Abstract
Background
National policy experts have estimated that the United States will be 15–20% short of physicians by the year 2020. In 2008, the Big Island of Hawai‘i was found to be 15% short of physicians. The current article describes research to determine the physician supply and demand across the State of Hawai‘i.
Methods
The researchers utilized licensure lists, all available sources of physician practice location information, and contacted provider offices to develop a database of practicing physicians in Hawai‘i. A statistical model based on national utilization of physician services by age, ethnicity, gender, insurance, and obesity rates was used to estimate demand for services. Using number of new state licenses per year, the researchers estimated the number of physicians who enter the Hawai‘i workforce annually. Physician age data were used to estimate retirements.
Results
Researchers found 2,860 full time equivalents of practicing, non-military, patient-care physicians in Hawai‘i (excluding those still in residency or fellowship programs). The calculated demand for physician services by specialty indicates a current shortage of physicians of over 600. This shortage may grow by 50 to 100 physicians per year if steps are not taken to reverse this trend. Physician retirement is the single largest element in the loss of physicians, with population growth and aging playing a significant role in increasing demand.
Discussion
Study findings indicate that Hawai‘i is 20% short of physicians and the situation is likely to worsen if mitigating steps are not taken immediately.
Keywords: Physician workforce, assessment, projections, supply, health workforce, manpower
Background
In 2006 the federal government's Health Resources and Services Administration (HRSA) released a report that forecast a 15%–20% across-the-board, national physician shortage by 2020 with perhaps even greater shortfalls in specialties that care for the elderly, such as cardiology, oncology, and urology. In addition, the federal government calculates that nearly 17,000 more practitioners are needed in HRSA designated shortage areas (rural and inner-city underserved areas) in which 65 million citizens reside.1 Since 2002 at least thirty-one states and twenty-two medical specialty societies have published independent reports, the large majority indicating current or projected future physician shortages.2 National organizations, such as the Association of American Medical Colleges (AAMC) and the Council on Graduate Medical Education (COGME), have called for a nationwide expansion of medical school enrollment by as much as 30%.3 Research in the State of Hawai‘i estimated that the Big Island of Hawai‘i was short by at least 45 physicians in 2007, with that number expected to climb in the future.4
Factors such as changing demographics and implementation of expanded medical coverage enacted under the Patient Affordable Care Act are anticipated to increase demand for health care services in Hawai‘i over the next decade. At the same time, the nation is not producing sufficient numbers of new physicians to maintain current patterns of health care utilization and delivery. Hawai‘i, like the nation, has a large number of physicians likely to retire at the same time that a growing elderly population will increase demand for services. Increasing national competition for health care providers requires that the state plan accordingly to train, attract, and retain providers to meet projected demand for services.
Methodology
Using a combination of Hawai‘i and national data, this research examines the size and makeup of the physician workforce in Hawai‘i and projects current and future demand for services. Human subjects research exemption was obtained for this project from the University of Hawai‘i Institutional Review Board (#15107).
Provider Supply Analysis
The researchers obtained the 2008 and 2010 licensure lists of all MD, DO, PA and APRN licensees from the Hawai‘i State Department of Commerce and Consumer Affairs (DCCA). Information obtained included name, license number, mailing address, and type of license. In December 2009, a voluntary online survey administered at the time of license renewal received 5,820 physician responses (92% response rate for answering at least one question). This survey collected information on practice specialty and practice location(s). All physicians with addresses outside of Hawai‘i were excluded from this analysis unless found to be practicing in Hawai‘i or evaluating/treating Hawai‘i residents (for example teleradiology). The research team used participating provider/staff lists and searched public sources (internet, yellow pages and healthcare directories) to identify practice locations and obtain physician contact information. Physician year of birth and gender were obtained from licensure records and public sources. Community contacts were queried to confirm providers practicing in their communities. The research team contacted physician offices to obtain/confirm practice location, specialty, and hours worked per week when necessary. If a provider office could not be reached but the provider was confirmed as working in the community by two or more sources, their hours worked were estimated by information provided. Specialties were determined by the listing in the American Board of Medical Specialties (AAMS),5 provider lists, and contact with physician offices. All data is stored in a secure access database.
