Abstract
Highly pathogenic avian H5N1 influenza viruses remain a pandemic threat. Antiviral drugs such as neuraminidase (NA) inhibitors will be crucial for disease control in the event of a pandemic. Should drug-resistant H5N1 viruses develop, all defense strategies will be compromised. To determine the likelihood and mechanisms of emergence of NA inhibitor-resistant H5N1 variants in humans, we serially passaged two H5N1 viruses, A/Hong Kong/213/03 and A/Turkey/65-1242/06, in normal human bronchial epithelial (NHBE) cells in the presence of oseltamivir, zanamivir, or peramivir. To monitor the emergence of changes associated with the adaptation of H5N1 viruses to humans, we passaged the strains in the absence of drugs. Under pressure of each NA inhibitor, A/Turkey/65-1242/06 developed mutations in the hemagglutinin (HA) (H28R and P194L/T215I) and NA (E119A) proteins that reduced virus binding to α2,3-sialyl receptor and NA activity. Oseltamivir pressure selected a variant of A/Hong Kong/213/03 virus with HA P194S mutation that decreased viral binding to α2,6 receptor. Under peramivir pressure, A/Hong Kong/213/03 virus developed a novel NA mutation, R156K, that reduced binding to all three drugs, caused about 90% loss of NA activity, and compromised replication in NHBE cells. Both strains were eliminated in NHBE cells when they were cultivated in the absence of drugs. Here, we show for the first time that decreased NA activity mediated through NA inhibitors is essential for the adaptation of pandemic H5N1 influenza virus to humans. This ability of decreased NA activity to promote H5N1 infection underlines the necessity to optimize management strategies for a plausible H5N1 pandemic.
INTRODUCTION
Highly pathogenic avian H5N1 influenza A viruses remain a potential pandemic threat due to their high virulence and lethality, global presence, and increasingly diverse avian reservoirs (32, 41, 43). Human H5N1 infection differs substantially from human seasonal influenza virus infection in its pathogenesis. Viral pneumonia is considered the primary cause of death from H5N1 infection, but the virus also disseminates beyond the respiratory tract and is accompanied by hypercytokinemia, leading to multiorgan failure (3, 32, 45). Infectious virus has been isolated from the upper and lower respiratory tract, brain, intestines, feces, blood, cerebrospinal fluid, and even from the placentas and fetuses of pregnant women infected with highly pathogenic H5N1 influenza virus (10). Although human-to-human transmission of the virus has been rare to date, the mutation of the H5N1 virus to allow transmission and rapid spread throughout the human population is still possible.
Vaccination, quarantine, personal protective equipment, and antiviral prophylaxis and treatment are currently the most effective methods to control influenza virus infection. Although vaccination is the preferred method of prophylaxis, at least 3 weeks and two applications are required to produce immunity against currently known influenza viruses. As immunity is often quite strain specific, an entirely new vaccine may have to be prepared against emerging H5N1 antigenic variants. In the face of an emerging pandemic, antiviral drugs will be one of our first control strategies for prevention of influenza; however, our armamentarium is small. To date, two classes of antivirals are licensed to treat influenza virus infections, the adamantanes (amantadine and rimantadine), which target the M2 ion channel of influenza A virus, and neuraminidase (NA) inhibitors (oseltamivir, zanamivir, and peramivir), which target the NA glycoproteins of influenza A and B viruses (11, 24, 27, 28, 39).
Notably, drug-resistant variants that emerge spontaneously or as a consequence of using antiviral therapy can substantially compromise our already limited treatment options (7, 14, 19, 26, 29). Recently, up to 95% of clade 1 avian H5N1 influenza viruses were found resistant to adamantanes though most representatives from other clades remain adamantane sensitive (5). Emergence of drug-resistant H5N1 variants caused by NA natural drift variations or by drug-induced selection pressure has also been reported (15, 25). The fitness of NA inhibitor-resistant H5N1 variants remains unknown. Early studies suggested that seasonal influenza virus resistant to NA inhibitors would be less infective and transmissible in vivo (11, 23); however, the unexpected dominance (∼98%) of oseltamivir-resistant H1N1 viruses from 2007 to 2009 demonstrated that NA inhibitor resistance could enhance fitness and transmissibility (14, 29). Recent data have shown that NA inhibitor-resistant H5N1 variants retain the replication efficiency and pathogenicity of a wild-type virus in vitro and in mice (44), and some data have suggested that NA inhibitor-resistant H5N1 variants are more virulent in a ferret animal model (17, 18). Understanding the mechanisms by which resistance to NA inhibitors may contribute to virulence and transmissibility of H5N1 influenza virus is a key defensive strategy to be prepared for an H5N1 pandemic. A first step toward this is to identify and characterize a number of NA inhibitor-resistant mutations that could arise in highly pathogenic H5N1 viruses under drug-selective pressure in humans.
However, use of the optimal model system must be considered for assessing the emergence of NA inhibitor-resistant variants. Previous studies have demonstrated that the functional balance between the receptor-binding HA activity and receptor-destroying NA activity of the surface influenza virus glycoproteins determines the pattern of emergence of NA inhibitor resistance (24, 39, 40). The disparate hemagglutinin (HA)-NA balance and the differences in sialic acid (SA) receptors between available continuous cell lines and human respiratory epithelial cells significantly limit the suitability of the commonly used cell cultures for phenotypic characterization of NA inhibitor resistance (21, 24, 39). Here, we used primary normal human bronchial epithelial (NHBE) cells, which possess human respiratory tract SA receptors; i.e., they express high concentrations of SA-α2,6-galactose (Gal)-containing receptors and lesser amounts of SA-α2,3-Gal receptors (22). Differentiated NHBE cells functionally and morphologically recapitulate human airway epithelium (22) and, therefore, can be considered an optimal model for assessing influenza virus fitness and predicting the emergence of NA inhibitor-resistant variants among H5N1 influenza viruses in humans. In the present study, we generated drug-resistant mutants of two H5N1 influenza viruses, A/Hong Kong/213/03 (HK/213) and A/Turkey/65-1242/06 (TK/65), by serial passages in NHBE cells under NA inhibitor drug-selective pressure and characterized their viral mutations, growth potential, hemagglutinin receptor specificity, NA protein cleavage activity, level of resistance to anti-influenza virus drugs, and induction of inflammation in human cells. To monitor the emergence of amino acid changes associated with the adaptation of H5N1 viruses to human airway epithelium, the parental strains were also passaged in the absence of drugs. Taken together, our experiments allowed us to assess an important interplay between two biological processes, the emergence of drug resistance and the adaptation of H5N1 influenza virus to the human host.
MATERIALS AND METHODS
Cells, viruses, and compounds.
Madin-Darby canine kidney (MDCK) and human embryonic kidney (293T) cells were obtained from the American Type Culture Collection. MDCK cells transfected with cDNA encoding human 2,6-sialyltransferase (MDCK-SIAT1 cells) were kindly provided by Mikhail N. Matrosovich. Primary NHBE cells were obtained from Cambrex BioScience. All cell cultures were maintained as previously described (16, 21, 22).
The H5N1 influenza viruses A/Hong Kong/213/03 and A/Turkey/65-1242/06 were obtained from the World Health Organization's collaborating laboratories. Viruses were plaque purified in MDCK cells and then passaged once in the allantoic cavities of 10-day-old embryonated chicken eggs for 32 h at 36°C to prepare a virus stock. For the reverse-genetics generation of recombinant wild-type viruses, the eight gene segments of A/Turkey/65-1242/06 (TK/65) virus were amplified by reverse transcriptase PCR (RT-PCR) and cloned into plasmid vector pHW2000 (12); eight plasmids carrying the eight gene segments of A/Hong Kong/213/03 (HK/213) virus were kindly provided by D. J. Hulse-Post. Recombinant viruses were generated by DNA transfection of 293T cells (12), and the point mutations were inserted into the HA or NA genes of wild-type viruses by using a QuickChange site-directed mutagenesis kit (Stratagene, La Jolla, CA). Stock viruses were prepared in MDCK-SIAT1 cells at 37°C for 72 h, and their entire HA and NA genes were sequenced to verify the presence of the mutations. All experimental work with the H5N1 viruses was performed in a biosafety level 3+ laboratory approved for use by the U.S. Department of Agriculture and the U.S. Centers for Disease Control and Prevention.
The NA inhibitors oseltamivir carboxylate (oseltamivir) ([3R,4R,5S]-4-acetamido-5-amino-3-[1-ethylpropoxy]-1-cyclohexene-1-carboxylic acid), zanamivir (4-guanidino-Neu5Ac2en), and peramivir ([1S,2S,3R,4R,1′S]-3-[1′-acetylamino-2′-ethyl]butyl-4-[(aminoimino)-methyl]amino-2-hydroxycyclopentane-1-carboxylicacid) were provided by Hoffmann-La Roche, Ltd. The compounds were dissolved in sterile distilled water, and aliquots were frozen at −70°C until used.
Drug susceptibility assay in NHBE cells.
The drug susceptibility of A/Hong Kong/213/03 (H5N1) and A/Turkey/65-1242/06 (H5N1) influenza viruses was determined by virus reduction assay in NHBE cells (16). NHBE cells were inoculated by exposure of the apical side to H5N1 viruses at a multiplicity of infection (MOI) of 0.1 in the presence of oseltamivir (0, 0.001, 0.01, 0.1, 1, 10, or 100 μM), zanamivir (0, 0.001, 0.01, 0.1, 1, 10, or 100 μM), or peramivir (0, 0.001, 0.01, 0.1, 1, 10, or 100 μM). After a 1-h incubation, the inoculum was removed, and the cells were incubated for another 24 h. Viruses released into the apical compartment of NHBE cells were harvested by the apical addition and collection of 300 μl of medium, which was allowed to equilibrate for 30 min. The virus titer was determined as the number of PFU/ml in MDCK cells. The drug concentration that caused a 50% decrease in the PFU titer, in comparison to control wells without drug, was defined as the 50% effective concentration (EC50). The results of three independent experiments were averaged.
