Abstract
The hemagglutinin-neuraminidase (HN) protein of paramyxoviruses carries out three distinct activities contributing to the ability of HN to promote viral fusion and entry: receptor binding, receptor cleavage (neuraminidase), and activation of the fusion protein. The relationship between receptor binding and fusion triggering functions of HN are not fully understood. For Newcastle disease virus (NDV), one bifunctional site (site I) on HN′s globular head can mediate both receptor binding and neuraminidase activities, and a second site (site II) in the globular head is also capable of mediating receptor binding. The receptor analog, zanamivir, blocks receptor binding and cleavage activities of NDV HN′s site I while activating receptor binding by site II. Comparison of chimeric proteins in which the globular head of NDV HN is connected to the stalk region of either human parainfluenza virus type 3 (HPIV3) or Nipah virus receptor binding proteins indicates that receptor binding to NDV HN site II not only can activate its own fusion (F) protein but can also activate the heterotypic fusion proteins. We suggest a general model for paramyxovirus fusion activation in which receptor engagement at site II plays an active role in F activation.
INTRODUCTION
Entry of enveloped viruses into host cells requires fusion of the viral and cell membranes. Viral fusion is driven by specialized fusion proteins that bring the viral and host membranes in close apposition to form a fusion pore (17, 21, 59, 64, 65). For many paramyxoviruses, the fusion protein (F) is activated when the receptor binding protein binds to a host receptor (55). Once activation occurs, the F protein undergoes a coordinated series of conformational changes that bring the two membranes together and promote membrane fusion (26, 37). The nature of the series of conformational changes that permit F to mediate membrane fusion, as well as the role that the receptor binding protein of paramyxoviruses plays in this fusion process, has been the subject of recent studies (16, 25, 31).
Paramyxoviruses possess envelope proteins that provide a binding function and, depending on the specific paramyxovirus family member, a receptor-cleaving (neuraminidase) activity. All of the paramyxovirus receptor binding proteins studied to date, with the possible exception of respiratory syncytial virus (RSV) and human metapneumovirus (hMPV), also possess a third, critical function: they activate the F protein to mediate the merger of the viral envelope with the host cell membrane. For measles virus and henipaviruses, the receptor binding proteins (H or G) recognize a proteinaceous receptor and do not possess a receptor cleavage function (6, 22, 42–44, 66). For human parainfluenza viruses, the envelope protein hemagglutinin-neuraminidase (HN) contains both sialic acid receptor binding and receptor-cleaving (neuraminidase) activities and, when receptor-bound, activates the F protein to initiate the conformational changes leading to fusion (38–40, 52, 53, 55). Crystallographic studies of the HNs of human parainfluenza virus type 3 (HPIV3) (29), Newcastle disease virus (NDV) (14, 69), and parainfluenza virus 5 (PIV5) (68) have shown that a single active/catalytic site on the globular head of the HN molecule, called “site I,” has both receptor binding and neuraminidase activities. The X-ray crystal structure of the globular head of NDV HN (69) also showed a second binding site (“site II”) in the globular head.
The efficiency of F activation by HN critically influences the degree of fusion mediated by F as well as the efficiency of viral entry (51, 55). The balance between the three functions of HN—binding, fusion activation, and neuraminidase—ultimately determines the outcome of infection (53). A clear mechanistic comprehension of how these activities are regulated is key for understanding viral entry and for designing strategies to block infection (37). We have proposed that a second binding site in the globular head of HPIV3 and site II observed in the structure of NDV HN′s globular head plays an important role in F protein triggering (47, 50, 51, 54).
For NDV HN, mutations in site I can alter sialic acid receptor binding and neuraminidase activity (11, 32), while mutations at site II alter receptor binding and fusion promotion without affecting neuraminidase activity (9). Small molecule receptor analogs designed to inhibit neuraminidase (e.g., zanamivir) inhibit NDV HN′s neuraminidase but not sialic acid receptor binding (54). We have previously investigated the functional relationship between NDV HN site II and the bifunctional site I and found that the engagement of site I with a receptor analog (zanamivir) leads to the activation of site II (50). Activated site II has higher receptor avidity than site I (50). It has recently been shown that NDV HNs with mutations in the NDV HN dimer interface, which led to decreased receptor binding, also impaired fusion promotion (13). Adding zanamivir to one of these HN mutants restored binding, suggesting that zanamivir binding to site I induced activation of site II in this mutant (33). In the present study, we demonstrate that receptor binding to NDV HN site II efficiently transmits the fusion signal to the stalk regions of not only NDV HN but also HPIV3 and Nipah virus (NiV) receptor binding proteins (HN and G). Our data suggest a unified model for paramyxovirus fusion activation in which receptor engagement at the globular head of the receptor binding protein plays an active role in F activation.
MATERIALS AND METHODS
Chemicals.
Zanamivir was prepared from Relenza Rotadisks (5 mg zanamivir with lactose). A 50 mM stock solution was prepared by dissolving each 5-mg blister capsule in 285 μl Optimem medium (Gibco). Stock solutions were stored at −20°C. Sialyllactose was obtained from Sigma-Aldrich (A0828), and a 10 mM stock solution was prepared by dissolving in CO2-independent medium (pH 7.3; Gibco).
Plasmids.
The genes of NiV wild-type (wt) G and wt F were codon optimized and synthesized by GeneArt (Germany) and subsequently subcloned into the mammalian expression vector pCAGGS using EcoRI or XhoI and BglII restriction enzyme sites. The various chimeric and mutated cDNAs were codon optimized and synthesized by Epoch Biolabs and subcloned into the mammalian expression vector pCAGGS. The NDV HN and F pCAGGS expression vectors were generously provided by Ronald Iorio, University of Massachusetts—Worcester.
Transient expression of the HPIV3 and NDV HN/F, NiV G/F, and chimeric cDNA genes.
Transfections were performed according to the Lipofectamine 2000 manufacturer's protocols (Invitrogen).
Cell cultures.
The human kidney epithelial 293T cell line was grown in Dulbecco's modified Eagle medium (DMEM) supplemented with 10% fetal bovine serum (FBS) and antibiotics at 37°C and 5% CO2.
HAD assays.
Hemadsorption (HAD) assays were performed and quantified as previously described (52). Briefly, growth medium from 293T monolayers cotransfected with HN/F in 24- or 48-well Biocoat plates (Becton Dickson Labware) was aspirated and replaced with 200 μl of 1% red blood cell (RBC) solution in serum-free, CO2-independent medium (pH 7.3; Gibco) with or without zanamivir and placed at 4°C for 30 min. The wells were then washed three times with 200 μl cold CO2-independent medium. The bound RBCs were lysed with 200 μl RBC lysis solution (0.145 M NH4Cl and 17 mM Tris-HCl), and absorbance was read at 405 nm using a Spectramax M5 (Molecular Devices) microplate reader.
Cell surface expression assay.
Monolayers of 293T cells were transiently transfected with HN or F constructs. The cells were washed twice in phosphate-buffered saline (PBS) and then incubated with a pool of anti-NDV HN monoclonal antibodies (Santa Cruz Biotechnology mouse monoclonal IgG1 [IC114], IgG2a [HN14f], and IgG2a [HN4a]) in PBS containing 3% BSA and 0.1% sodium azide for 1 h. Samples were then washed twice in PBS and incubated with 1:100 of anti-mouse fluorescein isothiocyanate (FITC) (BD Pharmingen). To quantify cell surface proteins in each sample, indirect immunofluorescence was measured by fluorescence-activated cell sorting (FACS) (FACSCalibur; Becton, Dickinson).
Measurements of neuraminidase activity.
Assays were performed in transiently transfected 293T cell monolayers as previously described (47, 52). Briefly, 293T cells expressing viral glycoproteins were added to 96-well plates in CO2-independent medium at pH 5.0 or 6.5. After adding reaction mixtures containing 20 mM 2′-(4-methylumbelliferyl)-alpha-d-N-acetylneuraminic acid (Toronto Research Chemicals Inc.) substrate with and without 2 mM zanamivir, the plates were incubated at 37°C for 1 h. Throughout this period, the fluorescence that occurred as a result of substrate hydrolysis was read at a 365-nm excitation wavelength and 450-nm emission wavelength using a Spectramax M5 microplate reader.
