Abstract
Clients with co-occurring posttraumatic stress disorder (PTSD) and substance use disorders present a unique challenge for clinicians in substance use treatment settings. Substance dependent individuals with PTSD tend to improve less during substance use treatment and relapse more quickly following abstinence attempts compared to those without PTSD. Recent scientific efforts have focused on understanding the potential benefit of providing PTSD treatment concurrent with substance use treatment. The current case study describes 4 individuals with PTSD in a residential substance use facility who received prolonged exposure therapy for treatment of PTSD, in addition to the substance use treatment. These individuals completed 9 bi-weekly 60-minute sessions of prolonged exposure, as well as in vivo and imaginal exposure homework between sessions. None of the clients met criteria for PTSD at the end of treatment, with these gains being maintained at 3- and 6-months post-treatment. Additionally, the clients did not relapse in response to undergoing exposure therapy. Implications for delivery of PTSD treatment in substance use treatment facilities are discussed.
Keywords: PTSD, Substance Use, Alcohol, Prolonged Exposure, Residential Treatment
Individuals with substance use disorders (SUD) have consistently evidenced elevated rates of axis I psychopathology compared to the general population (e.g., Grant et al., 2004). Posttraumatic stress disorder (PTSD), in particular, is disproportionately detected among individuals seeking treatment for a SUD. For example, past studies indicate half of individuals seeking SUD treatment meet criteria for current PTSD (e.g., Brown, Stout, & Mueller; 1999), while the lifetime prevalence rate of PTSD in the general U.S. population is estimated to be 8% (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). A PTSD diagnosis has negative implications for individuals attempting sobriety. For example, individuals with PTSD tend to report stronger drug and alcohol cravings (e.g., Coffey et al., 2002) and relapse more quickly following SUD treatment compared to individuals without PTSD (e.g., Brown et al., 1999). Therefore, it is important to provide treatment for PTSD in SUD treatment.
Past efforts to deliver combined non-exposure-based PTSD-SUD treatment have been made, although no treatment has been proven to be universally effective. For example, Seeking Safety (SS) has evidenced significant improvements in PTSD symptoms and substance abuse but has not demonstrated better outcomes than relapse prevention or health education interventions in randomized controlled trials (Hien et al., 2009; Hien, Cohen, Miele, Litt, & Capstick, 2004). In a recent study comparing SS + treatment-as-usual (TAU) to TAU alone (Zlotnick, Johnson, & Najavits, 2009), SS+TAU was associated with similar outcomes compared to TAU, although both SS+TAU and TAU evidenced significant improvements in both PTSD and SUD outcomes. Other psychotherapies, such as a cognitive therapy approach adapted from a manual used in serious mental illness populations (McGovern et al., 2009) and Transcend (an eclectic partial hospitalization protocol; Donovan et al., 2001) have evidenced minor improvements in PTSD and/or SUD outcomes but have only been tested in small samples with no control groups.
Given the absence of a proven therapy, it may be useful to focus empirical efforts on existing, well-established treatment approaches. Prolonged Exposure therapy (PE; Foa, Hembree, & Rothbaum, 2007), a cognitive-behavioral treatment approach, is one of the most effective treatments for PTSD (Foa, Keane, Friedman, & Cohen, 2008) and should be considered as an adjunct to SUD treatment. PE includes: psychoeducation, breathing retraining, in vivo exposure, and imaginal exposure (for a review, see Foa et al., 2007). Psychoeducation provides information about PTSD, a cognitive-behavioral model of PTSD onset and maintenance, and an overview treatment mechanisms. Breathing retraining is a relaxation skill that provides clients with a way to recover from the distress elicited in exposure. In vivo exposure involves clients and therapists identifying safe, trauma-related situations that are feared and avoided, and systematically and repeatedly engaging in those situations until the anxiety diminishes. Finally, imaginal exposure requires clients to tell the therapist their most bothersome trauma in the present tense repeatedly in-session for 45–60 minutes without stopping. Clients are instructed to listen to audio-recordings of their trauma script daily, which allows for emotional processing of the event. Typically, PE occurs for 9–12 60- or 90-minute sessions and has been shown to be an effective and lasting treatment for PTSD (Powers, Halpern, Ferenschak, Gillihan, & Foa, 2010).
Preliminary work indicates that PE may be successful and feasible within PTSD-SUD populations. For example, Brady and colleagues (2001) investigated imaginal and in vivo exposure for PTSD in combination with an outpatient cognitive behavioral cocaine dependence treatment. PTSD symptoms and cocaine use significantly decreased over the 16-session treatment, with gains maintained at 6-months post-treatment. In addition, cocaine use did not increase during the exposure portion of the protocol, indicating that exposure may be well tolerated in outpatient SUD populations. Triffleman (2000) similarly investigated a combined treatment approach termed Substance Dependence PTSD Therapy (SDPT), in which patients underwent a 5-month twice-weekly treatment, which included cognitive-behavioral coping skills training for SUD, followed by a cognitive-behavioral PTSD treatment (including exposure-based exercises). PTSD symptoms, but not substance use, decreased over the course of treatment, and substance use decreased over the follow-up. Finally, Najavits and colleagues (2005) investigated a treatment combining SS with exposure-based PTSD therapy, which also found positive PTSD and SUD outcomes. Interestingly, patients in this pilot study rated the exposure-based sessions as being the most useful treatment component.
