Abstract
Understanding the mechanisms contributing to correlated BMI outcomes in a social network such as siblings will help policy makers reduce the burden of disease associated with obesity. There are two potential mechanisms explaining correlated BMI outcomes in a biologically related social network: (i) time constant factors such as genetic heritability and habits formed during childhood and (ii) factors that change over time some of which are dependent on the frequency of interactions between the social network, for example, social norms shaped by the social network's shifting attitudes towards weight and behaviors related to weight, or environmental factors like opportunities for exercise. This study aims to distinguish between time constant factors from factors that are likely to change over time to gain a better understanding of the mechanisms explaining the correlation in sibling BMI. We exploit data from the Panel Study of Income Dynamics (PSID) over 1999–2007 estimating the correlation in BMI for adult siblings who currently live in separate households but grew-up in the same household and adolescent siblings currently living in the same household to isolate the influence of factors that change over time. The findings indicate that time constant factors explain some of the overall correlation in sibling BMI for both cohorts of siblings. Factors that change over time only significantly impact on the overall correlation in BMI for adolescent siblings suggesting if there is a social network influence on correlations in BMI this is facilitated by sharing the same household.
Introduction
Obesity rates remain persistently high in the United States. National obesity prevalence increased by 12.6% between 1990 and 2007 (1); and recent data reveals state by state variation, with the proportion of obese adults ranging from 18.6% in Colorado to 34.4% in Mississippi. (2) A social contagion effect in which obesity spreads throughout a social network has been proposed as one explanation for the persistence of high obesity rates (3,4,5,6,7). The theory suggests that weight gain of one member in a social group may affect the weight gain of other members of the network (8,9). One channel through which the spread of weight operates is social norms (10,11,12). Attitudes about body weight are formed by observing the weight of other members of one's social group. Individuals whose social group is heavier may view a higher weight as socially acceptable resulting in the spread of obesity in the social network.
The mechanisms behind the “anchoring” of social norms related to weight are not well understood. Social norms regarding acceptable weight may be formed in childhood, which suggests that these norms are constant over time. This will further be referred to as habits formed during childhood. This would contribute to a convergence of BMI over time if siblings formed similar habits during childhood that influenced their lifetime weight related behavior.
Another possibility is that social norms may be dependent on the frequency of interactions with members of the social network (13,14) implying that norms may change over time. Less frequent interactions with members of a social group would then suggest that members may have less of an influence on shaping weight norms. Weight may only spread through a social network where there is greater opportunity for face-to-face interaction of its members facilitating the establishment of shared social norms. We refer to this as a social network influence on BMI. It is hypothesized that social networks may strengthen the correlation in BMI for adolescent siblings living in the same household who are likely to have more face-to-face interactions with their siblings helping to shape their shared weight related social norms. Whereas for adult siblings living in separate households they may not have as frequent face-to-face interactions with their siblings leading to divergent weight related social norms, reducing the correlation in BMI.
We build upon previous research on correlated BMI outcomes in siblings (3,15,16) by distinguishing time constant factors representing genetic heritability and habits formed during childhood related to weight behavior from factors that change over time such as the social network influence on weight and environmental factors on the overall correlation in sibling BMI. Longitudinal data analysis is undertaken using two cohorts of siblings: adults siblings (27–55 years old) who grew up in the same household and are currently living in separate households and adolescent siblings (10–18 years old) who are currently living in the same household.
Methods and Procedures
Sample
The Panel Study of Income Dynamics (PSID) and the Child Development Supplement (CDS) were employed to investigate the factors contributing to correlated BMI outcomes in adult and adolescent sibling groups (17). The PSID is a nationally representative longitudinal survey of around 9,000 households which started in 1968. It has been used in numerous academic and policy studies (18). The quality of health data in the survey has been analyzed in relation to data from other nationally representative surveys such as the National Health Interview Survey and the Health and Retirement Survey. Results indicate that the quality of health data in the PSID is high suggesting that this data should give an accurate picture of the health status of the sample population (19). The adult dataset comes from the Survey Research Center component of the main sample of the PSID. Sample attrition and composition implies that the sample is no longer representative of the U.S. population. This component of the PSID is used because it contains parental characteristics, information necessary to test for the impact of habits formed during childhood and genetic heritability on correlated BMI outcomes. There are 838 adult sibling groups with 1,636 observations.
