Abstract
Background
Acne is considered a cosmetic nuisance in Malaysia since no insurance coverage is provided for its treatment. Its psychological impact is unknown.
Objective
The aim of this study is to determine the impact of acne on quality of life and its relationship with severity.
Methods
A cross-sectional study using the Cardiff acne disability index (CADI) and Global Acne Grading System for acne severity grading was done in three government-run dermatology clinics in Sarawak, Malaysia.
Results
The study cohort of 200 patients had a mean CADI score of 5.1. Most of the patients (59.5%) had mild CADI impairment, with the domain of feelings most affected. Patients with a family income <1,000 United States Dollor/month had a higher mean CADI (mean 5.5 vs. 4.4; p=0.04). Females, indigenous groups, and patients with tertiary education tended to have more severe CADI impairment (p>0.05). The correlation between CADI and mild acne severity was low (Pearson correlation coefficient=0.35; p<0.001) but became insignificant for moderate and severe acne.
Conclusion
Acne impairment in Sarawak was moderate and must be addressed. It should be viewed as a psychologically disabling disease requiring optimal management and resource allocation.
Keywords: Acne vulgaris, Disability, Quality of life
INTRODUCTION
Acne is often considered a cosmetic condition in Asia. There is currently no insurance coverage for the treatment of this condition in Malaysia, and most Malaysian government-run health care clinics manned by family medicine specialists do not have proper drugs to treat this condition. The poor resource allocations are probably due to the condition being sidelined by health administrators. Nevertheless, studies from Western countries have demonstrated that acne can cause various psychosocial problems including depression, anxiety, social withdrawal, and poor self-esteem1-4. It is also associated with suicidal ideations and attempts5.
There is a paucity of data on the quality of life impact of acne in Malaysia. The impact in Sarawak, a state in the East Malaysian Borneo, is unknown. Sarawak is populated by 2.4 million people comprising 40 ethnic groups6. Indigenous people comprise approximately 75% of the population. Data on the impact on these indigenous groups is unknown and would be interesting to study.
This study was undertaken to determine the impact of acne on quality of life using the Cardiff acne disability index (CADI) and its relationship with acne severity.
MATERIALS AND METHODS
This was a cross-sectional study in patients with acne vulgaris who were >12 years of age in the Dermatology Departments of Sarawak General Hospital, All consecutive patients seen between December 2008 and July 2009 were invited to participate. Those who agreed to participate were required to provide informed written consent. This study was approved by the Malaysian Ministry of Health Research and Ethics Committee of the National Institute of Health in Malaysia.
Quality of life was measured using the CADI7, a five-item questionnaire. Questions 1 ("As a result of having acne, during the last month have you been aggressive, frustrated, or embarrassed?") and 4 ("How would you describe your feelings about the appearance of your skin over the last month?") measure feelings, questions 2 ("Do you think that having acne during the last month interfered with your daily social life, social events or relationships with members of the opposite sex?") and 3 ("During the last month, have you avoided public changing facilities or wearing swimming costumes because of your acne?") measure social functioning, and question 5 ("Please indicate how bad you think your acne is now") measures perceived severity. Each question contains 4 possible answers with a score of 0~4. The CADI score is calculated by summing the score of each question resulting in a possible maximum score of 15 and a minimum score of 0. A score of 0~5 translates to mild quality of life impairment, 6~10 indicates moderate impairment, and 11~15 demonstrates severe impairment. Permission to use this questionnaire was granted by Professor Andrew Y Finlay.
Acne severity was measured using the Global Acne Grading System (GAGS)8, a numerical grading system based on the acne lesion types and locations. The GAGS divides the acne-prone areas into six regions (five on the face and one on the chest/upper back) and gives each an area factor. Scores are as follows: comedones, 1; papules, 2; pustules, 3; and nodules, 4. The chin and nose are given a factor of 1; the forehead and each cheek are given a factor of 2; and the chest/upper back are given a factor of 3. The score for each region is the product of severity score multiplied by the area factor. The total score is the sum of all six regional scores with minimum score of 1 and a maximum score of 44. A score of 1~18 is considered mild, 19~30 is considered moderate, and >31 is considered severe.
