Abstract
Influenza A viruses encoding an altered viral NS1 protein have emerged as promising live attenuated vaccine platforms. A carboxy-terminal truncation in the NS1 protein compromises its interferon antagonism activity, making these viruses attenuated in the host yet still able to induce protection from challenge with wild-type viruses. However, specific viral protein expression by NS1-truncated viruses is known to be decreased in infected cells. In this report, we show that recombinant H5N1 and H1N1 influenza viruses encoding a truncated NS1 protein expressed lower levels of hemagglutinin (HA) protein in infected cells than did wild-type viruses. This reduction in HA protein expression correlated with a reduction in HA mRNA levels in infected cells. NS1 truncation affected the expression of HA protein but not that of the nucleoprotein (NP). This segment specificity was mapped to the terminal sequences of their specific viral RNAs. Since the HA protein is the major immunogenic component in influenza virus vaccines, we sought to restore its expression levels in NS1-truncated viruses in order to improve their vaccine efficacy. For this purpose, we generated an NS1-truncated recombinant influenza A/Puerto Rico/8/34 (rPR8) virus carrying the G3A C8U “superpromoter” mutations in the HA genomic RNA segment. This strategy retained the attenuation properties of the recombinant virus but enhanced the expression level of HA protein in infected cells. Finally, mice immunized with rPR8 viruses encoding a truncated NS1 protein and carrying the G3A C8U mutations in the HA segment demonstrated enhanced protection from wild-type virus challenge over that for mice vaccinated with an rPR8 virus encoding the truncated NS1 protein alone.
INTRODUCTION
Vaccination remains the most effective way to protect against influenza virus infection. To date, two types of influenza virus vaccines are approved by the Food and Drug Administration for human use: inactivated split virus vaccines and live attenuated vaccines. Inactivated virus vaccines elicit protective immunity by inducing the production of neutralizing antibodies directed against the viral surface glycoproteins. On the other hand, live attenuated vaccines elicit virus-specific neutralizing antibodies as well as cross-reactive cell-mediated cytotoxicity against heterotypic influenza virus strains (12, 13). A clinical trial comparing these two forms of vaccination in young children demonstrated that the live attenuated vaccine had significantly better efficacy against antigenically well matched and drifted viruses than the inactivated vaccine (2).
Our group has previously developed influenza viruses expressing altered nonstructural protein 1 (NS1) as live attenuated viral vaccine candidates (31). NS1 is the main factor by which influenza viruses antagonize the host immune response (10). Influenza viruses encoding altered NS1 proteins have been shown to be highly attenuated but are still able to induce a protective immune response in mice, swine, equines, macaques, and poultry (1, 27, 29, 30), most likely due to their ability to stimulate dendritic cells (19).
The NS1 protein of influenza viruses has been extensively implicated in the inhibition of the type I interferon (IFN) response in infected cells (10, 14, 15). However, NS1 has also been associated with numerous IFN-independent activities, such as temporal regulation of viral RNA synthesis (7, 33), enhancement of viral mRNA translation, and control of viral mRNA splicing (6, 11). Previous studies employing NS1-truncated influenza viruses found reductions in the expression of specific viral proteins, such as hemagglutinin (HA) and matrix protein (M1), from that by wild-type virus (29, 30).
Concerns about the safety of live attenuated viral vaccines might be addressed either by further attenuating the viral vector, rendering the vaccine construct replication incompetent, or increasing immunogenicity so that lower doses of the vaccine can be administered while its protective effect is preserved. In this study, we examine the impact of the NS1 protein on viral protein expression in the context of NS1-truncated influenza viruses. We observe that cells infected with NS1-truncated viruses contain smaller amounts of HA protein and lower HA mRNA levels than wild-type viruses. Since the HA protein is an important constituent of influenza virus vaccines, an influenza A/Puerto Rico/8/34 (PR8) virus expressing C-terminally truncated NS1 (NS1 1-73) and the G3A C8U “superpromoter” mutations in the HA genomic segment was generated. This strategy rescued HA protein expression levels in infected cells while still retaining the growth attenuation observed for viruses with truncated NS1. More importantly, this increase in the level of HA expression enhanced the ability of the NS1-truncated virus to induce a protective anti-influenza virus immune response in mice.
MATERIALS AND METHODS
Cells.
293T, A549, and Vero cells and chicken embryo fibroblasts (CEF) were maintained in Dulbecco's modified Eagle's medium supplemented with 10% fetal calf serum (HyClone). Madin-Darby canine kidney (MDCK) cells and MDCK-HA cells, which stably express WSN influenza virus hemagglutinin (HA) protein (23), were maintained in modified Eagle's medium supplemented with 10% fetal calf serum (Gibco). All cells were maintained at 37°C under 5% CO2.
Generation of recombinant influenza viruses and virus propagation.
Recombinant A/Viet Nam/1203/04 (rVN1203) (H5N1) HALo influenza viruses encoding wild-type NS1 or a truncated protein (NS1 1-73) were generated using reverse genetics as described previously (30). These viruses had the wild-type HA multibasic cleavage site, associated with high pathogenicity, replaced by that of an influenza virus of low pathogenicity. A/Puerto Rico/8/34 (H1N1) (PR8) virus encoding wild-type NS1 or a truncated NS1 protein (NS1 1-73, NS1 1-113, or NS1 1-126) was generated by reverse genetics as described previously (31). A PR8 virus encoding a truncated NS1 protein and carrying a G38 C8U “superpromoter” in the HA segment was rescued using a helper virus, since we were unsuccessful in rescuing this virus using the plasmid rescue method. To generate the helper virus PR8-RFP-NS1 1-73 (a PR8 virus that expresses red fluorescent protein [RFP] instead of HA and expresses a truncated form of its NS1 protein), 0.5 μg of pDZ plasmids (27), encoding PR8 PB1, PB2, PA, neuraminidase (NA), nucleoprotein (NP), matrix protein (M), mutant NS (expressing truncated NS1 1-73 and a wild-type nuclear export protein [NEP]), and RFP flanked by the HA packaging sequences, was transfected into HEK 293T cells. Twenty-four hours later, the supernatant was used to infect MDCK-HA cells. PR8-RFP-NS1 1-73 was further passaged three times in MDCK cells expressing HA and was plaque purified. To rescue PR8 virus encoding the 1-73 NS1 truncation and carrying the G3A C8U superpromoter in the HA segment (S73), 293T cells were transfected with 4 μg of a PDZ plasmid encoding the PR8 HA segment with G3A C8U mutations in the promoter (pDZ-sHA). Eight hours after transfection, cells were infected with the helper virus PR8-RFP-NS1 1-73 at a multiplicity of infection (MOI) of 1. Twenty-four hours postinfection, the supernatants containing the transfectant virus were inoculated into 10-day-old embryonated eggs. Two days postinoculation, the allantoic fluid was harvested, and the virus was plaque purified on MDCK cells and sequenced.