Despite the existence of well-established PTSD treatments, current prevailing practice in SUD treatment settings does not include services for addressing co-occurring anxiety and mood disorders. Most often, individuals with comorbid psychopathology are referred from SUD treatment to anxiety and mood disorder clinics (McGovern, Xie, Segal, Siembab, & Drake, 2006). This is problematic, given that only one-third of patients will follow through with a referral between medical and psychiatric clinics, (e.g., Griswold, Homish, Pastore, & Leonard, 2010). One exception is the Veterans Health Administration (VHA), which now mandates that all VA PTSD programs must be able to address the needs of clients with co-occurring SUDs (Veterans Health Administration, 2008). Ideally, PTSD and other axis I conditions would be treated within SUD treatment centers (and vice versa) in civilian settings as well; however, a number of existing barriers to providing such treatment have been identified. A few of the most commonly cited barriers are staffing issues, insufficient training of staff, management support, and physical resources (McGovern et al., 2006).
Henslee and Coffey (2010) have identified a number of strategies for overcoming some of the common barriers to treating PTSD within residential SUD treatment settings, such as conducting PE sessions twice a week for 60 minutes (as opposed to 90) to fit within the typical residential structure. It is also recommended that the therapist loan clients a tape player and headphones so that they may complete imaginal exposure homework privately. Similarly, it is recommended to have clients utilize visual or auditory stimuli that invoke trauma-related anxiety for in vivo exposures (e.g., pictures/video clips, gunshot sound), with encouragement to continue the exposure exercises in the presence of the actual stimuli (if they are safe) upon discharge. The current study utilized in vivo procedures, given that they are typically included as a key treatment component of PE in effectiveness studies (Powers et al., 2010) and that the feasibility of having clients return for in vivo sessions post-discharge is questionable (i.e., clients come to this residential treatment program from various parts of the Southeast United States).
Another barrier to implementing PE in SUD treatment settings is staff-related concerns (e.g., increased substance use/cravings in response to trauma memories). Emerging literature suggests that concurrent PTSD and SUD treatment is feasible and likely does not lead to worsened SUD treatment outcomes (Brady et al., 2001; Coffey, Stasiewicz, Hughes, & Brimo, 2006; Riggs & Foa, 2008). However, clinical outcomes among individuals receiving treatment for PTSD in such programs have not been extensively studied. Specifically, it is important to understand whether clients with PTSD who are in residential SUD treatment centers are capable of completing PE and whether successful completion of PE leads to treatment gains in PTSD and SUD. The following case series intends to build upon the Henslee & Coffey (2010) manuscript by providing real-world clinical examples of individuals receiving concurrent PTSD and SUD treatment in a residential setting.
Clinical Case Series
The following case examples represent individuals who participated in PE while completing a residential SUD treatment program as part of a larger, ongoing randomized clinical trial. All individuals were receiving treatment for current alcohol dependence, with at least one heavy drinking day (i.e., 5 or more drinks in a single episode [4 for women]) in the 60 days prior to the initial assessment. In addition, all individuals met criteria for at least one DSM-IV Criterion A traumatic event (at least 30 days prior to the assessment) and a current PTSD diagnosis. At the initial assessment, and at 3- and 6-months post-PE, individuals completed assessments of PTSD, anxiety and mood disorders, and substance use. Clients with psychotic symptoms or imminent suicidality were excluded. Clients included Mary, Phil, James, and April. (Note: Names and identifying information of these clients have been changed to protect confidentiality).
The site was a 6-week residential SUD treatment facility located within a rural Southeastern US community that utilizes a 12-step treatment approach. Clients participated in 12-step groups throughout the week, and each client met with a treatment coordinator regularly. The PE staff members visited the treatment facility to assess PTSD and provide individual treatment to those who qualified (see below for assessment and treatment procedures). The PE staff members worked closely with the residential staff to coordinate care. For example, the residential staff provided encouragement to their clients who were completing the PE protocol, and the PE staff members provided psycho-educational materials to the residential staff regarding PTSD-SUD co-occurrence and best treatments for PTSD. A representative from the PE treatment team also attended a weekly residential staff meeting.
Assessment
Clients completed structured clinical interviews at baseline, post-treatment, and 3- and 6-month follow-ups. An expanded version of the National Women's Study PTSD Module (NWS; Resnick, 1996) adapted by Dansky and colleagues (Dansky, Byrne & Brady, 1999) to include additional items assessing intimate violence was administered to assess complete trauma history and Criterion A status (see Table 1). The Clinician Administered PTSD Scale (CAPS; Blake et al., 1995) was administered to assess PTSD symptom severity (sum of frequency and intensity items; Monson et al., 2006) and diagnosis for all PTSD Criterion A events, collectively. The CAPS was also utilized to assist clinicians in selecting the target trauma for PE (i.e., the trauma that was related to the greatest number of PTSD symptoms on the CAPS). The Mini International Neuropsychiatric Interview (MINI; Sheehan et al., 1998) was administered to assess current (past month) anxiety and mood disorders. The Computerized Diagnostic Interview Schedule (CDIS; Robins et al., 2000), was used to diagnose SUDs. The Time Line Follow-Back (TLFB; Sobell & Sobell, 1992), a calendar method to retrospectively gather information about participants' substance use, assessed substance use over the past 90 days.
