Abstract
Objective
To identify risk factors for inhospital mortality in patients with hip fractures using the Japanese Diagnosis Procedure Combination (DPC) nationwide administrative claims database.
Design
Retrospective observational study.
Setting
Hospitals adopting the DPC system during 2007–2009.
Participants
The authors analysed a total of 80 800 eligible patients aged ≥60 years with a single hip fracture (International Classification of Diseases, 10th Revision codes: S72.0 and S72.1). The DPC database includes patients treated between July and December each year.
Main outcome measures
Inhospital mortality after hip fracture.
Results
The overall inhospital mortality rate after hip fractures was 3.3%. Multivariate analysis indicated that inhospital mortality was significantly associated with male gender (OR 2.12, 95% CI 1.94 to 2.31), advancing age and number of comorbidities. Significantly higher mortality was observed in those treated conservatively (OR 4.25, 95% CI 3.92 to 4.61). Surgical delays of 5 days or more were significantly associated with higher rates of inhospital mortality (OR 1.34, 95% CI 1.20 to 1.50).
Conclusions
In patients with hip fractures, male gender, advancing age, high number of comorbidities, conservative treatment and the surgical delay of 5 days or more were associated with higher rates of inhospital mortality.
Article summary
Article focus
Hip fracture leads to impaired function, loss of independence and increased mortality of the patients.
The aim of this study was to identify risk factors for inhospital mortality in patients with hip fractures.
Key messages
Using the Japanese DPC nationwide administrative claims database, we analysed 80 800 hip fracture patients in total.
The overall inhospital mortality rate was 3.3%, and the inhospital mortality was significantly associated with male gender (OR 2.12 compared with female gender; p<0.001), advancing age (OR 1.57 in the 70–79 years age group, 2.28 in the 80–89 years age group and 3.51 in the ≥90 years age group compared with the 60–69 years age group; p<0.001), conservative treatment (OR 4.25 compared with the surgical treatment group; p<0.001) and number of comorbidities (OR 2.50 in patients with one comorbidity and 3.79 in those with two or more comorbidities compared with no comorbidity; p<0.001).
The proportion of patients with delay to surgery of 5 days or longer was 43.3%, and the delay was significantly associated with a higher rate of inhospital mortality (OR 1.34, 95% CI 1.20 to 1.50), while there was no significant difference in mortality among patients undergoing surgery within 4 days.
Strengths and limitations of this study
We analysed a large number of patients using the Japanese DPC administrative claims database, which included approximately 40% of all the inpatient admissions to acute care hospitals in Japan.
Complications occurring after admission are clearly differentiated with comorbidities that were already present at admission.
This is a retrospective observational study, and the database includes information only during the hospitalisation.
Introduction
Hip fracture is a serious injury related to bone fragility caused by osteoporosis, and it has emerged as a public health burden in an ageing society, such as that of Japan.1–5 It is estimated that the number of hip fractures worldwide will rise from 1.7 million in 1990 to 6.3 million in 2050.6 Recent studies have reported an increased incidence of hip fractures in Japan,3 5 although the incidence is decreasing in some Western countries.7 8 Hip fracture leads to impaired function, loss of independence and increased mortality of the patients. It has been reported that the increased mortality after hip fracture is associated with many factors, such as increasing age, comorbidity and prefracture functional disability of the patients.9–12 Hip fractures are usually treated by orthopaedic surgical procedures, such as hemiarthroplasty or internal fixation, and several studies have shown that early surgery is associated with lower rates of mortality,13–16 while other studies exhibited no benefit of early surgery in reducing mortality or improving functional recovery.17 18 Conservative treatment is often chosen for patients with severe comorbidities. However, it is not clear whether conservative treatment is actually superior in reducing mortality compared with surgical treatment in high-risk patients. In this study, we investigated the inhospital mortality rate of patients with hip fracture using data from the Japanese Diagnosis Procedure Combination (DPC) nationwide administrative claims database and compared mortality following hip fractures between groups treated surgically or conservatively.
