Abstract
West Nile virus (WNV) is a member of the family Flaviviridae and is a neurotropic pathogen responsible for severe human disease. Flavivirus-infected cells release virus particles that contain variable numbers of precursor membrane (prM) protein molecules at the viral surface. Consequently, antibodies are produced against the prM protein. These antibodies have been shown to activate the infectious potential of fully immature flavivirus particles in vitro. Here, we provide in vivo proof that prM antibodies render immature WNV infectious. Infection with antibody-opsonized immature WNV particles caused disease and death of mice, and infectious WNV was found in the brains and sera.
West Nile virus (WNV) is a mosquito-borne flavivirus and an emerging pathogen responsible for encephalitis and neurological disease in humans (Mackenzie et al., 2004). Members of the family Flaviviridae, which also include dengue virus (DENV) and tick-borne encephalitis (TBEV) virus, are enveloped, ssRNA viruses and contain three structural proteins: capsid (C), envelope (E) and membrane (M). In mature virions, E is organized as 90 homodimers that lie flat against the viral surface forming a ‘smooth’ protein shell (Kuhn et al., 2002).
Flaviviruses infect cells via receptor-mediated endocytosis, which is mediated by the E glycoprotein (Lindenbach, 2001; Mukhopadhyay et al., 2005; van der Schaar et al., 2007). Following RNA replication, immature virions are formed containing precursor membrane protein (prM) in a heterodimeric configuration with E extending from the viral surface as 60 trimeric spikes (Kuhn et al., 2002). These newly formed particles mature during virus egress through the secretory pathway, whereafter cleavage of prM by a furin-like protease generates infectious particles (Stadler et al., 1997). This cleavage is known to be fairly inefficient as the prM content of virus particles released from DENV- and WNV-infected cells is approximately 30 % (Moesker et al., 2010; Zybert et al., 2008). Furthermore, the prM content is variable on a per-particle basis, as recent studies have shown that both fully immature as well as partially immature, or nearly mature, particles exist in wild-type (wt) preparations of DENV and WNV (Junjhon et al., 2010; Li et al., 2008; Stadler et al., 1997).
Recent studies have shown that anti-prM is a major component of the serological response to DENV infection (Cardosa et al., 2002; Dejnirattisai et al., 2010). For a long time the role of prM antibodies during flavivirus infection was not understood, as numerous functional studies revealed that immature prM-containing flavivirus particles are non-infectious (Elshuber & Mandl, 2005; Stadler et al., 1997). Indeed, studies on TBEV, DENV and WNV have shown that cleavage of prM to M is required to activate the membrane-fusion machinery of the virus (Guirakhoo et al., 1991; Moesker et al., 2010; Stadler et al., 1997; Zybert et al., 2008). Interestingly, however, we recently observed that prM antibodies bind to fully immature DENV particles and facilitate cellular entry through Fc receptor and fusion in a furin-dependent manner (Rodenhuis-Zybert et al., 2010). Furthermore, antibodies against prM have been shown to enhance wt DENV infection (Huang et al., 2006) and the levels of prM antibodies were found to be higher in patients with secondary infections compared with sera from primary DENV infections (Lai et al., 2008). Moreover, a recent study showed that human anti-prM antibodies fail to efficiently neutralize immature DENV infection in primary monocytes and enhance infection 20–70 % even at high concentrations (Dejnirattisai et al., 2010). Also, human anti-prM antibodies did not significantly protect AG129 interferon-deficient mice from WNV infection (Calvert et al., 2011). This indicates that during natural flavivirus infection, depending on the proportion of mature and immature virions present in a population, prM antibodies may set the stage for antibody-dependent enhancement of infection. This also suggests that immature virus could potentially be an important component of flavivirus infection and as such contribute to the development of disease.