Table 1.
Summary of Clients' Trauma Exposure Histories
| Trauma Category | Mary | Phil | James | April |
|---|---|---|---|---|
| Natural disaster | 1 | 1 | - | - |
| Motor vehicle accident | 1 | - | 2 | 1 |
| Warfare/Combat | - | - | - | - |
| Sudden death of loved one | - | 8 | 1 | 2 |
| Life-threatening illness | - | - | - | 1 |
| Attempted suicide | - | - | - | 1 |
| Threatened with weapon | - | 1 | 1 | 1 |
| Physical assault with weapon | - | - | 7 | - |
| Physical assault by stranger | - | - | 1 | - |
| Physical assault by family/partner/friend | 1 | 3 | ||
| Sexual assault as child | 1 | - | - | 3 |
| Sexual assault as adult | 1 | - | 1 | 3 |
| Total Number of Traumas | 5 | 10 | 13 | 15 |
Note: Trauma history obtained from National Women's Study – PTSD Module (Resnick, 1996).
Clients completed self-report assessments weekly during treatment. The Impact of Event Scale-Revised (IES-R; Weiss & Marmar, 1997) assessed past-week PTSD symptoms related to the target trauma. The Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) assessed DSM-IV depressive symptoms. The Working Alliance Inventory (WAI; Horvath & Greenberg, 1989) assessed clients' perceptions of the therapeutic relationship between therapist and patient based on the components of bonds, goals, and outcomes. Clients provided Subjective Units of Distress Scale ratings (SUDS) every 5 minutes during imaginal exposure sessions and 3 times (pre-exposure, peak during exposure, and post-exposure) during imaginal and in vivo exposure homework assignments. The scale assesses emotional distress and ranges from 0 (“no distress or discomfort”) to 100 (“extreme distress or discomfort”).
Client #1: “Mary”
Mary was a 24-year-old unemployed Caucasian woman. Her target trauma was a motor vehicle accident (MVA) that occurred approximately 7 years prior to treatment. Mary had briefly looked away from the road and almost hit the car in front of her. She tried to swerve and slammed on her brakes, but the SUV behind her collided with her, causing her to hit the SUV in front of her. Her car spun off the road and stopped with the front end in the median. Mary met criteria for an additional 4 Criterion A traumatic events, including sexual and physical assaults as well as exposure to natural disaster (i.e., a tornado). In addition to PTSD and alcohol dependence, Mary met current criteria for bipolar disorder, panic disorder with agoraphobia, and obsessive-compulsive disorder, as well as amphetamine, sedative, and cocaine dependence.
Mary's case provides an illustration of the importance of working closely with the individual counselors of PE clients in residential treatment settings (see Henslee & Coffey, 2010 for relevant discussion). Specifically, Mary's target trauma was a MVA, but she did not have access to a car and was not able to leave the premises independently during her stay in treatment. This presented a challenge, given that Mary's in vivo hierarchy only included items related to driving, such as driving between two trucks (initial SUDS rating of 50) and riding in a small car with others (initial SUDS rating of 80). Mary's PE therapist coordinated with her primary counselor to discuss strategies for completing in vivo homework exercises during her residential treatment (e.g., Mary rode in the treatment facility's passenger van 1–2 times per week). During PE, Mary completed 3 exercises from her in vivo hierarchy: riding in the treatment center van (initial SUDS rating of 60); listening to an audio recording of a car accident (initial SUDS rating of 60); and once she transitioned to a secondary treatment facility (between sessions 7 and 8 of PE), driving her own car in a number of scenarios.
Mary completed her imaginal and in vivo exposure homework regularly, although she had to wait until discharge (after session 7 of PE) to complete the majority of her in vivo homework assignments due to the above limitations. Specifically, she completed in vivo exposure homework an average of 40% of the days between sessions (range from 0% to 75% completed), and she completed imaginal exposure homework an average of 76% of the days between sessions (range from 60% to 86% completed). Mary stated that she was very motivated to complete PE due to her perception of it being an integral part of her SUD treatment.
Client #2: “Phil”
Phil was a 26-year-old Caucasian man who was employed part-time as a bartender. Phil's target trauma was an assault with a weapon that occurred approximately 9 years prior to treatment. Phil approached a group of males in his car in an attempt to purchase marijuana. One of the males approached his window while two others tried to get in his back seat. The male at the window stole a CD player from Phil's lap, while another male held a gun to Phil's head. Phil drove away while shots were fired that shattered his front and back windows. He met criteria for an additional 9 Criterion A events, including exposure to a natural disaster and unexpected deaths of loved ones. In addition to PTSD and alcohol dependence, Phil met current criteria for major depressive disorder and social anxiety disorder. He also met current criteria for marijuana and sedative dependence and past criteria for amphetamine and hallucinogen dependence.
