To conceive a child to save a child
Planning the birth of a baby who could be a hematopoietic stem cell (HSC) donor for an older brother or sister affected by a pathology which can be treated by sibling HLA-compatible HSC transplant represents an “extreme remedy” as opposed to an “extreme evil”.1 We first faced this problem 25 years ago when the question was whether it was ethically acceptable to conceive one baby to “save” another. In October 1984, a couple was informed that their only daughter, who at the time was four years old, had been diagnosed with Ph+ chronic myeloid leukemia. They asked if it were possible to treat their daughter by bone marrow transplant. They had considered trying to conceive another child, hoping that this new baby would be HLA-compatible with the sister. We replied that this was a possible therapeutic strategy but that the probability of HLA matching was 25%.2 We immediately saw how determined the parents were to try to radically transform the unfavorable prognosis for their daughter to a 70% probability of success, and at the same time to avoid the prospect of being left without children. The parents did not accept the hypothesis of searching for a donor through an international bone marrow donor bank (Anthony Nolan, London) and we did not feel we had the right to interfere with their decision; subsequent declarations endorsed this opinion.3,4 Robertson says: “the principle of procreative privacy is a fundamental value, so there should be compelling reason to interfere with a couple’s legitimate decision”.5,6 In 1984, in Italy, the only chance of having a ‘savior child’ was through a natural physiological pregnancy. Only a few years earlier, in 1978 in the UK, the first baby had been born as a result of in vitro fertilization (IVF).7
The new baby was HLA-compatible and the transplant took place when he was 19 months old (3 April 1987). It has been stated that a very small child, “programmed” within a family unit as an HSC donor for an elder brother or sister is forced to undertake an act of “involuntary altruism”.8,9 One could also talk about “voluntary conception” on the part of the parents; “to conceive a child to save a child”.8,9 Perhaps these are ethical considerations along the lines of Kant’s view of the reasons, distinctions and aims with which one brings “new human beings” into the world. This is not a new argument but has, in fact, already been widely discussed.10,11 There is little doubt that the parents must accept the new baby even if a “failed expectation” occurs as a consequence of HLA-incompatibility.8 Nonetheless, the “fulfillment of the expectation” gives the new baby an “added value” in the socio-affective context of the family.1,2
Once the transplant had taken place, we reported our experience to the scientific community; an experience which was practically unprecedented.2 Details were made available in the literature together with some anecdotal observations and personal comments.12 In the meantime, our case was being reported in all the most important European newspapers and magazines. In any case, our refusal to go along with the parents decision, besides heralding a death (the choice and the experience of death for such a refusal have also been reported12), would have seemed like putting their intentions on trial, with the view of rather than not to treat the sick child but more as insisting on treating her at all costs. In fact, our experience2 was immediately discussed with great authority in the philosophical literature in the United States,10 and only 28 months later the experience was reprogrammed and repeated. In April 1990, a new “programmed” baby was born in Los Angeles destined to “save” a sister who, once again, had leukemia. “The case of Anissa A” went round the world.13
Preimplantation Genetic Diagnosis
In 2001, there was a decisive change of perspective. At the University of Minnesota Medical School, Molly N, affected by Fanconi anemia was transplanted using IVF, Preimplantation Genetic Diagnosis (PGD) and stem cells from umbilical cord blood. This was the first transplant to use PGD, a technique perfected by Verlinsky et al. in the 1990s, for the pre implant selection of a healthy and HLA-compatible embryo “programmed” to be an HSC sibling donor.14–16 This is a radical change which led to critical debate on the part of philosophers, ethicists, legal doctors and scientists in general who were interested in this field.17–22 And it must be remembered that although transplants of HSC from an unrelated donor, or rather, from a consanguineous haploidentical donor, are extremely valuable therapeutic resources, however, in order to achieve a successful transplant, some congenital pathologies require a family HLA-compatible donor. Fanconi anemia is a good example, and a “savior” sibling, when there is no suitable brother or sister available, becomes a true future family life-savior.