All viral stocks were grown in 10-day-old embryonated chicken eggs, and the titers were determined by plaque assays on MDCK cells.
Growth kinetics of virus in 10-day-old embryonated chicken eggs.
Ten-day-old embryonated chicken eggs were inoculated with recombinant PR8-derived viruses. Allantoic fluid was harvested and was subsequently assayed for viral growth at 0, 24, 48, and 72 h postinfection (hpi). The titer of virus present in allantoic fluid was determined by a plaque assay on MDCK cells.
Determination of the MLD50 of challenge virus.
Groups of six to eight week-old female BALB/c mice (Charles River Laboratories) were anesthetized with a ketamine-xylazine mixture and were then inoculated intranasally (n = 4) with 102, 103, 104, 105, or 106 PFU of PR8 in 50 μl of phosphate-buffered saline (PBS). Animals were monitored daily for mortality, weight loss, or other signs of disease over a 2-week period. Animals were sacrificed and were scored as dead if they had lost more than 25% of their initial body weight. Fifty percent mouse lethal dose (MLD50) values were calculated by the method of Reed and Muench (28).
Immunization and infection in mice.
Six- to 8-week-old BALB/c mice (Charles River Laboratories) were first anesthetized and then inoculated intranasally (n = 5) with 10 or 102 PFU of either PR8 NS1 1-73 or S73 in 50 μl of PBS. Negative-control mice were inoculated with 50 μl of PBS, whereas positive-control mice were inoculated with 10 PFU of wild-type PR8 virus. Mice were monitored daily for weight loss or other signs of disease over a 2-week period. Vaccinated mice were challenged 3 weeks postvaccination with 100 MLD50s of wild-type PR8 virus by the intranasal route and were monitored daily for weight loss or other signs of disease over a 2-week period. Additionally, sera were obtained from selected animals at 3 weeks postvaccination.
Purification of virions by a sucrose gradient.
Ten-day-old embryonated chicken eggs were infected with 100 PFU of either wild-type PR8 virus, rVN1203 HALo virus, or rVN1203 HALo NS1 1-73 virus. At 40 to 48 h postinfection, the supernatant was harvested and clarified (at 2,600 × g for 5 min at 4°C in a Sorvall RT6000D centrifuge). The clarified supernatant was layered over a 20% sucrose cushion in NTE buffer (100 mM NaCl, 10 mM Tris-Cl [pH 7.4], 1 mM EDTA), and the virus was concentrated by ultracentrifugation (at 112,600 × g for 2 h at 4°C in an SW28 rotor [Beckman Coulter, Fullerton, CA]). The concentrated virus was purified over a 30-to-60% sucrose gradient (at 112,600 × g for 3 h at 4°C), and the banded virus was then collected, diluted with NTE buffer, pelleted (at 112,600 × g for 90 min at 4°C), and resuspended in approximately 1 ml of NTE buffer.
ELISA.
Three weeks after vaccination, mice were bled, and serum was separated from red blood cells by a 15-min spin at 13,000 × g in a microcentrifuge. Sera were stored at −20°C until the enzyme-linked immunosorbent assay (ELISA) was performed. Wells of ELISA plates were coated with 50 μl of sucrose gradient-purified PR8 virus at a concentration of 2 μg per ml, and the plates were incubated overnight at 4°C. The plates were then incubated with blocking buffer (1% bovine serum albumin [BSA] in PBS) for 1 h at room temperature, washed with an autoplate washer, and incubated with 50 μl of serial dilutions of sera for 1 h at 37°C. After three washing steps, the plates were incubated for 60 min with 50 μl/well of 1:500 dilutions of alkaline phosphatase-linked secondary antibodies against mouse IgG (Zymed) at room temperature. The plates were then washed and incubated with a substrate (p-nitrophenyl phosphate [PNPP] substrate for alkaline phosphatase; Zymed) for 30 min at room temperature. The reaction was stopped with 50 μl of 0.75 N NaOH per well, and the plates were read at 405 nm in a plate reader.
Primer extension analysis.
Total RNA was harvested from infected cells using an RNeasy minikit (Qiagen). Five micrograms of RNA was subsequently used in a primer extension assay using avian myeloblastosis virus (AMV) reverse transcriptase (Promega) according to the manufacturer's instructions. The following primers were used: for HA mRNA/cRNA, GGTAACCAATGCAAATCTGATCAC; for HA viral RNA (vRNA), CCCTAGCACTGGCAATCATGG; for NP mRNA/cRNA, CAGTAGCATTCTGGCGTTCC; for NP vRNA, GAGGGCAGAACGTCTGACATG; and for 5S rRNA, ACCAGGCCCGACCCTGCTTA.
Transcription products were analyzed on 8% polyacrylamide gels containing 7 M urea in Tris-borate-EDTA (TBE) buffer and were detected by autoradiography.
Protein analysis.
Cell lysates and sucrose-purified virions were analyzed by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) followed by Western blotting. The H5 hemagglutinin was detected using a monoclonal antibody specific for H5 HA (anti-HALo) (30). The PR8 hemagglutinin was detected using a monoclonal antibody specific for PR8 HA (anti-PR8 HA). NP was detected using a rabbit polyclonal antibody raised against influenza virus NP (anti-NP). NS1 protein was detected using a monoclonal antibody specific for the NS1 protein (anti-NS1; 1A7), and the NEP was detected using a polyclonal antibody recognizing influenza virus NEP (anti-NEP) (31). The following monoclonal antibodies were also used: anti-β-actin (Sigma), anti-green fluorescent protein (anti-GFP) (Abcam), and anti-RFP (Cell Biolabs).