Data were collected using standardized case report forms, including sociodemographic data, GAGS, and CADI. In the sociodemographic variables, family income is divided into <1,000 United States Dollor (USD)/month and ≥1,000 USD/month to reflect socioeconomic status. Education level was divided into primary/secondary and tertiary.
The data collected were analysed using SPSS ver. 13 (SPSS Inc., Chicago, IL, USA). Categorical data were expressed as frequencies and percentages. Continuous data were expressed as means and standard deviations. Categorical data and continuous data were analysed using the chi square test and Student's t-test, respectively. Correlations between two continuous data were analyzed using the Pearson rank order correlation test. The level of significance was set at p<0.05.
RESULTS
A total of 200 patients (125 females, 75 males; 62.5% and 37.5%, respectively) enrolled in the study. The mean age was 22.4±6.73. Ethnic groups of the cohort included: Chinese, 41%; Malays, 40%; Ibans, 9.5%; Bidayuhs, 4.5%; and other indigenous groups, 5%. Mild acne was seen in 117 patients (58.5%), moderate acne was seen in 56 patients (28%), and severe acne was seen in 27 patients (13.5%).
The mean CADI score was 5.1±3.83 (range, 0~14). Recorded impairment levels included: mild, 119 patients (59.5%); moderate, 57 patients (28.5%); and severe, 24 patients (12%). The mean scores included: feelings, 2.2± 1.80; social functioning, 1.3±1.59; and perceived severity, 1.5±0.90. In terms of analysis based on the questions, the mean scores of the questions were: 1.1±0.97 (question 1); 0.7±0.83 (question 2); 0.7±0.84 (question 3); 1.2±0.93 (question 4); and 1.5±0.90 (question 5). Questions 2 and 3 were the least affected. With regard to question 2 ("Do you think that having acne during the last month interfered with your daily social life, social events or relationships with members of the opposite sex?"), 56% of patients answered not at all. Regarding question 3 ("During the last month, have you avoided public changing facilities or wearing swimming costumes because of your acne?"), 55% of patients answered not at all.
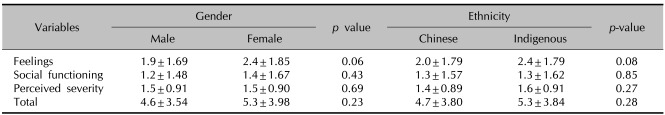
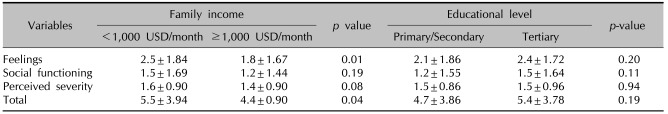
There were no significant differences in the quality of life impairment based on gender and ethnicity (Table 1). However, there was a tendency for females and indigenous groups to have a more severely impaired quality of life. Similarly, patients with tertiary education also had more severe quality of life impairment, although the differences were not statistically significant (Table 2).
Table 1.
Mean CADIs based on gender and ethnicity
CADI: Cardiff acne disability index score.
Table 2.
Mean CADI scores based on family income and educational level
CADI: Cardiff acne disability index, USD: United States Dollar.
Patients with family income <1,000 USD had higher mean CADI compared to those with family income ≥1,000 USD (mean score, 5.5 vs. 4.4; p=0.04). The former also had more severe impairment in the domain of feelings (mean score, 2.5 vs. 1.8; p=0.01). However, social functioning and perceived severity were not significantly different between the two groups, although the former tend to have higher mean scores.
The correlation between CADI and GAGS was low (Pearson rank order correlation coefficient=0.42; p<0.001). Based on acne severity, the correlation for patients with mild acne was low (Pearson rank order correlation coefficient=0.35; p<0.001) but it became insignificant for moderate (Pearson rank order correlation coefficient=0.04; p=0.79) and severe acne (Pearson rank order correlation coefficient=0.07; p=0.74).