The adolescent sample uses data from the CDS, a supplement to the main PSID sample (20). The CDS began in 1997, collecting additional data from PSID parents and their children aged between 0 and 12 years old providing information on 3,563 children. These families were recontacted in 2002–2003 for the CDS II and information on 2,907 children and adolescents between ages 5 and 18 were collected. A third round of the CDS was conducted in 2007 and 1,056 children between the ages of 10–19 were successfully reinterviewed. The analysis uses data from the CDS II and CDS III rounds of data collection following a sample of sibling children as they move from childhood to adolescence. The sample is restricted to sibling groups that are present in both rounds of data collection and are living in the same household. Supplemental parental information from the 2001, 2003, and 2007 rounds of the main PSID survey are included in the analysis. There are 236 sibling groups (472 observations).
Both the adolescent and adult cohort siblings are matched in the data using the Family Identification Mapping System allowing for the analysis of intragenerational ties (21). The sample includes only siblings who share at least one biological parent.
Measures
The outcome measure for both cohorts of siblings is BMI (measured as weight in kilograms divided by height in m2). For the adult sample, questions on height and weight that are self-reported by the survey respondent are used to calculate BMI. This information was collected on a biennial basis beginning in 1999. BMI data from the 1999, 2001, 2003, 2005, and 2007 rounds of data collection are used in the analysis. For the adolescent sample the BMI variable is taken from the CDS and was calculated from height measured in feet and inches and weight in pounds measured by the interviewer. BMI measures from the CDS are taken from the 2002 and 2007 data collection rounds.
We divide the explanatory variables into three categories of individual demographic characteristics, environmental factors, and family background. It is hypothesized that these three categories will control for time constant factors and factors that change over time that can be captured by observable variables. Additional questions are asked to survey respondents and primary caregivers in the CDS that are not asked to respondents that only appear in the main sample. Different explanatory variables are therefore used in the adult and adolescent model to control for observable factors impacting on the correlation in sibling BMI.
Adult models
The demographic characteristics included in the adult sibling model are age, a dummy variable that equals one if the respondent is female and is equal to zero otherwise, an indicator variable that equals one if the siblings are of the same gender and is equal to zero otherwise, an indicator variable controlling for if the respondent is married or cohabiting, a dummy variable that equals one if the respondent reports participating in vigorous physical activity at least once a week and is equal to zero otherwise, and finally a dummy variable that equals one if the respondent reports drinking alcohol and is equal to zero otherwise. It is expected that BMI will change with age which may impact on the correlation in sibling BMI. If siblings are of the same gender this may impact on the correlation in BMI. It is likely that siblings of the same gender will have a greater correlation in BMI. Being married and having a separate family may affect the amount of time that siblings spend together impacting on the social network influence on correlated BMI outcomes. Participating in physical activity and drinking alcohol may have an impact on BMI and be influenced by social network norms.
The environmental factors included in the adult model are regional dummies controlling for living in the Northeast, North Central, or Western states compared to the base category of living in Southern states. Respondents in Alaska and Hawaii are excluded from the analysis. A dummy variable is also included in the analysis that equals one if siblings live in the same state and is equal to zero otherwise. A binary variable that equals one if the respondent lives in a county with a city that has over 500,000 residents and is equal to zero otherwise is also included in the analysis. The regional dummies control for local social norms regarding weight that may influence BMI. If siblings live in the same state this may impact on the frequency of their face-to-face interactions which will affect the social network spread of BMI. They may also be exposed to similar local norms regarding weight. Having a large city in the county of residence may impact on the availability of healthy food and physical activity opportunities (22). A variable related to the household environment is also included in the analysis. It is a binary variable that equals one if the respondent eats with their family every day. Meals ate at home are likely to be healthier impacting on BMI. If adult siblings have different family meal experiences this may reduce the social network influence on BMI.