β-Gal complementation-based fusion assay.
We previously adapted a fusion assay based on alpha complementation of β-galactosidase (β-Gal) (36, 51). In this assay, receptor-bearing cells expressing the omega peptide of β-Gal are mixed with cells coexpressing envelope glycoproteins and the alpha peptide of β-Gal, and cell fusion leads to complementation. Fusion is stopped by lysing the cells, and after addition of the substrate, fusion is quantified on a Spectramax M5 microplate reader.
Measurement of fusion between RBCs and envelope glycoprotein-expressing cells.
Monolayers of 293T cells transiently expressing viral glycoproteins were washed and incubated with 1% RBC suspensions (pH 7.5) for 30 min at 4°C with or without zanamivir (2 mM). After the samples were rinsed to remove unbound RBCs, they were placed at 37°C for the indicated time with or without 2 mM zanamivir. The plates were then rocked, and the liquid phase was collected in V-bottom tubes for measurement of released RBCs. The cells were then incubated at 4°C with 200 ml of RBC lysis solution, where the lysis of unfused RBCs with NH4Cl removes RBCs that have not fused with cells coexpressing envelope glycoproteins. The liquid phase was collected in V-bottom 96-well plates for measurement of bound RBCs. The cells were then lysed in 200 μl 0.2% Triton X-100-PBS and transferred to flat-bottom 96-well plates for quantification of fused RBCs. The amount of RBCs in each of the above three compartments was determined by measuring the absorption at 405 nm.
Partial removal of sialic acid receptors from RBCs.
Partial receptor depletion of RBCs was achieved by treating 2 ml of a 10% RBC solution in serum-free medium for 2 h at 37°C with 0 to 200 mU of Clostridium perfringens neuraminidase (type V from C. perfringens, catalog no. N-2876; Sigma Scientific, St. Louis, MO) as previously described (41). Neuraminidase was then removed by washing the RBCs 3 times with serum-free medium. Each set of RBCs was then resuspended in serum-free, CO2-independent medium to achieve final 2% RBC stocks.
Assessment of HN receptor binding avidity with receptor-depleted RBCs.
RBCs partially depleted of their surface sialic acid receptors (described above) were used to determine the relative receptor binding avidities of variant HN molecules as previously described (41). In each experiment, all RBCs were obtained from the same preparation of depleted stocks (as described above). The RBCs were overlaid on 293T cell monolayers in 48-well plates transiently transfected 24 h prior with wt or variant HN expression vectors as described above. The plates were incubated at 4°C for 30 min to allow RBC binding. The cell monolayers were then washed at 4°C with cold CO2-independent medium to remove unbound RBCs, bound RBCs were lysed with RBC lysis buffer, and the absorbance was read at 405 nm on a Spectramax enzyme-linked immunosorbent assay (ELISA) reader. Results were presented as percent retention of RBCs relative to the control level (undepleted RBCs) versus the degree of depletion, expressed as mU of bacterial neuraminidase. For pretreatment of HN-expressing cells with neuraminidase, the monolayers were treated with 25 mU of the enzyme per well in 48-well plates (5 × 105 cells) for 3 h at 37°C, transferred to 4°C until they reach that temperature, and then washed.
Homology modeling of HPIV3-NDV chimera.
The HPIV HN(1–144)–NDV HN(123–599) chimera model was built from the crystal structure of NDV HN (PDB identifier 3T1E). Part of the HPIV3 HN sequence (residues 97 to 144) was sequence aligned with the stalk region of NDV HN. The HPIV3 HN stalk was then generated from 3T1E.pdb based on sequence alignment. The linker region between the HPIV3 stalk and NDV receptor binding domain was manually built in the Coot software program (18), and the complete model was energy minimized in the Phenix program (1).
RESULTS
Role of NDV HN site II in homotypic fusion activation.
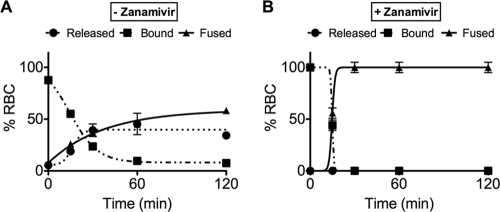
The specific role of NDV HN site II in driving F-mediated fusion has not been explored. To evaluate the roles of site II, we used the receptor analog zanamivir to occupy site I and activate site II (50). NDV (Australia-Victoria [AV]) wt HN was coexpressed with NDV F, and we evaluated the impact of the addition of zanamivir on the ability of HN to activate F, using an assay we had previously designed to distinguish between different states of F activation (47, 51, 55). The readout for F activation by HN in each case was fusion of red blood cells (RBC) with the HN/F-expressing cells. Cells coexpressing NDV F and NDV HN were allowed to bind to their sialic acid receptors on RBCs at 4°C in the presence or absence of 2 mM zanamivir (Fig. 1). The cells were then washed, and medium containing 0 or 2 mM zanamivir was added at 4°C. The cells were then transferred to 37°C to permit F activation. At different time points, we determined the amount of target RBCs that (i) were released into the medium, indicating that they had been attached only through HN and were released by the neuraminidase, which cleaves the sialic acid receptor (circles), (ii) were bound but had not fused, indicating that they were either bound by HN or by fusion peptide insertion (squares), or (iii) had undergone fusion (triangles), indicating that the F activation process proceeded past the transitional intermediate to achieve fusion. The NDV HN-F pair reached a maximum of 50% fusion in the absence of zanamivir (Fig. 1A). The same pair incubated in the presence of zanamivir, which blocks site I and activates site II, mediated fusion with 100% of the bound RBCs (Fig. 1B). In the absence of zanamivir, fusion promotion by NDV HN was most likely limited by the neuraminidase activity of site I, which cleaves the receptor and thereby halts the fusion process (53). In the presence of zanamivir, site I is engaged and cannot mediate receptor binding or neuraminidase activity, and therefore site II is capable of mediating both binding and fusion activation. In order to accomplish activation of site II, a functional site I is required; for example, mutations in site I that abolish neuraminidase activity of HN (i.e., D198R) also abolish both binding and fusion promotion (11, 32), and zanamivir does not activate site II in this mutant (data not shown). The results in Fig. 1 reveal that fusion occurs more efficiently when NDV HN site II is active and site I is engaged by zanamivir and that NDV HN site II alone is sufficient for binding and fusion activation.
Fig 1.
Role of HN in initiating the activation of F: requirement for site II stimulation for F activation. Monolayers of 293T cells coexpressing NDV wt HN and wt F were allowed to bind to receptor-bearing RBCs at 4°C in the absence (A) or presence (B) of 2 mM zanamivir. Upon transfer to 37°C, medium without (A) or with (B) 2 mM zanamivir was added. Values on the y axis reflect quantitation of RBCs that were released, bound, or fused. The values are means ± standard deviation (SD) of experiments performed in triplicate.
Chimeric receptor binding proteins mediate fusion.
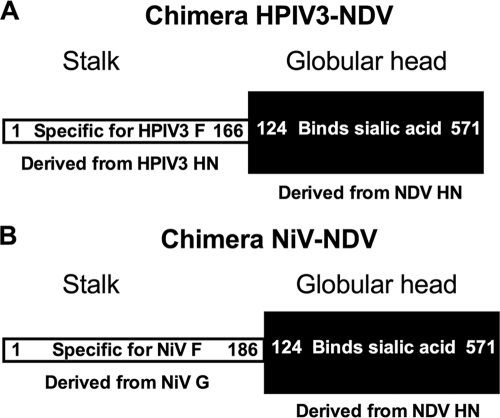
We have recently shown that an NiV G-NDV HN chimeric protein mediated fusion in the presence of zanamivir (49). Chimeric HPIV3 HN-NDV HN proteins have been described by us and others (19, 63), and we hypothesize that receptor engagement via NDV HN′s site II renders these chimeric proteins functional. Schematic diagrams of the two chimeric proteins used in the current studies are shown in Fig. 2. A beta-galactosidase complementation assay was used to quantify the fusion mediated by the chimeric proteins and their respective F proteins (the F protein homotypic to the stalk of each chimera). In cells coexpressing HPIV3 F and chimera HPIV3-NDV or HPIV3 HN (Fig. 3A) or coexpressing NiV F and chimera NiV-NDV or NiV G (Fig. 3B), each receptor binding protein activated the fusion protein corresponding to its specific stalk. If Fs were paired with chimeric receptor binding proteins bearing heterotypic stalks, fusion was not promoted (data not shown). The chimeric proteins promoted less fusion than the native receptor binding proteins, a difference that could result from multiple changes in the protein's properties.