In this study, we investigated the ability of prM antibodies to facilitate immature flavivirus infection in vivo by using the well-established model of West Nile virus (NY99) infection in mice. To this end, wt WNV was generated in baby hamster kidney (BHK) cells and immature WNV (prMWNV) was generated in furin-deficient LoVo cells, as described previously (Moesker et al., 2010). We previously reported that LoVo-derived WNV is almost completely immature, the prM content being 87±7 % (Moesker et al., 2010). The specific infectivity of LoVo-derived WNV was determined by measuring the number of infectious units by plaque assay on baby hamster kidney (clone 15) cells (BHK-15) and the number of genome-containing particles (GCPs) by quantitative PCR (qPCR). To determine the number of GCPs, viral RNA was extracted by using a QIAamp viral RNA mini kit (Qiagen). Next, cDNA was synthesized by RT-PCR and the qPCR was performed similarly to the method described before for DENV (van der Schaar et al., 2008). For WNV, the forward primer (5′-GTTGGCGGCTGTTTTCTTTC-3′), the reverse primer (5′-GGGATCTCCCAGAGCAGAATT-3′) and a TaqMan probe (5′-FAM–AATGGCTTATCACGATGCCCGCC–TAMRA-3′; Eurogentec) were used. The concentration of GCPs was determined by the use of a standard curve based on a cDNA plasmid encoding the non-structural genes of WNV NY99 (kind gift from Dr G.P. Pijlman, Wageningen University, The Netherlands). The p.f.u. : particle ratio of wt WNV was, on average (mean) 1 : 330 (n = 2), which is in agreement with earlier reports (Moesker et al., 2010; Wengler & Wengler, 1989). LoVo-derived virus was found to be virtually non-infectious, the p.f.u. : particle ratio being approximately 30 000-fold lower compared with that of wt WNV.
Next, the infectious properties of prMWNV particles in the presence of increasing concentrations of prM-specific antibody Ab25888 (Abcam) were determined in Fc-receptor expressing P388D1 mouse macrophage-like cells (Fig. 1). Virus or preformed virus–antibody complexes were added to P338D1 cells at a multiplicity of genome-containing particles (m.o.g.) of 10. At 24 h post-infection (p.i.), the media were harvested and the number of viral particles produced was measured by plaque assay on BHK-15 cells. Fig. 1 shows that prMWNV is non-infectious in P388D1 cells, as no p.f.u. are detected in the absence of antibodies. Interestingly, and consistent with DENV (Dejnirattisai et al., 2010; Rodenhuis-Zybert et al., 2010), prM antibodies render fully immature WNV particles infectious (Fig. 1a). The infectivity is markedly increased at antibody concentrations of 0.0005, 0.005 and 0.05 µg ml−1. At high antibody concentrations, no enhancement of infection is observed. Subsequently, immunofluorescence studies were performed to quantify the number of infected cells for wt and prM-opsonized immature virus (Fig. 1b). To this end, cells were fixed at 24 h p.i. with 4 % paraformaldehyde and stained with an anti-WNV-E-protein antibody conjugated with TRITC (L2). The percentage of infected cells was determined by counting the number of infected, fluorescently labelled, cells per 1000 cells in three separate experiments. We found that 4.77±1.02 % of the cells are infected with prM-opsonized immature WNV and 7.23±1.5 % with wt WNV, under the conditions of the experiment. This indicates that the specific infectivity of antibody-opsonized immature WNV, under conditions of efficient antibody-dependent enhancement of infection, is just over half of that of wt WNV. Enhancement of infection of prMWNV particles opsonized with antibodies was seen in multiple Fc-receptor-expressing cell lines, including human erythroleukaemic K562 cells and human leukaemic monocyte lymphoma U937 cells (data not shown). To determine whether the observed enhancement is dependent on the enzymic activity of furin, P388D1 cells were treated with 25 µM of the furin-specific inhibitor decanoyl-l-arginyl-l-valyl-l-lysyl-l-arginyl-chloromethylketone (decRRVKR-CMK; Calbiochem) prior to and during infection, as described previously (Rodenhuis-Zybert et al., 2010). Consistent with our results on DENV, enhancement of infection by prM-antibody-coated prMWNV particles is strictly dependent on furin activity (Fig. 1a).