Methods
DPC database
The DPC database is a diagnosis-dominant case-mix system administered by the Ministry of Health, Labour and Welfare of Japan, and linked with a lump-sum payment system.19 All 82 university teaching hospitals in Japan are obliged to adopt the DPC system, while adoption by community hospitals is voluntary. A comprehensive survey of the DPC hospitals is conducted between 1 July and 31 December each year by the DPC Research Group, funded by the Japanese government. Detailed patient data, as well as administrative claims data, are collected for all the inpatients discharged from the participating hospitals between 1 July and 31 December each year. The number of participating hospitals increased to 818 with 2.57 million patients in 2009, which represented approximately 40% of all the inpatient admissions to acute care hospitals in Japan. Hospitals send all the anonymised data for each month to the DPC Research Group for compilation in the database server in the Department of Health Management and Policy, the University of Tokyo.
The database includes the following data: hospital location; patients' age and sex; diagnoses, comorbidities at admission and complications after admission, recorded in accordance with the International Classification of Diseases, 10th Revision (ICD-10) codes and text data in the Japanese language; procedures coded with the Japanese original K codes; comorbidities at admission; complications after admission coded with the ICD-10 codes; inhospital mortality; length of stay and hospital charges.
This study was based on a secondary analysis of the administrative claims data. The requirement for informed consent was waived because of the anonymous nature of the data. Study approval was obtained from the institutional review board at the University of Occupational and Environmental Health.
Data compilation
We retrospectively collected data of patients coded S72.0 (fracture of the neck of the femur) and S72.1 (pertrochanteric fracture) between 2007 and 2009 from the DPC database. Exclusion criteria were as follows: age <60 years, patients with open fractures or multiple fractures and incomplete data. We extracted data on age, sex, method of treatment (surgical or conservative), number of acute beds and inhospital mortality. From the comorbidities at admission, we collected data on seven factors: malignancy, diabetes mellitus, cardiovascular disease, cerebrovascular disease, lung disease, renal failure and hepatic failure.
Statistical analysis
The χ2 test was used for univariate comparisons of the surgical and conservative treatment groups. Multivariate logistic regression analysis was performed to analyse the confounding effects of various factors on inhospital mortality. ORs and 95% CIs were determined. The OR of inhospital mortality in conservatively treated patients was analysed in subgroups of patients stratified according to the number of comorbidities or age. In addition, the effect of surgical delays in surgically treated patients was analysed. A p value <0.05 was considered significant. All the statistical analyses were performed using SPSS Statistics V.19.0 (IBM SPSS Inc.).
Results
Patient background
Data of 94 139 patients with hip fractures were extracted based on ICD-10 codes. We excluded 8956 patients with open fractures or multiple fractures, 496 patients with incomplete data and 3887 patients aged <60 years. Finally, 80 800 eligible patients were included in the analysis.
Table 1 presents the patients' characteristics. Overall, 79.1% were women. The mean (SD) age was 82.8 (8.3) years. The patients were categorised into the following four age groups: 60–69 years (n=5523), 70–79 years (n=18 618), 80–89 years (n=37 362) and ≥90 years (n=19 297). Approximately 83% (n=66 893) of patients underwent surgical treatment, while 17% (n=13 907) were treated conservatively. Hospital size was categorised into four groups according to the number of acute beds: ≤199 (13.9%), 200–399 (40.4%), 400–599 (28.6%) and ≥600 (15.0%). The proportion of patients with comorbidities at admission was as follows: malignancy (5.7%), diabetes mellitus (13.4%), cardiovascular disease (7.6%), cerebrovascular disease (8.0%), lung disease (6.4%), renal failure (4.4%) and hepatic failure (0.8%).
Table 1.