Fig 2.
Schematic diagram of chimeric HN proteins. (A) Schematic diagram of chimera HPIV3-NDV. The stalk region is derived from residues 1 to 166 of HPIV3 HN, and the globular head is derived from residues 124 to 571 of NDV HN. (B) Schematic diagram of chimera NiV-NDV. The stalk region is derived from residues 1 to 186 of NiV G and the globular head is derived from residues 124 to 571 of NDV HN.
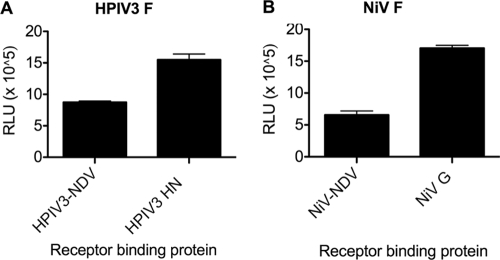
Fig 3.
Chimeric receptor binding proteins with NDV globular heads mediate fusion promotion. Cell-to-cell fusion mediated by the chimeric HPIV3-NDV protein with HPIV3 F (A) or chimeric NiV-NDV protein with NiV F (B), compared to the HPIV3 HN/F (A) or NiV G/F (B) proteins. Fusion is measured by a β-Gal complementation assay. The values are means ± SD of results from samples assessed in triplicate and are representative of the experiment repeated at least 4 times.
Expression, binding, and neuraminidase activity of chimeric receptor binding proteins.
To assess the properties of the chimeric proteins that may affect fusion promotion, we determined the expression levels of the two chimeric proteins compared to that of NDV HN. Expression levels were measured using a commercial kit (27, 28, 62) with pooled anti-NDV HN monoclonal antibodies. Expression is presented as the percentage of NDV HN expression in Fig. 4A. The HPIV3-NDV chimera had a higher expression level than NDV HN and the NiV-NDV chimera. To assess binding, cells expressing the indicated envelope proteins were allowed to bind RBCs at 4°C in the absence (clear bar) or presence (black bar) of zanamivir for 30 min, unbound RBCs were washed away, and the bound RBCs were quantified. Binding by the envelope glycoproteins was somewhat lower in the presence of zanamivir (Fig. 4B). Each protein exhibited neuraminidase activity in the absence (clear bar) or presence (black bar) of zanamivir (Fig. 4C), as calculated using our previously published assay (20, 47, 51). Although the cleavage activity was lower for the chimeric proteins than for NDV HN, the overall activity was still markedly higher than that of HPIV3 HN. Note that while the enzymatic site is contained in the globular head, the neuraminidase activity is influenced by the stalk domain; single-residue stalk alterations can affect neuraminidase activity (7, 15, 41, 50, 51, 55, 67), and it is therefore not surprising that transposing the NDV head onto a different stalk alters neuraminidase activity. The presence of zanamivir (black bar) decreased the neuraminidase activity of the chimeric proteins (Fig. 4C) without decreasing binding activity (Fig. 4B), suggesting that NDV HN site II likely mediates receptor binding when site I is blocked by the inhibitor.
Fig 4.
Chimeric protein expression, binding, and neuraminidase activity. (A) FACS analysis of cell surface expression from cells transfected with the chimeric proteins shown in Fig. 2. The results are presented as percentages of NDV HN cell surface expression. (B) Receptor binding in the absence (clear bar) or presence (black bar) of 2 mM zanamivir. The binding results are compared to NDV HN binding under the same conditions. (C) Neuraminidase activity of the receptor binding proteins, expressed in relative fluorescence intensity units (RFU) in the absence (clear bar) or presence (black bar) of 2 mM zanamivir. The neuraminidase results are compared to those for NDV HN and HPIV3 HN under the same conditions. The values are means ± SD of results from samples assessed in triplicate and are representative of the experiment repeated at least 4 times.
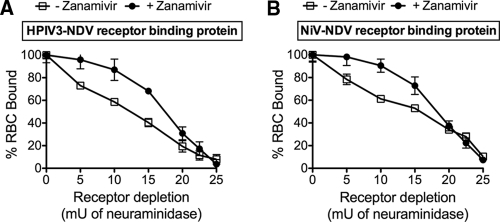
Zanamivir increases the receptor binding avidity of the chimeric proteins.
We have used a quantitative receptor avidity assay (41, 50, 51, 55) to show that NDV HN has low avidity for receptors on RBCs (either human or avian) compared to HPIV3 HNs (54). We have also compared the avidities of the two NDV HN sites and found that the receptor binding avidity of site II was higher than that of site I (50). RBCs with increasing sialic acid receptor depletion are bound to HN-expressing cells in a quantitative hemadsorption (HAD) assay, where greater receptor depletion required to reduce binding indicates higher avidity. At 4°C, the neuraminidase activity of NDV HN is not functional and therefore cannot contribute to RBC release. Thus, in the presence of zanamivir, HAD results from site II binding only, allowing its avidity to be assessed.
The binding avidity of the HPIV3-NDV chimeric protein (Fig. 5A) without zanamivir (open squares) declined rapidly, reaching 60% binding at a level caused by only 10 mU neuraminidase. However, in the presence of zanamivir, this chimera maintained approximately 90% binding, indicating that the receptor avidity of this chimera increased in the presence of zanamivir. Similarly, the binding avidity of the NiV-NDV chimeric protein (Fig. 5B) without zanamivir (open squares) also declined rapidly, reaching 60% binding at a level caused by only 10 mU neuraminidase. However, in the presence of zanamivir (filled circles), the decline was more gradual and remained at 90 to 100% binding at the same depletion level, indicating that the receptor avidity of NDV HN is increased in the presence of zanamivir. These results suggest that NDV HN′s site II is activated by zanamivir in the chimeric receptor binding proteins.
Fig 5.
The effects of zanamivir on receptor binding by chimeric proteins. A panel of RBCs with different degrees of receptor depletion was used to quantify HAD on cell monolayers expressing HPIV3-NDV (A) or NiV-NDV (B) in the absence (open squares) or presence (filled circles) of 2 mM zanamivir at 4°C (a temperature at which neuraminidase activity is negligible). The binding of each depleted RBC preparation (y axis) is expressed as a percentage of that of the control (i.e., of the amount of untreated, nondepleted RBCs bound to cells expressing the corresponding receptor binding protein). Data represent the means of results from triplicate monolayers from 3 representative experiments, with bars denoting standard deviations.
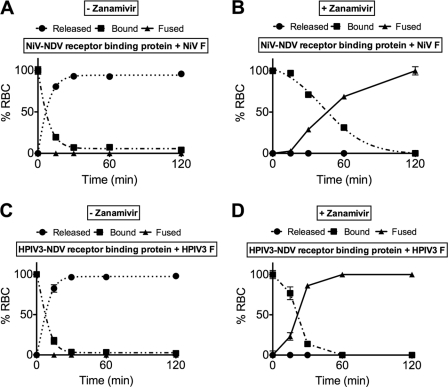
NDV HN site II transmits a fusion signal to HPIV3 or NiV F protein.
In NDV wt HN, the fusion signal is transmitted to the stalk region of the receptor binding protein as a result of activation of site II (47, 51, 55), with or without zanamivir (Fig. 1). Zanamivir blocks the cleavage activity of site I and establishes constant receptor engagement through the activation of site II, allowing us to determine whether site II activation is sufficient for the chimeric proteins to activate F. These conditions remove the variable of receptor cleaving activity, which can have variable effects depending on the virus; in the case of NiV, the receptor binding protein G does not have receptor cleaving activity and therefore remains bound to the receptor during F activation, while for HPIV3, the ratio of binding avidity to neuraminidase activity modulates F activation (53).