The family background variables included in the adult model are the total number of children born to the mother. The number of children will impact on the distribution of household resources and may influence the formation of lifelong habits related to weight. A binary variable that equals one if the mother was married at the time of the birth of the respondent and is equal to zero otherwise is also included in the model. Mother's marital status may have affected the resources available to the child in early life impacting on BMI. Finally a variable controlling for the age gap between siblings which is measured in years is included in the model. The social network influence of siblings is likely to be influenced by the age gap between them.
Adolescent models
The demographic characteristics included in the adolescent models are age, a dummy variable for being female, an indicator variable for siblings being of the same gender, a binary variable that equals one if the respondent eats breakfast each morning and is equal to zero otherwise, and a dummy variable that equals one if the respondent participates in an after school sports organization. The first three demographic variables are the same as in the adult models and are included for similar reasons. Eating breakfast every day is associated with increased likelihood of maintaining a healthy weight (23). Belonging to an afterschool sports organization suggests that the child is exercising at least once a week which may impact on BMI. Children who form healthy habits are more likely to make healthy choices as adults.
The environmental characteristics in the adolescent models are divided into three subcategories. The first subcategory controls for the safety of the local built environment which is a proxy for opportunities for exercise. These are three indicator variables: (i) caregivers being able to identify strangers in the neighborhood, (ii) caregivers feeling they are able to stop neighborhood children from stealing, and (iii) caregivers feeling they are able to stop individuals from selling drugs to neighborhood children. If the local environment is perceived as unsafe by caregivers then there may be fewer opportunities for children to spend time outside and engage in physical activity impacting on BMI. The second subcategory controls for other characteristics of the built environment. A dummy variable which equals one if the family has lived in the same place of residence for 5 years and is equal to zero otherwise is included in the model. Tenancy may affect the influence of the exercise opportunities afforded by the local built environment to impact on BMI. Similar to the adult models, a dummy variable controlling for if the largest city in the county has 500,000 or more respondents is included in the model. The final subcategory controls for household characteristics. A dummy variable that equals one if the child eats with their family at least once a week and is equal to zero otherwise is included in the model. Family meal time will help shape children's eating habits. In addition family's eating together will impact on the social network influence on correlated BMI outcomes. The model also includes an indicator variable which equals one if the child attends family gatherings at least once a month and is equal to zero otherwise. It is expected that more frequent family interactions will influence the impact of the family social network on BMI.
The family background characteristics included in the adolescent model are an indicator variable for the head of the household's employment status and a dummy variable controlling for if the head of the household is a single parent, and two indicator variables for head of household's educational attainment. These variables are used to control for household resources which may impact on correlated BMI outcomes in siblings. Parental education may also impact on their health knowledge which could affect their children's BMI outcomes. Finally, similar to the adult models a dummy variable for the age gap between siblings is included in the model.
Analysis
A statistical method commonly employed in quantitative genetics, restricted maximum likelihood, is used to distinguish the impact of time constant factors from factors that change over time on the correlation in BMI for the two cohorts of siblings (24,25). In quantitative genetics this methodology is applied to estimate the correlation in phenotypic expression that arises from shared genes rather than random environmental effects. This is accomplished by decomposing a known quantitative trait within family groups. A maximum likelihood function is applied to maximize the probability of the variance–covariance structure containing the factors related to shared genes and gene–environment interactions on phenotypic expression. The variance–covariance structure between family members is used to calculate the interclass correlation coefficient. This shows the heritability of the quantitative trait in question (26,27).
We calculate the correlation coefficient on BMI outcomes in the two sibling samples by estimating a variance–covariance matrix containing time constant factors such as mother's marital status at birth, age gap between siblings, and other immeasurable characteristics such as genetic information. The method used to calculate this component of the correlation in sibling BMI is analogous to the methods used in quantitative genetics. However, we do not have data on genetic information to isolate the genetic heritability of BMI between siblings from habits formed during childhood that are constant over time. We modify the quantitative genetics framework by adding an additional variance–covariance matrix to the decomposition of correlated sibling BMI outcomes. A separate variance–covariance matrix is estimated that captures factors that change over time such as age, eating breakfast everyday, participating in vigorous physical activity, and other immeasurable factors such as social influence. These two matrices are summed to calculate the overall correlation in sibling BMI.