Patients' characteristics
| Characteristic | n (%) |
| Gender | |
| Females | 63 920 (79.1) |
| Males | 16 880 (20.9) |
| Age, years | |
| 60–69 | 5523 (6.8) |
| 70–79 | 18 618 (23.0) |
| 80–89 | 37 362 (46.2) |
| ≥90 | 19 297 (23.9) |
| Treatment | |
| Surgical | 66 893 (82.8) |
| Conservative | 13 907 (17.2) |
| Hospital size (number of acute beds) | |
| ≤199 | 11 243 (13.9) |
| 200–399 | 32 613 (40.4) |
| 400–599 | 23 125 (28.6) |
| ≥600 | 12 099 (15.0) |
| Comorbidities | |
| Malignancy | 4753 (5.7) |
| Diabetes mellitus | 10 795 (13.4) |
| Cardiovascular disease | 6147 (7.6) |
| Cerebrovascular disease | 6438 (8.0) |
| Lung disease | 5179 (6.4) |
| Renal failure | 3554 (4.4) |
| Hepatic failure | 646 (0.8) |
| Number of comorbidities | |
| 0 | 51 544 (63.8) |
| 1 | 22 170 (27.4) |
| ≥2 | 7086 (8.8) |
Univariate analysis of inhospital mortality
Table 2 shows the factors associated with inhospital mortality according to the univariate analysis. The overall inhospital mortality rate was 3.3% (n=2681), with the average length of stay of 38 days. Male gender, advancing age, conservative treatment and smaller hospital size were significantly associated with higher mortality. As for comorbidities, patients with malignancy, lung disease, renal failure and hepatic failure at admission exhibited higher mortality rates. In contrast, diabetes mellitus, cardiovascular disease or cerebrovascular disease did not significantly affect the mortality of the patients. The number of comorbidities at admission was positively related to the mortality rate.
Table 2.
Risk factors for inhospital mortality (univariate analysis)
| Inhospital mortality |
||
| n (%) | p Value | |
| Total | 2681 (3.3) | |
| Gender | ||
| Females | 1677 (2.6) | <0.001 |
| Males | 1004 (5.9) | |
| Age, years | ||
| 60–69 | 97 (1.8) | <0.001 |
| 70–79 | 488 (2.6) | |
| 80–89 | 1223 (3.3) | |
| ≥90 | 873 (4.5) | |
| Treatment | ||
| Surgical | 1372 (2.1) | <0.001 |
| Conservative | 1309 (9.4) | |
| Hospital size (number of acute beds) | ||
| ≤199 | 454 (4.0) | <0.001 |
| 200–399 | 1080 (3.3) | |
| 400–599 | 672 (2.9) | |
| ≥600 | 412 (3.4) | |
| Comorbidities | ||
| Malignancy | 669 (14.6) | <0.001 |
| Diabetes mellitus | 365 (3.4) | 0.694 |
| Cardiovascular disease | 198 (3.2) | 0.659 |
| Cerebrovascular disease | 215 (3.3) | 0.920 |
| Lung disease | 516 (10.0) | <0.001 |
| Renal failure | 305 (8.6) | <0.001 |
| Hepatic failure | 126 (19.5) | <0.001 |
| Number of comorbidities | ||
| 0 | 968 (1.9) | <0.001 |
| 1 | 1139 (5.1) | |
| ≥2 | 574 (8.1) | |
Multivariate analysis of inhospital mortality
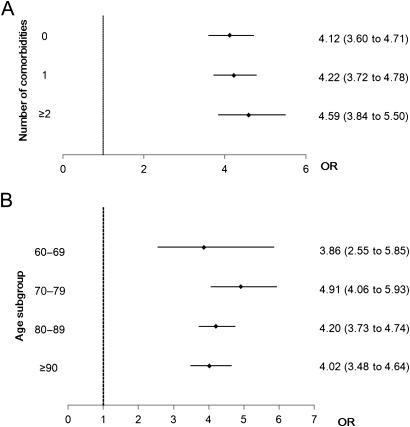
Table 3 shows the adjusted OR and 95% CI for inhospital mortality as determined by multivariate analysis. Consistent with the univariate analysis, the inhospital mortality was significantly associated with male gender (OR 2.12 compared with female gender; p<0.001), advancing age (OR 1.57 in the 70–79 years age group, 2.28 in the 80–89 years age group and 3.51 in the ≥90 years age group compared with the 60–69 years age group; p<0.001), conservative treatment (OR 4.25 compared with the surgical treatment group; p<0.001) and number of comorbidities (OR 2.50 in patients with one comorbidity and 3.79 in those with two or more comorbidities compared with no comorbidity; p<0.001). There was no association with hospital size. We then stratified the patients into the following three groups according to the number of comorbidities: no comorbidity (n=51 544), one comorbidity (n=22 170) and two or more comorbidities (n=7086). Regardless of the number of comorbidities, conservative treatment was significantly associated with higher mortality compared with surgical treatment (figure 1A). In addition, patients with conservative treatment exhibited higher mortality even when the patients were stratified according to age (figure 1B).