Although no licensure survey was conducted with physician assistants and advanced practice nurse practitioners, electronic searches, community contacts, and medical groups were queried regarding provider locations and whether specialty was in primary care. The data on primary care providers (MD, DO, APRN and PA) was combined for mapping and tracking purposes.
Estimates of future physician supply were based on training, retention and licensure data. Between 85 and 90 non-military physicians graduate from Hawai‘i residency programs every year and approximately 76 medical students will graduate annually (66 at the University of Hawai‘i John A. Burns School of Medicine, and 10 osteopathic physician students from the A.T. Stills University site at Waianae Coast Comprehensive Health Center). The AAMC reports that 40%–50% of the graduates of Hawai‘i training programs are actively practicing in Hawai‘i.6 Analysis of physician licensure numbers suggests that about 100 new physicians started practice in Hawai‘i each year during 2006–2009. While there is no comprehensive data available on physicians having left practice in Hawai‘i, year of birth data provides estimates of the number of physicians turning 65 in a given year (a proxy for retirements).
Provider Demand Analysis
Estimates of current and projected future demand for physician services came from a Physician Demand Model created by The Lewin Group.7 The proprietary model has been used to produce demand estimates for national associations and the Federal Bureau of Health Professions.7 The demand model utilized national healthcare use and delivery patterns to calculate specialty and setting specific provider-per-population ratios by patient age, gender, race/ethnicity, obesity status, and insurance status for physicians, nurse practitioners, and physician assistants. These ratios, combined with population estimates and projections by Hawai‘i region, produced estimates of physician demand under alternative healthcare delivery scenarios. The major data sources used to estimate these ratios include:
2005–2008 data from the National Ambulatory Medical CareSurvey, National Hospital Ambulatory Medical Care Survey, Nationwide Inpatient Sample and Medical Expenditure Panel Survey to model healthcare use by delivery setting and population group;
2008 American Medical Association Masterfile Database to estimate number of physicians by self-reported primary specialty;
data from various years from the American Medical Association, the Medical Group Management Association, the American Board of Internal Medicine Practice Characteristics Survey, and other published sources on the amount of patient care time physicians spend by healthcare delivery setting;
2008 American Community Survey and 2007–2008 Behavioral Risk Factor Surveillance System to provide Hawai‘i-specific estimates of, respectively, uninsured and obesity rates by demographic; and
US Census Bureau population projections for the civilian population of each island.
>
Some exceptions were made for the Hawai‘i model due to the geographic differences from the continental United States. Emergency Medicine physician demand was calculated based on local hospital and emergency department volume rather than using national patterns of care use and delivery. An assumption was made that minimal staffing of a full time ED was 5 FTEs. Similarly, critical care patterns of care delivery were expected to differ in Hawai‘i compared to the US average. Therefore for critical care we used current supply as an estimate for demand (under the assumption of no current shortfall of critical care physicians). Similarly, it is commonly accepted that Psychiatry is underutilized nationally so applying national use and delivery patterns would underestimate demand in Hawai‘i. Therefore, current demand for child and adult psychiatrists was estimated at the current supply level until further research can better identify demand.
Due to uncertainty regarding future healthcare use and delivery patterns, demand was projected under several scenarios. A baseline scenario extrapolated current use and delivery patterns to the future population taking into account changing demographics. This scenario also includes a projected modest increase in demand associated with expanded medical coverage starting in 2014 based on provisions in the national 2010 Affordable Care Act. This scenario assumed that health care use patterns for the newly insured in each demographic group would move from current patterns to patterns similar to those of their commercially insured counterparts.
Alternative scenarios assumed modest improvements in provider productivity and rising per capita use of ambulatory services. Improvements in technology (such as expanded use of decision support systems and electronic medical records) hold the potential to improve provider productivity. Analysis of National Ambulatory Medical Care Survey data over the past decade suggested that for the population aged 40 and older, there is a trend towards higher per capita use of ambulatory services (even after controlling for changing demographics).7 Such a trend could continue over the next decade if there is greater use of patient centered medical homes, accountable care organizations, or other concepts that increase use of ambulatory services (with the goal of preventing expensive hospital-based services). Under this scenario, the per capita annual number of ambulatory visits continues to rise each year by approximately 1.6%, 1.7%, and 2.9% among the age 45–64, 65–74, and 75 and older populations, respectively. This scenario produced a higher estimate of demand for specialties that provide predominantly ambulatory-based services. These proprietary analyses were conducted by The Lewin Group and are represented in Tables 1 and 2.