While our case (1987)2 and the case of Anissa A were leukemia patients, Molly N, who was transplanted using the PGD technique, and whose case was re-examined in detail from an ethical point of view by Damewood,18 was affected with Fanconi anemia.14,15 The scientists behind the development of this procedure (PGD and HLA typing), who carry out research in the genetics (illness, health, HLA) of a single blastomer from Day 3 cleaving embryos (IVF),14,16 consider (and continue to propose) it as a better alternative to conventional “prenatal diagnosis” on chorial villus which carries the obvious risk-program of interrupting the pregnancy in cases of “sick embryo”. The comments in “Genetic testing of embryos: a critical need for data”19 make a clear reference to our theme that “a small but growing number of families have used PGD to attempt to have a baby who is an immunological match for an existing ailing sibling in order to use the baby’s cord blood for a stem cell transplantation”. The huge success of the use of cord blood23 would soon not fail to include cases treated with PGD.24 The specter of these indications would also appear to have its limitations given the urgency, which is not always taken into sufficient consideration, with which it is often necessary to intervene. Another scrupulous examination of the care and attention needed when programming a PGD had been published a year before.4 The fact that PGD can provide confirmation of a “healthy embryo” at the same time as confirming that this embryo is HLA-compatible with the transplant recipient is extremely important.14,16
It is, however, at this point that PGD is burdened with ethical questions. By definition, these concerns, on the one hand, regard the selection of useful embryos from those which are not compatible. The other reservation regards the personal psychosomatic and socio-affective profile of the donor. This can be a risk both in the short and in the long term.15 More generally, literature published over the last fifteen years seems to show that there are now fewer reservations about PGD and there is less discussion of the ideologies which oppose it. In fact, there is now a greater respect for privacy and, in a final analysis, for the personal ethical and practical choices made.12 Sheldon and Wilkinson20 ask themselves ”Should selecting savior siblings be banned?” and analyze three psychologically important topics. Although their approach is critical it removes any reservations about the use of PGD. The three topics are: i) the donor child considered as a convenience; ii) the implicit ‘slippery-slope’ created by PGD; iii) the possibility that the donor could, in the very long-term, suffer from a reduced physical and psycho-social profile.
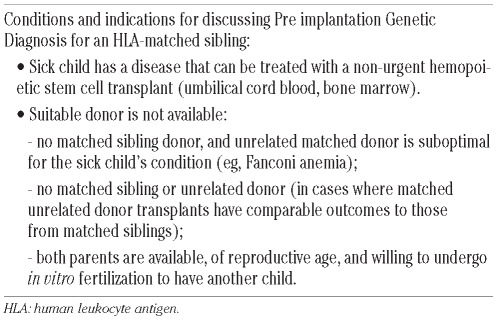
In reality, in 2004 in the UK, Gavaghan21 criticized the decisions of the Court of Appeal and the Human Fertilisation and Embryology Authority. In any case, even on the basis of more or less recent considerations,17,22 the indications presented in Australia by Strong25 (Table 1) are still important and of great value in maintaining a balanced view point and stimulating reflection. Obviously, the problem remains for those parents who live in countries where PGD following IVF to select HLA-compatible embryos is not allowed (for example, in Australia, not all states allow PGD to be performed26) and they cannot take the decision to look abroad. PGD is also not allowed in Italy. It is, however, important to remember that sometimes application of the law allows some legal room for manoeuvre, as in the sentence issued by the Bologna Law Courts (19 July 2010).27 Two weeks before, the German Court of Justice had pronounced an equally important sentence similar to that in Bologna.27
Table 1.
One could say that the 25 years which have passed since our first experience have not been in vain. It is important to underline the wisdom of careful and balanced reflection as to the possible future developments. Day to day reality means that in programming a savior donor for a sick child there are two roads open to us. The first suggests we should leave everything to chance. Opting for a normal, natural birth, however, is a gamble. The second option is a full blown and technically perfect PGD program which brings into the world a child who satisfies the two requirements needed to save the elder sibling’s life: a healthy child who is HLA-compatible.
A look back over the last 25 years in the life of our first patient
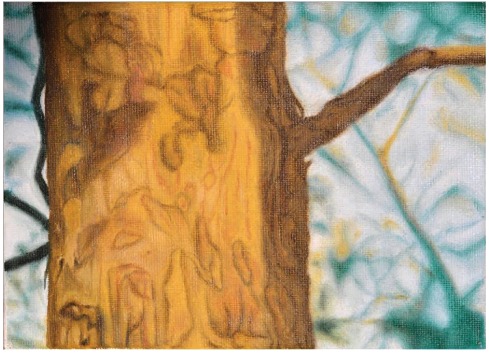
Over the last 25 years, besides the personal contacts maintained through periodic checkups, we have often had the opportunity to follow the life of our first patient (obviously being extremely careful to allow her to live her own life freely and with full respect for her individual privacy and autonomy).28 It is enough to say that our patient has completed her diploma course at the Brera Academy, Milan, with a thesis on “Nature in Art” (Figure 1). She has a regular, full time job and tells us with a big smile that she is happy and fulfilled in her work. She has a partner, and a cat who has been a member of the family since she left home four years ago. She gets on extremely well with her parents and is in touch with them every day. She also has an excellent relationship with her donor brother. He is happy working as a chef in an important restaurant in the town where he lives and has recently become the father of twins.