Generation of the H5N1 influenza virus variants with decreased susceptibility to NA inhibitors after passages in NHBE cells.
A/Hong Kong/213/03 (H5N1) and A/Turkey/65-1242/06 (H5N1) influenza viruses were cultivated in NHBE cells in the presence or absence of increasing concentrations of NA inhibitor (oseltamivir, zanamivir, or peramivir). The first passage of the viruses under NA inhibitor-selective pressure was performed at a concentration that was comparable to the EC50. Differentiated NHBE cell cultures were washed extensively with sterile phosphate-buffered saline (PBS) and then inoculated via the apical side with mixtures of H5N1 virus at an MOI of 0.1 and NA inhibitor in 100 μl of inoculum. After a 1-h incubation, the inoculum was removed, and the cells were then incubated at 37°C for 72 h. Viruses released into the apical compartment of NHBE cells were harvested by the apical addition and collection of 300 μl of medium and allowed to equilibrate for 30 min, and the HA titer was determined using 0.5% turkey erythrocytes. After the first passage, the cultured H5N1 viruses were repassaged in medium containing twice the drug concentration used in the previous passage. Both viruses, A/Hong Kong/213/03 (H5N1) and A/Turkey/65-1242/06 (H5N1), were maintained in culture a total of 15 times, at various concentrations of NA inhibitor (drug concentrations ranged from 0.6 nM to 480 nM) (see Tables S1 and S2 in the supplemental material), with harvests and characterization of virus stocks by the hemagglutination titer after each passage. Viruses that had grown to a titer of at least 2 HA units were used to reinfect NHBE cells at an increased drug concentration (2×); if no hemagglutination was observed, the passage was repeated with decreased concentrations of NA inhibitor until a positive HA titer was detected. The parental viruses were also passaged in parallel in the absence of NA inhibitors.
Infectivity of H5N1 influenza viruses.
The infectivity of H5N1 viruses was determined by PFU count and the 50% egg infectious dose (EID50). Briefly, confluent MDCK-SIAT1 cells were incubated at 37°C for 1 h with 10-fold serial dilutions of virus. The cells were then washed and overlaid with minimal essential medium containing 0.3% bovine serum albumin and 0.9% Bacto agar. After 3 days of incubation at 37°C, the cells were stained with 0.1% crystal violet in 10% formaldehyde solution, and the PFU count per milliliter and plaque size of any 10 plaques were determined using a Finescale Comparator (Los Angeles, CA).
The EID50 was determined in 10-day-old chicken eggs with 10-fold serially diluted viruses that were incubated for 48 h at 37°C and calculated by the Reed-Muench method (35).
Replication kinetics.
To determine multistep growth curves in NHBE cells, triplicate cell cultures growing in 12-mm-diameter inserts were washed extensively with sterile PBS to remove mucus secretions on the apical surface prior to infection and then were inoculated via the apical side with each recombinant H5N1 virus at an MOI of 0.1. After a 1-h incubation, the inoculum was removed. Viruses released into the apical compartment of NHBE cells were harvested at the time points indicated on the figures by the apical addition and collection of 300 μl of medium, which was allowed to equilibrate for 30 min. The virus titers were determined as log10 PFU/ml in MDCK cells.
NA enzyme activity and kinetics.
A modified fluorometric assay was used to determine the NA activity of the recombinant H5N1 viruses (34). We measured the NA enzyme kinetics at pH 6.5 with 33 mM 2-(N-morpholino)ethanesulfonic acid hydrate (MES; Sigma-Aldrich, St. Louis, MO), 4 mM CaCl2, and the fluorogenic substrate 2′-(4-methylumbelliferyl)-α-d-N-acetylneuraminic acid ([MUNANA] final substrate concentration, 0 to 2,000 μM; Sigma-Aldrich, St. Louis, MO). All H5N1 viruses were standardized to an equivalent dose of 107.5 PFU/ml. The reaction was conducted at 37°C in a total volume of 50 μl, and the fluorescence of released 4-methylumbelliferone was measured every 92 s for 45 min in a Fluoroskan II instrument (Labsystems, Vienna, VA) using excitation and emission wavelengths of 355 nm and 460 nm, respectively. To measure the inhibitory effect of oseltamivir, zanamivir, or peramivir on NA activity, H5N1 viruses were preincubated for 30 min at 37°C in the presence of various concentrations of the drugs (0.00005 to 100 μM). The kinetic parameters Michaelis-Menten constant (Km), maximum velocity of substrate conversion (Vmax), and inhibitory constant (Ki) of the NAs were calculated by fitting the data to the appropriate Michaelis-Menten equations by using nonlinear regression in the commercially available GraphPad Prism, version 5, software (GraphPad Software, La Jolla, CA).
NA enzyme inhibition assay.
Recombinant H5N1 viruses were standardized to equivalent NA activity and incubated for 30 min at 37°C with NA inhibitors at concentrations of 0.00005 to 100 μM with MUNANA (Sigma-Aldrich, St. Louis, MO) as a substrate. After 1 h, the reaction was terminated by the addition of 14 mM NaOH, and fluorescence was quantified in a Fluoroskan II (Labsystems, Vienna, VA) fluorometer. The 50% inhibitory concentration (IC50) of the NA inhibitor was determined by plotting the dose-response curve of inhibition of NA activity as a function of the compound concentration. Values are the means of two to three independent determinations.
Virus sequence analysis.
Viral RNAs were isolated from virus-containing cell culture fluid after transfection or after passages in NHBE cells by using an RNeasy Minikit (Qiagen, Germantown, MD). Samples were reverse transcribed and analyzed by PCR using universal primers specific for the HA and NA gene segments, as described previously (13). Sequencing was performed by the Hartwell Center for Bioinformatics and Biotechnology at St. Jude. The DNA template was sequenced by using rhodamine or dichlororhodamine (drhodamine) dye terminator cycle sequencing Ready Reaction Kits with AmpliTaq DNA Polymerase FS (PerkinElmer Applied Biosystems, Waltham, MA) and synthetic oligonucleotides. Samples were analyzed in a Perkin-Elmer Applied Biosystems DNA sequencer (model 373 or 377). DNA sequences were completed and edited by using a Lasergene sequence analysis software package (DNASTAR).
Receptor-binding assay.
The binding of recombinant H5N1 influenza viruses to fetuin (containing α2,3- and α2,6-linked sialyl receptors) was measured in a direct solid-phase assay using the immobilized virus and horseradish peroxidase-conjugated fetuin, as described previously (9). The affinity of viruses for synthetic 3′- and 6′-sialylglycopolymers obtained by conjugation of a 1-N-glycyl derivative of 3′- or 6′-sialyllactose (3′SL or 6′SL) or 3-aminopropylglycoside of 3′- or 6′-sialyllactosamine (3′SLN or 6′SLN) with poly(4-phenylacrylate) (4) was measured in a competitive assay based on the inhibition of binding to peroxidase-labeled fetuin (20). Association constant (Kass) values were determined as sialic acid (Neu5Ac) concentration at the point Amax/2 (where Amax is maximum absorbance) on Scatchard plots.
Minigenome assay for polymerase activity.
Subconfluent monolayers of 293T cells (7.5 × 105 cells in 35-mm dishes) were transfected with the luciferase reporter plasmid (enhanced green fluorescent protein [EGFP] open reading frame in pHW72-EGFP replaced with the firefly luciferase gene) (38) and a mix of PB2, PB1, PA and nucleoprotein (NP) expression plasmids (HK/213, TK/65, or mutated) in quantities of 1, 1, 1, and 2 μg, respectively. The plasmid pGL4.75(hRluc/CMV), which expresses Renilla luciferase (Promega, Madison, WI), was used as an internal control for a dual-luciferase assay. As a negative control, 293T cells were transfected with the same plasmids, with the exception of the NP expression plasmid. After 24 h of incubation at 33°C, 37°C, or 39°C, cell extracts were harvested and lysed, and luciferase levels were assayed with a dual-luciferase assay system (Promega, Madison, WI) and a BD Monolight 3010 luminometer (BD Biosciences, San Diego, CA). Experiments were performed in triplicate.
Statistical analysis.
The EC50s, virus yield, plaque size, binding to sialyl receptors, NA inhibitor susceptibility, NA enzyme kinetic parameters (IC50, Km, Vmax, and Ki), and polymerase activities of ribonucleoprotein (RNP) complexes of wild-type and mutant H5N1 influenza viruses were compared either by analysis of variance (ANOVA) or by unpaired t test. A probability value of 0.05 was prospectively chosen to indicate that the findings were not the result of chance alone.
RESULTS
Susceptibility of A/Hong Kong/213/03 (H5N1) and A/Turkey/65-1242/06 (H5N1) influenza viruses to NA inhibitors in NHBE cells.