Generation of the pPol I-NP-GFP-NP and pPol I-HA-RFP-HA constructs.
The pPol I vector was derived from the ambisense pDZ plasmid by removing the pPol-II promoter (27). pPOL-I NP-GFP-NP was made by first flanking the enhanced GFP (EGFP) gene (Clontech) with the 3′ 171 nucleotides (nt) and 5′ 145 nt of the NP packaging sequences and then inserting this construct into the pPol-I vector. All the ATG codons upstream of the EGFP start codon were mutated to TTG codons by site-directed mutagenesis. pPol-I HA-RFP-HA was derived from the pDZ HA-NSmut-HA plasmid by subcloning the RFP gene in place of the original NS open reading frame (ORF) and also removing the pPOL-II promoter (4, 9).
Minigenome reporter assay.
Human embryo kidney 293T cells were transfected with 4 μg of plasmid DNA by using Lipofectamine 2000 (Invitrogen). The plasmids used were pCAGGS-PB1, pCAGGS-PB2, pCAGGS-PA, pCAGGS-NP, pCAGGS-NS1(PR8), an empty pCAGGS vector (3, 30), and pPol I-NP-GFP-NP and pPol I-HA-RFP-HA. The polymerase and nucleoprotein plasmids (total, 1.2 μg) were used at an NP/PB1/PB2/PA ratio of 10:2:1:2. A total of 0.6 μg each of pCAGGS-NS1, pPol-I NP-GFP-NP, and pPoL-I HA-RFP-HA was used. The amount of DNA transfected was kept constant at 4 μg by transfecting the empty pCAGGS plasmid. Eighteen hours posttransfection, the cells were lysed, and a Western blot assay was used to determine the levels of RFP, GFP, and NS1.
Statistical analysis.
To assess statistical differences, a one-tailed unpaired Student t test was used. Welch's correction was applied when variances were calculated to be statistically different. All analysis was performed in Prism4 (GraphPad Software).
RESULTS
Levels of the HA protein are reduced in influenza viruses expressing a truncated NS1 protein.
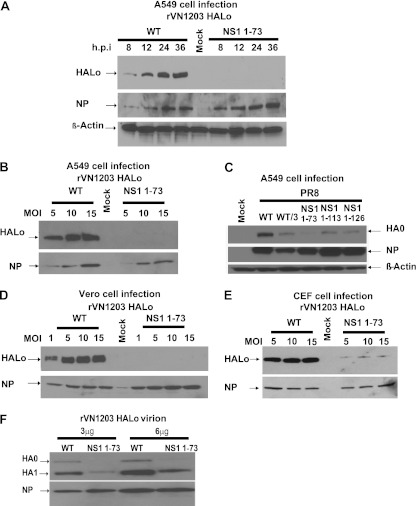
To determine the effect of NS1 truncation on the expression levels of the HA protein, A549 cells were infected with rVN1203 HALo encoding either a wild-type or a truncated (NS1 1-73) NS1 protein at an MOI of 1. At different time points after infection, HA and NP levels were determined by Western blot assays (Fig. 1A). There were no major differences in NP levels between cells infected with the different viruses; however, cells infected with the NS1-truncated virus exhibited HA protein levels significantly lower than those in wild-type-infected cells (Fig. 1A). HA expression levels in cells infected with the NS1-truncated virus were below the limit of detection by Western blotting (Fig. 1A). To find out whether the reduction in HA protein levels could still be observed at a high MOI, A549 cells were infected with increasing MOIs of rVN1203 HALo viruses encoding either a wild-type or a truncated NS1 protein (Fig. 1B). Twelve hours after infection, the level of HA protein expressed in cells infected with the NS1-truncated virus was significantly lower than that in cells infected with the wild-type virus at an MOI as high as 15 (Fig. 1B). In order to ensure that the phenotype observed is not strain and/or HA subtype specific, A549 cells were infected with a PR8 virus (A/Puerto Rico/8/34 H1N1) encoding either a wild-type or a truncated (NS1 1-73, NS1 1-113, or NS1 1-126) NS1 protein (31) (Fig. 1C). Twelve hours postinfection, cells infected with the NS1-truncated viruses displayed reductions of at least 3-fold in HA protein expression levels, as evidenced by the fact that cells infected with wild-type PR8 virus displayed more HA protein even when diluted three times in lysates from mock-infected cells (WT/3) (Fig. 1C).
Fig 1.
HA and NP levels in infected cells and purified virions. (A) A549 cells were infected at an MOI of 1 with either wild-type (WT) rVN1203 HALo virus or rVN1203 HALo virus encoding a truncated NS1 protein (NS1 1-73). Eight, 12, 24, and 36 h after infection, Western blotting was performed to detect HA, NP, and actin levels. (B) A549 cells were infected with either WT rVN1203 HALo virus or rVN1203 HALo NS1 1-73 virus at the indicated MOI. Twelve hours postinfection, Western blotting was performed to detect the levels of HA and NP. (C) A549 cells were infected with either WT PR8, PR8 NS1 1-73, PR8 NS1 1-113, or PR8 NS1 1-126. Twelve hours postinfection, Western blotting was performed to detect the levels of HA, NP, and actin. (D and E) Vero cells (D) and CEF (E) were either mock infected or infected with a virus at the indicated MOI. Twelve hours postinfection, Western blotting was performed to detect the levels of HA and NP. (F) Western blot showing the levels of HA and NP in sucrose gradient-purified virions. HA0, uncleaved HA protein; HA1, HA1 subunit of cleaved HA protein.