Table 1.
Projected Demand for FTE Physicians Using Different Scenarios as Calculated by The Lewin Group
| Impact | + | + | + | + | − | = |
| Baseline Scenario | Increasing Per Capita Use of Ambulatory Services | Increasing Provider Productivity | Combined Scenario | |||
| Year | Starting Year Demand | Changing Demographics | Health Care Reform | Net Total Demand | ||
| 2008 | 3,410 | - | - | - | - | 3,410 |
| 2009 | 40 | - | 10 | (20) | 3,440 | |
| 2010 | 80 | - | 20 | (30) | 3,480 | |
| 2011 | 130 | - | 40 | (50) | 3,530 | |
| 2012 | 180 | - | 50 | (70) | 3,570 | |
| 2013 | 240 | - | 60 | (90) | 3,620 | |
| 2014 | 290 | 20 | 80 | (110) | 3,690 | |
| 2015 | 340 | 20 | 100 | (130) | 3,740 | |
| 2016 | 390 | 20 | 110 | (150) | 3,780 | |
| 2017 | 440 | 30 | 130 | (170) | 3,840 | |
| 2018 | 500 | 20 | 150 | (190) | 3,890 | |
| 2019 | 550 | 20 | 170 | (210) | 3,940 | |
| 2020 | 600 | 30 | 190 | (230) | 4,000 | |
Table 2.
Projected FTE Physician Demand by Region (Baseline Scenario) from The Lewin Group
| Year | State | Island | |||
| Hawai‘i (Big Island) | O‘ahu | Kaua‘i | Maui | ||
| 2008 | 3,410 | 470 | 2,390 | 170 | 380 |
| 2009 | 3,450 | 480 | 2,410 | 180 | 380 |
| 2010 | 3,500 | 490 | 2,440 | 180 | 390 |
| 2011 | 3,530 | 500 | 2,460 | 180 | 390 |
| 2012 | 3,590 | 520 | 2,490 | 180 | 400 |
| 2013 | 3,640 | 530 | 2,510 | 190 | 410 |
| 2014 | 3,730 | 560 | 2,550 | 190 | 430 |
| 2015 | 3,770 | 570 | 2,570 | 200 | 430 |
| 2016 | 3,830 | 590 | 2,600 | 200 | 440 |
| 2017 | 3,880 | 600 | 2,630 | 200 | 450 |
| 2018 | 3,930 | 620 | 2,650 | 200 | 460 |
| 2019 | 3,990 | 630 | 2,680 | 210 | 470 |
| 2020 | 4,040 | 650 | 2,700 | 210 | 480 |
Results
Current and Projected Supply
The number of non-military physicians out of residency and fellowship training that provide any direct patient care in Hawai‘i (including part time patient care) totaled 3,203 as of January 31, 2010. Of this number, 2,945 worked at least 20 hours a week. The total FTE of patient-care physicians found working in the State of Hawai‘i is 2,860. This includes all physician specialties, but did not include time spent performing administration, research and non-patient care education. Of the 8,547 physicians licensed to practice medicine in Hawai‘i, only one third actually provided civilian patient-care services in the state.
Projecting future supply of physicians in Hawai‘i was challenging, as the patterns of practice in Hawai‘i are just now beginning to be studied quantitatively. Demographic analysis indicated that 24% of patient care physicians in Hawai‘i are women and that physicians' mean age is 52.5 years. In each year from 2006 to 2009, approximately 100 physicians began practice in Hawai‘i. While little data on workforce attrition is available for physicians in Hawai‘i, an estimated 30 physicians left the Hawai‘i workforce in 2009 for reasons other than retirement based on review of the newly created database. Furthermore, over the next decade nearly 1,200 physicians (42% of the current physician workforce) will reach retirement age (65 or older). Therefore, factoring in retirements, the best estimate of physician supply in the near-term, if no interventions are made, is that Hawai‘i will suffer a net loss of 50 physicians each year, despite a growing demand for services.