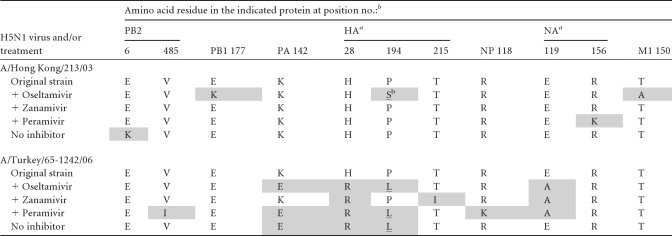
To test the susceptibility to NA inhibitors (oseltamivir, zanamivir, and peramivir) of two H5N1 influenza virus strains that belong to different clades of the H5 HA phylogenetic tree (A/Hong Kong/213/03 and A/Turkey/65-1242/06), we performed a virus reduction assay in NHBE cells (16). A/Hong Kong/213/03 virus was slightly more resistant to oseltamivir and zanamivir (mean EC50 increase, 2.0-fold [P < 0.05] and 2.5-fold for oseltamivir and zanamivir, respectively) and slightly more susceptible to peramivir (mean EC50 decrease, 1.7-fold; P < 0.05) than A/Turkey/65-1242/06 virus (Fig. 1). Thus, the two viruses differed in their susceptibilities to the NA inhibitors in differentiated NHBE cultures. The EC50 values were selected as the first-passage concentrations of three antiviral agents to obtain drug-resistant mutants of both H5N1 viruses in human cells (see Tables S1 and S2 in the supplemental material).
Fig 1.
NA inhibitors (oseltamivir, zanamivir, and peramivir) reduce the influenza virus yield in NHBE cells. Cells were infected with A/Hong Kong/213/03 (H5N1) (A) or A/Turkey/65–1242/06 (H5N1) (B) virus at an MOI of 0.1 in the presence of NA inhibitors. After a 1-h incubation, the inoculum was removed, and the cells were incubated for another 24 h. Viruses released into the apical compartment of NHBE cells were harvested by the apical addition and collection of 300 μl of medium allowed to equilibrate for 30 min. The virus titer was determined by plaque assay in MDCK cells. The drug concentration that caused a 50% decrease in the PFU titer in comparison to control wells without drug was defined as the EC50. Values are the means ± standard deviations of three independent experiments.
Generation of H5N1 mutants resistant to NA inhibitors in NHBE cells.
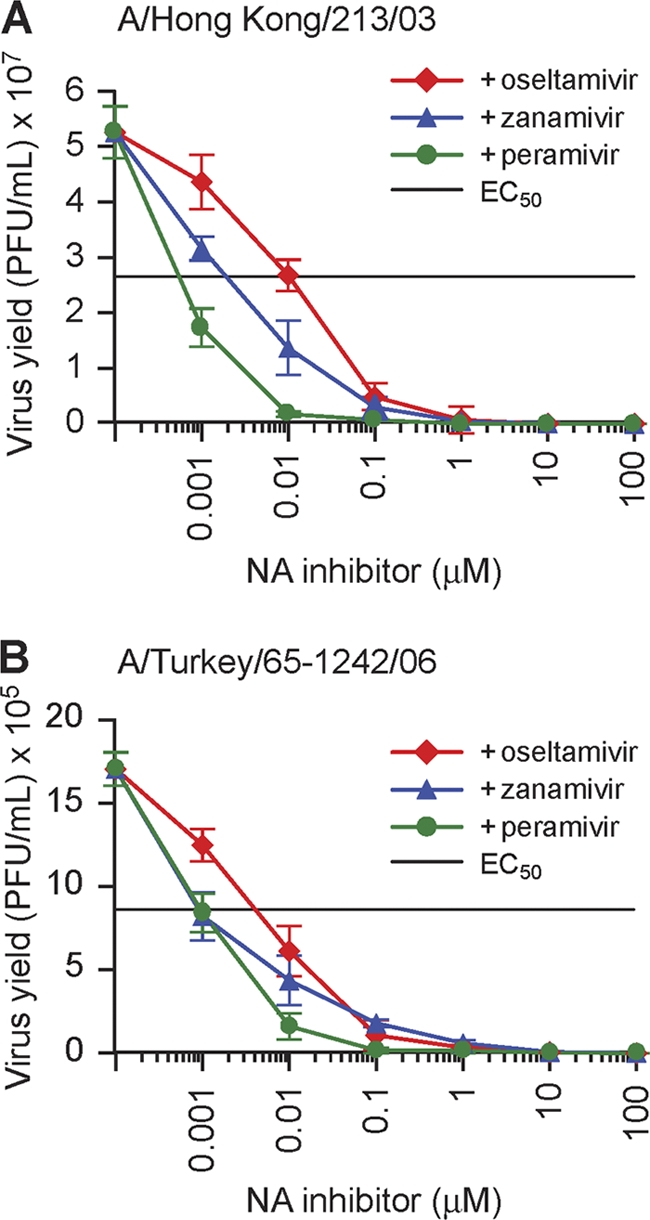
To determine whether drug-resistant H5N1 mutants could be selected ex vivo, we serially passaged A/Hong Kong/213/03 (H5N1) and A/Turkey/65-1242/06 (H5N1) strains 15 times in the presence of increasing concentrations of NA inhibitors in NHBE cells to provide an opportunity for selection of efficiently adapted and resistant phenotypes. We examined the HA and NA mutations of the virus progenies by sequencing (see Tables S1 and S2 in the supplemental material) and their virus yields by plaque assay in MDCK cells after each passage (Fig. 2). To monitor the emergence of any adaptive amino acid changes, we maintained the parental viruses in culture in parallel without any selective pressure.
Fig 2.
Generation of variant influenza viruses with decreased susceptibility to NA inhibitors in NHBE cells. Highly pathogenic H5N1 influenza viruses were cultivated in NHBE cells in the presence or absence of increasing or decreasing concentrations of NA inhibitor (oseltamivir, zanamivir, or peramivir). A/Hong Kong/213/03-like (H5N1) (A) and A/Turkey/65-1242/06-like (H5N1) (B) influenza virus variants with decreased susceptibility to NA inhibitors in NHBE cells were generated. At each passage, plaque assays were performed in MDCK cells to test the infectivity (as log10 PFU/ml) of the viruses.
Analysis of the A/Hong Kong/213/03 virus following culture in the presence of oseltamivir revealed the largest decrease in plaque number at passage 12 (P12) (3.1 ± 0.2 log10 PFU/ml) (Fig. 2A), which was associated with the selection of a P194S HA mutation (H5 HA numbering here and throughout the text). Passage of the A/Hong Kong/213/03 virus in the presence of zanamivir caused the largest reduction in plaque number at P11 (3.0 ± 0.2 log10 PFU/ml) (Fig. 2A) but did not result in selection of any HA or NA mutations. Cultivation of A/Hong Kong/213/03 virus in the presence of peramivir generated an NA mutation at residue 156 (N2 numbering here and throughout the text), which was first detected in a mixed viral population at P6 (see Table S1 in the supplemental material). Importantly, when we cultivated A/Hong Kong/213/03 virus in the absence of any NA inhibitor in NHBE cells, a mixed viral population was detected by plaque morphology in culture supernatants at P10 and P11 that were followed by complete elimination of virus yield at P12. To assay whether the A/Hong Kong/213/03 (H5N1) strain could still be adapted to human cells, we passaged P11 virus progeny once in embryonated chicken eggs; however, no viable virus was detected after two further passages in NHBE cells (Fig. 2A, black dashed line).
Analysis of the A/Turkey/65-1242/06 virus maintained in culture in the presence of oseltamivir in NHBE cells detected the emergence of three mutations, H28R, G46E, and P194L, in the HA protein at P3 (see Table S2 in the supplemental material). However, the G46E HA mutation was no longer detected after P7 when mutation in the second surface glycoprotein NA at residue 119 became dominant. Passages of the A/Turkey/65-1242/06 strain in the presence of zanamivir or peramivir generated two amino acid changes in HA (H28R and T215I or H28R and P194L, respectively), and one change in NA (E119A) by the end of the passaging protocol; the observed changes became dominant as early as P3. The largest decrease in virus yield was observed at P8 (Fig. 2B) after three preceding passages that contained mixed viral populations, indicating that mutations in other genes may have been selected. When we cultivated A/Turkey/65-1242/06 virus in the absence of any drug, a viral population containing two HA mutations (H28R and P194L) was detected in culture supernatants at P5 (see Table S2). Because no viable virus was detected at P6, we assayed whether A/Turkey/65-1242/06 (H5N1) virus could still be recovered in NHBE cells by cultivating P5 virus progeny once in chicken eggs, followed by passaging in human cells. Notably, as with A/Hong Kong/213/03 (H5N1) strain, no virus was detected after two further passages in differentiated NHBE cultures (Fig. 2B, black dashed line).