The NS1 protein of influenza viruses is a multifunctional protein with a prominent role in counteracting the host IFN response (13, 15, 16). Influenza viruses encoding a truncated NS1 protein have been shown previously to be highly attenuated for replication, except in IFN-deficient cells, such as Vero cells (10). In order to determine whether the reduction in HA protein levels in cells infected with NS1-truncated viruses is directly related to the inability of these viruses to antagonize the IFN-α/β-dependent responses, Vero cells were infected with increasing MOIs of rVN1203 HALo viruses encoding either a wild-type or a truncated NS1 protein (Fig. 1D). At 12 h postinfection, HA protein levels were still lower in Vero cells infected with an NS1-truncated virus than in cells infected with a wild-type NS1 virus (Fig. 1D). To test if the observed phenotype is specific to cells of mammalian origin, we used primary chicken embryo fibroblasts (CEF). When CEF were infected with viruses with either wild-type or truncated NS1 at increasing MOIs, HA protein levels at 12 h postinfection were significantly lower in cells infected with the NS1-truncated virus (Fig. 1E). We next investigated the HA protein levels in a suspension of egg-grown, sucrose gradient-purified rVN1203 HALo virions. As shown in Fig. 1F, at similar amounts of NP, purified rVN1203 HALo virus encoding a truncated NS1 protein exhibited a smaller amount of HA protein than rVN1203 HALo encoding wild-type NS1.
HA mRNA levels are reduced in cells infected with an rVN1203 HALo virus expressing a truncated NS1 protein.
Cells infected with influenza viruses contain three types of virus-specific RNA. Two are RNAs of positive polarity, of which the first is capped and polyadenylated and functions as an mRNA, while the second is noncapped and nonpolyadenylated (cRNA) and serves as a template for the synthesis of the third type of virus-specific RNA (vRNA), which is of negative polarity (24). The NS1 protein has been shown to be involved in viral RNA replication and translation; temperature-sensitive mutations in the NS gene reduced vRNA levels in infected cells, and the temporal regulation of vRNA synthesis was affected in NS1 mutant viruses (15, 33). In addition, NS1 has been shown to interact with the 5′ untranslated region (5′ UTR) of viral mRNAs, enhancing their translation (6). The NS1 protein has also been shown to interact with the viral polymerase complex (22). In order to investigate the effect of NS1 truncation on the replication of HA and NP RNAs, Vero and A549 cells (Fig. 2A and B) were infected with rVN1203 HALo virus encoding either a wild-type or a truncated NS1 protein. Two, 4, 8, and 12 h postinfection, total RNA was harvested and was used in a primer extension assay to quantify vRNA, cRNA, and mRNA levels for both the HA and the NP segment. In both cell types, truncation of the NS1 protein did not affect NP mRNA levels; however, HA mRNA levels were substantially reduced in cells infected with the NS1-truncated virus (Fig. 2A and B). HA cRNA levels were also reduced in cells infected with the NS1-truncated virus. In contrast, both HA and NP vRNA levels were slightly higher in cells infected with the NS1-truncated virus (Fig. 2A and B).
Fig 2.
HA and NP RNA levels in infected cells. Vero (A) and A549 (B) cells were either mock infected (M) or infected with either wild-type (WT) rVN1203 HALo or rVN1203 HALo NS1 1-73 virus at an MOI of 5. At the indicated time points, total RNA was harvested and was subjected to primer extension analysis.
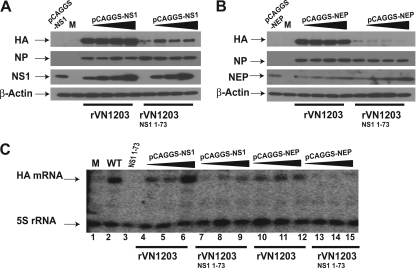
Expression of NS1 in trans rescues HA protein and mRNA expression from NS1-truncated viruses.
Since a carboxy-terminal truncation of the NS1 protein reduced the amount of HA protein and mRNA in the context of a viral infection, we next investigated whether expression of the full NS1 protein in trans could rescue HA protein and mRNA levels in NS1-truncated virus-infected cells. HEK 293T cells were transfected with increasing amounts of a plasmid encoding either the full NS1 protein or NEP as a control. Cells were later infected with rVN1203 HALo virus encoding either a wild-type or a truncated NS1 protein. As shown in Fig. 3A, overexpression of the NS1 protein did increase the levels of HA protein in cells infected with rVN1203 HALo NS1 1-73, as well as in cells infected with the wild-type virus. In contrast, overexpression of NEP did not increase HA protein levels in infected cells (Fig. 3B). In order to correlate the increase in HA protein expression with HA mRNA levels, total RNA was harvested and was used in a primer extension assay to detect HA-specific mRNA (Fig. 3C). As expected, overexpression of NS1 but not NEP increased HA mRNA levels in cells infected with the NS1-truncated virus (Fig. 3C, compare lane 3 to lanes 7 to 9 and lanes 13 to 15).
Fig 3.
Expression of NS1 protein in trans increases HA protein and mRNA expression in infected cells. (A and B) HEK 293T cells were transfected with increasing amounts of a plasmid (1 μg, 2 μg, or 3 μg) encoding PR8 NS1 protein (pCAGGS-NS1) (A) or PR8 NEP (pCAGGS-NEP) (B). The amount of DNA transfected was kept constant at 4 μg by transfecting a plasmid encoding GFP (pCAGGS-GFP) as filler. Eight hours posttransfection, cells were infected with either rVN1203 HALo or rVN1203 HALo NS1 1-73 at an MOI of 2. (A and B) Twelve hours postinfection, cell lysates were harvested and were used in a Western blot assay to detect the levels of HA, NP, NS1, NEP, and actin. M, mock infection. (C) The same HEK 293T cell lysates used for the HA protein expression experiments (for which results are shown in panels A and B) were used for RNA extraction and primer extension analysis to detect the levels of HA mRNA. 5S rRNA was used as a loading control. Cells were transfected with pCAGGS-NS1 (lanes 4 to 9) or pCAGGS-NEP (lanes 10 to 15). Lane 1, mock-infected cells; lanes 2, 4 to 6, and 10 to 12, cells infected with the wild-type (WT) rVN1203 HALo virus; lanes 3, 7 to 9, and 13 to 15, cells infected with the rVN1203 HALo NS1 1-73 virus.
Taken together, C-terminal truncation of the NS1 protein reduced the protein and mRNA levels of the HA but not the NP gene in infected cells, and this reduction was rescued when the NS1 protein was supplied in trans.
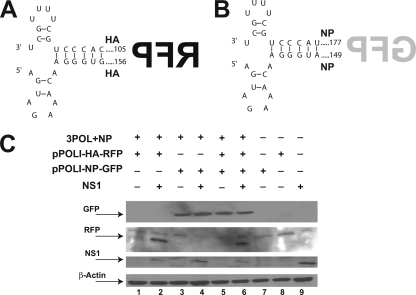
The NS1 protein affects the expression of influenza virus genes with HA terminal sequences but not NP terminal sequences.