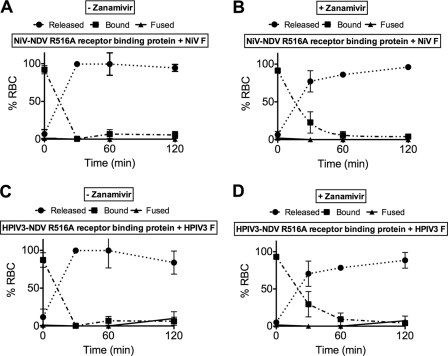
Here we used the same fusion assay to study the chimeras. Cells coexpressing the chimeric receptor binding proteins with the F proteins homotypic for the specific stalk region were allowed to bind to RBCs for 30 min at 4°C in the presence or absence of zanamivir (Fig. 6). The cells were washed, new medium with or without zanamivir was added, and the cells were transferred to 37°C to determine at different time points the percentages of sialic acid receptor-bearing RBCs that were released into the medium (circles), were bound but had not fused (squares), or had undergone fusion (triangles).
Fig 6.
NDV HN site II is required for F activation. 293T cells coexpressing NiV F with the NiV-NDV chimeric binding protein (A and B) or expressing HPIV3 F with the HPIV3-NDV chimeric binding protein (C and D) were allowed to bind to receptor-bearing RBCs at 4°C in the absence (A and C) or presence (B and D) of zanamivir. Zanamivir was added to activate NDV HN site II. Values on the y axis reflect quantitation of RBCs that were released, bound, or fused at the time points of incubation at 37°C indicated on the x axis. The values are means ± SD of results from triplicate monolayers from a representative experiment, repeated at least 3 times.
For the chimeric NiV-NDV and HPIV3-NDV proteins in the absence of zanamivir (Fig. 6A and C), no fusion was observed. However, in the presence of zanamivir, where site II is activated and site I is blocked, both chimeric proteins promoted fusion (Fig. 6B and D). As we and others have shown (2, 57, 60), the NiV fusion machinery is slower than that of HPIV3. Under the experimental conditions used for Fig. 6, the inherent triggering activity that results from the combination of the F protein and the receptor binding protein's specific stalk domain can be evaluated. The data are consistent with a requirement for activation of site II.
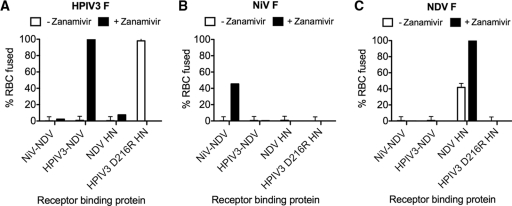
Stalk domains of chimeric receptor binding proteins confer specificity of fusion promotion, irrespective of constant receptor engagement or neuraminidase activity.
We considered the possibility that the fusion promoted by the chimeras resulted from constant receptor engagement instead of specific activation of F proteins. In that case, neuraminidase activity of HN could prevent the detection of heterotypic fusion activation, since the nonspecific heterotypic activation would be masked by disengagement from receptor binding in the absence of zanamivir. To address these questions, we performed cross-complementation of each chimera with each other's F protein and also included NDV HN, as well as an HPIV3 HN with a mutation that confers constitutive receptor engagement (D216R HN) (47, 50, 51, 54). Fusion was assessed in the absence (white bars) or presence (black bars) of zanamivir as for Fig. 6 at the 1-h time point. For HPIV3 F in the presence of zanamivir (Fig. 7A, black bars), only the HPIV3-NDV chimeric receptor binding protein promoted fusion, while in the absence of zanamivir (white bars), only the receptor-engaged HPIV3 HN promoted fusion. Neither NiV-NDV nor NDV HN promoted HPIV3 F fusion, even though these constructs mediate constant receptor binding in the presence of zanamivir. For NiV F, only the NiV-NDV chimeric receptor binding protein promoted fusion in the presence of zanamivir (Fig. 7B). No fusion was observed in the absence of zanamivir. Receptor binding proteins containing the HPIV3 stalk or the NDV stalk did not promote NiV F fusion. For NDV F in the presence of zanamivir (Fig. 7C, black bars), only the NDV HN promoted fusion, while in the absence of zanamivir this fusion was markedly reduced (consistent with the experiment shown in Fig. 1). Neither the chimera containing the HPIV3 stalk, the HPIV3 receptor-engaged HN, nor the chimera containing the NiV stalk promoted NDV F fusion. These results suggest that the cell-cell fusion observed here is mediated through the specific activation of F proteins by the stalk region of receptor binding proteins.
Fig 7.
Stalk domains of chimeric receptor binding proteins confer specificity of fusion promotion. 293T cells coexpressing HPIV3 F (A), NiV F (B), or NDV F (C) with the indicated receptor binding proteins (listed on the x axis) were allowed to bind to receptor-bearing RBCs at 4°C in the absence (white bars) or presence (dark bars) of zanamivir. Zanamivir was added to activate NDV HN site II. Values on the y axis reflect quantitation of RBCs that fused with the glycoprotein-expressing cells. The values are means ± SD of results of three experiments performed in triplicate.
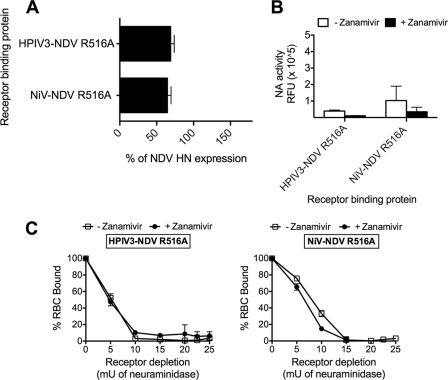
Mutation at NDV HN site II abolishes the ability of chimeric receptor binding proteins to promote fusion.
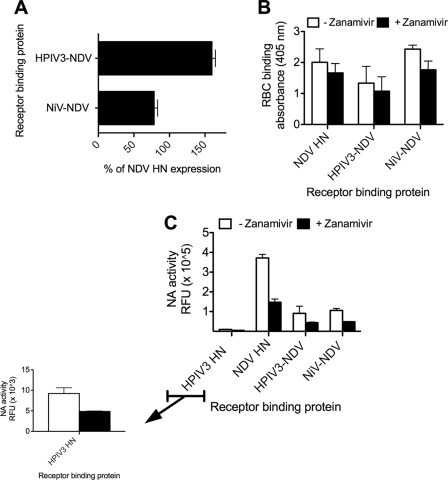
Mutations that abolish receptor binding at NDV HN′s site II have been described (9); specifically, a mutation at NDV HN residue R516 ablated binding of site II to sialic acid and reduced formation of syncytia. The arginine at position 516 is thus likely an important residue in this binding pocket. We introduced this mutation, R516A (9), into the globular head of the chimeric receptor binding proteins described in Fig. 2. Expression levels of the chimeric proteins with R516A were measured using a commercial kit (27, 28, 62) with pooled anti-NDV HN monoclonal antibodies. Expression is presented as the percentage of NDV HN expression in Fig. 8A. Each protein exhibited low but detectable neuraminidase activity, comparable to the activities of the chimeric proteins shown in Fig. 4C, in the absence (clear bar) or presence (black bar) of zanamivir (Fig. 8B), as calculated using our previously published assay (20, 47, 51). The binding avidity of the HPIV3-NDV R516A chimeric protein (Fig. 8C) without zanamivir (open squares) declined rapidly, reaching 50% binding at a receptor depletion level caused by only 10 mU neuraminidase. In the presence of zanamivir, this chimera's binding declined similarly, indicating that the receptor avidity of this chimera is not increased by zanamivir, as expected with an ablated site II. Similarly, the binding avidity of the NiV-NDV R516A chimeric protein (Fig. 8C) declined rapidly without zanamivir (open squares) or with zanamivir (filled circles), reaching 50 to 60% binding at a receptor depletion level caused by only 10 mU neuraminidase. These results suggest that for both chimeric proteins, the R516A mutation abolished the activation response to zanamivir at site II.
