465.1 (462.2, 468.0) |
| Injury and poisoning | 510.5 | 342.1 | 168.3 (167.5, 169.2) | 653.6 | 413.2 | 240.4 (239.1, 241.7) | 945.9 | 720.2 | 225.7 (223.6, 227.9) |
| Respiratory system other than asthma | 979.4 | 497.6 | 481.8 (480.6, 483.0) | 1588.9 | 536.6 | 1052.3 (1050.3, 1054.3) | 2853.5 | 926.9 | 1926.7 (1923.0, 1930.3) |
na, not applicable.
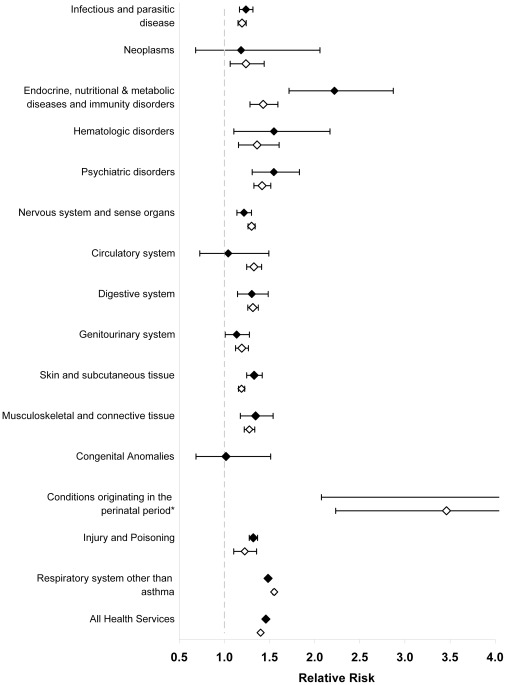
After adjusting for potential confounders, comorbidity in children four years and younger was 46% higher in those with compared to those without asthma (p<0.001; Figure 1). Higher comorbidity was found for most of the 14 disease categories but was highest (50% or greater) for respiratory disease (other than asthma); psychiatric disorders; metabolic and immunity disorders; hematologic disorders; and perinatal disorders (p<0.001 for each disease category).
Figure 1. Adjusted relative risks and 95% confidence intervals of comorbidity, as indicated by health services use, among individuals four years and younger and five to 17 years with compared to without asthma in 14 disease categories.
Solid diamonds represent relative risks for individuals four years and younger; hollow diamonds represent relative risks for individuals five to 17 years. All analyses were adjusted for age, sex, socioeconomic status, rural/urban place of residence, a co-diagnosis of COPD, and other comorbidity as indicated by ICD-9 category. * Relative risk for conditions originating in the perinatal period among individuals zero to four years old: 5.03, 95% CI: 2.08 to 12.21 and among individuals five to 17 years old: 3.46 (2.23 to 5.36).
Similarly, comorbidity was 40% higher among children aged five to 17 years with compared to without asthma (p<0.001; Figure 1). Significantly higher physician claim rates were found in all 14 disease categories (p<0.05) but were highest (more than 50% higher) for respiratory disease other than asthma and perinatal disorders.
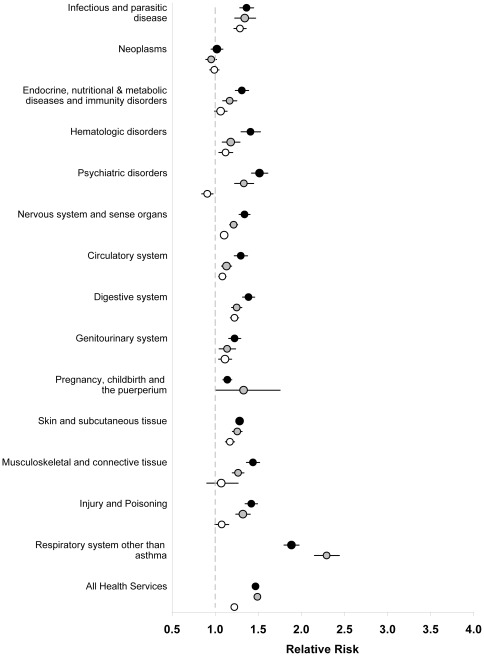
Among those aged 18 to 44 and 45 to 64 years of age, comorbidity was 47% and 49% higher among those with compared to those without asthma (p<0.001; Figure 2). Among those aged 18 to 44 and 45 to 64 years, physician claims were significantly elevated for all disease categories (p<0.001) except for neoplasms (RR 1.02 [95% CI 0.95 to 1.09] and 0.95 [95% CI: 0.89 to 1.02] respectively, Figure 2). Risk of respiratory disease (other than asthma) was about double, and risk of psychiatric disorders and infectious diseases was approximately 33% to 51% higher in individuals with asthma (p<0.001 for each disease category).