The influenza virus genomic RNA possesses segment-specific RNA packaging signals that include both the 3′ and 5′ noncoding regions (NCRs), as well as adjacent terminal sequences, which are coding sequences at the two ends of each open reading frame (ORF) (9). In order to investigate the role of these terminal sequences in the observed NS1-dependent segment-specific phenotype (HA versus NP), we generated plasmid DNA-based constructs where the RFP open reading frame and the GFP open reading frame were flanked by the terminal sequences of HA and NP, respectively (Fig. 4A and B). These constructs were under the control of the polymerase I promoter and were cloned upstream of the 3′ NCR in order to generate negative-sense vRNA upon transfection into cells (Fig. 4A and B). Thus, GFP and RFP would be expressed only when the three influenza virus polymerases (PB1, PB2, and PA) as well as the NP were supplied in trans (Fig. 4C, lanes 7 and 8). The expression of the GFP gene, which is flanked by the NP terminal sequences, was not affected by the presence or absence of the NS1 protein (Fig. 4C lanes 3 and 4). However, there was little RFP expression in the absence of the NS1 protein. Interestingly, when the latter protein was supplied in trans, RFP expression increased significantly (Fig. 4C, lanes 1 and 2). In addition, when both the GFP and RFP constructs were transfected together, the expression of the NS1 protein correlated with an increase in the expression of RFP but not of GFP (Fig. 4C, lanes 5 and 6). These observations implicate the HA terminal sequences in the segment-specific gene regulation by the NS1 protein.
Fig 4.
NS1 protein affects the expression of genes with HA terminal sequences but not NP terminal sequences. (A and B) Schematic representations of the negative-sense RNA encoding RFP flanked by HA terminal sequences (A) and GFP flanked by NP terminal sequences (B). (C) Western blot showing GFP and RFP levels in transfected HEK 293T cells in the presence or absence of NS1 expression.
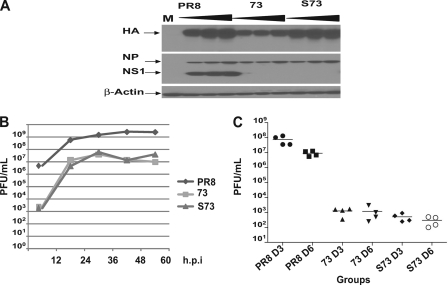
G3A C8U “superpromoter” mutations in the HA segment increase the expression of HA protein in NS1-truncated virus-infected cells while maintaining virus attenuation.
Recombinant influenza viruses expressing a truncated NS1 protein are promising live attenuated vaccine candidates, since they elicit a mucosal humoral and cell-mediated immune response (8, 31). Since the HA protein of influenza virus is one of the major immunogens of influenza virus vaccines, and since the expression of this protein is reduced in NS1-truncated viruses, we sought to generate a live NS1-truncated virus vaccine that restores HA expression to wild-type levels without increasing the virulence of the virus. Previous studies have demonstrated that the mutation of two nucleotides (G3A C8U) in the promoter region of an influenza A virus segment enhanced reporter gene expression in an influenza virus minigenome assay (26). Therefore, we rescued an influenza A/Puerto Rico/8/34 (H1N1) virus carrying the G3A C8U mutations in the HA segment and encoding a truncated NS1 protein (S73 virus [see Materials and Methods]). Cells infected with this virus had HA protein expression levels comparable to those of cells infected with wild-type PR8 virus (Fig. 5A). The replication of NS1-truncated viruses has been shown previously to be attenuated in IFN-competent systems (10). To determine whether the S73 virus is still attenuated, 10-day-old embryonated chicken eggs were infected with 100 PFU of the PR8, PR8 NS1 1-73, or S73 virus. At different time points after inoculation, allantoic fluid was harvested, and virus titers were determined (Fig. 5B). The S73 virus displayed growth kinetics similar to those of the PR8 NS1 1-73 virus: both exhibited significantly attenuated growth patterns compared to those of the wild-type virus (Fig. 5B). In order to determine whether the S73 virus was also attenuated in an animal model, mice were infected intranasally with 103 PFU of wild-type PR8 virus or with 106 PFU of either the PR8 NS1 1-73 or the S73 virus. At day 3 and day 6 postinfection, lungs were harvested, and viral titers were determined by plaque assays on MDCK cells (Fig. 5C). The two NS1-truncated viruses displayed similar growth kinetics in mice, and their growth was significantly attenuated compared to that of a wild-type PR8 virus (Fig. 5C).
Fig 5.
Phenotype of an NS1-truncated PR8 virus encoding G3A C8U “superpromoter” mutations in its HA segment. (A) A549 cells were infected with increasing MOIs (1, 3, and 5) of either wild-type PR8, PR8 NS1 1-73 (73), or PR8 NS1 1-73 containing G3A C8U mutations in the HA segment (S73). Twelve hours postinfection, cell lysates were harvested and were used in a Western blot assay to detect the levels of HA, NP, NS1, and actin protein. Note that the exposure of the HA blot here is longer than that in Fig. 1C. (B) Ten-day-old embryonated chicken eggs were inoculated with 100 PFU of the indicated viruses. At the indicated hours postinfection (hpi), allantoic fluids were harvested, and virus titers were determined by plaque assays on MDCK cells. (C) Mice were infected with 103 PFU of wild-type PR8 or with 106 PFU of either S73 or PR8 NS1 1-73 (73) virus. At day 3 (D3) and D6 postinfection, viral lung titers were determined for each group (4 mice per group).
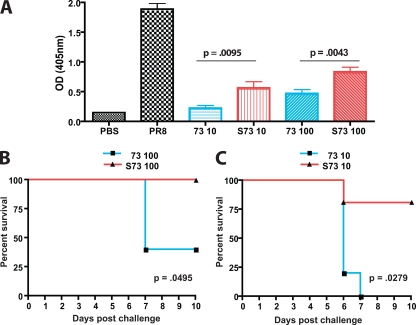
Vaccination of mice with NS1-truncated viruses carrying a “superpromoter” in the HA segment confers enhanced anti-influenza virus serum titers and improved survival following challenge.