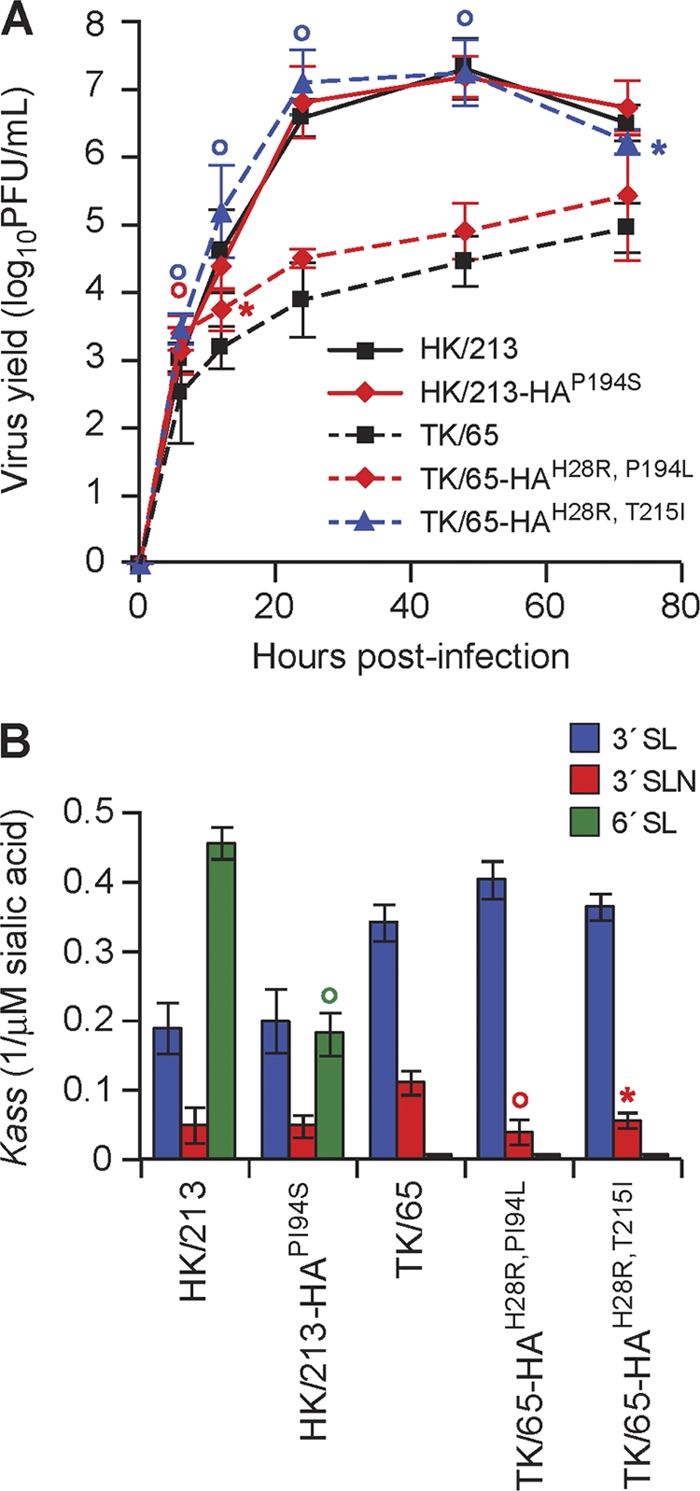
Sequence analysis of H5N1 selected variants.
To monitor the emergence of all amino acid changes that occurred in H5N1 influenza viruses during cultivation in NHBE cells, we sequenced the complete genomes of eight selected variants by the end of the passaging protocol (Table 1). Sequence analysis mapped the acquired mutations to HA, NA, nucleoprotein (NP), matrix 1 (M1) and all three polymerase proteins (PB1, PB2, and PA). A total of 11 amino acid substitutions affecting five viral proteins were involved in the adaptation of A/Hong Kong/213/03 (H5N1) and A/Turkey/65-1242/06 (H5N1) strains to human cells. Passage of A/Hong Kong/213/03 virus in the presence of oseltamivir resulted in the detection not only of a P194S HA mutation leading to acquisition of the potential glycosylation site but also of two additional mutations, E177K in PB1 protein and T150A in M1 protein (Table 1). The E6K PB2 mutation was observed in a mixed viral population recovered after P11 in NHBE cells in the absence of drug. Taking into consideration that we were unable to continue further cultivation of A/Hong Kong/213/03 virus in human cells after P11 (Fig. 2A), this PB2 substitution may have contributed to an unviable phenotype in nature.
Table 1.
Amino acid substitutions identified in selected H5N1 influenza viruses
Sequence analysis of the whole genome of A/Turkey/65-1242/06 (H5N1) virus passaged in the presence of oseltamivir identified two mutations (H28R and P194L) in HA, one mutation (E119A) in NA, and one mutation (K142E) in PA proteins (Table 1). Because the same mutations were selected in the HA and PA proteins when H5N1 virus was cultivated ex vivo without any selective pressure, we concluded that K142E PA and H28R P194L HA changes are necessary for the adaptation of A/Turkey/65-1242/06 virus to replicate in human cells. We also identified additional amino acid substitutions in PB2 (V485I) and NP (R118K) proteins in the variant selected after 15 passages in the presence of peramivir (Table 1).
Effect of HA amino acid substitutions on viral growth and receptor specificity.
To study the effect of HA amino acid substitutions that were acquired during passages of H5N1 viruses in the presence or absence of NA inhibitors in NHBE cells on viral biological properties, we used the reverse-genetics technique to generate recombinant viruses carrying these HA mutations. Specifically, we introduced the P194S mutation into the background of recombinant A/Hong Kong/213/03 (HK/213) influenza virus (yielding the construct HK/213-HAP194S) and H28R P194L and H28R T215I changes into the background of recombinant A/Turkey/65-1242/06 (TK/65) influenza virus (yielding the constructs TK/65-HAH28R,P194L and TK/65-HAH28R,T215I). All recombinant viruses were successfully rescued from transfected 293T cells, and virus stocks were prepared in MDCK-SIAT1 cells, which exhibit more α2,6-linked terminal SA than α2,3-linked terminal SA on the cell surface (21), rather than in MDCK cells to avoid any “avian-type” background exposure. Sequence analysis of the stock viruses and individual plaques obtained in MDCK-SIAT1 cells revealed that the introduced HA mutations were stably maintained in all viruses, and no additional HA or NA mutations were observed (data not shown).
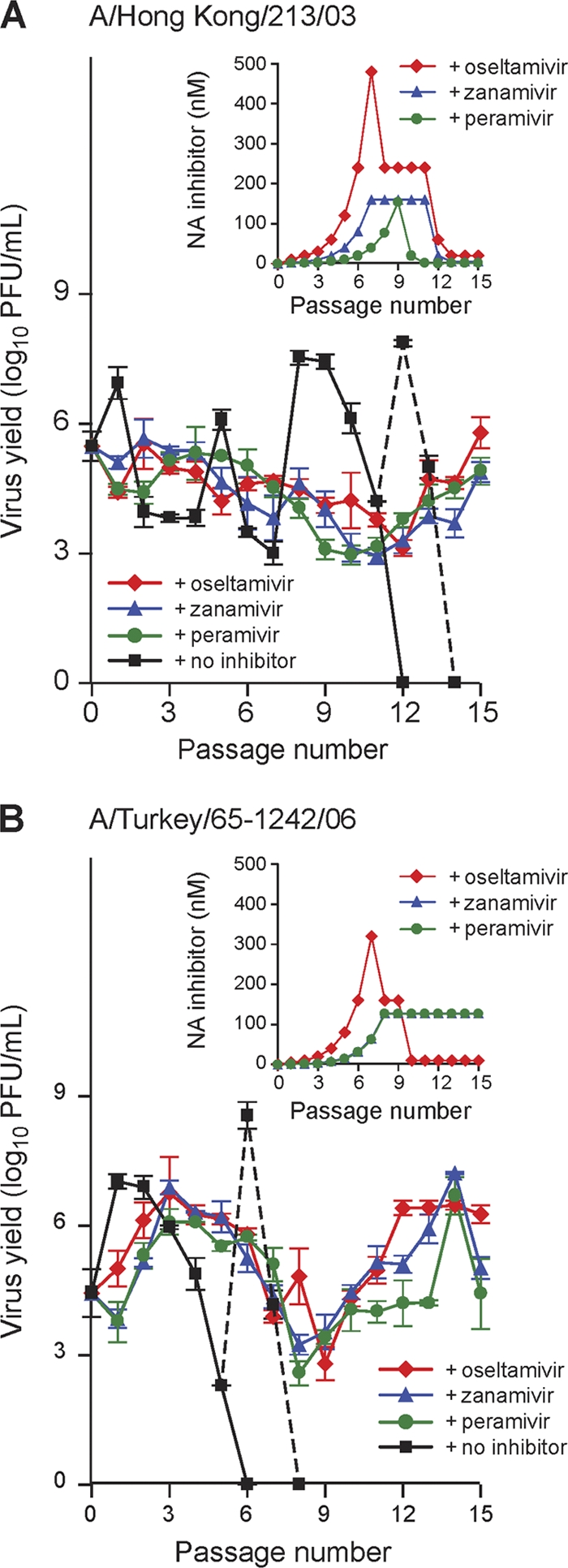
We first studied the growth of HK/213-HAP194S, TK/65-HAH28R,P194L, and TK/65-HAH28R,T215I variants in eggs and MDCK-SIAT1 cells (Table 2). None of the variants grew to significantly higher titers in eggs than their respective wild-type viruses (P < 0.05). However, the yields and plaque sizes of HK/213-HAP194S and TK/65-HAH28R,T215I viruses increased in MDCK-SIAT1 cells (1.1- and ∼2.9-fold, respectively) compared to those of their parental wild-type strains (P < 0.05) (Table 2). To further evaluate the replication ability of recombinant H5N1 viruses carrying different HA mutations, we assayed their viral yields in comparison with respective wild-type strains after multiple replication cycles in NHBE cells (Fig. 3A). The replication ability of the HK/213-HAP194S variant did not differ from that of the HK/213 wild-type virus. TK/65-HAH28R,P194L grew to significantly higher titers than TK/65 only at 6 and 12 h after infection (∼0.8 logs; P < 0.05), and the yield of the TK/65-HAH28R,T215I mutant was significantly higher than that of wild-type virus at all postinfection time points (P < 0.05) (Fig. 3A).
Table 2.