Figure 2. Adjusted relative risks and 95% confidence intervals of comorbidity, as indicated by health services use, among individuals age 18 to 44 years, 45 to 64 years and 65 years and older with compared to without asthma in 14 disease categories.
Solid black circles represent relative risks for individuals 18 to 44 years; solid grey circles represent relative risks for individuals 45 to 64 years; hollow circles represent relative risks for individuals age 65 years and older. All analyses were adjusted for age, sex, socioeconomic status, rural/urban place of residence, a co-diagnosis of COPD, and other comorbidity as indicated by ICD-9 category.
Finally, comorbidity was 22% higher among individuals aged 65 years and older with compared to those without asthma (p<0.001; Figure 2). Although significantly greater health services use was seen in most disease categories, relative risks in this age group were generally lower compared to other age groups. Physician claim rates for respiratory disease (other than asthma) were still higher (RR: 2.08, 95% CI [1.99 to 2.17]) in individuals with asthma, but there was no increase rates for neoplasms, metabolic and immunity disorders, and musculoskeletal disorders and rates for psychiatric disorders was slightly lower (RR: 0.91, 95% CI [0.84 to 0.98]; Figure 2).
Comorbidity for conditions associated with asthma
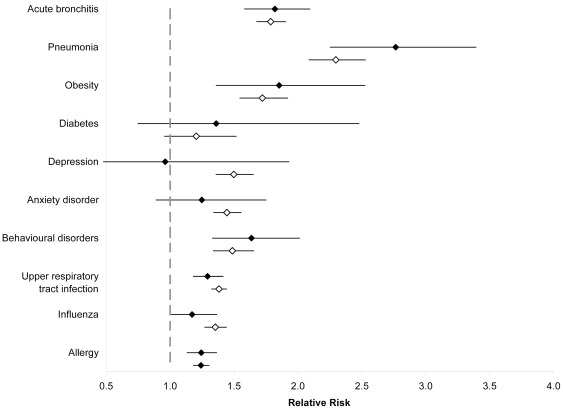
Comorbidity, as indicated by physician claims, for several specific conditions previously shown to be associated with asthma was also examined (Tables 4 and 5). Among children four years and younger, physician claim rates for most conditions were significantly higher among those with compared to those without asthma (Figure 3). More than 50% higher claim rates (in some cases more than double) were seen for acute bronchitis, pneumonia, obesity, and behavioral disorders (p<0.001 for each disease condition). Among children aged five to 17 years, physician claim rates for almost all conditions studied was significantly higher among those with compared to those without asthma (Figure 3). More than 50% higher claim rates were seen for acute bronchitis, pneumonia, obesity, and depression (p<0.001 for each disease condition).
Table 4. Rates of health services claims among individuals with and without asthma for specific disease conditions, according to age (Pediatric population).