Fig. 1.
prM-specific antibody Ab25888 renders immature WNV particles infectious in a furin-dependent manner. (a) P388D1 cells were infected with immature WNV at a m.o.g. of 10 in the presence of increasing concentrations of anti-prM antibody Ab25888. When indicated, 25 µM furin inhibitor (FI) was added to the cells prior and during infection. At 26 h p.i. the supernatant was harvested and the production of virus particles was measured by plaque assay on BHK-15 cells. Data are expressed as means of duplicate experiments. The error bars indicate sd. (b) WNV-infected P388D1 cells were fixed with 4 % paraformaldehyde and stained with an antibody against WNV E protein conjugated to TRITC. Representative images are shown for WT WNV infection (upper panels) and prM antibody-opsonized immature WNV (lower panels).
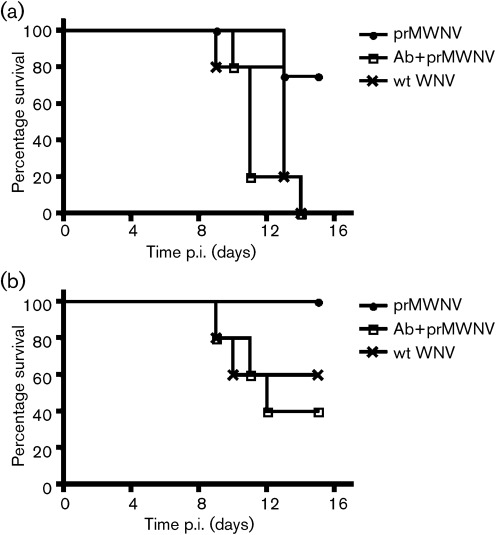
After confirming the infectivity of antibody-opsonized prMWNV in vitro, we wanted to determine whether the virus was infectious in vivo. If antibody-opsonized prMWNV particles are infectious in vivo, wt WNV particles should be produced after a single round of infection, leading to encephalitis and death in mice (Bai et al., 2009; Wang et al., 2004). Furthermore, if antibody-opsonized prMWNV can cause similar mortality due to encephalitis, it may indicate that these virions are able to contribute to disease and pathogenesis during natural infection. To test this, prMWNV was incubated with PBS (pH 7.2) alone or 10 µg prM antibody ml−1 for 1 h at 37 °C. Infection was done via intra-peritoneal injection into strain c57L/b6 mice. The final concentration of opsonized virus was 3.4×105 or 3.4×106 GCPs per mouse. The same number of GCPs of wt WNV was used to infect a control group of mice. The number of GCPs given to the mice was calculated on the basis of 103 or 104 infectious particles of wt WNV, respectively. For each infectious condition n = 5. The mice injected with either 3.4×105 or 3.4×106 GCPs of prMWNV alone did not show any signs of infection and had a much greater survival rate than mice infected with wt WNV. Interestingly, the prM antibody-opsonized prMWNV caused similar disease and death to that seen for the wt WNV-infected mice, thus demonstrating that prM antibodies render prMWNV particles infectious (Fig. 2).
Fig. 2.
prM-specific antibody Ab25888 renders prMWNV particles infectious in vivo. Mice were infected with wt WNV, prMWNV or prM antibody-opsonized (Ab) prMWNV via intra-peritoneal injection. Curves show percentage survival up until 16 days p.i. For each curve, n = 5 and P<0.05. (a) Infection with 3.4×106 GCPs WNV per mouse. (b) Infection with 3.4×105 GCPs WNV per mouse.