Results
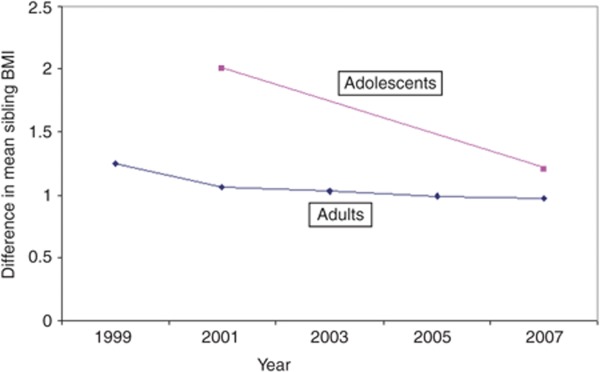
Figure 1 investigates the trend in sibling BMI over the sample period by showing the difference in mean BMI between adult siblings over the 1999–2007 period and adolescent siblings over the 2002–2007 period. If mean sibling BMI is converging over this period this suggests that there are some factors either related to time constant factors such as genetic heritability or habits formed in childhood or factors that change over time such as the social spread of BMI that may be influencing this convergence. In 1999, the mean difference between adult siblings BMI was 1.10; this decreased to 0.97 in 2007. The mean difference between adolescent siblings BMI was 2 in 2002 which decreased to 1.2 in 2007. The statistical significance of the linear trend of a convergence in BMI within sibling groups was tested by estimating a Cochran–Armitage (28,29) type test for continuous data using a variance weighted least square regression. The null-hypothesis of no trend is rejected (P = 0.000).
Figure 1.
Difference in mean sibling BMI 1999–2007.
The next step of the analysis investigates the mechanisms contributing to the overall correlation in sibling BMI focusing on two distinct components: the role of time constant factors and factors that change over time which includes the social network influence on BMI.
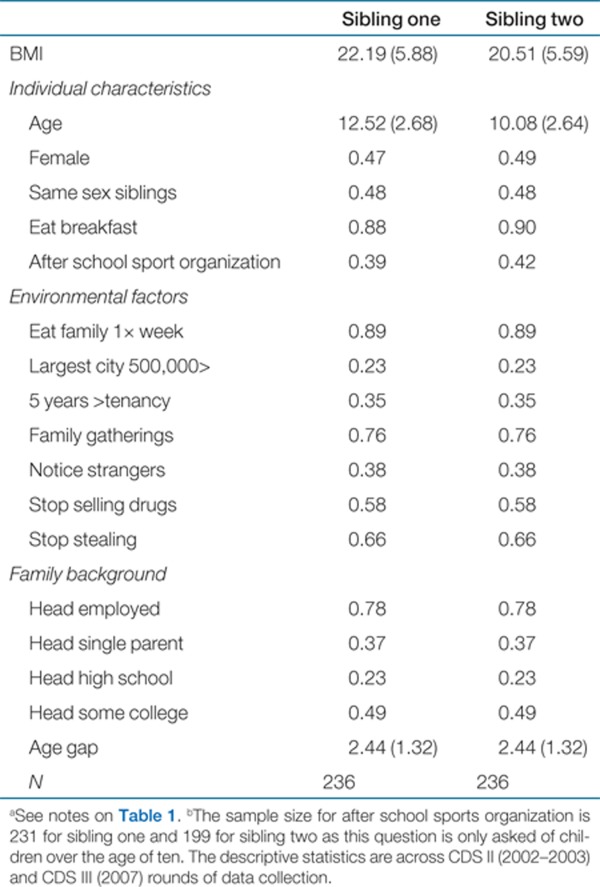
Tables 1 and 2 show the descriptive statistics of the variables included in the models for the adult and adolescent equations. Sibling one is the oldest sibling in the household, sibling two is the younger sibling. In households with more than two siblings, sibling two is the mean for each variable in the descriptive statistics of all younger siblings. The mean age of the older adult sibling is ~46 years old and the mean age of younger sibling(s) is 41 years old. Most of the adult sample is married or cohabiting and was born to a mother that was married at time of birth. The mean age of sibling one in the adolescent sample is 12 years old and the mean age of the younger sibling(s) is 10 years old. The majority of the adolescent sample eats breakfast everyday, eats with their family once a week, and is in a family where the head of household is currently employed.