Fig 8.
Chimeric receptor binding proteins with mutation at NDV HN site II: expression, neuraminidase activity, and binding avidity. (A) FACS analysis of cell surface expression from cells transfected with the chimeric proteins described. The results are presented as percentages of NDV HN cell surface expression. (B) Neuraminidase activity of the receptor binding proteins, expressed in relative fluorescence intensity units (RFU) in the absence (clear bar) or presence (black bar) of 2 mM zanamivir. (C) A panel of RBCs with different degrees of receptor depletion was used to quantify HAD on cell monolayers expressing HPIV3-NDV R516A HN or NiV-NDV R516A HN in the absence or presence of 2 mM zanamivir at 4°C. The binding of each depleted RBC preparation (y axis) is expressed as a percentage of that of the control (i.e., of the amount of untreated, nondepleted RBCs bound to cells expressing the corresponding receptor binding protein). Data represent the means of results from triplicate monolayers from 3 representative experiments, with bars denoting standard deviations.
To determine whether the fusion signal can still be transmitted to the stalk region of the receptor binding protein despite the site II mutation, we used the assay described for Fig. 1 and 6 (47, 51, 55), with or without zanamivir. Cells coexpressing the mutated chimeric receptor binding proteins with the F proteins homotypic for the specific stalk region were allowed to bind to RBCs for 30 min at 4°C in the presence or absence of zanamivir (Fig. 9). The cells were washed, new medium with or without zanamivir was added, and the cells were transferred to 37°C to allow F activation. We determined at different time points the amount of sialic acid receptor-bearing RBCs that were released into the medium (circles), were bound but had not fused (squares), or had undergone fusion (triangles). For the NiV-NDV R516A and HPIV3-NDV R516A receptor binding proteins, no fusion was observed in the absence of zanamivir (Fig. 9A and C) or presence of zanamivir (Fig. 9B or D). The mutation at R516 abolished fusion activation by both chimeric receptor binding proteins. The data are consistent with a requirement for an intact site II for fusion promotion.
Fig 9.
Mutation at NDV HN site II abolishes the ability of chimeric receptor binding proteins to promote fusion. 293T cells coexpressing NiV F with NiV-NDV R516A chimeric binding protein (A and B) or expressing HPIV3 F with HPIV3-NDV R516A chimeric binding protein (C and D) were allowed to bind to receptor-bearing RBCs at 4°C in the absence (A and C) or presence (B and D) of zanamivir. Values on the y axis reflect quantitation of RBCs that were released, bound, or fused at the time points of incubation at 37°C indicated on the x axis. The values are means ± SD of results from triplicate monolayers from a representative experiment, repeated at least 3 times.
Mutation at NDV HN site II abolishes activation of site II in the NDV globular head in the presence of zanamivir.
We have previously shown that only certain receptor mimics effectively activate the NDV HN′s site II via occupation of site I; yet without activation of this second site, binding is mediated entirely by site I (50). To inhibit NDV HN′s binding, a molecule must either block both sites or block site I without activating site II. Sialyllactose, a naturally occurring substrate of the HN neuraminidase, blocks site I without activating site II (50). In determining that NDV HN′s site II becomes active only when site I is occupied by zanamivir, we found that sialyllactose and zanamivir competed for site I and had antagonistic effects. In the absence of zanamivir, sialyllactose completely abolished binding by NDV HN. However, once zanamivir inhabited site I, binding was activated at site II, and sialyllactose does not inhibit. Here we took advantage of the differential effect of the two small molecules to assess the effect of mutation at site II (R516A) on NDV HN receptor binding.
Cells expressing either the NDV HN, the NiV-NDV, or the HPIV3-NDV chimeric receptor binding protein, with or without the R516A mutation in HN, were allowed to bind RBCs at 4°C in the presence of 5 mM sialyllactose and 2 mM zanamivir (Fig. 10) for 30 min, unbound RBCs were washed away, and the bound RBCs were quantified. The nonmutated receptor binding molecules (NDV HN, NiV-NDV, and HPIV3-NDV) bound as expected (50). However, the same three molecules with the R516A mutation were completely inhibited, demonstrating close to zero receptor binding, showing that the mutation at R516 in NDV HN abolishes the antagonistic effect of zanamivir versus sialyllactose. Similarly, for the two chimeric proteins bearing the NDV globular head, the mutation at R516 abolished the antagonistic effect and conferred sensitivity to inhibition by sialyllactose. These findings are consistent with the R516A mutation abolishing activation at site II of the NDV globular head, so that now site II cannot rescue receptor binding in the presence of sialyllactose.
Fig 10.
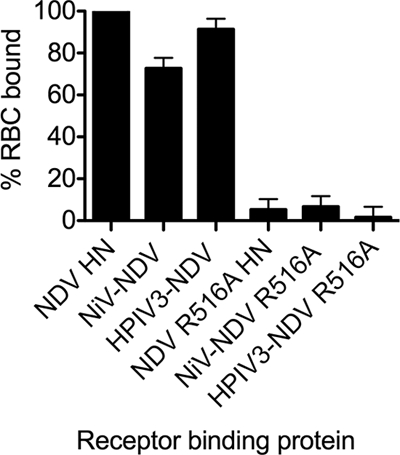
Mutation at NDV HN site II abolishes activation of site II in the NDV globular head in the presence of zanamivir. 293T cells expressing the indicated receptor binding proteins (listed on the x axis) were allowed to bind to receptor-bearing RBCs at 4°C in the presence of 5 mM sialyllactose plus 2 mM zanamivir. Values on the y axis reflect percentages of RBCs bound to the glycoprotein-expressing cells, compared with RBCs bound in the absence of inhibitors. The values are means ± SD of results from triplicate monolayers from a representative experiment, repeated 3 times.
DISCUSSION
The relationship between HN receptor binding and the subsequent activation of the F protein and the exact nature of how the signal is transmitted from HN to F during this process are of great interest. Previous models of HN-F interaction have suggested that either the HN-F interaction occurs in the absence of receptor and the two proteins separate upon receptor engagement or the HN-F interaction occurs only upon receptor binding (25, 26, 32, 61). We recently showed that HN and F interact prior to receptor engagement (56) and stay in contact during the triggering of fusion and that receptor engagement by HN is required not only for the initial activation of F but also at later stages in the fusion process (49). To analyze the series of events involved in fusion activation, we used the globular head of HN of one virus (NDV) to activate the fusion machinery of other viruses. We found that activation of NDV HN site II is required for proper transmission of the fusion signal. A mutation in HN′s site II that prevents its activity abolishes the ability of the NDV HN globular head to trigger F-mediated fusion under our experimental conditions (Fig. 9), and in the absence of zanamivir to activate NDV HN′s site II (Fig. 5) (50), the chimeric proteins do not efficiently trigger fusion (Fig. 3 and 6). Cross talk between the globular domain and the stalk of each receptor binding protein is essential for fusion activation. The specificity conferred by each virus's stalk is evident in the failure of the receptor binding proteins (chimeric or wt) to cross-complement each other's F proteins, even when the receptor binding proteins are continuously receptor bound (Fig. 7).
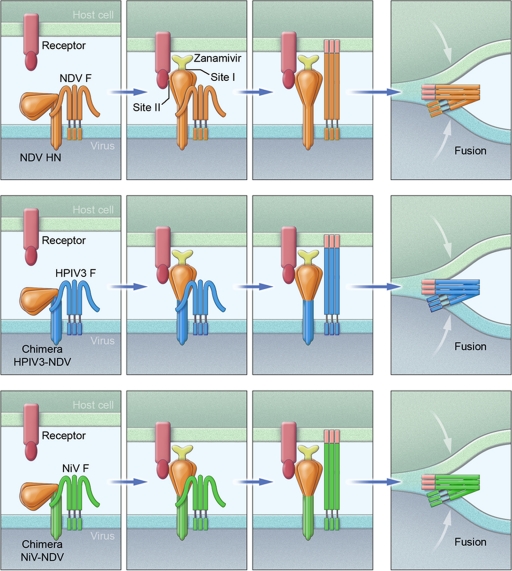
A summary of the experiments is shown schematically in Fig. 11. The receptor binding proteins are comprised of the stalk corresponding to the F protein in each pair (NDV, HPIV3, or NiV; each has its own color) and the globular head domain of NDV HN. Each row depicts a different receptor binding protein stalk/F pair. In the presence of zanamivir, the neuraminidase activity of site I of the NDV HN heads is occupied, and binding site II is activated. Upon engagement of site II with sialic acid receptor, each F is triggered, inserting its fusion peptide into the target membrane, and fusion ensues. The chimeric proteins were found to efficiently activate their respective fusion proteins, despite having a head region belonging to a very different virus, but did not activate the heterologous F protein. We propose that these findings provide a strong indication that the globular head of HN, once receptor bound, transmits the signal to the receptor binding protein's stalk, permitting fusion to proceed.