| Health Services Claims per 1000 person years | ||||||
| 4 years and younger | 5 to 17 years of age | |||||
| Individuals with asthma | Individuals without asthma | Absolute rate difference | Individuals with asthma | Individuals without asthma | Absolute rate difference | |
| Specific Condition | (95% confidence interval) | (95% confidence interval) | ||||
| Pneumonia | 77.4 | 32.1 | 45.3 (44.5, 46.0) | 22.9 | 10.6 | 12.3 (12.1, 12.5) |
| Influenza | 32.6 | 24.5 | 8.1 (7.6, 8.6) | 20.9 | 15.0 | 5.9 (5.8, 6.1) |
| Upper Respiratory Tract Infection | 787.9 | 609.1 | 178.8 (176.3, 181.3) | 362.5 | 259.3 | 103.2 (102.4, 104.0) |
| Depression | 1.7 | 1.0 | 0.6 (0.5, 0.7) | 30.1 | 21.9 | 8.2 (8.0, 8.4) |
| Anxiety disorder | 40.9 | 26.9 | 13.9 (13.4, 14.5) | 178.8 | 136.1 | 42.7 (42.2, 43.3) |
| Behavioural disorders | 77.0 | 43.4 | 33.6 (32.8, 34.3) | 65.0 | 38.9 | 26.1 (25.7, 26.4) |
| Obesity | 11.7 | 6.2 | 5.5 (5.2, 5.8) | 20.1 | 12.7 | 7.4 (7.2, 7.6) |
| Allergy | 183.1 | 144.1 | 39.0 (37.8, 40.2) | 120.4 | 91.1 | 29.3 (28.8, 29.7) |
| Acute bronchitis | 179.9 | 101.5 | 78.4 (77.3, 79.6) | 92.4 | 49.6 | 42.8 (42.4, 43.1) |
| Diabetes | 7.3 | 5.6 | 1.7 (1.5, 2.0) | 18.1 | 14.8 | 3.3 (3.1, 3.5) |
Table 5. Rates of health services claims among individuals with and without asthma for specific disease conditions, according to age (Adult population).
| Health Services Claims per 1000 person years | |||||||||
| 18 to 44 years | 45 to 64 years | 65 years and older | |||||||
| Individuals with asthma | Individuals without asthma | Absolute rate difference | Individuals with asthma | Individuals without asthma | Absolute rate difference | Individuals with asthma | Individuals without asthma | Absolute rate difference | |
| Specific Condition | (95% confidence interval) | (95% confidence interval) | (95% confidence interval) | ||||||
| Angina | 9.5 | 6.6 | 3.0 (2.9, 3.1) | 91.8 | 64.2 | 27.5 (27.0, 28.0) | 273.6 | 211.2 | 62.4 (61.3, 63.6) |
| Cataracts | 4.6 | 3.7 | 0.9 (0.8, 1.0) | 96.2 | 66.6 | 29.6 (29.1, 30.1) | 449.1 | 394.7 | 54.4 (52.9, 55.9) |
| Osteroporosis | 4.6 | 3.2 | 1.4 (1.3, 1.4) | 44.6 | 36.6 | 8.0 (7.7, 8.4) | 93.0 | 83.0 | 10.0 (9.3, 10.7) |
| Glaucoma | 8.4 | 7.4 | 1.1 (1.0, 1.2) | 70.8 | 54.5 | 16.3 (15.9, 16.8) | 204.4 | 179.4 | 25.0 (24.0, 26.0) |
| Myocardial infarction | 15.5 | 13.1 | 2.5 (2.3, 2.6) | 154.3 | 119.9 | 34.4 (33.8, 35.1) | 549.9 | 456.2 | 93.7 (92.0, 95.3) |
| Pneumonia | 36.2 | 14.7 | 21.5 (21.3, 21.7) | 107.1 | 34.6 | 72.6 (72.0, 73.1) | 435.2 | 182.4 | 252.8 (251.3, 254.2) |
| Influenza | 21.4 | 14.7 | 6.8 (6.6, 6.9) | 36.5 | 23.6 | 12.9 (12.6, 13.2) | 54.9 | 47.9 | 7.0 (6.5, 7.5) |
| Upper Respiratory Tract Infection | 303.3 | 196.8 | 106.5 (105.8, 107.1) | 274.5 | 146.7 | 127.8 (127.0, 128.7) | 254.4 | 148.0 | 106.4 (105.3, 107.5) |
| Depression | 131.1 | 68.4 | 62.7 (62.2, 63.1) | 154.5 | 79.4 | 75.1 (74.4, 75.7) | 94.3 | 66.9 | 27.5 (26.8, 28.1) |
| Anxiety disorder | 678.7 | 392.7 | 286.0 (285.0, 287.0) | 819.0 | 446.3 | 372.7 (371.2, 374.2) | 491.7 | 347.9 | 143.8 (142.2, 145.4) |