Phil's in vivo exposure homework included listening to an audio recording of gun shots (initial SUDS rating of 30), looking at pictures of a shattered windshield (initial SUDS rating of 40), and holding a real bullet (initial SUDS rating of 40). Phil progressed from an item given an initial SUDS rating of 30 (listening to an audio recording of gunshot sounds) to items rated a 40 (e.g., holding a real bullet). Items higher on his hierarchy were not feasible to complete while in treatment, given that they involved having Phil visit a specific neighborhood in person. Phil completed his in vivo and imaginal exposure homework regularly. Specifically, he completed his in vivo exposure homework an average of 78% of the days between sessions (range of completed homework from 75% to 80%), and he completed his imaginal exposure homework an average of 73% of the days between sessions (range of completed homework from 50% to 80%).
Client #3: “James”
James was a 45-year-old African American man who was employed full-time as a chef. James's target trauma was hearing about his daughter getting stabbed and killed during an altercation with a gang member. Her murder occurred 2 years prior to treatment. Before her death, James had re-established contact with her and was planning a reunion with her. He met criteria for an additional 12 Criterion A events, including physical assault, an MVA, witnessing others get killed, and finding out his daughter was raped. In addition to PTSD and alcohol dependence, James met current criteria for agoraphobia and marijuana and cocaine dependence.
James missed a session early in treatment due to an appointment at drug court. He also reported ongoing financial stress related to the cost of residential SUD treatment and stated at multiple sessions that he planned to leave treatment. Ultimately, he remained in treatment and even continued into the secondary treatment program, due partially to encouragement from his family and primary counselor. James also appeared to have some difficulty comprehending the SUDS rating system at times; however, he gradually evidenced improved understanding of the scale and was able to achieve treatment gains in spite of this difficulty.
James's in vivo homework included seeing a picture of funeral flowers (initial SUDS rating of 30), watching women's basketball (initial SUDS rating of 50), talking with his daughter's cousins (initial SUDS rating of 60), and seeing pictures of gang-related graffiti (initial SUDS rating of 90). James progressed through his in vivo hierarchy from an item with an initial SUDS rating of 30 (i.e., seeing a picture of roses) to items given an initial SUDS rating of 90 (e.g., speaking with certain family members). James completed his in vivo exposure homework an average of 79% of the days between sessions (range of completed homework from 43% to 100%) and his imaginal exposure homework an average of 92% of the days between sessions (range of completed homework from 75% to 100%).
Client #4: “April”
April was a 43-year-old Caucasian woman who was employed full-time as an accountant and office manager. April's target trauma was experiencing childhood sexual abuse, which occurred over 30 years prior to treatment. While staying at a neighbor's house, the neighbor's husband kissed her and got into bed with her against her wishes. He fondled her breasts, pushed his pelvis against her, and pulled her underwear down to touch her genital area. He stopped when April threatened to tell his wife. She met criteria for an additional 14 Criterion A events, including an MVA, physical and sexual assaults, sudden deaths of loved ones, and life-threatening medical problems. In addition to PTSD and alcohol dependence, April met criteria for bipolar disorder (current depressive episode), panic disorder with agoraphobia, and social anxiety disorder, as well as amphetamine, sedative, and cocaine dependence.
April's in vivo exposure hierarchy included lying on her bed with her back to the door (initial SUDS rating of 40) and seeing a picture of her family's old house (initial SUDS rating of 70). April progressed from items given an initial SUDS rating of 30 (e.g., seeing a picture of a nightgown) to items initially rated 80 (e.g., lying on her bed with her back to the door with someone opening it). April reported being extremely motivated for treatment, despite feeling high levels of anticipatory anxiety early in treatment. She completed her homework regularly, although there was one week that she was not able to obtain a picture necessary for her in vivo assignment. April experienced ongoing physical illness throughout her treatment but stayed committed to PE. April completed her in vivo homework an average of 69% of the days between sessions, or 83% if not including the week she was not able to obtain the picture (range of completed homework 0% to 100%). She completed imaginal exposure homework an average of 73% of the days between sessions (range of completed homework 40% to 100%).
Treatment Outcome
At the start of treatment, all clients met diagnostic criteria for current PTSD and alcohol dependence. All clients endorsed multiple Criterion A events (range = 4–14). Furthermore, all clients met criteria for additional current axis I disorders (range of additional disorders = 1 – 3) and SUDs (range = 2 – 3). Given that all clients evidenced at least a 70% reduction in PTSD symptoms from baseline by session 8, termination occurred at session 9 (per recommendations in Foa et al., 2005). Had clients not exhibited a 70% reduction, additional sessions would have been offered. For all clients, PE was completed within a 6-week period.