Fig 11.
Schematic representation of fusion activation by NDV site II. See Discussion, describing the use of NDV HN or chimeric HPIV3 HN-NDV HN or NiV G-NDV HN as receptor binding proteins, paired with NDV, HPIV3, or NiV F. Each row depicts a different HN stalk/F pair, as indicated. The NDV HN heads engage sialic acid receptors in the presence of zanamivir (the yellow molecule appearing in the second column). Zanamivir blocks binding by NDV HN′s site I but activates binding site II. Upon engagement of site II, each F inserts its fusion peptide into the target membrane, and fusion ensues.
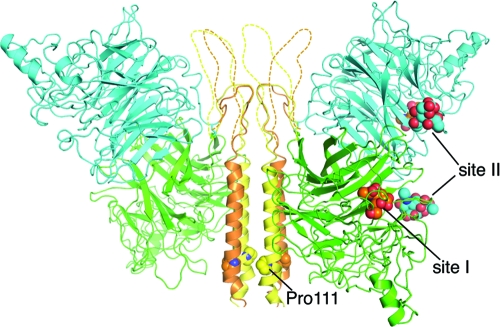
Binding site II on NDV HN, revealed by cocrystallization with thiosialoside (69), is at the dimer interface of the molecule and made up of hydrophobic residues from both monomers. Mutations at residue R516, a residue involved in the interaction with sialic acid, resulted in HNs that when coexpressed with F are less efficient in fusion promotion (9). In a previous report, NDV HNs mutated at site II (R516A or R516S) were found to bind RBCs similarly to wt HN in hemagglutination (HA) assays, a finding interpreted to mean that site II did not contribute to receptor binding activity (9). We have shown that the R516A mutation ablates the activation of site II in response to zanamivir and thereby alters binding avidity of site II in the presence of zanamivir. The finding that zanamivir does not inhibit receptor binding for the receptor binding protein bearing the R516A mutation was unexpected in light of a previous report showing that the small transition state analog BCX2798 blocked binding by NDV HN R516A (9). Unavailability of BCX2798 prevents a direct experimental comparison; however, we speculate that the Kansas NDV globular head used in that study differs from the AV NDV globular head used here and/or that it is possible for site I to retain binding function even when occupied by zanamivir. The experiments shown in Fig. 8, 9, and 10 indicate that mutation at site II abolishes activation of that site and that receptor binding proteins bearing the mutated site II in the head of NDV fail to efficiently promote the fusion process for the HPIV3 and NiV paramyxovirus F proteins.
Site II of NDV HN is activated in the presence of zanamivir but not in the presence of the receptor analog sialyllactose (50). We hypothesize that our results with this artificial addition of zanamivir are indicative of what may happen during viral infection. Zanamivir was designed based on transition state analogs and is similar in structure to the unsaturated derivative 2-deoxy-2,3-dehydro-N-acetylneuraminic acid (DANA), which naturally occurs as a by-product of the HN′s neuraminidase activity (58, 69). We propose that the generation of a transition state compound in active site I during receptor interaction leads to activation of site II. Such a reaction intermediate, which would resemble zanamivir rather than sialyllactose, may activate site II under physiological conditions. In this case, after initial binding of NDV HN via its bifunctional site I to a new cell and initiation of neuraminidase cleavage of receptor moieties, site II, which binds more avidly but lacks neuraminidase, becomes activated (50, 69). Although this hypothesis will need to be confirmed with additional studies in the future, this would explain the absolute requirement, at least for NDV, of neuraminidase activity for proper binding of HN and consequent fusion (23, 32). The interplay between the two NDV sites, which is needed for proper fusion activation, is also a novel target for the development of new inhibitors. The mechanism by which the binding of zanamivir to site I activates site II is of great interest, since it would provide insight into the roles of distinct regions of NDV HN in the multiple functions of this molecule (16, 24, 25, 30).
Our laboratory together with others has proposed that a second receptor binding site for several different HNs exists (8, 35, 47, 51), even though crystallographic evidence for viruses other than NDV is currently lacking (69). In previous studies, we identified a putative HPIV3 site II that is involved in receptor binding and fusion activation (47, 51). The HN mutation H552Q conferred partial resistance to both zanamivir (54) and another site I binding/neuraminidase inhibitor, BCX2855 (35), consistent with the notion that the mutation enhances binding by site II. Removal of glycans at various positions on HN (4, 35) unmasks receptor binding at site II, as demonstrated in the presence of small molecules that block site I. A conflicting report suggested that for HPIV1, mutation at residue 523 creates a second receptor binding site (8, 35, 47, 51). While only structural studies will settle these matters, there is now clear evidence of the existence of a site II for HPIV3 and HPIV1 HNs. For HPIV3, mutations in site II of HN modulate viral growth in the natural host (46). Future studies will assess whether the globular head of HPIV3 is able to activate stalk regions of other receptor binding proteins and whether this activation depends on site I or on the putative site II (51).
The recent availability of the crystal structures of the NDV and PIV5 stalk regions confirms that these domains form four-helical bundles (7, 67). In the NDV crystal, the stalk is connected to the globular head by an unresolved connecting region, and the globular head is bent to the side (67). The structural data led, in that report, to the suggestion that upon receptor engagement, the globular head is pulled up (67). In Fig. 12, we show a homology model of the HPIV3-NDV chimera, based on the crystal structure of NDV HN (67). The stalk region of the chimera was built by sequence alignment of HPIV3 HN (residues 97 to 144) with NDV HN. The conserved Pro111 in the stalk domain of HPIV3 is aligned with Pro93 in NDV HN proteins. The residues in the linker region (dashed lines) that are disordered in the crystal structure were manually built to connect the C-terminal end of the stalk with the nearest N terminus of the receptor binding domain. We previously showed that a chimera of HPIV3 HN(1-144)–NDV(124-571) is functional for receptor engagement and fusion promotion (19). The chimera that we present here, with the extended linker region (HPIV3 HN 1 to 166; Fig. 2A), also activates the F protein in the presence of zanamivir. Comparing these chimeric HPIV3-NDV receptor binding proteins reveals that different lengths of loop between the stalk and the globular head are tolerated, consistent with the proposed mechanism that upon receptor engagement, the globular head is pulled up, which then leads to the transmission of the fusion signal through the receptor binding protein's stalk domain (Fig. 12). For measles virus receptor binding protein (H) as well, it has been shown that the length of the intervening region between the stalk and the globular head can be altered without complete loss of function (45). A special case may occur for respiratory syncytial virus (RSV), where infection does not seem to require any surface protein other than F and the mechanism of activation of F remains to be determined (10).
Fig 12.
Homology model of HPIV3-NDV HN chimera. Fusion-related conformational changes are relayed from the receptor binding domain to the stalk through the domain interface. The chimeras of HPIV3 HN (yellow and orange) and NDV HN (green and cyan) likely preserve structural elements at the interface that are important for fusion activation. The chimera of HPIV3 HN(1–166)–NDV HN(124–571) has a long linker region (indicated by a dashed line) compared with the HPIV3 HN(1–144) chimera (in solid line) and wt NDV HN.