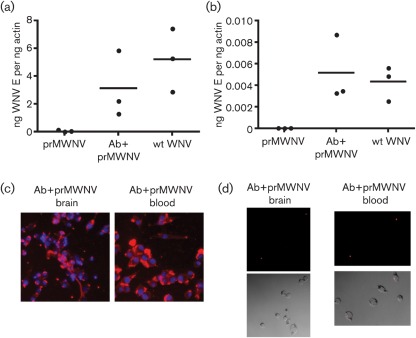
To confirm that the mortality in the mice was because of WNV infection in the brain, an additional group of mice were infected with either wt WNV, prMWNV alone or antibody-opsonized prMWNV. Blood was drawn from the mice on day 3 p.i. and on day 7 p.i. the brains were collected and homogenized in 1 ml PBS. RNA was isolated from both whole blood and brain homogenate, and the cDNA made was used in a qPCR to detect the presence of the WNV E gene. WNV was detected in the blood on day 3 and the brain on day 7 for mice that received prM antibody-opsonized prMWNV, but not in blood or brain from mice injected with prMWNV alone (Fig. 3a, b). The day-3 blood and day-7 brain homogenates were also used to infect P388D1 macrophage-like cells. As expected, the mice that received prMWNV alone did not produce any infectious virus in their blood or brains. The mice that were infected with wt WNV and antibody-opsonized prMWNV had infectious virus in their blood on day 3 of infection and in their brains on day 7 of infection (Fig. 3c). To confirm that the fluorescent signal seen in Fig. 3(c) reflects production of infectious WNV virus, and not simply staining of already-infected cells from the blood and brain, we harvested the media from these cultures and used these to infect new P388D1cells. We were able to detect WNV infection in these cells via immunofluorescence staining by using an antibody against WNV E protein conjugated with TRITC (Fig. 3d). Taken together, these results confirm that mice infected with antibody-opsonized prMWNV particles died from a typical wt WNV infection.
Fig. 3.
Brain homogenates and blood from prM-opsonized prMWNV are infectious and infected cells produce new infectious WNV. Mice were infected with 107 GCPs of either wt WNV, prMWNV or prM antibody-opsonized (Ab) prMWNV via intra-peritoneal injection. RNA was isolated from brain (a) or blood (b) of infected mice and qPCR was used to detect the WNV E gene. Data are shown as ng WNV E per ng β-actin; n = 3 per group. (c, d) Brains from mice infected with prM-specific antibody-opsonized WNV were homogenized in 1 ml PBS and used to infect P388D1 cells (c, left panel). Blood samples from the same mice were used to infect P388D1 cells (c, right panel). (d) At 7 days p.i., cell-culture supernatants were used to infect new P388D1 cells. Cells were fixed with 4 % paraformaldehyde and stained with an antibody against WNV E conjugated to TRITC (red colour). A DAPI counterstain was used to show the nucleus in (c). Representative images are shown for each infection.
A major risk factor for the development of severe dengue infection is the presence of pre-existing antibodies (Halstead, 2003). It is well accepted that antibodies target DENV particles to cells that are highly permissive to infection, leading to a higher number of infected cells and eventually to increased disease burden (Halstead, 2003). This report shows for the first time that prM antibodies have the capacity to enhance the number of infectious particles present in vivo and strengthens the notion that immature particles and prM antibodies may increase flaviviral disease burden in humans.
Recent characterization of the humoral response of dengue patients with severe disease identified prM antibodies as the dominant fraction of the human antibody repertoire (Dejnirattisai et al., 2010). Furthermore, Rai et al. (2008) showed a positive correlation between the circulating prM antibody titre and disease severity. These observations not only suggest that prM antibodies may be unfavourable for the host but might also have important repercussions for vaccine development. Generation of antibodies against the prM protein activates the infectious properties of immature DENV particles and therefore may have adverse effects on protection from infection. Future clinical studies are therefore required to probe the role of prM antibodies and immature particles in disease pathogenesis, and to determine which types of antibodies are necessary for protection against disease.