Table 3.
Risk factors for inhospital mortality (multivariate analysis)
| OR (95% CI) | p Value | |
| Gender | ||
| Females | Reference | |
| Males | 2.12 (1.94 to 2.31) | <0.001 |
| Age, years | ||
| 60–69 | Reference | |
| 70–79 | 1.57 (1.25 to 1.96) | <0.001 |
| 80–89 | 2.28 (1.84 to 2.82) | <0.001 |
| ≥90 | 3.51 (2.83 to 4.37) | <0.001 |
| Treatment | ||
| Surgical | Reference | |
| Conservative | 4.25 (3.92 to 4.61) | <0.001 |
| Hospital size (number of acute beds) | ||
| ≤199 | Reference | |
| 200–399 | 0.99 (0.88 to 1.11) | 0.814 |
| 400–599 | 0.88 (0.77 to 1.00) | 0.043 |
| ≥600 | 0.93 (0.81 to 1.07) | 0.304 |
| Number of comorbidities | ||
| 0 | Reference | |
| 1 | 2.50 (2.28 to 2.74) | <0.001 |
| ≥2 | 3.79 (3.38 to 4.24) | <0.001 |
Figure 1.
ORs of inhospital mortality and 95% CIs in conservatively treated patients with hip fracture. (A) Patients were stratified into three groups according to the number of comorbidities. (B) Patients were stratified into four groups according to age.
We finally analysed the effect of surgical delays on inhospital mortality in patients treated surgically. The proportion of patients with delay to surgery of 5 days or longer was 43.3%, and the delay was significantly associated with a higher rate of inhospital mortality (OR 1.34, 95% CI 1.20 to 1.50), while there was no significant difference in mortality among patients undergoing surgery within 4 days.
Discussion
Previous studies have reported that 3.6%–6.0% of patients with hip fractures die during hospitalisation9 20 and that the 1-year mortality rate is between 10.1% and 27.3%.12 21 The reasons for the high mortality rate after hip fracture have been extensively studied. Frost et al9 recently reported that men had a 2.4 times higher risk of inhospital death compared with women, and advancing age increased the risk by 2.06 times for every 10-year increase in age. Maggi et al22 reported that 6-month mortality was positively associated with increasing age, comorbidity, prefracture functional disability and having surgery more than 48 h after admission. Hu et al10 identified the following 12 preoperative predictors of postoperative mortality in patients with hip fracture through systematic review: advanced age, male gender, nursing home or facility residence, poor preoperative walking capacity, poor activities of daily living, higher ASA (American Society of Anesthesiologists) grading, poor mental state, multiple comorbidities, dementia or cognitive impairment, diabetes, cancer and cardiac disease.
In this study, we investigated the inhospital mortality rate after hip fractures using the Japanese DPC administrative claims database. The DPC database is equivalent in several ways to the Nationwide Inpatient Sample Database in the USA, but there is an advantage of the DPC database whereby complications occurring after admission are clearly differentiated with comorbidities that were already present at admission.
In our study, 83% of the patients underwent surgery and 17% were treated conservatively, which were similar rates to previous studies.21 The proportion of conservative treatment was higher than that in the Western countries, which may be due to the insurance system in Japan, which allows patients a longer hospital stay.