Current and Projected Demand
Applying the 2008 national physician-to-population ratios (Lewin Group model described above) to the 2008 population in Hawai‘i and adjusting for differences between Hawai‘i and the US in demographics, rates of uninsured, and obesity rates suggested demand for 3,410 FTE physicians. Between 2008 and 2010 demand for physicians in Hawai‘i grew to approximately 3,500 based on population growth and aging. Estimates were based on the non-military, resident population in Hawai‘i. To estimate demand by tourists, we used medical claims to calculate the percentage of physician encounters that involved patients whose ZIP code was from outside Hawai‘i. For example, approximately 4.5% of encounters by Hawai‘i emergency physicians were for patients with an address outside of Hawai‘i. Across all medical specialties, patients from outside Hawai‘i accounted for approximately 1.4% of physician services (equal to demand for approximately 50 FTE physicians). This demand by non-residents includes approximately 5 FTE emergency physicians, 15 FTE primary care physicians, and 30 FTEs across all the other specialties combined. Primary care specialties include: Family Medicine, General Practice, General Internal Medicine, General Pediatrics, and Geriatrics.
We projected future demand for physicians in Hawai‘i under alternative scenarios, starting with a demand estimate of 3,410 FTEs in 2008. Between 2008 and 2020, growth and aging of the population is projected to increase demand by 600 FTEs (Table 1). Expanded medical coverage under Health Care Reform will likely increase demand by 20–30 FTEs starting in 2014. Under the baseline scenario, by 2020 demand for physicians is likely to increase to approximately 4,040 FTEs. If the trend of increasing per capita use of ambulatory services continues, then by 2020 there could be an additional demand for approximately 190 FTEs. However, if there were modest (0.5% per year) gains in physician productivity, by 2020 the same level of care could be provided by 230 fewer physicians than projected under the baseline scenario. In the aggregate, the decrease in demand from modest productivity gains offset the trend towards higher per capita use of ambulatory services suggesting that by 2020 Hawai‘i will require approximately 4,000 FTEs to provide a level of care comparable to the current US level of care.
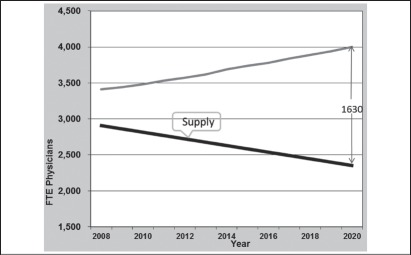
The trends, in isolation, form a range of estimates. If healthcare use and delivery patterns remain constant, then by 2020 Hawai‘i would need slightly more than 4,000 FTEs to provide the current national level of care. If per capita use of ambulatory services were to continue rising, in the absence of productivity gains, then by 2020 demand would rise to over 4,200 FTEs. If there were productivity gains and no increase in per capita use of ambulatory services, then demand would be approximately 3,800 FTEs. This provides a range of 3,800 to 4,200 FTEs, with demand most likely to be approximately 4,000 FTEs by 2020 as demonstrated in Figure 1.
Figure 1.
Projected Demand through 2020
Demand growth will be uneven across medical specialties. Between 2010 and 2020, FTE demand for primary care physicians is projected to grow from 1,240 to 1,430 (15%); demand for internal medicine subspecialties is projected to grow from 460 to 540 (17%); demand for surgical specialties is projected to grow from 690 to 790 (14%); and demand for other patient care specialties is projected to grow from 1,100 to 1,250 (14%).
With 2010 FTE supply and demand of approximately 2,860 and 3,500, respectively, this would suggest the state is short approximately 640 FTEs. However, in some specialties the available supply slightly exceeds projected demand. Summing the shortfall across those specialties where demand exceeds supply suggests a shortfall of approximately 670 FTE physicians. Of this, approximately one half is primary care (with the shortfall primarily among family practice and general internal medicine) and a significant shortfall for cardiology, neurosurgery, infectious disease and general surgery.