It will be important to apply the set of experimental strategies that we used here to additional paramyxoviruses that lack receptor destroying (or cleaving) activity and whose receptors are not sialic acid based. For these viruses, including measles virus, it has been suggested that the receptor binding protein mainly exerts a repressive role (3, 5, 12, 25, 30, 34, 42, 48); the receptor binding proteins stabilize the metastable state of the fusion proteins prior to receptor engagement, and upon receptor binding, the fusion proteins are released and proceed independently to fusion (25, 30, 34, 42). Based on the results presented here, taken together with our previous data, we favor a model for paramyxovirus fusion activation in which receptor engagement is required for the activation of F. The finding that one paramyxovirus receptor binding protein's globular head domain can activate at least two other paramyxovirus F proteins to proceed through fusion suggests that activation proceeds via similar mechanisms for these different viruses. The sialic acid binding NDV HN head activates the F protein of a virus whose receptor binding protein (G) binds proteinaceous receptors (6, 43), suggesting that despite the use of different specific receptor molecules by these viruses, the mechanism may be similar.
ACKNOWLEDGMENTS
We are grateful to Ashton Kutcher and Jonathan Ledecky for their support, to Dan and Nancy Paduano for support of innovative research projects, and to the Friedman Family Foundation for renovation of our laboratories at Weill Cornell Medical College. We acknowledge flow cytometry support from Sergei Rudchenko in the Flow Cytometry Facility of the Hospital for Special Surgery/Weill Cornell Medical College.
The work was supported by NIH (NIAID) grants R01 AI31971 to A.M. and R21 EBO11707 to M.P. R.X. and I.A.W. were supported in part by NIAID grant AI058113 (to I.A.W.) and the Skaggs Institute for Chemical Biology.
Footnotes
Published ahead of print 21 March 2012
This is publication 21539 from The Scripps Research Institute.
REFERENCES
- 1. Afonine PV, Grosse-Kunstleve RW, Adams PD. 2005. A robust bulk-solvent correction and anisotropic scaling procedure. Acta Crystallogr. D Biol. Crystallogr. 61:850–855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Aguilar HC, Aspericueta V, Robinson LR, Aanensen KE, Lee B. 2010. A quantitative and kinetic fusion protein-triggering assay can discern distinct steps in the Nipah virus membrane fusion cascade. J. Virol. 84:8033–8041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Aguilar HC, et al. 2006. N-glycans on Nipah virus fusion protein protect against neutralization but reduce membrane fusion and viral entry. J. Virol. 80:4878–4889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Alymova IV, et al. 2008. Loss of the N-linked glycan at residue 173 of human parainfluenza virus type 1 hemagglutinin-neuraminidase exposes a second receptor-binding site. J. Virol. 82:8400–8410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bishop KA, et al. 2008. Residues in the stalk domain of the hendra virus G glycoprotein modulate conformational changes associated with receptor binding. J. Virol. 82:11398–11409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bonaparte MI, et al. 2005. Ephrin-B2 ligand is a functional receptor for Hendra virus and Nipah virus. Proc. Natl. Acad. Sci. U. S. A. 102:10652–10657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bose S, et al. 2011. Structure and mutagenesis of the parainfluenza virus 5 hemagglutinin-neuraminidase stalk domain reveals a four-helix bundle and the role of the stalk in fusion promotion. J. Virol. 85:12855–12866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bousse T, Takimoto T. 2006. Mutation at residue 523 creates a second receptor binding site on human parainfluenza virus type 1 hemagglutinin-neuraminidase protein. J. Virol. 80:9009–9016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bousse TL, et al. 2004. Biological significance of the second receptor binding site of Newcastle disease virus hemagglutinin-neuraminidase protein. J. Virol. 78:13351–13355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chaiwatpongsakorn S, Epand RF, Collins PL, Epand RM, Peeples ME. 2011. Soluble respiratory syncytial virus fusion protein in the fully cleaved, pretriggered state is triggered by exposure to low-molarity buffer. J. Virol. 85:3968–3977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Connaris H, et al. 2002. Probing the sialic acid binding site of the hemagglutinin-neuraminidase of Newcastle disease virus: identification of key amino acids involved in cell binding, catalysis, and fusion. J. Virol. 76:1816–1824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Corey EA, Iorio RM. 2007. Mutations in the stalk of the measles virus hemagglutinin protein decrease fusion but do not interfere with virus-specific interaction with the homologous fusion protein. J. Virol. 81:9900–9910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Corey EA, Mirza AM, Levandowsky E, Iorio RM. 2003. Fusion deficiency induced by mutations at the dimer interface in the Newcastle disease virus hemagglutinin-neuraminidase is due to a temperature-dependent defect in receptor binding. J. Virol. 77:6913–6922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Crennell S, Takimoto T, Portner A, Taylor G. 2000. Crystal structure of the multifunctional paramyxovirus hemagglutinin-neuraminidase. Nat. Struct. Biol. 7:1068–1074 [DOI] [PubMed] [Google Scholar]
- 15. Deng R, Wang Z, Mirza A, Iorio R. 1995. Localization of a domain on the paramyxovirus attachment protein required for the promotion of cellular fusion by its homologous fusion protein spike. Virology 209:457–469 [DOI] [PubMed] [Google Scholar]
- 16. Dutch RE. 2010. Entry and fusion of emerging paramyxoviruses. PLoS Pathog. 6:e1000881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Eckert DM, Kim PS. 2001. Mechanisms of viral membrane fusion and its inhibition. Annu. Rev. Biochem. 70:777–810 [DOI] [PubMed] [Google Scholar]
- 18. Emsley P, Lohkamp B, Scott WG, Cowtan K. 2010. Features and development of Coot. Acta Crystallogr. D Biol. Crystallogr. 66:486–501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Farzan SF, et al. 2011. Premature activation of the paramyxovirus fusion protein before target cell attachment with corruption of the viral fusion machinery. J. Biol. Chem. 286:37945–37954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Greengard O, Poltoratskaia N, Leikina E, Zimmerberg J, Moscona A. 2000. The anti-influenza virus agent 4-GU-DANA (Zanamivir) inhibits cell fusion mediated by human parainfluenza virus and influenza virus HA. J. Virol. 74:11108–11114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Harrison SC. 2008. Viral membrane fusion. Nat. Struct. Mol. Biol. 15:690–698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hashiguchi T, et al. 2011. Structure of the measles virus hemagglutinin bound to its cellular receptor SLAM. Nat. Struct. Mol. Biol. 18:135–141 [DOI] [PubMed] [Google Scholar]
- 23. Iorio RM, et al. 2001. Structural and functional relationship between the receptor recognition and neuraminidase activities of the Newcastle disease virus hemagglutinin-neuraminidase protein: receptor recognition is dependent on neuraminidase activity. J. Virol. 75:1918–1927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Iorio RM, Mahon PJ. 2008. Paramyxoviruses: different receptors—different mechanisms of fusion. Trends Microbiol. 16:135–137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Iorio RM, Melanson VR, Mahon PJ. 2009. Glycoprotein interactions in paramyxovirus fusion. Future Virol. 4:335–351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lamb RA, Paterson RG, Jardetzky TS. 2006. Paramyxovirus membrane fusion: lessons from the F and HN atomic structures. Virology 344:30–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Latger-Cannard V, et al. 2000. Determination of polymorphonuclear neutrophil adhesion receptors. Effect of pre-analytic factors. J. Mal. Vasc. 25:181–186 (In French.) [PubMed] [Google Scholar]
- 28. Latger-Cannard V, et al. 2000. Use of standard for quantitation of adhesion of polynuclear neutrophils by flow cytometry. Ann. Biol. Clin. (Paris) 58:337–343 (In French.) [PubMed] [Google Scholar]
- 29. Lawrence MC, et al. 2004. Structure of the haemagglutinin-neuraminidase from human parainfluenza virus type III. J. Mol. Biol. 335:1343–1357 [DOI] [PubMed] [Google Scholar]