Previous studies have demonstrated that influenza viruses encoding a C-terminally truncated NS1 protein are nonpathogenic in mice and can elicit a protective immune response after influenza virus challenge (27, 30, 30, 31). In this study, we investigated whether increased HA protein expression in the context of an NS1-truncated virus offers a protective advantage for mice. Mice either were immunized with various doses (10 or 100 PFU) of the S73 or PR8 NS1 1-73 virus or were inoculated with 10 PFU of wild-type PR8 virus as a positive control or with PBS as a negative control. Three weeks postimmunization, serum from mice vaccinated with the S73 virus displayed significantly more anti-influenza virus antibodies than serum from mice immunized with the PR8 NS1 1-73 virus (Fig. 6A). As expected, mice inoculated with wild-type PR8 virus presented the largest amount of virus-specific antibodies, reflecting the increased replication (lack of attenuation) of the wild-type virus; however, despite similar levels of replication for the PR8 NS1 1-73 and S73 viruses in mice (Fig. 5C), only 10 PFU of the S73 virus was needed to induce an antibody response similar to that induced by 100 PFU of the PR8 NS1 1-73 virus (Fig. 6A). The levels of antibody against a purified PR8 HA protein in the sera of mice vaccinated with the S73 virus were also higher than those for mice vaccinated with the PR8 NS1 1-73 virus (data not shown). Mice were subsequently challenged with 100 MLD50s of wild-type PR8 virus. All mice vaccinated with wild-type PR8 virus survived the challenge and did not lose weight (data not shown). However, we observed significant differences in survival between mice vaccinated with the different NS1-truncated viruses (Fig. 6B and C). All mice vaccinated with 100 PFU of the S73 virus survived the viral challenge, compared to only 40% of the mice vaccinated with the same dose of the PR8 NS1 1-73 virus (73) (Fig. 6B). In addition, vaccination with 10 PFU of the S73 virus resulted in an 80% survival rate, whereas none of the mice vaccinated with the same dose of PR8 NS1 1-73 virus survived the challenge (Fig. 6C).
Fig 6.
Vaccination of mice with NS1-truncated viruses encoding a “superpromoter” in the HA segment confers enhanced serum anti-influenza virus titers and improved survival following challenge. Mice (5 per group) were vaccinated with 10 PFU or 100 PFU of either the PR8 NS1 1-73 virus (73) or the PR8 NS1 1-73 virus encoding the G3A C8U mutations in the HA segment (S73). Positive-control mice were vaccinated with 10 PFU of the wild-type PR8 virus. Negative-control mice were immunized with PBS. Three weeks postvaccination, mice were bled; then they were challenged with 100 MLD50s of the wild-type PR8 virus. (A) Serum anti-influenza virus antibody titers 3 weeks postvaccination. Shown is the average titer (with the standard error) for 5 mice per group at a 1/800 dilution of the sera. OD, optical density. (B and C) Survival curves of mice vaccinated with 100 PFU (B) or 10 PFU (C) of the indicated viruses and challenged with 100 MLD50s of wild-type PR8 virus 3 weeks postimmunization.
DISCUSSION
The activation of the type I IFN system constitutes one of the earliest and most effective defense mechanisms mounted by the host to limit the proliferation of invading viruses (20). However, in order to establish an effective infection, viruses encode products that interfere with the IFN action of the host cell, allowing the viruses to survive and replicate. The NS1 protein of influenza A viruses has been consistently implicated in antagonizing the host IFN response (15). In light of these observations, we and others have generated influenza viruses encoding altered NS1 proteins as promising live attenuated influenza virus vaccines (30–32). These viruses have been proven to be highly attenuated yet still able to provide a potent influenza virus-specific protective immune response.
In this study, we first examined the impact of a truncated NS1 (NS1 1-73) protein on the expression of the HA protein in the context of virus infection. Our results indicate that cells infected with NS1-truncated viruses express lower levels of HA proteins than do wild-type virus-infected cells (Fig. 1). The reduction of HA protein expression is not the consequence of the attenuated capacity of NS1-truncated viruses to replicate, since the levels of NP (Fig. 1) and PB1 (data not shown) were comparable for cells infected with the wild-type virus versus the NS1-truncated viruses. Since this phenotype cannot be rescued in an IFN deficient system, such as Vero cells (Fig. 1D) (6), we conclude that the reduction of HA protein expression is not related to the inability of the truncated NS1 protein to counteract the IFN response. However, we cannot exclude a possible role for other cellular stress responses that may be antagonized by a wild-type NS1 protein.
The C-terminal truncation of the NS1 protein induced a reduction in the expression levels of the HA protein in transformed mammalian cell lines, in primary chicken embryonic cells, and in sucrose-purified virus (Fig. 1). This phenotype has also been observed in a previous study employing A/Swine/Texas/4199-2/98 influenza viruses encoding truncated NS1 proteins (29) and in numerous other studies employing temperature-sensitive viruses with mutations in the NS1 gene (7, 16, 33). These observations implicate the NS1 protein of influenza virus in the regulation of the expression of specific viral genes.
The NS1 protein has been shown previously to interact with the viral RNA replication/transcription complex; in addition, NS1 protein exhibits binding to influenza virus vRNA (17, 18, 22). Our results reveal that the C-terminal domain of the NS1 protein is required during infection for the efficient transcription of the HA gene; however, the transcription of the NP gene seems to be less affected (Fig. 2). In addition, HA protein and mRNA expression levels in cells infected with an NS1-truncated virus were increased by supplying the NS1 protein in trans (Fig. 3). These observations indicate that the NS1 protein regulates the transcription of viral RNA in a segment-specific manner. Our results are in agreement with a previous study by Ludwig et al. where a temperature-sensitive influenza virus resulting from a point mutation in the NS1 gene exhibited reduced amounts of HA mRNA at the restrictive temperature, whereas the NP mRNA levels were less affected (21). However, not all temperature-sensitive mutations in the NS1 gene induce a transcriptional block; different phenotypes have been observed in a number of studies for different mutants, ranging from a decrease in HA and M vRNA replication to various blocks in posttranscriptional processes affecting mostly late gene expression (HA and M) 7, 16, 33). In addition, Min et al. demonstrated that a mutant NS1 protein that is incapable of binding the protein kinase R (PKR) protein enhanced viral RNA synthesis at early time points after infection (25). Our results also indicate that a C-terminal truncation in the NS1 protein slightly increased the vRNA levels of the HA and NP segments in infected cells (Fig. 2); however, this increase was consistent throughout all time points after infection and was specific to the vRNA only. These partial disagreements can be attributed to the use of different virus strains and/or different NS1 mutations; Nevertheless, the alteration of the NS1 protein affected the expression of viral genes, especially the HA and M genes, which are considered to be late viral genes.