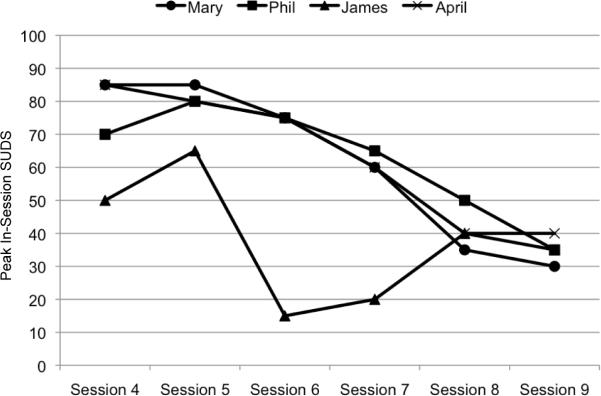
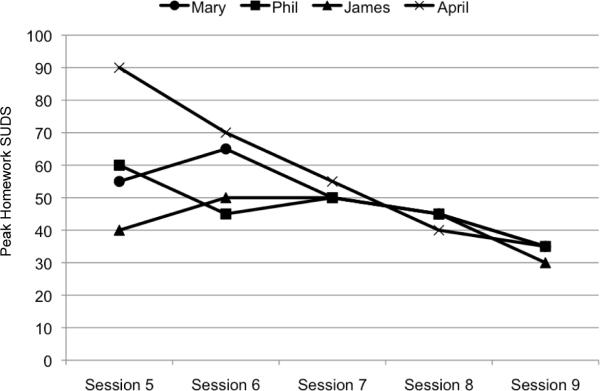
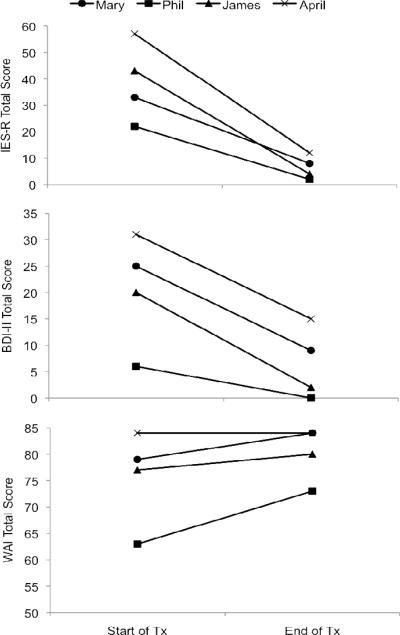
Clients evidenced substantial decreases in their peak SUDS ratings during in-session and homework imaginal exposure exercises (see Figures 1 and 2). Collectively, clients evidenced declines in their peak SUDS ratings equivalent to approximately 50% of their initial anxiety ratings. They also reported substantial decreases in PTSD symptoms (in relation to target event), regardless of initial symptom severity (see Figure 3). Specifically, all clients reported past-week IES-R total scores ranging from 2 to 12 at their last treatment session. Clients also experienced a decrease in depressive symptoms (see Figure 3). Mary and James initially endorsed symptoms in the “moderate” severity range on the BDI-II but, by the end of treatment, endorsed symptoms in the “minimal” severity range (Beck et al., 1996). Similarly, April initially rated her symptoms in the “severe” range but reported reductions in her depressive symptoms that left her with only “mild” symptom severity by treatment completion. Phil endorsed only “minimal” symptoms at treatment onset and remained in the “minimal” range throughout the treatment phase. All clients in this series reported very positive therapeutic alliance with their therapist (see Figure 3). In fact, Phil, who reported the lowest levels of therapeutic alliance at the start of treatment, indicated improvements in his perception of the alliance throughout treatment.
Figure 1.
Peak SUDS Ratings during In-Session Imaginal Exposure Exercises Note: SUDS = Subjective Units of Distress Scale.
Figure 2.
Peak SUDS Ratings during Imaginal Exposure Homework Exercises Note: SUDS = Subjective Units of Distress Scale.
Figure 3.
Change in IES-R, BDI-II, and WAI from Start to End of Treatment Note: IES-R = Impact of Events Scale – Revised (Weiss & Marmar, 1997); BDI-II = Beck Depression Inventory-II (Beck et al., 1996); WAI = Working Alliance Inventory (Horvath & Greenberg, 1989); all measures completed for past week.
All clients evidenced significant improvements in global PTSD symptoms (no positive diagnoses post-treatment) and substance use. Importantly, decreases in overall PTSD symptoms were maintained at 3- and 6-months post-treatment (see Figure 4). Phil and James endorsed minimal PTSD symptoms (CAPS total severity scores of 0 and 8, respectively) at post-treatment and maintained their gains at 3- and 6-months post-treatment. Mary and April began treatment with greater levels of PTSD symptoms relative to the men (CAPS severity scores of 83 and 101, respectively) and reported sub-clinical PTSD symptoms (i.e., elevations in symptom severity that do not meet the threshold for a PTSD diagnosis) post-treatment (scores of 39 and 36, respectively). Interestingly, both Mary and April continued to experience declines in their PTSD symptoms during the 3–6 months following treatment, reporting total severity scores of 8 and 0, respectively, by the 6-month assessment. This may be due to increased opportunity to complete in vivo exposure exercises following discharge from residential treatment. Finally, all clients maintained SUD treatment gains following discharge from residential treatment (see Table 2). Notably, all clients reached 99–100% abstinence from drugs and alcohol at 6 months post-treatment and reported no heavy drinking days following treatment.
Figure 4.