Acknowledgements
This work was supported by the Pediatric Dengue Vaccine Initiative (J. M. S.), NIH grants UO1 AI070343 and T32 AI07404 (E. F.), and by the Dutch Organization for Scientific research (NWO-ALW) to J. M. S. E. F. is an investigator with the Howard Hughes Medical Institute.
References
- Bai F., Town T., Qian F., Wang P., Kamanaka M., Connolly T. M., Gate D., Montgomery R. R., Flavell R. A., Fikrig E. (2009). IL-10 signaling blockade controls murine West Nile virus infection. PLoS Pathog 5, e1000610 10.1371/journal.ppat.1000610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvert A. E., Kalantarov G. F., Chang G. J., Trakht I., Blair C. D., Roehrig J. T. (2011). Human monoclonal antibodies to West Nile virus identify epitopes on the prM protein. Virology 410, 30–37 10.1016/j.virol.2010.10.033 [DOI] [PubMed] [Google Scholar]
- Cardosa M. J., Wang S. M., Sum M. S., Tio P. H. (2002). Antibodies against prM protein distinguish between previous infection with dengue and Japanese encephalitis viruses. BMC Microbiol 2, 9 10.1186/1471-2180-2-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dejnirattisai W., Jumnainsong A., Onsirisakul N., Fitton P., Vasanawathana S., Limpitikul W., Puttikhunt C., Edwards C., Duangchinda T., et al. & other authors (2010). Cross-reacting antibodies enhance dengue virus infection in humans. Science 328, 745–748 10.1126/science.1185181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elshuber S., Mandl C. W. (2005). Resuscitating mutations in a furin cleavage-deficient mutant of the flavivirus tick-borne encephalitis virus. J Virol 79, 11813–11823 10.1128/JVI.79.18.11813-11823.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guirakhoo F., Heinz F. X., Mandl C. W., Holzmann H., Kunz C. (1991). Fusion activity of flaviviruses: comparison of mature and immature (prM-containing) tick-borne encephalitis virions. J Gen Virol 72, 1323–1329 10.1099/0022-1317-72-6-1323 [DOI] [PubMed] [Google Scholar]
- Halstead S. B. (2003). Neutralization and antibody-dependent enhancement of dengue viruses. Adv Virus Res 60, 421–467 10.1016/S0065-3527(03)60011-4 [DOI] [PubMed] [Google Scholar]
- Huang K. J., Yang Y. C., Lin Y. S., Huang J. H., Liu H. S., Yeh T. M., Chen S. H., Liu C. C., Lei H. Y. (2006). The dual-specific binding of dengue virus and target cells for the antibody-dependent enhancement of dengue virus infection. J Immunol 176, 2825–2832 [DOI] [PubMed] [Google Scholar]
- Junjhon J., Edwards T. J., Utaipat U., Bowman V. D., Holdaway H. A., Zhang W., Keelapang P., Puttikhunt C., Perera R., et al. & other authors (2010). Influence of pr-M cleavage on the heterogeneity of extracellular dengue virus particles. J Virol 84, 8353–8358 10.1128/JVI.00696-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn R. J., Zhang W., Rossmann M. G., Pletnev S. V., Corver J., Lenches E., Jones C. T., Mukhopadhyay S., Chipman P. R., Strauss E. G. (2002). Structure of dengue virus: implications for flavivirus organization, maturation, and fusion. Cell 108, 717–725 10.1016/S0092-8674(02)00660-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai C. Y., Tsai W. Y., Lin S. R., Kao C. L., Hu H. P., King C. C., Wu H. C., Chang G. J., Wang W. K. (2008). Antibodies to envelope glycoprotein of dengue virus during the natural course of infection are predominantly cross-reactive and recognize epitopes containing highly conserved residues at the fusion loop of domain II. J Virol 82, 6631–6643 10.1128/JVI.00316-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L., Lok S. M., Yu I. M., Zhang Y., Kuhn R. J., Chen J., Rossmann M. G. (2008). The flavivirus precursor membrane-envelope protein complex: structure and maturation. Science 319, 1830–1834 10.1126/science.1153263 [DOI] [PubMed] [Google Scholar]