| Lung Cancer | 59.5 | 34.2 | 25.3 (25.0, 25.6) | 73.8 | 36.6 | 37.2 (36.8, 37.7) | 21.2 | 13.5 | 7.7 (7.4, 8.0) |
| Obesity | 3.1 | 2.3 | 0.8 (0.8, 0.9) | 54.1 | 33.6 | 20.6 (20.2, 20.9) | 147.8 | 91.7 | 56.1 (55.2, 56.9) |
| Allergy | 112.6 | 81.8 | 30.7 (30.3, 31.1) | 126.0 | 84.3 | 41.8 (41.2, 42.3) | 156.6 | 119.3 | 37.4 (36.5, 38.3) |
| Acute bronchitis | 3.1 | 2.3 | 0.8 (0.8, 0.9) | 54.1 | 33.6 | 20.6 (20.2, 20.9) | 147.8 | 91.7 | 56.1 (55.2, 56.9) |
| Diabetes | 112.6 | 81.8 | 30.7 (30.3, 31.1) | 126.0 | 84.3 | 41.8 (41.2, 42.3) | 156.6 | 119.3 | 37.4 (36.5, 38.3) |
Figure 3. Adjusted relative risks and 95% confidence intervals of comorbidity, as indicated by health services use, use among individuals 4 years and younger and 5 to 17 years with compared to without asthma for specific disease conditions.
Solid diamonds represent relative risks for individuals four years and younger; hollow diamonds represent relative risks for individuals five to 17 years. All analyses were adjusted for age, sex, socioeconomic status, rural/urban place of residence, a co-diagnosis of COPD, and other comorbidity as indicated by ICD-9 category.
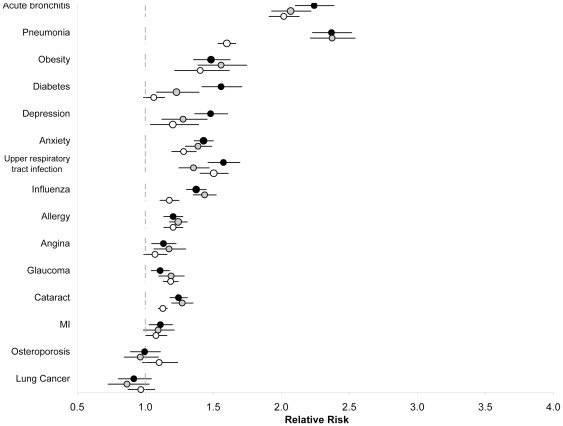
Significantly higher physician claim rates for most conditions were found among individuals aged 18 to 44 and 45 to 64 years with asthma compared to those without (p<0.05 for all conditions except lung cancer, osteoporosis and acute myocardial infarction in 45 to 64 year olds; Figure 4). Of particular note were acute bronchitis and pneumonia, which were at least twice as common in those with asthma (p<0.001). Finally, with few exceptions, comorbidity was similar in the 65 years and older age group (Figure 4) where physician claims were twice as common for acute bronchitis and 60% higher for pneumonia.
Figure 4. Adjusted relative risks and 95% confidence intervals of comorbidity, as indicated by health services use, among individuals age 18 to 44 years, 45 to 64 years and 65 years and older with compared to without asthma for specific disease conditions.
Solid black circles represent relative risks for individuals 18 to 44 years; solid grey circles represent relative risks for individuals 45 to 64 years; hollow circles represent relative risks for individuals 65 years and older. All analyses were adjusted for age, sex, socioeconomic status, rural/urban place of residence, a co-diagnosis of COPD, and other comorbidity as indicated by ICD-9 category.
Sensitivity Analysis
In the unlikely scenario that individuals who were potentially misclassified as having asthma had twice the comorbidity as those with true asthma, misclassification could have accounted for the results seen. In the more likely scenario that individuals who were potentially misclassified with asthma had less comorbidity than those with true asthma (ie. they were overdiagnosed with asthma), the relative risk of comorbidity would be much greater than that observed [22].