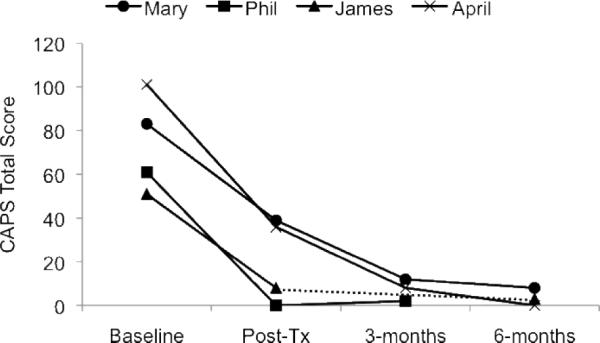
Change in Overall PTSD Symptoms (CAPS Total Severity) Note: CAPS (Clinician-Administered PTSD Scale; Blake et al., 1995) assessed past-month PTSD symptoms for all Criterion A events, collectively.
Table 2.
Alcohol and Illicit Drug Use in Past 90 Days, Assessed at Pre-Treatment and 3-/6-Month Follow-Up
| Mary | Phil | James | April | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | 3-mo. | 6-mo. | Pre | 3-mo. | 6-mo. | Pre | 3-mo. | 6-mo. | Pre | 3-mo. | 6-mo. | |
| Percent Days Abstinent from Alcohol | 70% | 100% | 100% | 12% | 100% | -- | 99% | -- | 100% | 72% | 100% | 100% |
| Number of Heavy Drinking Days | 27 | 0 | 0 | 79 | 0 | -- | 1 | -- | 0 | 25 | 0 | 0 |
| Percent Days Abstinent from Illicit Drugs | 51% | 100% | 100% | 17% | 99% | -- | 99% | -- | 100% | 84% | 100% | 100% |
Note: Alcohol and drug use assessed with the 90-day Timeline Follow-back (TLFB; Sobell & Sobell, 1992). “Heavy drinking day” = 5 or more drinks (4 or more for women) within one drinking episode. Phil and James did not complete assessment sessions at 6- and 3-months, respectively.
Summary
Together, the clients presented in this case series illustrated successful PTSD treatment within residential SUD treatment. Specifically, none of the clients met criteria for PTSD following PE, with these gains being maintained at 3- and 6-months post-treatment. These observations are noteworthy, particularly given that the clients presented for treatment with multiple SUDs and axis I diagnoses, as well as complex trauma histories (e.g., varied trauma types, multiple trauma exposures). In fact, the clients in this series not only completed PE in spite of such comorbidities, but also reported decreased levels of depressive symptoms from preto post-treatment. These treatment gains must be considered within the scope of the entire treatment package that clients received (i.e., 12-step based residential treatment program and PE therapy). It is also important to note that PE did not lead to SUD treatment dropout or increased levels of substance use following discharge from residential treatment. Although the current clients were within a controlled environment during PE, this finding is consistent with empirical study indicating that PTSD treatment is safe for individuals in treatment for co-occurring SUDs (Brady et al., 2001; Coffey et al., 2006; Riggs & Foa, 2008).
This case series also demonstrated the feasibility of conducting PE within the constraints of residential treatment, as outlined theoretically by Henslee and Coffey (2010). For example, the sessions were successfully completed within the 60-minute session structure of the treatment facility and fit within the 6-week residential treatment model. Additionally, clients were able to complete imaginal exposure homework between sessions with the use of tape players and headphones, as well as in vivo homework assignments with the use of printed images and audio recordings. Coordination with the primary SUD counselors proved invaluable, as illustrated in the case of Mary, who was given access to riding as a passenger on outings in the treatment center van for in vivo exposure. Treatment was successfully delivered due to a strong collaboration between the PE therapist and SUD treatment counselors, as well as the therapist's willingness to be creative and flexible with execution of exposure exercises.
Although the current case series demonstrated the potential benefits of completing PE in a residential facility, there are a number of limitations and related future directions for this work. First, the current study provides one example of PE in a residential treatment facility. More comprehensive studies including control participants are needed. Second, the current study provides no insight into whether provision of PE in outpatient SUD treatment settings is effective, although other studies have provided preliminary evidence to support the use of trauma-focused exposure therapy in outpatient SUD treatment settings (e.g., Brady et al., 2001; Coffey et al., 2006). Future work would benefit from investigating PE among comorbid individuals in multiple treatment settings. Third, although preliminary data assessing the utility of empirically supported treatments for PTSD among minority populations (e.g., African American, low-income) are promising (Lester, Resick, Young-Xu, & Artz, 2010; Feske, 2008), the current case series did not include measurements to address clients' experiences with or perceptions of PE on the basis of race or culture. Future work would greatly benefit from focusing on the role of multiple cultural factors. For a broader discussion of multicultural issues in treatment, please refer to the APA Multicultural Guidelines (http://www.apa.org/pi/oema/resources/policy/multicultural-guideline.pdf). Fourth, clients received a variety of treatment components during the residential program. Larger controlled studies will facilitate our understanding of the role of PE in various clinical outcomes. Finally, the current case series did not systematically investigate how best to incorporate PE and other mental health treatments into existing treatment centers. Dissemination and implementation work is greatly needed to incorporate empirically based treatments into community settings.
Acknowledgments
This research was supported, in part, by National Institute on Alcohol Abuse and Alcoholism grant R01AA016816 (PI: Coffey).