Influenza virus genomic RNAs possess segment-specific packaging signals that include both noncoding regions (NCRs) and adjacent terminal coding region sequences (9). The truncation of the NS1 protein has been shown previously not to affect the packaging of viral RNA segments (30). In this study, we examined the role of these terminal sequences in the regulation of viral gene expression in the presence or absence of the NS1 protein. In a minigenome assay, the presence of the NS1 protein was shown to be essential for the expression of a gene that is flanked by the HA terminal sequences but not the NP terminal sequences (Fig. 4). This observation implies a role for the NS1 protein in regulating viral gene expression in a segment-specific manner, and this segment specificity can be mapped to the terminal (packaging) sequences of the influenza virus vRNA. Further studies will be needed to address the precise mechanism behind these findings and the question of whether other viral genes are affected in a similar manner.
The amount of HA protein present in an influenza virus vaccine is critical for its efficacy. The HA protein is one of two surface glycoproteins present on the viral envelope and is the target for most of the neutralizing antibodies, making it an important immunogen. The observation that the truncation of the NS1 protein leads to a reduced level of HA protein expression offered the possibility of improving the potency of this live attenuated influenza virus vaccine candidate by increasing the level of HA expression. Therefore, we generated a PR8-based vector encoding a truncated NS1 protein (NS1 1-73) and carrying the G3A C8U “superpromoter” mutations in its HA segment (S73). The levels of HA expression in cells infected with this recombinant virus were comparable to those in cells infected with a wild-type virus (Fig. 5A). The increase in HA protein levels correlated with an increase in HA mRNA levels (data not shown). More importantly, this increase in HA protein levels does not alter the replication characteristics of the virus in vitro or in vivo (Fig. 5B and C). Finally, in order to demonstrate that the increase in HA expression offers an immunogenic advantage, mice were vaccinated with NS1-truncated PR8 viruses carrying either a “superpromoter” or a wild-type promoter in the HA segment. Our results indicate that vaccination of mice with the vector carrying the HA “superpromoter” induced significantly higher virus-specific serum antibody titers (Fig. 6A), which correlated with improved survival following lethal challenge (Fig. 6B and C).
A previous report established a positive correlation between the levels of antigen expression and antigen-specific protective immune response in the context of a live viral vaccine (5). In this study, we demonstrate that an increase in HA expression improves the protective efficacy of NS1-truncated influenza viruses and that this correlates with an enhanced antibody response. However, we cannot attribute this enhanced protection from challenge solely to an increase in HA-specific antibodies, since the role of HA-specific cytotoxic T cells still needs to be investigated. In addition, since influenza viruses encoding a “superpromoter” appear to generate more immunostimulatory RNA, resulting in increased induction of IFN, it is possible that this property might also improve their immunogenicity (A. Belicha-Villanueva et al. submitted for publication). In conclusion, the C-terminal truncation of the NS1 protein reduces the levels of HA protein and mRNA in infected cells, but the introduction of a “superpromoter” mutation in the HA segment rescues the levels of HA protein expression and increases the immunogenicity of this live attenuated influenza virus vaccine candidate without increasing its virulence.
ACKNOWLEDGMENTS
We thank Chen Wang, Richard Cadagan, and Osman Lizardo for excellent technical assistance.
This work has been supported by National Institutes of Health (NIH) grants UOI AI070469 and U54 AI057158, NIAID grants RO1 AI046954 and U19 AI083025, CRIP (Center for Research on Influenza Pathogenesis, NIAID CEIRS contract HHSN266200700010C), and a research collaboration agreement with PATH. N. Pica was supported by Mount Sinai Medical Scientist Training Grant T32 GM007280. F. Krammer was supported by an Erwin Schrödinger Fellowship (J 3232) from the Austrian Science Fund (FWF).
Mount Sinai School of Medicine owns intellectual property in influenza virus reverse genetics and vaccines.