DISCUSSION
The mean CADI score of 5.1 indicates that the average patient in Sarawak experienced moderately impaired quality of life due to their acne. This mean score was comparable to that of a community study in France9. In that study, the mean CADI score was 5.57 in female patients 12~16 years and 5.26 for females 17~23 years. However, the CADI score wasHoIit wasit two-fold higher than that of university students in Hong Kong. In that study, the mean score was only 2.5610. This difference might be due to the variation in the study setting. The Hong Kong study utilized students entering university in the community, whereas this current study examined patients with acne in dermatology clinics. It is postulated that patients seeking treatment in the specialist dermatology clinics usually have more psychological distress due to their condition even before the consultation. However, the mean CADI was two-fold higher in France compared to Hong Kong. This might be due to the fact that individuals in Western communities are encouraged to express their feelings and concerns, whereas Asians are not. This probably explained the comparable quality of life impairment between the community study in France and a clinic based study in Sarawak.
Patients in Sarawak were least affected in the domain of social functioning. This is probably attributed to the upbringing of this population, which encourages stoicism11. Indigenous and rural Chinese populations usually feel uneasy discussing their private social lives, especially with regard to relationships. On question 3, 55% of patients expressed no concerns because there are very few swimming pools in Sarawak. Moreover, it is not common practice to wear swimming costumes. Most people in Sarawak wear sport suits to swimming pools or beaches. In addition, Muslims ladies are required to cover their entire bodies and expose only their faces.
One of the implications of this study puts greater emphasis on the quality of life issues in patients with lower socioeconomic status. Quality of life impairment was significantly more severe in patients with family income <1,000 USD. One of the reasons for this might be that these patients could not afford good over-the-counter medications or proper care with private dermatologists. They are also more likely to be staying in rural areas, making visits to dermatology clinics in the town center difficult. This probably contributed to the higher default rate and, therefore, poorer response to treatment and more severe quality of life impairment. Moreover, patients with lower socioeconomic status who make an effort to visit dermatology clinics tend to be more concerned about their condition.
It is imperative that quality of life issues based on gender, ethnicity, and educational status not be judged. Few studies have found that females have more severe quality of life impairment due to their acne10,12. However, this study showed no significant difference in quality of life issues based on gender, although females tended to have more severe impairment. Similarly, there was no difference based on ethnicity, although there was a tendency for indigenous people to have more severe impairment. This finding is surprising since it has been postulated that more affluent Chinese are more concerned about their emotional and physical conditions. On a similar note, more highly educated patients are thought to have more severe quality of life impairments. However, contrary to the hypothesis, there was no significant difference in quality of life issues based on educational status. Thus, it is important that practicing clinicians equally delve into the quality of life issues in all patients with acne.
Quality of life impairment was poorly correlated with acne severity. There was also no correlation in patients with moderate and severe acne, indicating that quality of life should not be judged based on severity. Hence, it is imperative that quality of life issues be addressed in all patients with acne. This is an important point that must be stressed in the training of medical students and junior doctors since the treatment of acne should not be based on acne severity alone but also on the degree of quality of life impairment. Health administrators should also be informed that treatment with isotretinoin, one of the most expensive dermatology medications, should not be confined to patients with severe acne but also be offered to patients with severely impaired quality of life.
Health care administrators and insurance agencies should view acne as a psychologically disabling condition. The current study demonstrated that the quality of life impairment in Malaysia was more severe than that in Hong Kong and comparable to that in France. Hence, acne should not be considered a cosmetic nuisance and should be treated optimally. Moreover, medical students and junior doctors should be educated on quality of life issues in addition to the usual education on disease process and treatment. More continuing medical education on the aspect of quality of life in acne should also be organized.