Biographies
ERIN C. BERENZ received her PhD in Clinical Psychology from the University of Vermont. She is currently a postdoctoral fellow at the Virginia Institute for Psychiatric and Behavioral Genetics at Virginia Commonwealth University. Her primary research interests are in the areas of posttraumatic stress disorder and co-occurring substance use disorders.
LAUREN ROWE received her BA from the University of Mississippi. She is currently a medical student at the University of Mississippi Medical Center, where she plans to specialize in Pediatrics or Internal Medicine.
JULIE A. SCHUMACHER received her PhD in Clinical Psychology from the State University of New York at Stony Brook. She is currently an Associate Professor of Psychiatry at the University of Mississippi Medical Center. Her primary research interests are in the areas of drug and alcohol abuse and violent behavior.
PAUL R. STASIEWICZ received his PhD in Clinical Psychology from The State University of New York at Binghamtom. He is currently a Research Scientist at the University at Buffalo's Research Institute on Addictions. His research interests include learning-based processes of addiction and the application of basic behavioral processes to the development of new clinical interventions.
SCOTT F. COFFEY received his PhD in Clinical Psychology from the University of Mississippi. He is Professor and Director of the Division of Psychology in the Department of Psychiatry and Human Behavior at the University of Mississippi Medical Center. His research interests include substance use disorders, posttraumatic stress disorder (PTSD), the co-occurrence of PTSD and substance abuse, cue reactivity, psychotherapy treatment development, and impulsivity.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/pro
References
- Beck A, Steer R, Brown G. Manual for the Beck Depression Inventory-II. Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Blake D, Weathers F, Nagy L, Kaloupek D, Gusman F, Charney D, et al. The development of a Clinician-Administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Brady K, Dansky B, Back S, Foa E, Carroll K. Exposure therapy in the treatment of PTSD among cocaine-dependent individuals: Preliminary findings. Journal of Substance Abuse Treatment. 2001;21:47–54. doi: 10.1016/s0740-5472(01)00182-9. doi: 10.1016/S0740-5472(01)00182-9. [DOI] [PubMed] [Google Scholar]
- Brown P, Stout R, Mueller T. Substance use disorder and posttraumatic stress disorder comorbidity: Addiction and psychiatric treatment rates. Psychology of Addictive Behaviors. 1999;13:115–122. doi: 10.1037//0893-164X.13.2.115. [Google Scholar]
- Coffey S, Saladin M, Drobes D, Brady K, Dansky B, Kilpatrick D. Trauma and substance use cue reactivity in individuals with comorbid posttraumatic stress disorder and cocaine or alcohol dependence. Drug and Alcohol Dependence. 2002;65:115–127. doi: 10.1016/s0376-8716(01)00157-0. doi: 10.1016/S0376-8716(01)00157-0. [DOI] [PubMed] [Google Scholar]
- Coffey S, Stasiewicz P, Hughes P, Brimo M. Trauma-focused imaginal exposure for individuals with comorbid posttraumatic stress disorder and alcohol dependence: Revealing mechanisms of alcohol craving in a cue reactivity paradigm. Psychology of Addictive Behaviors. 2006;20:425–435. doi: 10.1037/0893-164X.20.4.425. doi: 10.1037/0893-164X.20.4.425. [DOI] [PubMed] [Google Scholar]
- Dansky B, Bryne C, Brady K. Intimate violence and post-traumatic stress disorder among individuals with cocaine dependence. American Journal of Drug and Alcohol Abuse. 1999;25:257–268. doi: 10.1081/ada-100101859. doi: 10.1081/ADA-100101859. [DOI] [PubMed] [Google Scholar]
- Donovan B, Padin-Rivera E, Kowaliw S. “Transcend”: Initial outcomes from a posttraumatic stress disorder/substance abuse treatment program. Journal of Traumatic Stress. 2001;14:757–772. doi: 10.1023/A:1013094206154. doi: 10.1023/A:1013094206154. [DOI] [PubMed] [Google Scholar]
- Feske U. Treating low-income and minority women with posttraumatic stress disorder: A pilot study comparing prolonged exposure and treatment as usual conducted by community therapists. Journal of Interpersonal Violence. 2008;23:1027–1040. doi: 10.1177/0886260507313967. doi: 10.1177/0886260507313967. [DOI] [PubMed] [Google Scholar]
- Foa E, Hembree E, Cahill S, Rauch S, Riggs D, Feeny N, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005:953–964. doi: 10.1037/0022-006X.73.5.953. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- Foa E, Hembree E, Rothbaum B. Prolonged Exposure Therapy for PTSD: Emotional processing of traumatic experiences. Oxford Press; New York: 2007. [Google Scholar]
- Foa E, Keane T, Friedman M, Cohen J, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. 2nd Ed. Guilford Press; New York: 2008. [Google Scholar]