Table 1. Adult sibling characteristics: Panel study of income dynamics 1999–2007.
Table 2. Adolescent characteristics: child development supplement 2002 and 2007.
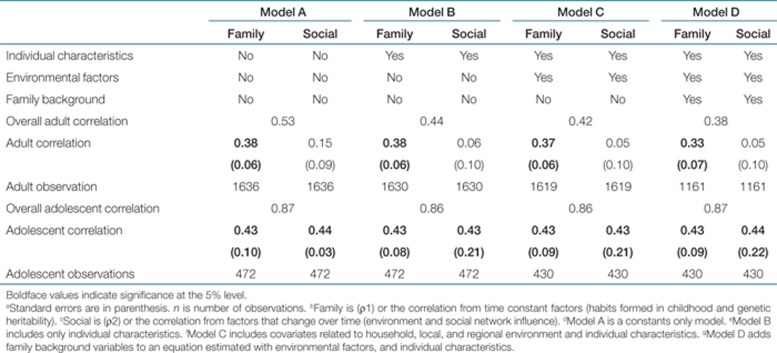
Table 3 shows the results from the quantitative analysis investigating the mechanisms explaining the overall correlation in sibling BMI for the two cohorts of siblings. If the household facilitates the social network spread of obesity by operating through factors that change over time the magnitude of the coefficient on the correlation in sibling BMI will be different for the two cohorts of siblings. If changes to the environment, such as types of food available or parental behaviors and characteristics related to weight as a response to environmental incentives, impacts on the influence of time constant factors on BMI then the correlation in BMI may differ for the adult and adolescent sample who may have been exposed to different environmental factors that influence BMI (30,31). This implies that habits formed during childhood BMI may have cohort effects.
Table 3. Decomposition of correlations in sibling BMI.
Model A in Table 1 is a constants only model that includes all observable and unobservable factors influencing the correlation in sibling BMI. The total adult sibling correlation coefficient is 0.53; 38% (95% confidence interval (CI), 0.26–0.51) of this stems from time constant factors and 15% (P > 0.05) comes from factors that change over time. For Model A, the total adolescent sibling BMI correlation coefficient is 0.87. Time constant factors contribute 43% (95% CI: 0.23–0.63) and factors that change over time contribute 44% (95% CI, 0.38–0.50).
Model B adds a vector of observable demographic characteristics to the analysis. These observable demographic characteristics are therefore removed from the estimated covariance–variance matrices used to calculate the overall correlation in sibling BMI. After controlling for observable demographic characteristics, the total adult correlation in BMI is reduced to 0.44 with time constant factors still accounting for 38% (95% CI, 0.26–0.51) of this correlation and factors that change over time now contributing only 6% (P > 0.05). In Model B for the adolescent sample, the overall BMI correlation coefficient is more or less the same as in Model A at 0.86.
Model C adds environmental factors to the analysis. The regression equation estimated includes variables controlling for individual characteristics and environmental factors. For both adult and adolescent siblings the correlation coefficients and relative shares of time constant factors and factors that change over time are the same as in model B.
Model D adds family background characteristics to the regression equation. The model estimated includes observable demographic characteristics, environmental factors, and family background characteristics which are removed from the covariance–variance matrices used to estimate the correlation coefficients. The overall adult sibling BMI correlation coefficient is slightly reduced to 0.38 with time constant factors contributing 33% (95 CI, 0.19–0.46) and factors that change over time contributing 5% (P > 0.10). The adolescent correlation coefficient and relative shares of time constant factors and factors that change over time are once again unchanged.
