Abstract
Background
Access to care for patients in Hawai‘i is compromised by a significant primary care workforce shortage. Not only are there not enough primary care providers, they are often not practicing in locations of high need such as rural areas on the neighbor islands or in the Pacific.
Methods
This study used geographic information systems (GIS) spatial analysis to look at practice locations for 86 University of Hawai‘i Family Medicine and Community Health graduates from 1993 to the 2010. Careful alumni records were verified and entered into the data set using the street address of major employment. Questions to be answered were (1) what percentage of program graduates remain in the state of Hawai‘i and (2) what percentage of graduates practice in health professional shortage areas (HPSAs) throughout the United States.
Results
This study found that 73 percent of graduates remain and practice in Hawai‘i with over 36 percent working in Health Professional Shortage Areas.
Discussion
Spatial analysis using GIS residency footprinting may be an important analytic tool to ensure that graduate medical education programs are meeting Hawai‘i's health workforce needs.
Introduction
The University of Hawai‘i (UH), John A. Burns School of Medicine, Department of Family Medicine and Community Health has a mission to create family physicians to serve the diverse healthcare needs of underserved areas of Hawai‘i and the Pacific. The shortage of physicians in Hawai‘i and other areas of the Pacific, specifically in rural and neighbor island settings, has led to a call to expand graduate medical education programs.1
Geographic information systems (GIS) are increasingly recognized as a tool for spatial analysis with application to health systems planning.2 This project analyzed the impact of the University of Hawai‘i Family Medicine Residency Program by locating graduate clinical practice sites worldwide. The study attempted to determine the impact on the State of Hawai‘i regarding retention of program graduates and percentage practicing in health professional shortage areas.
Methods
The UH Family Medicine Residency Program has maintained contact with all of its graduates and has a Microsoft Excel database which contains information including: (1) the graduates' year of residency completion; (2) if the graduate meets the HRSA definition of a “medically underrepresented minority” group; (3) practice location and type; (4) designation of the practice in a federally designated health professional shortage area (HPSA), or medically underserved area or population (MUA/P), rural Oahu, neighbor islands of Hawai‘i; and (5) whether the graduate is in academic medicine or plays a leadership/directorship role in their practice. The American Academy of Family Physicians database and a Google search were used to validate the current home and practice location of each graduate. When necessary, emails were sent to the graduates to verify information. ID numbers were assigned to zip codes (or country names for graduates in international settings) and the information was plotted using Environmental Systems Research Institute (ESRI, Redlands, CA) ArcGIS version 9.3.1 GIS software. For the detailed map of Oahu, HPSA designation and number of graduates in each site was overlaid.
Results
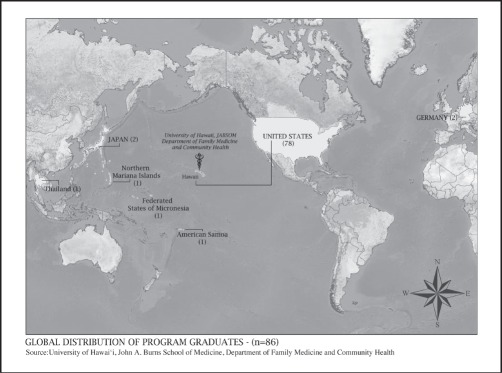
Map 1 shows the global distribution of program graduates (N = 86) with the majority (78) remaining in the United States, three in the US Affiliated Pacific, three in the Asian Pacific Rim, and two in Western Europe (Germany).
Map 1.
Distribution of UH Family Medicine Residency Program Graduates across the World
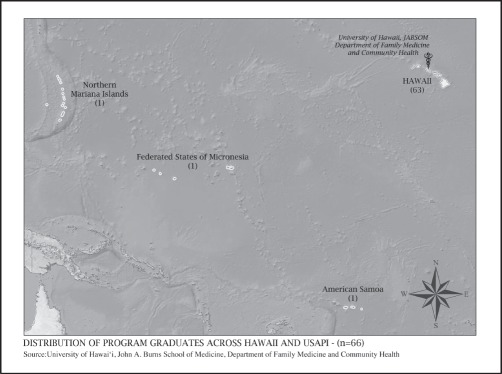
Map 2 shows the distribution of program graduates throughout the Pacific (N = 66) with 63 remaining in Hawai‘i and three in the US Affiliated Pacific including one each in the Commonwealth of the Northern Mariana Islands, the Federated States of Micronesia (Yap State, and the Territory of American Samoa).
Map 2.
Distribution of UH Family Medicine Residency Graduates across Hawaii and USAPI
Maps 3 and 4 depict the distribution of graduates across the continental United States by state and county (N = 15), and the distribution across the State of Hawai‘i by county (N = 63) with the majority working on O‘ahu.
Maps 3 & 4.
Distribution of UH Family Medicine Residency Graduates across the United States (grouped by county)
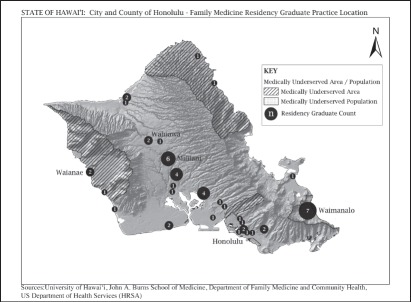
Map 5 depicts the medically underserved areas on the island of Oahu overlaid with the distribution of family physician practice locations (N = 50).
Map 5.
Distribution of UH Family Medicine Residency Graduates across O‘ahu (grouped by practice address)
Discussion
While physician shortage has received a great deal of attention in discussions on improving health in Hawai‘i, clearly geographic distribution is an equally vexing problem. The question is not only how many physicians, but also where physicians practice in relation to patient population and needs. This study found that 73 percent of graduates remain and practice in Hawai‘i with over 36 percent working in HPSA's. These findings suggest that the UH Family Medicine Residency Program meets its mission of retaining program graduates in Hawai‘i and the Pacific and providing physicians to medically underserved areas of the state.
While this project examined a single residency program, other physicians as well as non-physician providers make up the primary care workforce. Understanding the contributions and geographic distribution of all health providers may be useful for health planning. These particular maps fail to depict cultural differences in relation to health seeking behavior. Further mapping projects might identify particular ethnic/cultural groups with disparate health status and link physician capacity in those communities. As the University of Hawai‘i and the state go forward to plan the health workforce of the future, understanding the ability of graduate medical education programs to retain their graduates and place them in areas of high need will be important. This residency footprinting project suggests that local training is an important strategy to retain physicians in communities of need and should be expanded. Spatial analysis using GIS residency footprinting may be an important analytic tool for guiding this process.
Conflict of Interest
None of the authors identify any conflict of interest.
References
- 1.Report on Findings from the Hawaii Physician Workforce Assessment Project. John A. Burns School of Medicine, Area Health Education Center; 2010. Dec, [Google Scholar]
- 2.Reese VF, McCann JL, Bazemore AW, Phillips RL., Jr Residency footprints: Assessing the impact of training programs on the local physician workforce and communities. Family Medicine. 2008;40(5):339–344. [PubMed] [Google Scholar]