Overall, 3.3% of patients died during the hospitalisation. The mortality rate was slightly lower than that in previous reports. In multivariate analysis, we found that male gender, advancing age and number of comorbidities were positively and independently associated with the mortality, which is consistent with previous studies. The size of hospital as determined by the number of acute beds had no significant relationship with inhospital mortality in our study. This result may suggest that high-risk patients are not necessarily treated at large hospitals. Schilling et al20 reported that decreased hospital-wide nurse staffing levels are associated with increased inhospital mortality among patients with hip fracture. In contrast, Browne et al23 reported that hospital volume is not associated with decreased mortality in the treatment of hip fractures. There are various scales to represent hospital quality, so more studies may be needed to clarify the relationship between hospital quality and hip fracture mortality.
Interestingly, conservative treatment was an independent risk factor for inhospital mortality. The analysis indicated that this did not arise because of patients with higher risks being more likely to undergo conservative treatment, as patients treated conservatively exhibited more than four times higher risk for mortality even after stratification according to the number of comorbidities or age. The exact reason for the higher mortality in conservatively treated patients is unclear, but the patients treated surgically can start rehabilitation earlier and therefore avoid the complications caused by long-term bed rest, such as bedsores, venous thromboembolism, atelectasis and hypostatic pneumonia.
We found that surgical delays of 5 days or more were significantly associated with higher rates of inhospital mortality, which was consistent with the recent prospective cohort study by Vidan et al,15 showing that surgical delays longer than 5 days were associated with higher mortality and medical complication rates.
Our study has several limitations. First, this is a retrospective observational study. Thus, patient allocation was non-randomised, and the cohort of patients we analysed did not constitute random sampling. Consequently, our results are potentially biased due to unmeasured confounders. Second, the DPC-adopting hospitals are generally of large size, although the DPC database covered more than 40% of all inpatient admissions in Japan. Third, this database is for administrative claims, so recorded diagnoses may be less well validated than in planned prospective surveys. Finally, this database includes information only during the hospitalisation, and we were unable to determine the condition of patients before admission or after discharge. Despite these limitations, our study provides helpful information about the risk factors of inhospital mortality for treatment decision-making in patients with hip fractures.
Conclusion
This study has shown that male gender, advancing age, high number of comorbidities, conservative treatment and surgical delay were associated with higher rates of inhospital mortality in patients with hip fractures.
Supplementary Material
Footnotes
To cite: Shoda N, Yasunaga H, Horiguchi H, et al. Risk factors affecting inhospital mortality after hip fracture: retrospective analysis using the Japanese Diagnosis Procedure Combination Database. BMJ Open 2012;2:e000416. doi:10.1136/bmjopen-2011-000416
Contributors: NS, HY, HH and ST designed the study, analysed and interpreted the data and drafted the manuscript. YK contributed to the study design, analysis, and interpretation of the data. SM interpreted the data and made significant contributions to drafts of the manuscript. All authors had full access to all data (including statistical reports and tables) in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. NS, HY and ST are guarantors.
Funding: This study was supported in part by Grants-in-Aid for Research on Policy Planning and Evaluation from the Ministry of Health, Labour and Welfare, Japan; the Funding Program for World-Leading Innovative R&D on Science and Technology (FIRST program) from the Council for Science and Technology Policy, Japan; and a research grant from Japan Osteoporosis Foundation. The funding source was not involved in the design, conduct or interpretation of the study or in the writing of the submitted work. Grant numbers H22-Policy-031, 0301002001001.
Competing interests: None declared.