Figure 1.
Evelina, “Corteccia nel verde”, 2004.
Conclusions
There is little doubt that if it had not been for the first programmed donor2 (“savior baby”),26 there would never have been the extraordinary consequences of biosolidarity which our experience has offered. The birth of this baby made two parents happy; two parents who would otherwise have lived lonely, empty lives. It cannot be denied that the “savior baby” is also important for having made it possible for a life to continue and enjoy new prospects. This is an importance which, even only in the sense of a momentary involuntary altruism,9 remains constant in its long-term consequences: a “life-savior” who makes “living for life” more noble. In his courteous reply to the Nobel prize laureate Rita Levi Montalcini who had taken a contrasting position to ours, the philosopher Marcello Pera said that “we are born also to live” (Corriere della Sera, 8 July 1987). Certainly, opinions can differ concerning the choice of decisive therapeutic solutions, above all when these decisions are “difficult” and problematic. However, management of an HSC transplant requested by the parents of a sick child (especially a transplant from a “savior baby”) is in the hands of the physicians attending the intended recipient. To overrule their expert decision, taken with a great sense of responsibility according to what they consider to be the carefully considered priorities of the case, would undermine the very heart of an institutionalized system which has been carefully built on a codified and exemplary clinical experience.
Supplementary Material
Footnotes
Financial and other disclosures provided by the author using the ICMJE (www.icmje.org) Uniform Format for Disclosure of Competing Interests are available with the full text of this paper at www.haematologica.org.
References
- 1.Burgio GR, Locatelli F. Ethics of creating programmed stem cell donors. Lancet. 2000;356(9245):1868–9. doi: 10.1016/S0140-6736(00)03254-2. [DOI] [PubMed] [Google Scholar]
- 2.Burgio GR, Nespoli L, Porta F. Programming of bone marrow donor for a leukaemic sibling. Lancet. 1987;1(8548):1484–5. doi: 10.1016/s0140-6736(87)92227-6. [DOI] [PubMed] [Google Scholar]
- 3.Kahn JP. Making lives to save lives. Bioethics and law forum. J Andrology. 2001;22(22):191. [PubMed] [Google Scholar]
- 4.Fost NC. Conception for donation. JAMA. 2004;291(7):2125–6. doi: 10.1001/jama.291.17.2125. [DOI] [PubMed] [Google Scholar]
- 5.Robertson JA, Kahn JP, Wagner JE. Conception to obtain hematopoietic stem cells. Hastings Cent Rep. 2002;32(3):34–40. [PubMed] [Google Scholar]
- 6.Robertson JA. Extending preimplantation genetic diagnosis: the ethical debate. Hum Reprod. 2003;18(3):465–71. doi: 10.1093/humrep/deg100. [DOI] [PubMed] [Google Scholar]
- 7.Steptoe PC, Edwards RG. Birth after the reimplantation of a human embryo. Lancet. 1978;312:366. doi: 10.1016/s0140-6736(78)92957-4. [DOI] [PubMed] [Google Scholar]
- 8.Jecker NS. Conceiving a child to save a child: reproductive and filial ethics. J Clin Ethics. 1990;1(2):99–103. discussion 103–7. [PubMed] [Google Scholar]
- 9.Lantos JD. Children as organ donors: an argument for involuntary altruism. In: Burgio GR, Lantos JD, editors. Primum non Nocere today. Elsevier; 1994. pp. 67–75. [Google Scholar]
- 10.Pera M. Should science be supervised and if so, by whom? In: Shea WR, Sitter B, editors. Scientists and their responsibility. Watson Publishing International; 1989. pp. 58–72. [Google Scholar]
- 11.Zucker A. Baby marrow ethicists and privacy. J Med Ethics. 1992;18(3):125–7. doi: 10.1136/jme.18.3.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rachels J. When philosophers shoot from the hip. J Clin Epidemiol. 1992;45(7):799–801. doi: 10.1016/0895-4356(92)90058-u. [DOI] [PubMed] [Google Scholar]