Growth characteristics of recombinant H5N1 influenza viruses
| H5N1 virus | Virus yield in: |
Plaque size (mm)c | |
|---|---|---|---|
| Eggs (log10 EID50/ml ± SD)a | MDCK-SIAT1 cells (log10 PFU/ml ± SD)b | ||
| HK/213 | 8.3 ± 0.1 | 6.9 ± 0.1 | 0.4 ± 0.1 |
| HK/213-HAP194S | 7.3 ± 0.1*d | 7.6 ± 0.5* | 1.3 ± 0.2* |
| HK/213-NAR156K | 6.3 ± 0.1* | 5.5 ± 0.3* | 0.3 ± 0.1 |
| TK/65 | 7.5 ± 0.1 | 5.4 ± 0.1 | 0.8 ± 0.2 |
| TK/65-HAH28R,P194L | 6.9 ± 0.3* | 4.9 ± 0.1* | 0.9 ± 0.2 |
| TK/65-HAH28R,T215I | 7.3 ± 0.1 | 6.0 ± 0.2* | 1.9 ± 0.3* |
| TK/65-NAE119A | 7.9 ± 0.1* | 5.3 ± 0.2 | 0.5 ± 0.4 |
Values are from three independent determinations. The EID50 was determined in 10-day-old chicken eggs with 10-fold serially diluted viruses that were incubated for 48 h at 37°C and calculated by the Reed-Muench method (35).
Values are from three independent determinations. The PFU count was determined in MDCK-SIAT1 cells by plaque assay after 3 days of incubation at 37°C with 10-fold serially diluted viruses.
Values are mean plaque diameter ± standard deviation as measured by using a Finescale Comparator.
*, P < 0.05 compared with value for respective wild-type virus (one-way ANOVA).
Fig 3.
Replication and receptor specificity of drug-resistant H5N1 viruses.(A) Replication of HK/213, HK/213-HAP194S, TK/65, TK/65-HAH28R,P194L, and TK/65-HAH28R,T215I viruses in NHBE cells. NHBE cell cultures were infected via the apical side with each virus at an MOI of 0.1. The progeny viruses released from the apical surface of infected cultures were collected at the indicated time points and titrated in MDCK cells by plaque assay. Representative results expressed as log10 PFU/ml from three independent experiments are shown. *, P < 0.05; °, P < 0.01 (compared with the value for respective wild-type virus, unpaired t test, or one-way ANOVA). (B) Receptor specificity of HK/213, HK/213-HAP194S, TK/65, TK/65-HAH28R,P194L, and TK/65-HAH28R,T215I viruses. Association constants (Kass) of virus complexes with synthetic sialylglycopolymers conjugated to 3′SL(N) and 6′SL are shown. Higher Kass values indicate stronger binding. Values are the means ± standard deviations of four independent experiments.*, P < 0.05; °, P < 0.01 (compared with the value for respective wild-type virus, unpaired t test, or one-way ANOVA).
To determine whether identified HA mutations affect the HA affinity to sialyl receptors, we next measured the receptor specificity of generated recombinant H5N1 viruses to synthetic sialic substrates (3′SL/N and 6′SL/N) (Fig. 3B). HK/213-HAP194S virus showed significantly less binding to “human-type” 6′SL receptor than did wild-type HK/213 virus (2.5-fold difference; P < 0.01). The binding pattern to the second human-type receptor (6′SLN) was negligible among all viruses tested (data not shown). Furthermore, as shown by the Kass values, TK/65-HAH28R,P194L and TK/65-HAH28R,T215I variants exhibited a significant decrease in affinity toward avian-type 3′SLN polymer from that of the wild-type TK/65 (∼2.4-fold; P < 0.05) (Fig. 3B).
Effect of NA amino acid substitutions on viral growth, NA inhibitor susceptibility, and NA enzyme kinetics.
To study the impact of NA amino acid substitutions that were acquired during passages of A/Hong Kong/213/03 (H5N1) and A/Turkey/65-1242/06 (H5N1) viruses in the presence or absence of NA inhibitors in NHBE cells on viral biological properties, we introduced the R156K mutation into the background of HK/213 virus (yielding the construct HK/213-NAR156K) and the E119A mutation into the background of TK/65 virus (yielding the construct TK/65-NAE119A). Similar to H5N1 recombinant viruses carrying mutations in the HA protein, HK/213-NAR156K and TK/65-NAE119A recombinant viruses were successfully rescued from transfected 293T cells, and virus stocks were prepared in MDCK-SIAT1 cells. Sequence analysis of the stock viruses and individual plaques obtained in MDCK-SIAT1 cells suggested that R156K and E119A NA mutations were stably maintained in the respective HK/213 and TK/65 virus backgrounds, and no additional HA or NA mutations were observed (data not shown).
We first assessed whether the introduced NA changes affected growth of recombinant H5N1 viruses in vitro (Table 2). HK/213-NAR156K replicated to significantly lower titers both in eggs and MDCK-SIAT1 cells than did wild-type HK/213 virus (1.4 to 2.0 logs; P < 0.05). The TK/65-NAE119A mutant grew comparably in cell culture and to significantly higher titers in eggs than TK/65 (P < 0.05) (Table 2). Multistep growth curves showed comparable titers of TK/65 and TK/65-NAE119A viruses in differentiated cultures of NHBE cells at all time points (Fig. 4A). In contrast, the yield of HK/213-NAR156K was only approximately 81% of that of the recombinant wild-type HK/213 at 24, 48, and 72 h after infection (P < 0.01) (Fig. 4A).
Fig 4.
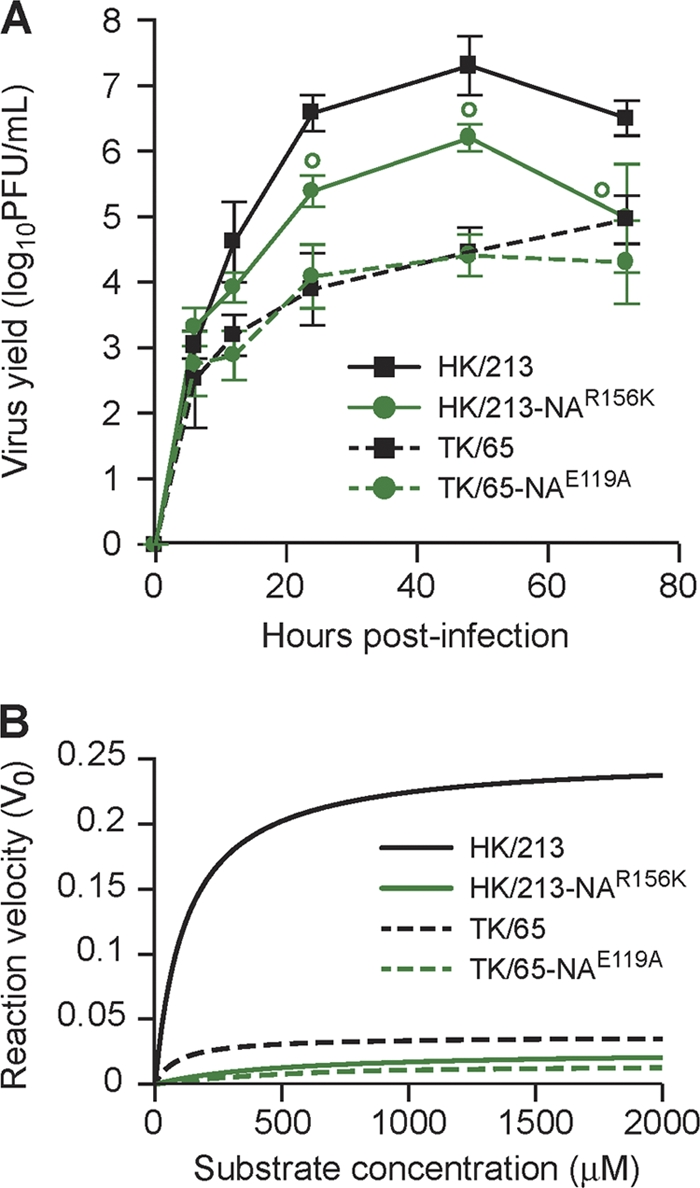
Replication and neuraminidase activity in drug-resistant H5N1 viruses. (A) Replication of HK/213, HK/213-NAR156K, TK/65, and TK/65-NAE119A viruses in NHBE cells. NHBE cell cultures were infected via the apical side with each virus at an MOI of 0.1. The progeny viruses released from the apical surface of infected cultures were collected at the indicated time points and titrated in MDCK cells by plaque assay. Representative results expressed as log10 PFU/ml from three independent experiments are shown. °, P < 0.01, compared with the value for respective wild-type virus by an unpaired t test. (B) NA enzyme kinetics of the recombinant HK/213, HK/213-NAR156K, TK/65, and TK/65-NAE119A viruses. Substrate conversion velocity (V0) of NA is shown as a function of substrate concentration. Fluorogenic MUNANA substrate was used at a final concentration of 0 to 2,000 μM. The viruses were standardized to an equivalent dose of 107.5 PFU/ml. Fluorescence was measured every 92 s for 45 min at 37°C, using excitation and emission wavelengths of 355 and 460 nm, respectively.
An enzymatic NA inhibition assay was used to characterize the susceptibilities of H5N1 recombinant HK/213, HK/213-NAR156K, TK/65, and TK/65-NAE119A viruses to NA inhibitors. HK/213-NAR156K and TK/65-NAE119A viruses were moderately more resistant to oseltamivir and peramivir (2.2- to 67.4-fold increase in mean IC50 values) and markedly more resistant to zanamivir (∼245-fold increase in mean IC50) than were respective wild-type viruses (Table 3). We observed that NA proteins harboring the E119A and R156K mutations exhibited significantly lower affinities for the substrate (mean Km decrease, 8.4-fold) than the respective wild-type virus NAs (Table 3) (P < 0.01). The inhibition constant (Ki) values of all NA glycoproteins were consistent with their IC50s, clearly indicating that the reduced susceptibility to the NA inhibitors was caused by decreased affinity of the mutant NAs to the antiviral drugs. We also determined NA enzymatic activity (Vmax) values for each of the generated recombinant H5N1 viruses (Fig. 4B) and calculated their Vmax ratios in relation to that of the respective wild-type virus NA (Table 3). NA proteins with mutations at residues 119 and 156 significantly reduced the NA activities of the respective wild-type viruses (Vmax ratios 0.5 and 0.1, respectively) (Table 3 and Fig. 4B).