Discussion
We conducted a retrospective study using universal health administrative data to describe and quantify asthma comorbidity in a large, complete, real world population and found asthma to be associated with significant rates of various types of comorbidity in individuals of different age. Specifically, compared to people without asthma, individuals with asthma had at least 50% or more comorbidity, as indicated by health services use, for respiratory disease (other than asthma) in all age groups; psychiatric disorders in individuals age four and under and age 18 to 44; perinatal disorders in individuals 17 years and under, and metabolic and immunity, and hematologic disorders in children four years and under. While most of these types of asthma comorbidity have been described before,[1], [23]–[26] their differential impact on individuals of different ages adjusting for a number of confounders like socioeconomic status and other comorbidity has, to the best of our knowledge, never been reported. These findings may be used to guide the development of strategies to recognize and manage asthma comorbidity throughout the lifespan to improve asthma care.
Comorbidity may occur in patients with asthma for several reasons and our study was not designed to determine causality. First, asthma itself may cause or contribute to comorbidity. For example, asthma control is often suboptimal and the consequent physical activity limitations and disturbed sleep could contribute to psychiatric disorders and obesity [7], [27], [28]. Second, therapies for asthma may also cause or contribute to comorbidity. For example, inhaled corticosteroids may predispose to pneumonia [29]. Third, some comorbidity such as allergy may be linked to asthma via common genetic and environmental factors as part of a larger diathesis. Fourth, some comorbidity may increase the risk, severity, or likelihood of asthma. This has been well-documented for allergic rhinitis and, more controversially, may also be true for obesity [30], [31]. Finally, it might be possible that some of the comorbidity we observed in individuals with asthma was due to diagnostic confusion or lack of precision.
Most of the disease associations with asthma in the current study have been previously described; however, there were also some, such as metabolic and immunity disorders and hematologic disorders in children 4 years and younger, that we do not believe have been associated with asthma before. This is most likely because they have not been examined before and not because they do not exist. On further examination, differences in the former group appeared to be driven by obesity and diabetes (Table 6) and in the later by iron deficiency anemia (Table 7). Their further investigation would be of interest. There were also a few findings, such as the lack of association with osteoporosis, that appeared to contradict previous studies [1]. This could have been due to differences in measurement of the condition between our study and previous ones and/or differences in analysis–specifically in potential confounding variables adjusted for. In our study we adjusted for many variables including socioeconomic status and other comorbidity which were not adjusted for in previous studies.
Table 6. Rates of the 10 most common conditions in the Endocrine, nutritional, and metabolic diseases, and immunity disorders disease category in individuals with asthma age four years and younger and the corresponding rates in individuals without asthma.
| Health services claims per 1000 person years | ||
| Individuals with asthma | Individuals without asthma | |
| Condition | (95% confidence interval) | (95% confidence interval) |
| Obesity | 8.8 (8.6, 9.1) | 4.6 (4.5, 4.7) |
| Diabetes mellitus | 7.3 (7.1, 7.5) | 5.6 (5.5, 5.6) |
| Other metabolic disorders | 6.2 (6.0, 6.4) | 2.7 (2.6, 2.7) |
| Other endocrine disorders | 4.0 (3.9, 4.2) | 2.5 (2.5, 2.6) |
| Vitamin and other nutritional deficiencies | 3.2 (3.0, 3.3) | 3.0 (3.0, 3.1) |
| Unspecified malnutrition | 2.2 (2.1, 2.4) | 2.0 (2.0, 2.1) |
| Hypogammaglobulinemia, agammaglobulinemia, other immunity disorders | 1.9 (1.8, 2.0) | 1.0 (1.0, 1.1) |
| Disorders of lipid metabolism | 0.9 (0.8, 1.0) | 0.6 (0.5, 0.6) |
| Acquired hypothyroidism | 0.8 (0.8, 0.9) | 0.7 (0.6, 0.7) |
| Congenital hypothyroidism | 0.6 (0.5, 0.7) | 0.4 (0.4, 0.4) |
Table 7. Rates of the 10 most common conditions in the Hematologic disorders disease category in individuals with asthma age 4 years and younger and the corresponding rates in individuals without asthma.