In conclusion, the CADI impairment in Sarawak was moderate and comparable with that in the community study in France. Patients with lower socioeconomic status had significantly more severe impairment. There was a low correlation between the quality of life impairment and mild acne, but it became insignificant with regard to moderate and severe acne. Thus, quality of life issues must be addressed in all patients with acne vulgaris. Health care providers and administrators should view acne as a psychologically disabling disease requiring optimal management and resource allocation. The education of medical students and junior doctors should also incorporate quality of life issues.
ACKNOWLEDGMENTS
The author would like to thank Dr Pubalan Muniandy, Datuk Dr Roshidah Baba, Datin Dr Asmah Johar, Dr Chang Choong Chor, Dr Goh Pik Pin, Clinical Research Centre, Sarawak Foundation and all the staff of Dermatology Departments of Sarawak General Hospital, Sibu Hospital and Miri Hospital.
References
- 1.Cunliffe WJ. Acne and unemployment. Br J Dermatol. 1986;115:386. doi: 10.1111/j.1365-2133.1986.tb05757.x. [DOI] [PubMed] [Google Scholar]
- 2.Aktan S, Ozmen E, Sanli B. Anxiety, depression, and nature of acne vulgaris in adolescents. Int J Dermatol. 2000;39:354–357. doi: 10.1046/j.1365-4362.2000.00907.x. [DOI] [PubMed] [Google Scholar]
- 3.Koo J. The psychosocial impact of acne: patients' perceptions. J Am Acad Dermatol. 1995;32:S26–S30. doi: 10.1016/0190-9622(95)90417-4. [DOI] [PubMed] [Google Scholar]
- 4.Law PM, Chuh AAT, Lee A. Acne: its psychological consequences and management. Hong Kong Prac. 2006;28:1–5. [Google Scholar]
- 5.Purvis D, Robinson E, Merry S, Watson P. Acne, anxiety, depression and suicide in teenagers: a cross-sectional survey of New Zealand secondary school students. J Paediatr Child Health. 2006;42:793–796. doi: 10.1111/j.1440-1754.2006.00979.x. [DOI] [PubMed] [Google Scholar]
- 6.Yap FB. Clinical characteristics of basal cell carcinoma in a tertiary hospital in Sarawak, Malaysia. Int J Dermatol. 2010;49:176–179. doi: 10.1111/j.1365-4632.2009.04342.x. [DOI] [PubMed] [Google Scholar]
- 7.Motley RJ, Finlay AY. Practical use of a disability index in the routine management of acne. Clin Exp Dermatol. 1992;17:1–3. doi: 10.1111/j.1365-2230.1992.tb02521.x. [DOI] [PubMed] [Google Scholar]
- 8.Doshi A, Zaheer A, Stiller MJ. A comparison of current acne grading systems and proposal of a novel system. Int J Dermatol. 1997;36:416–418. doi: 10.1046/j.1365-4362.1997.00099.x. [DOI] [PubMed] [Google Scholar]
- 9.Poli F, Taieb C, Ambonati M, Bousetta S. Acne and quality of life: the pertinence of the CADI score. J Am Acad Dermatol. 2009;60:AB 21. [Google Scholar]
- 10.Law MP, Chuh AA, Lee A, Molinari N. Acne prevalence and beyond: acne disability and its predictive factors among Chinese late adolescents in Hong Kong. Clin Exp Dermatol. 2010;35:16–21. doi: 10.1111/j.1365-2230.2009.03340.x. [DOI] [PubMed] [Google Scholar]
- 11.Yap FB. Psoriasis among Sarawakian natives in a tertiary skin centre in Sarawak. Australas J Dermatol. 2010;51:210–211. doi: 10.1111/j.1440-0960.2010.00647.x. [DOI] [PubMed] [Google Scholar]
- 12.Abdel-Hafez K, Mahran AM, Hofny ER, Mohammed KA, Darweesh AM, Aal AA. The impact of acne vulgaris on the quality of life and psychologic status in patients from upper Egypt. Int J Dermatol. 2009;48:280–285. doi: 10.1111/j.1365-4632.2009.03838.x. [DOI] [PubMed] [Google Scholar]