The estimation strategy investigates the impact of observed and unobserved time constant factors and factors that change over time on the correlation in sibling BMI. The observed demographic, environmental, and family background characteristics in models B, C, and D do not contribute to the explanation of factors contributing to the correlation in sibling BMI for the adolescent cohort. Similarly, environmental factors do not contribute to explaining the correlation in BMI in the adult models. To test the validity of these variables in explaining individual BMI, simple OLS regressions were run on the adult and an adolescent sample. For both adults and adolescent having a city with more than 500,000 residents significantly impacted on individual BMI. For the adolescent sample all of the family background characteristics and belonging to an afterschool sports organization significantly impacted on individual BMI. This implies, that especially for the adolescent models, these variables may not explain correlated BMI outcomes between siblings but are still reasonable at explaining individual BMI. The main results of this research are found in what is not observed. Time constant factors significantly explain the correlation in BMI for both cohorts of siblings whereas unobserved and immeasurable factors that change over time only significantly explain the correlation in BMI for adolescent siblings.
Discussion
Time constant factors which includes genes, gene–environment interactions, and parental behaviors and characteristics significantly explains some of the correlation in BMI for both cohorts of siblings. These results conform to findings from the behavioral genetics literature highlighting the importance of genetic factors in explaining weight outcomes (32,33,34). The results suggest that family background characteristics play an important role in explaining adult outcomes supporting our hypothesis regarding the formation of habits formed during childhood impacting on weight outcomes in adulthood.
We hypothesize that factors that change over time may be capturing some of the social network influence on BMI which are not captured by any of the observable variables. Geographical distance may play a role in the social network influence on BMI operating through the frequency of face-to-face interactions of members of a social network. Other studies that have investigated BMI outcomes in adult siblings using secondary data have used datasets that focus on respondents living in a particular city (3). Adult siblings living in the same city may have more face-to-face interactions influencing perceptions about an acceptable weight and weight outcomes. By using a national study, we highlight the limits of using social networks to explain the spread of health related outcomes. This suggests that prior studies may have overestimated the social network influence on BMI. If the social network influence of BMI is partially determined by shifting attitude regarding weight perception and weight related behavior (3,35), then it is likely that siblings who are separated by large geographical distances and have infrequent face-to-face interactions will not be able to influence each other's weight in this manner.
Finally, previous research (3,4,5,6,7) has not separated time constant factors from factors that change over time influencing the overall correlation in BMI. This may have led to a misspecification of the mechanisms leading to a perceived spread in BMI.
Implications
Our study has important implications for obesity policy. Evidence from the adult models suggests that family background significantly impacts on the correlation in sibling BMI. This demonstrates the importance of early childhood interventions and prevention programs to promote a healthier population.
Using social networks to spread healthy behaviors has been suggested as a cost-effective public health policy tool (2,35). Our findings indicate that if social network influence is captured in the variance covariance matrix controlling for factors that change over time, the household may facilitate the spread of health related behaviors. The results have shown an important limitation of the social network approach finding no evidence of significant impact of factors that change over time on the correlation in sibling BMI for adults living in separate households. Using social networks to spread healthy behaviors may only be a feasible intervention tool for participants that can engage in face-to-face interactions with social network members helping to anchor social norms that change over time.
Limitations
There are some important limitations to this study. Observational data have well known limitations. Sample attrition for the adult sample means our results are not nationally representative of adult siblings. The small sample sizes are also a potential limitation. Larger sample sizes may lead to more robust findings especially for the adolescent sample. Different explanatory variables are used in the adult and adolescent equations which may impact on the correlation coefficients. Because of the different variables available in the dataset there is no method to adequately control for cohort affects that may impact on our findings. We are unable to determine the number of interactions between siblings. We assume that interactions are captured in the unobserved component of the variance-covariance matrix of factors that change over time. The data also does not allow the separation of genetics from habits that are formed during childhood giving an upper bound on the influence of habits formed during childhood on the correlation in sibling BMI.
The lack of a contribution of environmental factors to the correlation in BMI for both cohorts of siblings is a potential limitation of this work. It is possible that a wider range of environmental controls such as number of parks or fast food outlet concentration would be needed. However, this is beyond the scope of this study. What we can say is that demographic characteristics and family background do significantly contribute to the correlation in BMI for adult siblings. Unobserved and immeasurable factors that change over time only significantly explain the correlation in adolescent sibling BMI. From these findings we can extrapolate that the household facilitates the impact of factors that change over time on correlations in sibling BMI. The influence of factors that change over time on correlated BMI outcomes is not present in adult siblings living in separate households.