| Health Services Claims per 1000 person years | ||
| Individuals with asthma | Individuals without asthma | |
| Condition | (95% confidence interval) | (95% confidence interval) |
| Iron deficiency anemia | 10.5 (10.3, 10.8) | 8.8 (8.7, 8.9) |
| Other diseases of blood, marrow, spleen | 4.6 (4.4, 4.8) | 3.1 (3.1, 3.2) |
| Hereditary hemolytic anemia | 3.8 (3.7, 4.0) | 1.7 (1.7, 1.7) |
| Purpura, thrombocytopenia, other hemorrhagic conditions | 2.2 (2.1, 2.3) | 1.6 (1.5, 1.6) |
| Neutropenia, agranulocytosis, eosinophilia | 2.2 (2.0, 2.3) | 1.6 (1.6, 1.7) |
| Coagulation defects | 1.9 (1.8, 2.0) | 0.8 (0.7, 0.8) |
| Other anemias | 0.9 (0.8, 1.0) | 0.9 (0.9, 0.9) |
| Aplastic anemia | 0.6 (0.5, 0.7) | 0.5 (0.5, 0.6) |
| Pernicious anemia | 0.3 (0.3, 0.4) | 0.3 (0.3, 0.3) |
| Acquired hemolytic anemia, excluding hemolytic disease of newborn | 0.2 (0.2, 0.2) | 0.1 (0.1, 0.1) |
The strengths of our study were its ability to examine and quantify all physician health services use in a large real-world, population of individuals of various ages with and without asthma. It also has limitations that merit emphasis. To begin, we used a definition of asthma based on health administrative data, which does not contain a measure of lung function so misclassification could have occurred. This is of greatest concern in the four and under age group because they cannot perform pulmonary function testing making diagnosis of asthma can be very difficult. However, misclassification would have caused the asthma and non-asthma groups we studied to be more similar than they actually were, which would have lessened the differences in comorbidity between the groups and attenuated the relative risks of comorbidity we measured. Thus any misclassification would have caused our study to underestimate (not overestimate) the true impact of comorbidity on individuals with asthma. This was confirmed in our sensitivity analysis which showed that only in the extremely unlikely scenario where those misclassified with asthma had twice the amount of comorbidity as those with true asthma, would the increased relative risks of comorbidity associated with asthma be negated. Our definition of asthma was also likely to overlook milder cases and, because it was not dependent on standardized diagnostic criteria, may have varied in terms of who it identified. A second limitation was that increased health services use may occur for many reasons and our study could not distinguish increased use due to asthma comorbidity from increased use due to other causes such as better access to health care or learned behavior. Even though Ontario has universal health care insurance and we controlled for barriers to access like low socioeconomic status, other obstacles to health care access still exist and individuals who have obtained prior health care access because of their asthma might have been more likely to have found a way to overcome these obstacles. Alternatively, using health care may partly be a learned behavior and those who had accessed the health care system for their asthma might have learned to use, and perhaps overuse, health services for other conditions as well. We believe that these factors may have accounted for a small amount of increased health services use across all categories, but not for the notably higher levels seen in some disease categories. Further study investigating the reasons for increased health services use in individuals with asthma would help to determine if they were contributing factors. Finally, a third limitation was that physicians in Ontario can only provide one diagnosis per claim. Therefore, for example, if a patient presented with asthma and allergic rhinitis (which commonly co-exist) only one would be recorded. This might have accounted for a possible underestimate of the relative risk of allergy in people with asthma.
In summary, we conducted a retrospective cohort study of a large, complete, real world population and found that, compared to people without asthma, those with asthma had notably higher rates of many different types of comorbidity which varied according to age. Asthma comorbidity has important implications in terms of the evaluation and management of asthma and should be recognized, investigated and treated appropriately. Future investigation is needed to confirm and study the unique findings of this study in more detail, sort out the complex interactions between asthma and its comorbidity, and develop better approaches to educating about and managing asthma comorbidity in order to improve asthma care and the health of the asthma population overall.
Supporting Information
List of disease categories and conditions, their associated International Classification of Disease, 9th Revision (ICD-9) codes, and the specific populations in which they were studied.