Adequacy of Supply by Hawai‘i Region
Projected growth in demand will be uneven across regions, reflecting differences in demographics and Census Bureau projections of population growth (Table 2). Across Hawai‘i, demand is projected to grow approximately 15% between 2010 and 2020 (see figure 2). In percentage terms, growth is highest on the Big Island (33%) and Maui (23%), followed by Kaua‘i (17%) and O‘ahu (11%). In absolute terms, the increase in demand of approximately 540 FTEs between 2010 and 2020 (under the baseline scenario) comes primarily from O‘ahu (+260 FTEs) and the Big Island (+160), followed by Maui (+90) and Kaua‘i (+30).
Figure 2.
Supply and Demand Forecast
Finally, based on an analysis of medical claims that indicate the ZIP code of patients who received care, we calculated demand for physicians in each region (controlling for demographics). Summary findings from this analysis suggest that patients on Oahu have greater access to specialist services but use relatively fewer primary care services.
Primary Care Data Analysis
ArcGIS mapping software was utilized to map current (2010) supply and demand of the Hawai‘i primary care workforce (DO, MD, PA, APRN) based on the calculations described above and the information in Table 3 (see figure 3).
Table 3.
Supply and Demand Estimates for Primary care Physician Assistants and Nurse Practitioners 2011
| Kaua‘i | O‘ahu | Lana‘i | Moloka‘i | Maui | Hawai‘i (Big Island) | |
| Physician Assistants (primary care) Demand |
4 | 37 | 0.2 | 0.4 | 7.5 | 11 |
| Physician Assistants (primary care) Supply |
2.6 | 8.6 | 0.0 | 0.0 | 9.5 | 4 |
| Nurse Practitioners (primary care) Demand |
16 | 175 | 0.7 | 1.7 | 33.6 | 45 |
| Nurse Practitioners (primary care) Supply |
8.2 | 113.4 | 0.8 | 1.6 | 7.6 | 30.9 |
Figure 3.
Primary Care Supply and Demand Comparison by Island
Discussion
Prior to this analysis, healthcare experts in Hawai‘i generally accepted national estimates based on AMA Masterfile data in which the state consistently ranked in the top ten in terms of physicians per population.8 The data now shows that Hawai‘i is at least 600 physicians, or 15 to 20% short of the number needed to provide services comparable to the nation as a whole. This shortfall may grow to 1,600 providers by 2020 if systemic changes are not implemented. At present, the greatest shortages are in primary care, cardiology, infectious disease, neurology, gastroenterology, and surgical specialties such as neurosurgery. Furthermore, the state also has a maldistribution problem, as many shortages are significantly worse on the neighbor islands.
The study found that if current trends continue, Hawai‘i will suffer a net loss of practicing physicians every year. Physician retirement is the single largest contributor to the projected growing provider shortage, although population growth and aging also play a significant role by increasing demand. Unfortunately, as the national physician shortage worsens, Hawai‘i should expect to encounter growing competition for doctors from communities throughout the country, which may limit the inflow of physicians and put Hawai‘i in an even more precarious position with respect to providing consistent access to medical care.
Study Strengths and Limitations
Estimates of current supply reflect a labor intensive process to account for each active physician in Hawai‘i and found significant discrepancies between the number of physicians licensed to practice in the state and those actually providing patient care. The demand analysis uses a standardized approach and consistent data sources to model supply and demand by medical specialty and region across Hawai‘i. The study uses the most recently available data, with the approach consistent with that used by the Federal Bureau of Health Professions and national professional associations.
Limitations of this study include the use of average US utilization statistics, which may vary from Hawai‘i utilization rates even after adjusting for differences in demographics, rates in medical insurance coverage, and obesity rates. Hawai‘i, which has the nation's lowest Medicare physician and hospital spending per beneficiary,9 also has indigenous groups with greater health challenges than most of the US population and a very diverse ethnic mix. While current patterns of care delivery reflect the realities of the health care system in terms of access to care, these patterns do not indicate true need for services. For specialties such as psychiatry where there is a national perception of under-supply, utilization will be lower than actual need. Furthermore, this analysis does not factor in productivity issues related to generational and gender changes in the workforce or the likely growth of the “concierge medicine” business model, which all decrease available physician supply. The scenario modeling productivity increases are based on conservative assumptions, but little information is known about how implementation of new technologies will affect physician productivity. On the supply side, physician hours worked and retirement patterns in Hawai‘i and propensity to move out of the state are not well understood.