- Lindenbach D. R. C. M. (2001). Flaviviridae: the viruses and their replication. In Fields Virology, 4th edn, pp. 991–1041 Edited by Knipe D. M., Howley P. M., Griffin D. E., Lamb R. A., Roizman B., Strauss S. E. Philadelphia, PA: Lippincott Williams & Wilkins [Google Scholar]
- Mackenzie J. S., Gubler D. J., Petersen L. R. (2004). Emerging flaviviruses: the spread and resurgence of Japanese encephalitis, West Nile and dengue viruses. Nat Med 10 (Suppl.), S98–S109 10.1038/nm1144 [DOI] [PubMed] [Google Scholar]
- Moesker B., Rodenhuis-Zybert I. A., Meijerhof T., Wilschut J., Smit J. M. (2010). Characterization of the functional requirements of West Nile virus membrane fusion. J Gen Virol 91, 389–393 10.1099/vir.0.015255-0 [DOI] [PubMed] [Google Scholar]
- Mukhopadhyay S., Kuhn R. J., Rossmann M. G. (2005). A structural perspective of the flavivirus life cycle. Nat Rev Microbiol 3, 13–22 10.1038/nrmicro1067 [DOI] [PubMed] [Google Scholar]
- Rai C.-I., Lei H.-Y., Lin Y.-S., Liu H.-S., Chen S.-H., Chen L.-C., Yeh T.-R. (2008). Epitope mapping of Dengue-virus-enhancing monoclonal-antibody using phage display peptide library. Am J Infect Dis 4, 76–84 10.3844/ajidsp.2008.76.84 [DOI] [Google Scholar]
- Rodenhuis-Zybert I. A., van der Schaar H. M., da Silva Voorham J. M., van der Ende-Metselaar H., Lei H. Y., Wilschut J., Smit J. M. (2010). Immature dengue virus: a veiled pathogen? PLoS Pathog 6, e1000718 10.1371/journal.ppat.1000718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stadler K., Allison S. L., Schalich J., Heinz F. X. (1997). Proteolytic activation of tick-borne encephalitis virus by furin. J Virol 71, 8475–8481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Schaar H. M., Rust M. J., Waarts B. L., van der Ende-Metselaar H., Kuhn R. J., Wilschut J., Zhuang X., Smit J. M. (2007). Characterization of the early events in dengue virus cell entry by biochemical assays and single-virus tracking. J Virol 81, 12019–12028 10.1128/JVI.00300-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Schaar H. M., Rust M. J., Chen C., van der Ende-Metselaar H., Wilschut J., Zhuang X., Smit J. M. (2008). Dissecting the cell entry pathway of dengue virus by single-particle tracking in living cells. PLoS Pathog 4, e1000244 10.1371/journal.ppat.1000244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang T., Town T., Alexopoulou L., Anderson J. F., Fikrig E., Flavell R. A. (2004). Toll-like receptor 3 mediates West Nile virus entry into the brain causing lethal encephalitis. Nat Med 10, 1366–1373 10.1038/nm1140 [DOI] [PubMed] [Google Scholar]
- Wengler G., Wengler G. (1989). Cell-associated West Nile flavivirus is covered with E+pre-M protein heterodimers which are destroyed and reorganized by proteolytic cleavage during virus release. J Virol 63, 2521–2526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zybert I. A., van der Ende-Metselaar H., Wilschut J., Smit J. M. (2008). Functional importance of dengue virus maturation: infectious properties of immature virions. J Gen Virol 89, 3047–3051 10.1099/vir.0.2008/002535-0 [DOI] [PubMed] [Google Scholar]