Another important limitation is that there are only two observations for the adolescent sibling pairs. A lack of variation in the sibling data suggests that our estimates will be the upper bound of the correlation in adolescent sibling BMI. There may be measurement bias in the adult BMI measures since these are self-reported. There is evidence (36) to suggest that self-reported measures of BMI are relatively reliable for population based observational studies. In addition, continuous measures of BMI are more reliable than cut-offs for overweight and obesity if there is misreporting near the boundaries of the weight categories.
This article found that time constant factors explain some of the overall correlation in BMI for both cohorts of siblings. Shared family background and demographic characteristics explain some of this time constant correlation in adult sibling BMI. Factors that change over time only significantly explain some of the correlation in BMI for adolescent siblings living in the same household. These results highlight the importance of distinguishing between different mechanisms that are associated with the correlation in sibling BMI when developing effective health policy.
Acknowledgments
The authors thank Jason Fletcher, Bhashkar Mazumder, Bob Schoeni, and Vicki Freedman for their helpful comments on draft versions of this paper. This research is funded by the MRC/ESRC/NIHR under grant G0802291.
The authors declared no conflict of interest.
REFERENCES
- Smith TG, McCluskey JJ.The economic psychology of body weight evidence from country level obesity rates in the OECD. Washington State University, School of Economic Sciences, 2009. Accessed on 23 February 2011 < < http://www.ses.wsu.edu/People/TSmith/OECDslides.pdf >
- Sherry B, Blanck HM, Galuska DA, Pan L, Dietz WH, Balluz L. Vital signs: State specific obesity prevalence among adults-United States 2009. MMWR Morb Mortal Wkly Rep. 2010;59 [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357:370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- Cohen-Cole E, Fletcher JM. Is obesity contagious? Social networks vs. environmental factors in the obesity epidemic. J Health Econ. 2008;27:1382–1387. doi: 10.1016/j.jhealeco.2008.04.005. [DOI] [PubMed] [Google Scholar]
- Halliday TJ, Kwak S. Weight gain in adolescents and their peers. Econ Hum Biol. 2009;7:181–190. doi: 10.1016/j.ehb.2009.05.002. [DOI] [PubMed] [Google Scholar]
- Renna F, Grafova IB, Thakur N. The effect of friends on adolescent body weight. Econ Hum Biol. 2008;6:377–387. doi: 10.1016/j.ehb.2008.06.005. [DOI] [PubMed] [Google Scholar]
- Trogdon JG, Nonnemaker J, Pais J. Peer effects in adolescent overweight. J Health Econ. 2008;27:1388–1399. doi: 10.1016/j.jhealeco.2008.05.003. [DOI] [PubMed] [Google Scholar]
- Newman MEJ. The structure and function of complex networks. SIAM Rev. 2003;45:167–25. [Google Scholar]
- Watts DJ, Strogatz SH. Collective dynamics of 'small-world' networks. Nature. 1998;393:440–442. doi: 10.1038/30918. [DOI] [PubMed] [Google Scholar]
- Burke MA., and, Heiland F. Social dynamics of obesity. Econ Inq. 2007;45:571–591.. [Google Scholar]
- Etilé F. Social norms, ideal body weight and food attitudes. Health Econ. 2007;16:945–966. doi: 10.1002/hec.1251. [DOI] [PubMed] [Google Scholar]
- Oswald AJ, Powdthavee N. Obesity, unhappiness, and the challenge of affluence: Theory and evidence. Economic J. 2007;117:441–454.. [Google Scholar]
- Homans GC. Social behaviour as exchange. Amer J Sociol. 1958;63:597–606. [Google Scholar]
- Adams BN. Interaction theory and the social network. Sociometry. 1967;30:64–78. [PubMed] [Google Scholar]
- Röbl M, Knerr I, Keller KM.et al. [Obesity in children and adolescents and their parents. Correlation of standardized body mass index between patients, their parents and siblings from the multicentre APS data] Dtsch Med Wochenschr 20081332448–2453. [DOI] [PubMed] [Google Scholar]
- Provencher V, Pérusse L, Bouchard L.et al. Familial resemblance in eating behaviors in men and women from the Quebec Family Study Obes Res 2005131624–1629. [DOI] [PubMed] [Google Scholar]
- Panel Study of Income Dynamics, public use dataset. Ann Arbor, MI.: Produced and distributed by the University of Michigan with primary funding from the National Science Foundation, the National Institute of Aging, and the National Institute of Child Health and Human Development, 2011
- Zimmerman FJ, Bell JF. Associations of television content type and obesity in children. Am J Public Health. 2010;100:334–340. doi: 10.2105/AJPH.2008.155119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreski P, McGonagle K, Schoeni RF. Analysis of the quality of the health data in the PSID. Panel Study Of Income Dynamics Technical Paper Series. 2009;09-02. [Google Scholar]
- Child Development Supplement. Panel Study of Income Dynamics. < . < http://psidonline.isr.umich.edu/CDS/cdsguide.html >. ( 2010. Accessed 8 February 2010.