Table 3.
Enzymatic properties of the neuraminidase of recombinant H5N1 influenza viruses
| H5N1 recombinant virus | Kinetics of NA |
|||||||
|---|---|---|---|---|---|---|---|---|
| Mean IC50 ± SD (nM) with:a |
Mean Km ± SD (μM)b | Vmax ratioc | Mean Ki ± SD (nM) with:d |
|||||
| Oseltamivir carboxylate | Zanamivir | Peramivir | Oseltamivir carboxylate | Zanamivir | Peramivir | |||
| HK/213 | 12.2 ± 1.3 | 4.4 ± 0.1 | 1.7 ± 0.1 | 110.5 ± 28.5 | 1.0 | 4.8 ± 0.5 | 1.8 ± 0.1 | 0.7 ± 0.1 |
| HK/213-NAR156K | 26.5 ± 1.3*e | 1049.0 ± 5.3* | 59.1 ± 0.8* | 520.3 ± 36.2* | 0.1 | 20.0 ± 1.0* | 794.0 ± 3.8* | 44.8 ± 0.6* |
| TK/65 | 39.0 ± 3.4 | 8.3 ± 0.7 | 2.8 ± 0.1 | 78.9 ± 7.3 | 1.0 | 12.5 ± 1.1 | 2.7 ± 0.2 | 0.9 ± 0.1 |
| TK/65-NAE119A | 380.6 ± 9.7* | 2116.3 ± 53.3* | 188.8 ± 16.0* | 528.1 ± 76.0* | 0.5 | 289.2 ± 7.4* | 1607.7 ± 40.5* | 143.4 ± 12.2* |
The NA inhibition assay was performed with H5N1 viruses standardized to equivalent NA activity and incubated with NA inhibitors (0.00005 to 100 μM) and MUNANA substrate. IC50 was determined by plotting the dose-response curve of inhibition of NA activity as a function of the compound concentration. Values represent three independent determinations.
The Km represents a half-maximal catalytic rate. The enzyme kinetic data were fit to the Michaelis-Menten equation using GraphPad Prism, version 5. Values are the means ± standard deviations from one representative experiment done in triplicate.
Ratio of the mutant virus NA Vmax to the Vmax of the respective recombinant wild-type virus NA. The Vmax was calculated using a nonlinear regression of the curve according to the Michaelis-Menten equation.
Determined by enzymatic kinetic analysis and calculated using nonlinear regression of the plot of initial velocity as a function of inhibitor concentration.
*, P < 0.01, compared to respective recombinant wild-type virus (unpaired t test).
Effect of amino acid substitutions in the RNP complex on viral polymerase activity.
To investigate whether the mutations observed in the ribonucleoprotein (RNP) complexes of A/Hong Kong/213/03 (H5N1) and A/Turkey/65-1242/06 (H5N1) viruses that had been passaged in NHBE cells in the presence or absence of NA inhibitors changed viral transcription and replication activity, we analyzed reconstituted RNP complexes in 293T cells by luciferase minigenome assay. We observed that the PB1 E177K amino acid substitution significantly increased polymerase activity of A/Hong Kong/213/03 polymerase complex approximately 117% at 33°C and 37°C but did not change the activity at 39°C(P < 0.05), indicating that PB1 E155K is a temperature-sensitive mutation (Fig. 5A). In contrast, amino acid change E6K in the PB2 protein significantly reduced polymerase activity by 24% at 33°C and 37°C (P < 0.05). Furthermore, single point mutations PA K142E and NP R118K increased polymerase activity of A/Turkey/65-1242/06 RNP complex as much as 170% and 130%, respectively, at all temperatures studied (P < 0.01); however, their stepwise combination did not lead to a further rise (Fig. 5B). In contrast, the amino acid change V485I in the PB2 protein suppressed enzymatic activity by about 40% when it was introduced alone or in any combination, indicating that PB2 V485I is a downregulating mutation.
Fig 5.
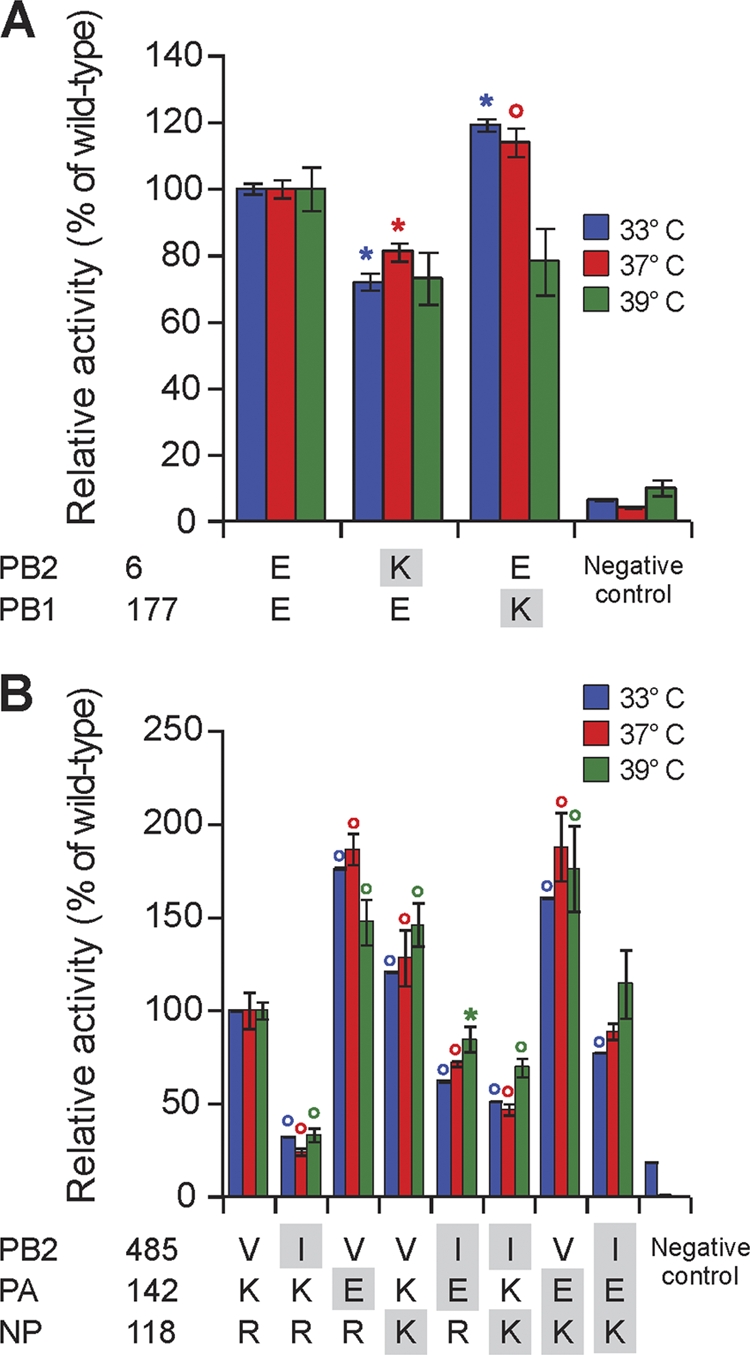
Polymerase activity of ribonucleoprotein complexes of wild-type A/Hong Kong/213/03 (H5N1) (A) and A/Turkey/65–1242/06 (H5N1) (B) viruses and their variants with single point mutations. Amino acid mutations are indicated by shading of a residue below each plot. The polymerase activities were determined by dual-luciferase reporter assay in three independent experiments. The 293T cells were transfected in triplicate with luciferase and Renilla reporter plasmids, with plasmids expressing PB2, PB1, PA, and NP from HK/213, TK/65, or mutated viruses. Cells were incubated at 33°C, 37°C, or 39°C for 24 h, and cell lysates were analyzed to measure firefly luciferase and Renilla activities. The latter was used to normalize transfection efficiency. Values shown represent the means ± standard deviations of activities of each RNP complex relative to that of the respective wild-type virus. *, P < 0.05; °, P < 0.01 (compared with the value for respective wild-type virus by one-way ANOVA).
DISCUSSION
NA inhibitors are an important component of influenza pandemic preparedness. They have broad antiviral spectrum and potency, prophylactic and therapeutic effectiveness, favorable pharmacokinetics, tolerability, and safety (1, 11, 24, 27, 28, 33, 36, 39). However, concerns exist that drug resistance may occur and will reduce the effectiveness of antiviral therapy. The picture would be even starker if drug resistance is linked to enhanced transmissibility or virulence. With the H5N1 influenza virus, such an event could lead to the spread of life-threatening infection, with little benefit from existing NA-inhibitor stockpiles. It is not clear at what frequency NA inhibitor-resistant variants emerge during treatment of patients infected with H5N1 viruses.