Ethics approval: Ethics approval was provided by the institutional review board at the University of Occupational and Environmental Health.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int 1997;7:407–13 [DOI] [PubMed] [Google Scholar]
- 2.Hagino H, Furukawa K, Fujiwara S, et al. Recent trends in the incidence and lifetime risk of hip fracture in Tottori, Japan. Osteoporos Int 2009;20:543–8 [DOI] [PubMed] [Google Scholar]
- 3.Hagino H, Sakamoto K, Harada A, et al. Nationwide one-decade survey of hip fractures in Japan. J Orthop Sci 2010;15:737–45 [DOI] [PubMed] [Google Scholar]
- 4.Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int 2004;15:897–902 [DOI] [PubMed] [Google Scholar]
- 5.Orimo H, Yaegashi Y, Onoda T, et al. Hip fracture incidence in Japan: estimates of new patients in 2007 and 20-year trends. Arch Osteoporos 2009;4:71–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sambrook P, Cooper C. Osteoporosis. Lancet 2006;367:2010–18 [DOI] [PubMed] [Google Scholar]
- 7.Abrahamsen B, Vestergaard P. Declining incidence of hip fractures and the extent of use of anti-osteoporotic therapy in Denmark 1997-2006. Osteoporos Int 2010;21:373–80 [DOI] [PubMed] [Google Scholar]
- 8.Leslie WD, O'Donnell S, Jean S, et al. Trends in hip fracture rates in Canada. JAMA 2009;302:883–9 [DOI] [PubMed] [Google Scholar]
- 9.Frost SA, Nguyen ND, Black DA, et al. Risk factors for in-hospital post-hip fracture mortality. Bone 2011;49:553–8 [DOI] [PubMed] [Google Scholar]
- 10.Hu F, Jiang C, Shen J, et al. Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury. Published Online First: 15 June 2011. doi:10.1016/j.injury.2011.05.017 [DOI] [PubMed] [Google Scholar]
- 11.Meyer HE, Tverdal A, Falch JA, et al. Factors associated with mortality after hip fracture. Osteoporos Int 2000;11:228–32 [DOI] [PubMed] [Google Scholar]
- 12.Panula J, Pihlajamaki H, Mattila VM, et al. Mortality and cause of death in hip fracture patients aged 65 or older: a population-based study. BMC Musculoskelet Disord 2011;12:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bottle A, Aylin P. Mortality associated with delay in operation after hip fracture: observational study. BMJ 2006;332:947–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gdalevich M, Cohen D, Yosef D, et al. Morbidity and mortality after hip fracture: the impact of operative delay. Arch Orthop Trauma Surg 2004;124:334–40 [DOI] [PubMed] [Google Scholar]
- 15.Vidan MT, Sanchez E, Gracia Y, et al. Causes and effects of surgical delay in patients with hip fracture: a cohort study. Ann Intern Med 2011;155:226–33 [DOI] [PubMed] [Google Scholar]
- 16.Simunovic N, Devereaux PJ, Sprague S, et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ 2010;182:1609–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Orosz GM, Magaziner J, Hannan EL, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA 2004;291:1738–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siegmeth AW, Gurusamy K, Parker MJ. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br 2005;87:1123–6 [DOI] [PubMed] [Google Scholar]
- 19.Matsuda S, Ishikawa KB, Kuwabara K, et al. Development and use of the Japanese case-mix system. Eurohealth 2009;14:25–30 [Google Scholar]
- 20.Schilling P, Goulet JA, Dougherty PJ. Do higher hospital-wide nurse staffing levels reduce in-hospital mortality in elderly patients with hip fractures: a pilot study. Clin Orthop Relat Res 2011;469:2932–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sakamoto K, Nakamura T, Hagino H, et al. Report on the Japanese Orthopaedic Association's 3-year project observing hip fractures at fixed-point hospitals. J Orthop Sci 2006;11:127–34 [DOI] [PubMed] [Google Scholar]
- 22.Maggi S, Siviero P, Wetle T, et al. A multicenter survey on profile of care for hip fracture: predictors of mortality and disability. Osteoporos Int 2010;21:223–31 [DOI] [PubMed] [Google Scholar]
- 23.Browne JA, Pietrobon R, Olson SA. Hip fracture outcomes: does surgeon or hospital volume really matter? J Trauma 2009;66:809–14 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.