Footnotes
Published ahead of print 7 March 2012
REFERENCES
- 1. Baskin CR, et al. 2007. Functional genomic and serological analysis of the protective immune response resulting from vaccination of macaques with an NS1-truncated influenza virus. J. Virol. 81:11817–11827 doi:10.1128/JVI.00590-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Belshe RB, et al. 2007. Live attenuated versus inactivated influenza vaccine in infants and young children. N. Engl. J. Med. 356:685–696 doi:10.1056/NEJMoa065368 [DOI] [PubMed] [Google Scholar]
- 3. Bortz E, et al. 2011. Host- and strain-specific regulation of influenza virus polymerase activity by interacting cellular proteins. mBio 2(4):e00151–11 doi:10.1128/mBio.00151-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Campbell RE, et al. 2002. A monomeric red fluorescent protein. Proc. Natl. Acad. Sci. U. S. A. 99:7877–7882 doi:10.1073/pnas.082243699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Carnero E, et al. 2009. Optimization of human immunodeficiency virus Gag expression by Newcastle disease virus vectors for the induction of potent immune responses. J. Virol. 83:584–597 doi:10.1128/JVI.01443-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. de la Luna S, Fortes P, Beloso A, Ortin J. 1995. Influenza virus NS1 protein enhances the rate of translation initiation of viral mRNAs. J. Virol. 69:2427–2433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Falcon AM, et al. 2004. Defective RNA replication and late gene expression in temperature-sensitive influenza viruses expressing deleted forms of the NS1 protein. J. Virol. 78:3880–3888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ferko B, et al. 2004. Immunogenicity and protection efficacy of replication-deficient influenza A viruses with altered NS1 genes. J. Virol. 78:13037–13045 doi:10.1128/JVI.78.23.13037-13045.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gao Q, Palese P. 2009. Rewiring the RNAs of influenza virus to prevent reassortment. Proc. Natl. Acad. Sci. U. S. A. 106:15891–15896 doi:10.1073/pnas.0908897106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Garcia-Sastre A, et al. 1998. Influenza A virus lacking the NS1 gene replicates in interferon-deficient systems. Virology 252:324–330 [DOI] [PubMed] [Google Scholar]
- 11. Garfinkel MS, Katze MG. 1993. Translational control by influenza virus. Selective translation is mediated by sequences within the viral mRNA 5′-untranslated region. J. Biol. Chem. 268:22223–22226 [PubMed] [Google Scholar]
- 12. Gorse GJ, Belshe RB. 1990. Enhancement of anti-influenza A virus cytotoxicity following influenza A virus vaccination in older, chronically ill adults. J. Clin. Microbiol. 28:2539–2550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gorse GJ, Belshe RB. 1991. Enhanced lymphoproliferation to influenza A virus following vaccination of older, chronically ill adults with live-attenuated viruses. Scand. J. Infect. Dis. 23:7–17 [DOI] [PubMed] [Google Scholar]
- 14. Hale BG, Albrecht RA, Garcia-Sastre A. 2010. Innate immune evasion strategies of influenza viruses. Future Microbiol. 5:23–41 doi:10.2217/fmb.09.108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hale BG, Randall RE, Ortin J, Jackson D. 2008. The multifunctional NS1 protein of influenza A viruses. J. Gen. Virol. 89:2359–2376 doi:10.1099/vir.0.2008/004606-0 [DOI] [PubMed] [Google Scholar]
- 16. Hatada E, Hasegawa M, Shimizu K, Hatanaka M, Fukuda R. 1990. Analysis of influenza A virus temperature-sensitive mutants with mutations in RNA segment 8. J. Gen. Virol. 71(Pt 6):1283–1292 [DOI] [PubMed] [Google Scholar]
- 17. Hatada E, Saito S, Okishio N, Fukuda R. 1997. Binding of the influenza virus NS1 protein to model genome RNAs. J. Gen. Virol. 78(Pt 5):1059–1063 [DOI] [PubMed] [Google Scholar]
- 18. Hatada E, Takizawa T, Fukuda R. 1992. Specific binding of influenza A virus NS1 protein to the virus minus-sense RNA in vitro. J. Gen. Virol. 73(Pt 1):17–25 [DOI] [PubMed] [Google Scholar]
- 19. Haye K, Burmakina S, Moran T, Garcia-Sastre A, Fernandez-Sesma A. 2009. The NS1 protein of a human influenza virus inhibits type I interferon production and the induction of antiviral responses in primary human dendritic and respiratory epithelial cells. J. Virol. 83:6849–6862 doi:10.1128/JVI.02323-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Levy DE, Garcia-Sastre A. 2001. The virus battles: IFN induction of the antiviral state and mechanisms of viral evasion. Cytokine Growth Factor Rev. 12:143–156 [DOI] [PubMed] [Google Scholar]
- 21. Ludwig S, Vogel U, Scholtissek C. 1995. Amino acid replacements leading to temperature-sensitive defects of the NS1 protein of influenza A virus. Arch. Virol. 140:945–950 [DOI] [PubMed] [Google Scholar]
- 22. Marion RM, Zurcher T, de la Luna S, Ortin J. 1997. Influenza virus NS1 protein interacts with viral transcription-replication complexes in vivo. J. Gen. Virol. 78(Pt 10):2447–2451 [DOI] [PubMed] [Google Scholar]
- 23. Martinez-Sobrido L, et al. 2010. Hemagglutinin-pseudotyped green fluorescent protein-expressing influenza viruses for the detection of influenza virus neutralizing antibodies. J. Virol. 84:2157–2163 doi:10.1128/JVI.01433-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mikulasova A, Vareckova E, Fodor E. 2000. Transcription and replication of the influenza A virus genome. Acta Virol. 44:273–282 [PubMed] [Google Scholar]
- 25. Min JY, Li S, Sen GC, Krug RM. 2007. A site on the influenza A virus NS1 protein mediates both inhibition of PKR activation and temporal regulation of viral RNA synthesis. Virology 363:236–243 doi:10.1016/j.virol.2007.01.038 [DOI] [PubMed] [Google Scholar]
- 26. Neumann G, Hobom G. 1995. Mutational analysis of influenza virus promoter elements in vivo. J. Gen. Virol. 76(Pt 7):1709–1717 [DOI] [PubMed] [Google Scholar]
- 27. Quinlivan M, et al. 2005. Attenuation of equine influenza viruses through truncations of the NS1 protein. J. Virol. 79:8431–8439 doi:10.1128/JVI.79.13.8431-8439.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Reed LJ, Muench H. 1938. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 27:493–497 [Google Scholar]
- 29. Solorzano A, et al. 2005. Mutations in the NS1 protein of swine influenza virus impair anti-interferon activity and confer attenuation in pigs. J. Virol. 79:7535–7543 doi:10.1128/JVI.79.12.7535-7543.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Steel J, et al. 2009. Live attenuated influenza viruses containing NS1 truncations as vaccine candidates against H5N1 highly pathogenic avian influenza. J. Virol. 83:1742–1753 doi:10.1128/JVI.01920-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Talon J, et al. 2000. Influenza A and B viruses expressing altered NS1 proteins: a vaccine approach. Proc. Natl. Acad. Sci. U. S. A. 97:4309–4314 doi:10.1073/pnas.070525997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wacheck V, et al. 2010. A novel type of influenza vaccine: safety and immunogenicity of replication-deficient influenza virus created by deletion of the interferon antagonist NS1. J. Infect. Dis. 201:354–362 doi:10.1086/649428 [DOI] [PubMed] [Google Scholar]
- 33. Wolstenholme AJ, Barrett T, Nichol ST, Mahy BW. 1980. Influenza virus-specific RNA and protein syntheses in cells infected with temperature-sensitive mutants defective in the genome segment encoding nonstructural proteins. J. Virol. 35:1–7 [DOI] [PMC free article] [PubMed] [Google Scholar]