In the present study, we demonstrated four patterns of development of HA and NA mutations in two H5N1 strains, A/Hong Kong/213/03 and A/Turkey/65-1242/06, under drug-selective pressure (1). A/Turkey/65-1242/06 strain developed concomitant mutations in the HA (H28R and P194L/T215I) and NA (E119A) genes. Taking into account the balance between the functions of the HA and NA glycoproteins (40), we surmise that this mechanism of resistance involved compensating HA mutations because they resulted in reduced virus binding for the cell receptor 3′SLN and, as a consequence, led to the increased efficiency of viral release from the infected cell, with less dependence on the reduced NA function (2). Oseltamivir pressure selected a variant of A/Hong Kong/213/03 virus with mutation in the HA gene (P194S), which decreased viral binding affinity to 6′SL (3). Under peramivir selective pressure, A/Hong Kong/213/03 (H5N1) virus developed NA mutation R156K. This NA substitution resulted in a 4- to 441-fold reduction in binding to all three NA inhibitors (P < 0.01) and in at least 90% loss of enzyme catalytic activity and was associated with a reduction in replication in eggs, MDCK-SIAT1 cells, and NHBE cells (P < 0.05) (4). No amino acid substitutions were selected in the HA or NA genes of A/Hong Kong/213/03 virus under zanamivir pressure that could lead to overall viral suppression, and no mechanism of resistance was observed. However, because the virus was maintained after 15 sequential passages, we conclude that decreased NA activity mediated by the presence of NA inhibitor is important for H5N1 virus viability in human cells.
To monitor the emergence of amino acid changes associated with the adaptation of highly pathogenic influenza viruses to human airway epithelium, we passaged the parental viruses in parallel in the absence of antivirals. We identified two mutations in the HA protein, H28R and P194L, one mutation in the PA protein, K142E, and one change in the PB2 protein, E6K, that partially and more likely independently controlled adaptation of pandemic viruses to airway epithelium. When we cultured H5N1 viruses in the absence of any NA inhibitor, A/Hong Kong/213/03 and A/Turkey/65-1242/06 viruses were completely eliminated after P11 and P5, respectively. This result indicates that neither virus was able to adapt to the human cells. However, since both viruses were stably maintained after 15 sequential passages in the presence of antivirals, NA inhibitors are probably necessary for the adaptation of H5N1 influenza virus to human epithelium. Taken together, our results show that NA inhibitor resistance arises in NHBE cell cultures due to the development of NA mutations that decrease NA inhibitor-binding affinity and enzyme catalytic activity. These mutations arise with or without concomitant HA mutations, which decrease virus receptor-binding affinity. Highly pathogenic H5N1 viruses can adapt to human airway epithelium because of the reduced NA enzyme activity (achieved either by acquisition of NA mutation [E119A] or the presence of NA inhibitor [zanamivir]) with or without the acquisition of HA amino acid changes that reduce viral binding to the respective cellular receptors. Therefore, we conclude that interplay between two biological processes, the emergence of resistance and adaptation of H5N1 influenza virus to the human host, could play a role in the emergence of a pandemic.
HA amino acid substitutions identified in this study were located either next to the HA receptor-binding pocket (positions 194 and 215) or in the HA stem domain (position 28) (42). Two HA mutations observed at the same position, P194S and P194L, were associated with the acquisition of a potential glycosylation site. HA glycosylation affects the specificity or affinity of influenza viruses for cellular receptors (2, 8, 31). The introduction of carbohydrate side chains adjacent to the receptor-binding site decreases the capacity of the virus to bind to the host cells (31). The most likely explanation is that the acquisition of an oligosaccharide attachment site next to the tip of the HA1 subunit creates steric hindrance that limits the accessibility of the receptor pocket to the cellular SA-containing receptor by this oligosaccharide, thereby reducing the efficiency of virus binding (31). Thus, we speculate that the P194S mutation identified in the HA gene of A/Hong Kong/213/03 (H5N1) virus results in a weak binding affinity to the 6′SL human-type receptor most likely due to the attachment of a carbohydrate residue. Our results also suggest that the decrease in virus binding of TK/65-HAH28R,P194L to 3′SLN was mediated by the single point mutation P194L in HA.
Two amino acid changes in the NA protein, one at the framework residue 119 and the other at the framework residue 156, were selected in H5N1 viruses after passaging in NHBE cultures in the presence of NA inhibitors. The R156K NA substitution is a novel mutation that has not been previously reported to confer resistance to NA antiviral drugs. We observed that both NA mutations were viable and genetically stable and were associated with similar moderate resistance to oseltamivir and peramivir (2.2- to 67.4-fold increase in mean IC50s, which were far below the expected plasma concentrations of 1,244 nM and 30,488 nM, respectively [1, 26]) and substantial resistance to zanamivir (∼245-fold increase in mean IC50, which far exceeded the expected plasma concentration of 142 nM [33]), indicating that E119A and R156K NA changes might result in reduced clinical efficacy of zanamivir but not of peramivir or oseltamivir.
Previous reports have demonstrated that N1 NAs contain a large cavity (150-cavity) adjacent to the active site, which is about 10 Å long and 5 Å wide and deep (37). Both NA mutations, E119A and R156K, occurred at positions that play an important role in the conformation of this cavity. The acidic residue Glu 119 defines the width of the 150-cavity (37). The conserved Arg 156, the side chain of which is located approximately midway between the two other acidic residues, is located at the base of the 150-cavity; therefore, it defines the entrance from the active site into the 150-cavity (37). The NA inhibitor-resistant mutations E119A and R156K could lead to changes in the size and/or structure of the N1 NA 150-cavity. Ala and Lys have shorter side chains than Glu and Arg, respectively; this difference may impede the interaction between HK/213-NAR156K and TK/65-NAE119A mutants and NA inhibitors.
Additionally, our data showed that E119A and R156K changes significantly reduced the activities of the respective mutant NA enzymes (Vmax ratios of 0.5 and 0.1, respectively). However, viral growth was compromised only in the HK/213-NAR156K mutant observed in cultures of MDCK-SIAT1 and NHBE cells, whereas TK/65-NAE119A grew comparably in cell culture and to a significantly higher titer in eggs than wild-type TK/65 (P < 0.05). In our previous study in the ferret model, in which the influenza virus pathogenesis closely resembles that of humans, we demonstrated that A/Turkey/15/06 (H5N1) virus carrying the E119A NA mutation was more virulent (i.e., lethal in 1 of 3 animals) and was associated with significantly higher titers in the lungs and liver and inflammation in the lungs (17). The impact of an NA amino acid substitution at residue 156 on the fitness of highly pathogenic A/Hong Kong/213/03 (H5N1) virus should be the subject of further investigation.
Mutations at five points of the RNP complex (namely E6K and V485I in PB2, E177K in PB1, K142E in PA, and R118K in NP) and one mutation in M1 protein (T150A) were involved in the adaptation of highly pathogenic H5N1 isolates to human airway epithelium. To investigate whether these amino acid changes occur in other highly pathogenic isolates, we analyzed the H5N1 sequences deposited in the Influenza Research Database (data were obtained from the National Institute of Allergy and Infectious Diseases database [http://www.fludb.org]). Two amino acid substitutions, E6K in PB2 and T150A in M1, were not present in any H5N1 strains examined. This can be partially explained by the fact that we were unable to rescue A/Hong Kong/213/03 (H5N1) virus carrying mutation E6K in PB2 from transfected 293T cells in three independent experiments (data not shown). The remaining four mutations (V485I in PB2, E177K in PB1, K142E in PA, and R118K in NP) were found in 0.1% to 0.4% of contemporary H5N1 isolates. We found that substitutions in only the PB1, PA, and NP proteins are sufficient to significantly enhance the transcription and replication activity of viral polymerase complexes. An amino acid change of the same residue 142 in PA occurred in the A/Turkey/65-1242/06 (H5N1) strain in three independent experiments, indicating that this event is not a chance of fluctuation; rather, it is one of the strong viral determinants of the virulence and replication of highly pathogenic H5N1 viruses in humans. We speculate that the increased polymerase activity caused by the identified mutations is necessary for optimized interaction of the H5N1 viral polymerase with the host proteins. In contrast, amino acid changes in the PB2 protein (E6K and V485I) significantly suppressed the polymerase activity of H5N1 RNP complexes, indicating that these changes compromise the infectivity of H5N1 viruses due to the downregulation of their replication ability.
In conclusion, we identified E119A and R156K as the major viral NA amino acid substitutions that are involved in the profile of NA inhibitor resistance of H5N1 influenza viruses. Complete characterization of genetic stability, infectivity, and pathogenicity of identified NA inhibitor-resistant H5N1 viruses in an appropriate animal model is warranted to more accurately predict the outcomes of antiviral treatment in H5N1 virus-infected patients. We also provided for the first time direct evidence that decreased NA activity, mediated through NA inhibitors, is essential for the adaptation of pandemic H5N1 influenza virus to the human airway epithelium. It is worth mentioning that we used primary cultures of NHBE cells, which lack a functional adaptive immune system, which would definitely play a role in virus adaptation and could affect H5N1 influenza virus evolution scenarios. The observed ability of decreased NA enzymatic activity to promote H5N1 infection underlines the necessity for further preclinical studies, which are the only available option for optimizing the prophylactic use of NA inhibitor compounds for persons at high risk of infection with avian influenza viruses. We believe that the obtained results are essential for devising appropriate preventive measures for a plausible H5N1 pandemic.
Supplementary Material
ACKNOWLEDGMENTS
We are especially grateful to Diane J. Hulse-Post for providing the plasmids for A/Hong Kong/213/03 (H5N1) influenza virus. The NA inhibitors oseltamivir, zanamivir, and peramivir were provided by Hoffmann-La Roche, Ltd. We thank Peter F. Wright for helpful discussions and review of the manuscript, Bindumadhav Marathe for excellent technical assistance, Betsy Williford for illustrations, and Angela McArthur for editorial assistance.
This study was supported by the National Institute of Allergy and Infectious Diseases, National Institutes of Health, Department of Health and Human Services, under contract number HHSN266200700005C, by RAS Presidium Grant Molecular and Cell Biology, and by the American Lebanese Syrian Associated Charities.