- 30. Lee B, Ataman ZA. 2011. Modes of paramyxovirus fusion: a Henipavirus perspective. Trends Microbiol. 19:389–399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lee KK, et al. 2011. Capturing a fusion intermediate of influenza hemagglutinin with a cholesterol-conjugated peptide: a new antiviral strategy for influenza virus. J. Biol. Chem. 286:42141–42149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Li J, Quinlan E, Mirza A, Iorio RM. 2004. Mutated form of the Newcastle disease virus hemagglutinin-neuraminidase interacts with the homologous fusion protein despite deficiencies in both receptor recognition and fusion promotion. J. Virol. 78:5299–5310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mahon PJ, Mirza AM, Iorio RM. 2011. Role of the two sialic acid binding sites on the Newcastle disease virus HN protein in triggering the interaction with the F protein required for the promotion of fusion. J. Virol. 85:12079–12082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mirza AM, et al. 2011. Triggering of the Newcastle disease virus fusion protein by a chimeric attachment protein that binds to Nipah virus receptors. J. Biol. Chem. 286:17851–17860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mishin VP, et al. 2010. N-linked glycan at residue 523 of human parainfluenza virus type 3 hemagglutinin-neuraminidase masks a second receptor-binding site. J. Virol. 84:3094–3100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Moosmann P, Rusconi S. 1996. Alpha complementation of LacZ in mammalian cells. Nucleic Acids Res. 24:1171–1172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Moscona A. 2005. Entry of parainfluenza virus into cells as a target for interrupting childhood respiratory disease. J. Clin. Invest. 115:1688–1698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Moscona A, Peluso R. 1991. Properties of the human parainfluenza virus type 3 RNA polymerase/replicase in vitro: consensus with other negative-stranded RNA viruses. J. Virol. 65:4470–4474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Moscona A, Peluso RW. 1992. Fusion properties of cells infected with human parainfluenza virus type 3: receptor requirements for viral spread and virus-mediated membrane fusion. J. Virol. 66:6280–6287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Moscona A, Peluso RW. 1993. Relative affinity of the human parainfluenza virus 3 hemagglutinin-neuraminidase for sialic acid correlates with virus-induced fusion activity. J. Virol. 67:6463–6468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Murrell M, Porotto M, Weber T, Greengard O, Moscona A. 2003. Mutations in human parainfluenza virus type 3 HN causing increased receptor binding activity and resistance to the transition state sialic acid analog 4-GU-DANA (zanamivir). J. Virol. 77:309–317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Navaratnarajah CK, et al. 2011. The heads of the measles virus attachment protein move to transmit the fusion-triggering signal. Nat. Struct. Mol. Biol. 18:128–134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Negrete OA, et al. 2005. EphrinB2 is the entry receptor for Nipah virus, an emergent deadly paramyxovirus. Nature 436:401–405 [DOI] [PubMed] [Google Scholar]
- 44. Noyce RS, et al. 2011. Tumor cell marker PVRL4 (nectin 4) is an epithelial cell receptor for measles virus. PLoS Pathog. 7:e1002240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Paal T, et al. 2009. Probing the spatial organization of measles virus fusion complexes. J. Virol. 83:10480–10493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Palermo L, et al. 2009. Human parainfluenza virus infection of the airway epithelium: the viral hemagglutinin-neuraminidase regulates fusion protein activation and modulates infectivity. J. Virol. 83:6900–6908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Palermo LM, Porotto M, Greengard O, Moscona A. 2007. Fusion promotion by a paramyxovirus hemagglutinin-neuraminidase protein: pH modulation of receptor avidity of binding sites I and II. J. Virol. 81:9152–9161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Plemper RK, Hammond AL, Gerlier D, Fielding AK, Cattaneo R. 2002. Strength of envelope protein interaction modulates cytopathicity of measles virus. J. Virol. 76:5051–5061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Porotto M, et al. 2011. Spring-loaded model revisited: Paramyxovirus fusion requires engagement of a receptor binding protein beyond initial triggering of the fusion protein. J. Virol. 85:12867–12880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Porotto M, et al. 2006. Paramyxovirus receptor-binding molecules: engagement of one site on the hemagglutinin-neuraminidase protein modulates activity at the second site. J. Virol. 80:1204–1213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Porotto M, Fornabaio M, Kellogg G, Moscona A. 2007. A second receptor binding site on the human parainfluenza 3 hemagglutinin-neuraminidase contributes to activation of the fusion mechanism. J. Virol. 81:3216–3228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Porotto M, Greengard O, Poltoratskaia N, Horga M-A, Moscona A. 2001. Human parainfluenza virus type 3 HN-receptor interaction: the effect of 4-GU-DANA on a neuraminidase-deficient variant. J. Virol. 75:7481–7488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Porotto M, Murrell M, Greengard O, Doctor L, Moscona A. 2005. Influence of the human parainfluenza virus 3 attachment protein's neuraminidase activity on its capacity to activate the fusion protein. J. Virol. 79:2383–2392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Porotto M, et al. 2004. Inhibition of parainfluenza type 3 and Newcastle disease virus hemagglutinin-neuraminidase receptor binding: effect of receptor avidity and steric hindrance at the inhibitor binding sites. J. Virol. 78:13911–13919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Porotto M, Murrell M, Greengard O, Moscona A. 2003. Triggering of human parainfluenza virus 3 fusion protein(F) by the hemagglutinin-neuraminidase (HN): an HN mutation diminishing the rate of F activation and fusion. J. Virol. 77:3647–3654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Porotto M, Palmer SG, Palermo LM, Moscona A. 2012. Mechanism of fusion triggering by human parainfluenza virus type III: communication between the viral glycoproteins during entry. J. Biol. Chem. 287:778–793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Porotto M, Yokoyama C, Orefice G, Kim H-S, Moscona A. 2009. Kinetic dependence of paramyxovirus entry inhibition. J. Virol. 83:6947–6951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Ryan C, et al. 2006. Structural analysis of a designed inhibitor complexed with the hemagglutinin-neuraminidase of Newcastle disease virus. Glycoconj. J. 23:135–141 [DOI] [PubMed] [Google Scholar]
- 59. Sapir A, Avinoam O, Podbilewicz B, Chernomordik LV. 2008. Viral and developmental cell fusion mechanisms: conservation and divergence. Dev. Cell 14:11–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Smith EC, Dutch RE. 2010. Side chain packing below the fusion peptide strongly modulates triggering of the Hendra virus F protein. J. Virol. 84:10928–10932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Smith EC, Popa A, Chang A, Masante C, Dutch RE. 2009. Viral entry mechanisms: the increasing diversity of paramyxovirus entry. FEBS J. 276:7217–7227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Smith KB, Ellis SA. 1999. Standardisation of a procedure for quantifying surface antigens by indirect immunofluorescence. J. Immunol. Methods 228:29–36 [DOI] [PubMed] [Google Scholar]
- 63. Wang Z, Mirza AM, Li J, Mahon PJ, Iorio RM. 2004. An oligosaccharide at the C-terminus of the F-specific domain in the stalk of the human parainfluenza virus 3 hemagglutinin-neuraminidase modulates fusion. Virus Res. 99:177–185 [DOI] [PubMed] [Google Scholar]
- 64. Weissenhorn W, Hinz A, Gaudin Y. 2007. Virus membrane fusion. FEBS Lett. 581:2150–2155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. White JM, Delos SE, Brecher M, Schornberg K. 2008. Structures and mechanisms of viral membrane fusion proteins: multiple variations on a common theme. Crit. Rev. Biochem. Mol. Biol. 43:189–219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Yanagi Y, Takeda M, Ohno S, Hashiguchi T. 2009. Measles virus receptors. Curr. Top. Microbiol. Immunol. 329:13–30 [DOI] [PubMed] [Google Scholar]
- 67. Yuan P, et al. 2011. Structure of the Newcastle disease virus hemagglutinin-neuraminidase (HN) ectodomain reveals a four-helix bundle stalk. Proc. Natl. Acad. Sci. U. S. A. 108:14920–14925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Yuan P, et al. 2005. Structural studies of the parainfluenza virus 5 hemagglutinin-neuraminidase tetramer in complex with its receptor, sialyllactose. Structure 13:803–815 [DOI] [PubMed] [Google Scholar]
- 69. Zaitsev V, et al. 2004. Second sialic acid binding site in Newcastle disease virus hemagglutinin-neuraminidase: implications for fusion. J. Virol. 78:3733–3741 [DOI] [PMC free article] [PubMed] [Google Scholar]