- Grant B, Stinson F, Dawson D, Chou S, Ruan W, Pickering R. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States. Archives of General Psychiatry. 2004;61:361–368. doi: 10.1001/archpsyc.61.4.361. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- Griswold K, Homish G, Pastore P, Leonard K. A randomized trial: Are care navigators effective in connecting patients to primary care after psychiatric crisis? Community Mental Health Journal. 2010;46:398–402. doi: 10.1007/s10597-010-9300-x. doi: 10.1007/s10597-010-9300-x. [DOI] [PubMed] [Google Scholar]
- Henslee A, Coffey S. Exposure therapy for posttraumatic stress disorder in a residential substance use treatment facility. Professional Psychology: Research and Practice. 2010;41:34–40. doi: 10.1037/a0018235. doi: 10.1037/a0018235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien D, Cohen L, Miele G, Litt L, Capstick C. Promising treatments for women with comorbid PTSD and substance use disorders. American Journal of Psychiatry. 2004;161:1426–1432. doi: 10.1176/appi.ajp.161.8.1426. doi: 10.1176/appi.ajp.161.8.1426. [DOI] [PubMed] [Google Scholar]
- Hien D, Wells E, Jiang H, Suarez-Morales L, Campbell A, Cohen L, et al. Multisite randomized trial of behavioral interventions for women with co-occurring PTSD and substance use disorders. Journal of Consulting and Clinical Psychology. 2009;77:607–619. doi: 10.1037/a0016227. doi: 10.1037/a0016227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath A, Greenberg L. Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology. 1989;36:223–233. doi: 10.1037//0022-0167.36.2.223. [Google Scholar]
- Kessler R, Sonnega A, Bromet E, Hughes M, Nelson C. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Lester K, Resick P, Young-Xu Y, Artz C. Impact of race on early treatment termination and outcomes in posttraumatic stress disorder treatment. Journal of Consulting and Clinical Psychology. 2010;78:480–489. doi: 10.1037/a0019551. doi: 10.1037/a0019551. [DOI] [PubMed] [Google Scholar]
- McGovern M, Xie H, Segal S, Siembab L, Drake R. Addiction treatment services and co-occurring disorders: Prevalence estimates, treatment practices, and barriers. Journal of Substance Abuse Treatment. 2006;31:267–275. doi: 10.1016/j.jsat.2006.05.003. doi: 10.1016/j.jsat.2006.05.003. [DOI] [PubMed] [Google Scholar]
- McGovern M, Lambert-Harris C, Acquilano S, Xie H, Alterman A, Weiss R. A cognitive behavioral therapy for co-occurring substance use and posttraumatic stress disorders. Addictive Behaviors. 2009;34:892–897. doi: 10.1016/j.addbeh.2009.03.009. doi: 10.1016/j.addbeh.2009.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monson C, Schnurr P, Resick P, Friedman M, Young-Xu Y, Stevens S. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2006;74:898–907. doi: 10.1037/0022-006X.74.5.898. doi: 10.1037/0022-006X.74.5.898. [DOI] [PubMed] [Google Scholar]
- Najavits L, chmitz M, Gotthardt S, Weiss R. Seeking Safety plus exposure therapy: An outcome study on dual diagnosis men. Journal of Psychoactive Drugs. 2005;37:425–435. doi: 10.1080/02791072.2005.10399816. [DOI] [PubMed] [Google Scholar]
- Powers M, Halpern J, Ferenschak M, Gillihan S, Foa E. A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review. 2010;30:635–641. doi: 10.1016/j.cpr.2010.04.007. doi: 10.1016/j.cpr.2010.04.007. [DOI] [PubMed] [Google Scholar]
- Resnick H. Psychometric review of National Women's Study (NWS) Event History-PTSD module. In: Stamm B, editor. Measurement of stress, trauma, and adaptation. Sidran Press; Lutherville, MD: 1996. [Google Scholar]
- Riggs D, Foa E. Treatment for co-morbid posttraumatic stress disorder and substance use disorder. In: Stewart S, Conrod P, editors. Anxiety and Substance Use Disorders. Springer; New York: 2008. [Google Scholar]
- Robins L, Cottler L, Bucholz K, Compton W, North C, Rourke K. Diagnostic Interview Schedule for the DSM-IV (DIS) Washington University; St. Louis, MO: 2000. [Google Scholar]
- Sheehan D, Lecrubier Y, Sheehan K, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59:34–57. doi: [PubMed] [Google Scholar]
- Sobell L, Sobell M. Timeline followback: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen J, editors. Measuring alcohol consumption: Psychosocial and biological methods. Humana Press; New Jersey: 1992. pp. 41–72. [Google Scholar]
- Triffleman E. Gender differences in a controlled pilot study of psychosocial treatments in substance dependent patients with posttraumatic stress disorder: Design considerations and outcomes. Alcoholism Treatment Quarterly. 2000;18:113–126. [Google Scholar]
- Veterans Health Administration . Uniform mental health services in VA medical centers and clinics (VHA Handbook 1160.01) U.S. Department of Veterans Affairs; Washington, DC: 2008. [Google Scholar]
- Weiss D, Marmar C. The Impact of Event Scale – Revised. In: Wilson J, Keane T, editors. Assessing Psychological Trauma and PTSD. The Guilford Press; NY: 1997. pp. 399–411. [Google Scholar]
- Zlotnick C, Johnson J, Najavits LM. Randomized controlled pilot study of cognitive-behavioral therapy in a sample of incarcerated women with substance use disorder and PTSD. Behavior Therapy. 2009;40:325–336. doi: 10.1016/j.beth.2008.09.004. doi: 10.1016/j.beth.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]