Footnotes
Published ahead of print 29 February 2012
Supplemental material for this article may be found at http://jvi.asm.org/.
REFERENCES
- 1. Alexander WJ, et al. 2007. Nasal and pharyngeal concentrations of peramivir following intramuscular and intravenous administration in health volunteers, poster A-1410. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother American Society for Microbiology, Washington, DC [Google Scholar]
- 2. Aytay S, Schulze IT. 1991. Single amino acid substitutions in the hemagglutinin can alter the host range and receptor binding properties of H1 strains of influenza A virus. J. Virol. 65:3022–3028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Beigel JH, et al. 2005. Avian influenza A (H5N1) infection in humans. N. Engl. J. Med. 353:1374–1385 [DOI] [PubMed] [Google Scholar]
- 4. Bovin NV, et al. 1993. Synthesis of polymeric neoglycoconjugates based on N-substituted polyacrylamides. Glycoconj. J. 10:142–151 [DOI] [PubMed] [Google Scholar]
- 5. Cheung CL, et al. 2006. Distribution of amantadine-resistant H5N1 avian influenza variants in Asia. J. Infect. Dis. 193:1626–1629 [DOI] [PubMed] [Google Scholar]
- 6. Colman PM. 1994. Influenza virus neuraminidse: structure, antibodies, and inhibitors. Protein Sci. 3:1687–1696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. de Jong MD, et al. 2005. Oseltamivir resistance during treatment of influenza A (H5N1) infection. N. Engl. J. Med. 353:2667–2672 [DOI] [PubMed] [Google Scholar]
- 8. Deom CM, Caton AJ, Schulze IT. 1986. Host cell-mediated selection of a mutant influenza A virus that has lost a complex oligosaccharide from the tip of the hemagglutinin. Proc. Natl. Acad. Sci. USA 83:3771–3775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gambaryan AS, Matrosovich MN. 1992. A solid-phase enzyme-linked assay for influenza virus receptor-binding activity. J. Virol. Methods 39:111–123 [DOI] [PubMed] [Google Scholar]
- 10. Gu J, et al. 2007. H5N1 infection of the respiratory tract and beyond: a molecular pathology study. Lancet 370:1137–1145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hayden FG. 2001. Perspectives on antiviral use during pandemic influenza. Philos. Trans. R. Soc. Lond. B. Biol. Sci. 356:1877–1884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hoffmann E, Neumann G, Kawaoka Y, Hobom G, Webster R. 2000. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. U. S. A. 97:6108–6113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hoffmann E, Stech J, Guan Y, Webster RG, Perez DR. 2001. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 146:2275–2289 [DOI] [PubMed] [Google Scholar]
- 14. Hurt AC, et al. 2009. Emergence and spread of oseltamivir-resistant A(H1N1) influenza viruses in Oceania, South East Asia and South Africa. Antiviral Res. 83:90–93 [DOI] [PubMed] [Google Scholar]
- 15. Hurt AC, et al. 2007. Susceptibility of highly pathogenic A (H5N1) avian influenza viruses to the neuraminidase inhibitors and adamantanes. Antiviral Res. 73:228–231 [DOI] [PubMed] [Google Scholar]
- 16. Ilyushina NA, Govorkova EA, Gray TE, Bovin NV, Webster RG. 2008. A switch to human-like receptor specificity does not affect the neuraminidase-inhibitor susceptibility of influenza A (H5N1) viruses. PLoS Pathog. 4:e1000043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ilyushina NA, Seiler JP, Rehg JE, Webster RG, Govorkova EA. 2010. Effect of neuraminidase inhibitor–resistant mutations on pathogenicity of clade 2.2 A/Turkey/15/06 (H5N1) influenza virus in ferrets. PLoS Pathog. 6:e1000933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kiso M, et al. 2011. Effect of an asparagines-to-serine mutation at position 294 in neuraminidase on the pathogenicity of highly pathogenic H5N1 influenza A virus. J. Virol. 85:4667–4672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Le QM, et al. 2005. Avian flu: isolation of drug-resistant H5N1 virus. Nature 437:1108. [DOI] [PubMed] [Google Scholar]
- 20. Matrosovich MN, et al. 1993. Probing of the receptor-binding sites of the H1 and H3 influenza virus hemagglutinins by synthetic and natural sialosides. Virology 196:111–123 [DOI] [PubMed] [Google Scholar]
- 21. Matrosovich MN, Matrosovich T, Carr J, Roberts NA, Klenk H-D. 2003. Overexpression of the α-2,6-sialyltransferase in MDCK cells increases influenza virus sensitivity to neuraminidase inhibitors. J. Virol. 77:8418–8425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Matrosovich MN, Matrosovich TY, Gray T, Roberts NA, Klenk H-D. 2004. Human and avian influenza viruses target different cell types in cultures of human airway epithelium. Proc. Natl. Acad. Sci. U. S. A. 101:4620–4624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McKimm-Breschkin J, et al. 2003. Neuraminidase sequence analysis and susceptibilities of influenza virus clinical isolates to zanamivir and oseltamivir. Antimicrob. Agents Chemother. 47:2264–2272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. McKimm-Breschkin JL. 2000. Resistance of influenza viruses to neuraminidase inhibitors—a review. Antiviral Res. 47:1–17 [DOI] [PubMed] [Google Scholar]
- 25. McKimm-Breschkin JL, Selleck PW, Usman TB, Johnson MA. 2007. Reduced sensitivity of influenza A (H5N1) to osletamivir. Emerg. Infect. Dis. 13:1354–1357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Memoli MJ, et al. 2011. Multidrug resistant 2009 pandemic influenza A(H1N1) viruses maintain fitness and transmissibility in ferrets. J. Infect. Dis. 203:348–357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Monto AS. 2005. The threat of an avian influenza pandemic. N. Engl. J. Med. 352:323–325 [DOI] [PubMed] [Google Scholar]
- 28. Moscona A. 2008. Medical management of influenza infection. Annu. Rev. Med. 59:397–413 [DOI] [PubMed] [Google Scholar]
- 29. Moscona A. 2009. Global transmission of oseltamivir-resistant influenza. N. Engl. J. Med. 360:953–956 [DOI] [PubMed] [Google Scholar]
- 30. Nobusawa E, et al. 1991. Comparison of complete amino acid sequences and receptor-binding properties among 13 serotypes of hemagglutinins of influenza A viruses. Virology 182:475–485 [DOI] [PubMed] [Google Scholar]
- 31. Ohuchi M, Ohuchi R, Feldmann A, Klenk H-D. 1997. Regulation of receptor binding affinity of influenza virus hemagglutinin by its carbohydrate moiety. J. Virol. 71:8377–8384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Peiris JSM, de Jong MD, Guan Y. 2007. Avian influenza virus (H5N1): a threat to human health. J. Microb. Rev. 20:243–267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Peng AW, Milleri S, Stein DS. 2000. Direct measurement of the anti-influenza agent zanamivir in the respiratory tract following inhalation. Antimicrob. Agents Chemother. 44:1974–1976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Potier M, Mameli L, Belisle M, Dallaire L, Melanxon SB. 1979. Fluorometric assay of neuraminidase with a sodium (4-methylumbelliferyl-alpha-d-N-acetylneuraminate) substrate. Anal. Biochem. 94:287–296 [DOI] [PubMed] [Google Scholar]
- 35. Reed LJ, Muench H. 1938. A simple method for estimating fifty percent endpoints. Am. J. Hyg. 27:493–497 [Google Scholar]
- 36. Roche Pharmaceuticals 2006. Tamiflu (oseltamivir carboxylate) capsules and for oral suspension. Package insert. Hoffmann-La Roche Inc., Nutley, NJ: http://www.tamiflu.com [Google Scholar]
- 37. Russell RJ, et al. 2006. The structure of H5N1 avian influenza neuraminidase suggests new opportunities for drug design. Nature 443:45–49 [DOI] [PubMed] [Google Scholar]
- 38. Salomon R, et al. 2006. The polymerase complex genes contribute to the high virulence of the human H5N1 influenza virus isolate A/Vietnam/1203/04. J. Exp. Med. 203:689–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Tisdale M. 2000. Monitoring of viral susceptibility: new challenges with the development of influenza NA inhibitors. Rev. Med. Virol. 10:45–55 [DOI] [PubMed] [Google Scholar]
- 40. Wagner R, Matrosovich MN, Klenk H-D. 2002. Functional balance between haemagglutinin and neuraminidase in influenza virus infections. Rev. Med. Virol. 12:159–166 [DOI] [PubMed] [Google Scholar]
- 41. Webster RG, Govorkova EA. 2006. H5N1 influenza—continuing evolution and spread. N. Engl. J. Med. 355:2174–2177 [DOI] [PubMed] [Google Scholar]
- 42. Wiley DC, Skehel JJ. 1987. The structure and function of the hemagglutinin membrane glycoprotein of influenza virus. Annu. Rev. Biochem. 56:365–394 [DOI] [PubMed] [Google Scholar]
- 43. World Health Organization 2011. Technical update: current evolution of avian influenza H5N1 viruses. World Health Organization, Geneva, Switzerland: http://www.who.int/influenza/human_animal_interface/tripartite_notes_H5N1.pdf [Google Scholar]
- 44. Yen HL, et al. 2007. Neuraminidase inhibitor-resistant recombinant A/Vietnam/1203/04 (H5N1) influenza viruses retain their replication efficiency and pathogenicity in vitro and in vivo. J. Virol. 81:12418–12426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Yuen KY, et al. 1998. Clinical features and rapid viral diagnosis of human disease associated with avian influenza A H5N1 virus. Lancet 351:467–471 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.