The authors realize that this study is very physician-centric and that the picture of healthcare in Hawai‘i is incomplete without better information on other primary care providers, particularly physician assistants and nurse practitioners. While further research will be performed in this area, a particular challenge faced by researchers was finding practice locations for providers who do not advertise in phone books or on the Internet. Although 91% of physicians who relicensed online filled out part of all of the survey described above, such a survey was not implemented for physician assistants or nurse practitioners. While there are less than 100 full time practicing physician assistants, there are over 300 full-time equivalents of practicing nurse practitioners, many of whom are employed by medical practices or groups, but not publicized, so the researchers could not be sure all practicing primary care APRNs were identified. Therefore the all-provider primary care maps in Figure 4 may reflect an under-documentation of nurse practitioners and this will be further examined.
Other limitations include difficulty in assessing the use of telemedicine in Hawai‘i. However, utilization is very low as assessed by the Pacific Basin Telemedicine Association, and it is a target area for meeting workforce shortages. The fact that only a third of the physicians licensed in Hawai‘i actually practice patient care is an area for further study. Initial investigations indicate this is a result of the high military presence (the fact that military providers only need to maintain a license in one state, but can practice elsewhere for military facilities), the low licensure fees, the possibility that some providers hope to move to Hawai‘i, and the tendency for retired physicians to maintain their licenses. Finally, it is difficult to compare the result to findings in other states, as there is no comparable data collection and analysis performed in the US to date. However, the authors believe that the counting of FTEs directly (instead of estimating based on national databases), and the use of a national model for demand was the most practical method to follow in order to obtain a statewide demand picture.
Future Research
The above limitations suggest important areas for future research. Future research will include tracking practice location of physicians trained in, entering and leaving practice in Hawai‘i, as well as collaborative efforts to identify all practicing providers. Inclusion of questions in the Hawai‘i Health Survey regarding whether patients are able to obtain needed services will help inform the research base. Finally, a qualitative analysis of needs for psychiatric services is being designed to better assess demand in Hawai‘i.
Conflict of Interest
None of the authors report any conflict of interest.
References
- 1.Health Resources Services Administration, author. Bureau of Health Professions. Shortage Designation: HPSAs, MUAs & MUPs. [January 13, 2011]. Available from: http://bhpr.hrsa.gov/shortage/
- 2.Association of American Medical Colleges, Recent Studies and Reports on Physician Shortages in the U.S. 2010. Nov, [January 18, 2011]. Available from: https://www.aamc.org/download/100598/data/recentworkforcestudiesnov09.pdf.
- 3.Association of American Medical Colleges, author. AAMC Statement on the Physician Workforce. 2006. Jun, [May 15, 2008]. Available from: http://www.aamc.org/workforce/workforceposition.pdf.
- 4.Withy K, Andaya J, Vitousek S, Sakamoto D. Hawaii Island Health Workforce Assessment 2008. Hawaii Med J. 2009 Dec;68(11):268–272. [PubMed] [Google Scholar]
- 5.American Board of Medical Specialties, author. The Official ABMS Directory of Board Certified Medical Specialists 2009. New York: Elsevier; 2008. Dec, [Google Scholar]
- 6.Association of American Medical Colleges, author. 2009 State Physician Workforce Data Book. 2009. Nov, [January 17, 2011]. Available from: https://www.aamc.org/download/47340/data/statedata2009.pdf.
- 7.Association of American Medical Colleges, The Complexities of Physician Supply and Demand: Projections Through 2025. 2008. Nov, [January 13, 2011]. Available from: http://services.aamc.org/publications/showfile.cfm?file=version122.pdf.
- 8.Health Resources and Services Administration, National Center for Health Workforce Analysis, author. The Hawaii Health Workforce: Highlights from the Health Workforce Profile. [April 3, 2010]. Available from: http://bhpr.hrsa.gov/healthworkforce/reports/statesummaries/hawaii.htm.
- 9.Centers for Medicare and Medicaid Services, author. Physician Fee Schedule per PRS Carrier Specific Files. [April 3, 2010]. Available from: http://www.cms.gov/PhysicianFeeSched/PFSCSF/list.asp#TopOfPage.