- 13.Toufexis A, Harbison G. Ethics: Creating a Child to save another. Time. 1990 Mar 5; [PubMed] [Google Scholar]
- 14.Verlinsky Y, Rechitsky S, Schoolcraft W, Strom C, Kuliev A. Preimplantation diagnosis for Fanconi anemia combined with HLA matching. JAMA. 2001;285(24):3130–3. doi: 10.1001/jama.285.24.3130. [DOI] [PubMed] [Google Scholar]
- 15.Grewal SS, Kahn JP, MacMillan ML, Ramsay NK, Wagner JE. Successful hematopoietic stem cell transplantation for Fanconi anemia from an unaffected HLA-genotype-identical sibling selected using preimplantation genetic diagnosis. Blood. 2004;103(3):1147–51. doi: 10.1182/blood-2003-02-0587. [DOI] [PubMed] [Google Scholar]
- 16.Kuliev A, Rechitsky S, Tur-Kaspa I, Verlinsky Y. Preimplantation genetics: Improving access to stem cell therapy. Ann NY Acad Sci. 2005;1054:223–7. doi: 10.1196/annals.1345.028. [DOI] [PubMed] [Google Scholar]
- 17.Boyle RJ, Savulescu J. Ethics of using preimplantation genetic diagnosis to select a stem cell donor for an existing person. BMJ. 2001;323(7323):1240–3. doi: 10.1136/bmj.323.7323.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Damewood MD. Ethical implications of a new application of preimplantation diagnosis. JAMA. 2001;285(24):3143–4. doi: 10.1001/jama.285.24.3143. [DOI] [PubMed] [Google Scholar]
- 19.Baruch S, Adamson GD, Cohen J, Gibbons WE, Hughes MR, Kuliev A, Munné S, Rebar RW, Simpson JL, Verlinsky Y, Hudson KL. Genetic testing of embryos: a critical need for data. Reprod Biomed Online. 2005;11(6):667–70. doi: 10.1016/s1472-6483(10)61681-1. [DOI] [PubMed] [Google Scholar]
- 20.Sheldon S, Wilkinson S. Should selecting saviour siblings be banned? J Med Ethics. 2004;30(6):533–7. doi: 10.1136/jme.2003.004150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gavaghan C. “Designer donors”?: Tissue-typing and the regulation of pre-implantation genetic diagnosis. 3 Web JCLI Web Journal of Current Legal Issue Ltd. 2004. http.//webcli.ncl.ac.uk/2004/issue3/gav-aghan3.html.
- 22.Samuel GN, Strong KA, Kerridge I, Jordens CF, Ankeny RA, Shaw PJ. Establishing the role of pre-implantation genetic diagnosis with human leucocyte antigen typing: what place do ”saviour siblings” have in pediatrics transplantation? Arch Dis Child. 2009;94(4):317–20. doi: 10.1136/adc.2008.138529. [DOI] [PubMed] [Google Scholar]
- 23.Gluckman E, Broxmeyer HA, Auerbach AD, Friedman HS, Douglas CW, Devergie A, et al. Hematopoietic reconstitution of a patient with Fanconi’s anemia by means of umbilical cord from an HLA identical sibling. N Eng J Med. 1989;321(17):1174–8. doi: 10.1056/NEJM198910263211707. [DOI] [PubMed] [Google Scholar]
- 24.Bielorai B, Hughes MR, Auerbach AD, Nagler A, Loewenthal R, Rechavi G, Toren A. Successful umbilical cord blood transplantation for Fanconi anemia using preimplantation genetic diagnosis for HLA-matched donor. Am J Hematol. 2004;77(4):397–9. doi: 10.1002/ajh.20201. [DOI] [PubMed] [Google Scholar]
- 25.Strong KA. Informing patient above the emerging treatment options: created “saviour sibling” for haematopoietic stem transplant. MJA. 2009;190(9):506–7. doi: 10.5694/j.1326-5377.2009.tb02531.x. [DOI] [PubMed] [Google Scholar]
- 26.Spriggs M, Savulescu J. Saviour siblings. J Med Ethics”. 2002;28(5):289. doi: 10.1136/jme.28.5.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Petrini C. Notiziario di bioetica: Fatti, persone, interpretazioni in Italia e nel mondo. Biologi Italiani. 2011;1:9–14. [Google Scholar]
- 28.Burgio GR, Verri AP, Nespoli L. Bone marrow transplantation from programmed donor, five years on. Psycho-oncology. 1994;3:61–4. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.