- Family Identification and Mapping System. Panel Study of Income Dynamics. < . < http://simba.isr.umich.edu/FIMS/ > ( 2010. Accessed 10 March 2010.
- Ver Ploeg M, Breneman V, Farrigan T.et al. Access to affordable and nutritious food-Measuring and understanding food deserts and their consequences Report to Congress . CDC Administrative Publication 2009A036160 [Google Scholar]
- Timlin MT, Pereira MA, Story M, Neumark-Sztainer D. Breakfast eating and weight change in a 5-year prospective analysis of adolescents: Project EAT (Eating Among Teens) Pediatrics. 2008;121:e638–e645. doi: 10.1542/peds.2007-1035. [DOI] [PubMed] [Google Scholar]
- Searle SR, Casella G, McCulloch H. New York, NY: Wiley; 1992. Variance Components; pp. 90–108. [Google Scholar]
- Demidenko E. New York, NY: Wiley; 2004. Mixed Models: Theory and Application; pp. 45–116. [Google Scholar]
- Mishchenko K, Holmgren S, Ronnegård L. Newton-type methods for REML estimation in genetic analysis of quantitative traits. Journal of Computational Methods in Science and Engineering. 2008;8:53–67.. [Google Scholar]
- Lynch M, Walsh B. Sunderland, MA: Sinauer Associates; 1998. Genetics and Analysis of Quantitative Traits; pp. 560–563. [Google Scholar]
- Cochran WG. Some methods for strengthening the common chi-square tests. Biometrics. 1954;10:417–451. [Google Scholar]
- Armitage P. Tests for linear trends in proportions and frequencies. Biometrics. 1955;11:375–386. [Google Scholar]
- Johanssen DL, Johanssen NM, Specker BL. Influence of parent's eating behaviors and child-feeding practices on children's weight status. Obesity. 2006;14:431–439. doi: 10.1038/oby.2006.57. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Birch LL. Parents' and children's adiposity and eating style. Pediatrics. 1994;94:653–661. [PubMed] [Google Scholar]
- Maes HH, Neale MC, Eaves LJ. Genetic and environmental factors in relative body weight and human adiposity. Behav Genet. 1997;27:325–351. doi: 10.1023/a:1025635913927. [DOI] [PubMed] [Google Scholar]
- Comuzzie AG, Allison DB. The search for human obesity genes. Science. 1998;280:1374–1377. doi: 10.1126/science.280.5368.1374. [DOI] [PubMed] [Google Scholar]
- Knuiman MW, Divitini ML, Welborn TA, Bartholomew HC. Familial correlations, cohabitation effects, and heritability for cardiovascular risk factors. Ann Epidemiol. 1996;6:188–194. doi: 10.1016/1047-2797(96)00004-x. [DOI] [PubMed] [Google Scholar]
- Thaler R, Sunstein C. Nudge: Improving Decisions About health, Wealth, and Happiness. New Haven, CT: Yale University Press; 2008. pp. 53–72. [Google Scholar]
- Kuckmarzi RJ, Fanelli M, Najjar T. Effects of age on validity of self reported height, weight and Body Mass Index: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. J American Dietetic Association. 2001;101:28–34. doi: 10.1016/S0002-8223(01)00008-6. [DOI] [PubMed] [Google Scholar]