(DOCX)
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: Dr. Gershon was supported by an Ontario Ministry of Health Career Scientist Award when she worked on this study. Dr. To is supported by The Dales Award in Medical Research from the University of Toronto, Toronto, Ontario, Canada. Funding for this project was made available through the Government of Ontario who had no role in study design, collection, analysis, interpretation of data, writing of the report, or in the decision to submit the report for publication. This study was also supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario Ministry of Health and Long-Term Care is intended or should be inferred. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Soriano JB, Visick GT, Muellerova H, Payvandi N, Hansell AL. Patterns of comorbidities in newly diagnosed COPD and asthma in primary care. Chest. . 2005;128(4):2099–2107. doi: 10.1378/chest.128.4.2099. [DOI] [PubMed] [Google Scholar]
- 2.Onufrak SJ, Abramson JL, Austin HD, Holguin F, McClellan WM, et al. Relation of adult-onset asthma to coronary heart disease and stroke. Am J Cardiol. . 2008;101(9):1247–1252. doi: 10.1016/j.amjcard.2007.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chun TH, Weitzen SH, Fritz GK. The asthma/mental health nexus in a population-based sample of the United States. 2008;Chest. 134(6):1176–1182. doi: 10.1378/chest.08-1528. [DOI] [PubMed] [Google Scholar]
- 4.Gershon AS, Wang C, Guan J, To T. Burden of comorbidity in individuals with asthma. Thorax. . 2010;65(7):612–618. doi: 10.1136/thx.2009.131078. [DOI] [PubMed] [Google Scholar]
- 5.Wijnhoven HA, Kriegsman DM, Hesselink AE, de Haan M, Schellevis FG. The influence of co-morbidity on health-related quality of life in asthma and COPD patients. Respir Med. . 2003; 2003;97(5):468–475. doi: 10.1053/rmed.2002.1463. [DOI] [PubMed] [Google Scholar]
- 6.Deshmukh VM, Toelle BG, Usherwood T, et al. The association of comorbid anxiety and depression with asthma-related quality of life and symptom perception in adults. Respirology. 2008;13(5):695–702. doi: 10.1111/j.1440-1843.2008.01310.x. [DOI] [PubMed] [Google Scholar]
- 7.Boulet LP. Influence of comorbid conditions on asthma. Eur Respir J. . 2009;33(4):897–906. doi: 10.1183/09031936.00121308. [DOI] [PubMed] [Google Scholar]
- 8.Lehrer PM, Karavidas MK, Lu SE, Feldman J, Kranitz L. Psychological treatment of comorbid asthma and panic disorder: a pilot study. J Anxiety Disord. 2008;22(4):671–683. doi: 10.1016/j.janxdis.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eneli IU, Skybo T, Camargo CA Weight loss and asthma: a systematic review. Thorax. 2008;63(8):671–676. doi: 10.1136/thx.2007.086470. [DOI] [PubMed] [Google Scholar]
- 10. Global Initiative for Asthma (GINA). Global Strategy for Asthma Management and Prevention. 2009. [Google Scholar]
- 11.Population by selected ethnic origins, by province, territory . www40.statcan.ca/l01/cst01/demo26g-eng.htm. Accessed on January 15, 2012; 2006 Census. (Ontario). [Google Scholar]
- 12.Gershon AS, Wang C, Vasilevska-Ristovska J, Guan J, Cicutto L, et al. Identifying Patients with physician diagnosed asthma in health administrative databases. Can Respir J. 2009;16(6):183–188. doi: 10.1155/2009/963098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gershon AS, Guan J, Wang C, To T. Trends in asthma prevalence and incidence in Ontario, Canada, 1996–2005: a population study. Am J Epidemiol. . 2010;172(6):728–736. doi: 10.1093/aje/kwq189. [DOI] [PubMed] [Google Scholar]
- 14.To T, Wang C, Guan J, McLimont S, Gershon AS. What Is the Lifetime Risk of Physician-diagnosed Asthma in Ontario, Canada? Am J Respir Crit Care Med. . 2010;181(4):337–343. doi: 10.1164/rccm.200907-1035OC. [DOI] [PubMed] [Google Scholar]
- 15.Starfield B, Lemke KW, Bernhardt T, Foldes SS, Forrest CB. Comorbidity: implications for the importance of primary care in ‘case’ management. Ann Fam Med. . 2003;1(1):8–14. doi: 10.1370/afm.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Starfield B, Lemke KW, Herbert R, Pavlovich WD, Anderson G. Comorbidity and the use of primary care and specialist care in the elderly. Ann Fam Med. . 2005;3(3):215–22. doi: 10.1370/afm.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organizatio. Geneva: World Health Organization; 1977. Manual of the international statistical classification of diseases, injuries, and causes of death. [Google Scholar]
- 18.Statistics Canada. Including Postal Codes to December 2003. Ottawa: Statistics Canada; 2004. PCCF+ Version 4D User's Guide (Geocodes/PCCF). Automated Geographic Coding Based on the Statistics Canada Postal Code Conversion Files, [Google Scholar]
- 19.Plessis V, Beshiri R, Bollman R, Clemenson H. Ottawa: Statistics Canada; 2002. Definitions of “Rural”. [Google Scholar]
- 20.Gershon AS, Wang C, Guan J, Vasilevska-Ristovska J, Cicutto L, et al. Identifying individuals with physcian diagnosed COPD in health administrative databases. COPD. 2009;6(5):388–394. doi: 10.1080/15412550903140865. [DOI] [PubMed] [Google Scholar]
- 21.Schneeweiss S. Sensitivity analysis and external adjustment for unmeasured confounders in epidemiologic database studies of therapeutics. Pharmacoepidemiol Drug Saf. . 2006;15(5):291–303. doi: 10.1002/pds.1200. [DOI] [PubMed] [Google Scholar]
- 22.Aaron SD, Vandemheen KL, Boulet LP, McIvor RA, Fitzgerald JM, et al. Overdiagnosis of asthma in obese and nonobese adults. CMAJ. 2008;179(11):1121–1131. doi: 10.1503/cmaj.081332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adams RJ, Wilson DH, Taylor AW, Daly A, Tursan DE, et al. Coexistent chronic conditions and asthma quality of life: a population-based study. 2006;Chest. 129(2):285–291. doi: 10.1378/chest.129.2.285. [DOI] [PubMed] [Google Scholar]
- 24.Ben Noun L. Characteristics of comorbidity in adult asthma. Public Health Review. . 2001;29(1):49–61. [PubMed] [Google Scholar]
- 25.Zhang T, Carleton BC, Prosser RJ, Smith AM. The added burden of comorbidity in patients with asthma. J Asthma. . 2009;46(10):1021–1026. doi: 10.3109/02770900903350473. [DOI] [PubMed] [Google Scholar]
- 26.Yuksel H, Sogut A, Yilmaz O. Attention deficit and hyperactivity symptoms in children with asthma. J Asthma. . 2008;45(7):545–547. doi: 10.1080/02770900801990016. [DOI] [PubMed] [Google Scholar]
- 27.Chida Y, Hamer M, Steptoe A. A bidirectional relationship between psychosocial factors and atopic disorders: a systematic review and meta-analysis. Psychosom Med. . 2008;70(1):102–116. doi: 10.1097/PSY.0b013e31815c1b71. [DOI] [PubMed] [Google Scholar]
- 28.Chapman KR, Boulet LP, Rea RM, Franssen E. Suboptimal asthma control: prevalence, detection and consequences in general practice. Eur Respir J. . 2008;31(2):320–325. doi: 10.1183/09031936.00039707. [DOI] [PubMed] [Google Scholar]
- 29.Ernst P, Suissa S. Pneumonia in elderly patients with chronic obstructive pulmonary disease. Curr Infect Dis Rep. . 2008;10(3):223–228. doi: 10.1007/s11908-008-0037-4. [DOI] [PubMed] [Google Scholar]
- 30.Watson WT, Becker AB, Simons FE. Treatment of allergic rhinitis with intranasal corticosteroids in patients with mild asthma: effect on lower airway responsiveness. J Allergy Clin Immunol. . 91(1 Pt. 1993;1):97–101. doi: 10.1016/0091-6749(93)90301-u. [DOI] [PubMed] [Google Scholar]
- 31.Flaherman V, Rutherford GW. A meta-analysis of the effect of high weight on asthma. Arch Dis Child. 2006;91(4):334–339. doi: 10.1136/adc.2005.080390. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
List of disease categories and conditions, their associated International Classification of Disease, 9th Revision (ICD-9) codes, and the specific populations in which they were studied.
(DOCX)