Abstract
BACKGROUND
The polymorphisms of cytochrome P450 2C19 (CYP2C19) gene are major prognostic factors for the response to clopidogrel therapy in patients with coronary artery diseases (CAD). The CYP2C19*2 is the most important allele responsible for resistance to clopidogrel therapy. This study examined CYP2C19 gene polymorphism (CYP2C19*1 and *2) in Iranian patients.
METHODS
This cross-sectional study was performed on 43 Iranian patients with CAD who underwent percutaneous coronary intervention (PCI) and received drug-eluted stents (DES). CYP2C19 polymorphisms were assessed using real time PCR and frequency of CYP2C19*1 and CYP2C19*2 were determined, and then homo- or heterozygous state of genes was detected by Melt Curve Analysis method.
RESULTS
Forty three patients (mean age = 58.8 ± 10.0 years, 79.1% male) participated in this study. CYP2C19*1/CYP2C19*1 genotype was observed in 31 (72.1%) of participates, CYP2C19*1/CYP2C19*2 genotype in 10 (23.3%), and CYP2C19*2/CYP2C19*2 genotype in 2 patients (4.7%). The frequency of CYP2C19*2 allele in the sample was 27.9%.
CONCLUSION
This study demonstrated a high prevalence of CYP2C19*2 gene polymorphism in Iranian patients. Further studies with larger samples or longitudinal are required to determine the effects of this polymorphism on the prognosis of CAD patients in our population.
Keywords: CYP2C19, Polymorphism, Clopidogrel, Coronary Artery Disease, Iran
Introduction
Despite considerable improvements in preventive programs and increasing access to specialized medical care, atherosclerosis and its subsequent complications, such as ischemic heart diseases, have remained the leading causes of mortality all over the world, especially in developing countries.1,2 In Iran, coronary artery disease (CAD) is still the most important cause of mortality, with nearly 40% of all deaths, and also the most important cause of morbidity.3,4 Reperfusion of the coronary arteries by surgical or medical interventions is the first-line treatment in ischemic heart disease, which significantly reduce the mortality and morbidity in patients with CAD. The treatment methods are the administration of fibrinolytic drugs or surgical intervention including coronary artery bypass surgery (CABG) and percutaneous coronary intervention (PCI). Indeed, PCI is the treatment of choice for acute myocardial infarction (MI), if it is done on time.5,6
Currently, coronary artery stents, particularly drug-eluting stents (DES), are used in the majority of patients who undergo PCI, which results in a significant decrease in the rate of thrombosis and restenosis in coronary arteries. It can reduce acute closure of the artery from 2 to 10 percent to less than 1 percent and restenosis from 30 to 40 percent to less than 10 percent.7–9 However, stent thrombosis is a rare but serious complication that can occur in either acute (in 24 hours), subacute (in 30 days) or late (in one year) after stent placement. Many studies have been conducted on the prevention of stent thrombosis with antiplatelet therapy. The American Society of Cardiology (ASC) guideline has recommended the administration of clopidogrel, in combination with aspirin, in patients using bare metal stents (BMS) for at least one month (and up to 12 months in recent studies10 and in patients using DES stents for at least 12 months.11
Clopidogrel is a pro-drug agent that, after becoming an active metabolite, selectively blocks ADP dependent platelet activation and aggregation. The drug requires the enzyme cytochrome P450 2C19 (CYP2C19) function for its activation and antiplatelet effects. In some patients (with different prevalence in different communities), clopidogrel has no antiplatelet effect or its effect is reduced. The responsiveness to clopidogrel is determined by genetic and acquired factors, and is one of the important factors in stent thrombosis and cardiac events after the stent placement in patients with CAD.12 Single nucleotide polymorphisms of CYP2C19 that reduce the activity of this enzyme are among the causes of racial differences in response to the antiplatelet effects of clopidogrel.12 The presence of CYP2C19*2 allele decreases the response to antiplatelet effects of clopidogrel.13 According to a meta-analysis, the risk of restenosis in the stent place in people who had at least one non-functional allele were 1.77 times more than those who were carrying two functional alleles.14 Furthermore, according to another meta-analysis, the major cardiovascular events in individuals carrying the allele CYP2C19*2 are 30% more than non-carriers. In addition, they had a higher risk for mortality (OR=1.79) and stent thrombosis (OR=3.45).15
According to recent review studies, initial individualize treatment based on the CYP2C19 genotype is controversial.13,14,16 However, considering the importance of prevention of complications of stent thrombosis, the study of CYP2C19 polymorphisms in each population can be suggestive for the prognosis of the response to the treatment and the provisions needed for patients undergoing PCI. Considering that there was no report determining the prevalence of CYP2C19 polymorphisms in patients undergoing PCI in the Iranian population, this study was conducted to determine the prevalence of this gene polymorphism for ethnically Iranian patients.
Materials and Methods
This cross-sectional study was performed on ethnically Iranian patients who were diagnosed with CAD and undergone coronary angioplasty and stenting (DES) in Shahid Chamran, Sepahan, and Sina hospitals in Isfahan (IRAN) in 2011. Considering the prevalence of clopidogrel resistance as 30% and the acceptable error of 0.14, 43 patients were randomly selected from the centers. The study was approved by the Medical University of Isfahan Ethics Committee and written informed consent was obtained from all participants. To determine the genotype of the patient's blood sample was taken, and Genomic DNA extracted from 200 micro liter of blood using the High Pure PCR Template Preparation Kit. The CYP2C19*2 and CYP2C19*1 genotypes were proliferated with specific PCR kits using Real-Time PCR Corbett Research 6600 in the laboratory. Melt Curve Analysis method was used for distinguishing the homozygous and heterozygous types of the genes. The data were analyzed by the SPSS version 16.0.
Results
In this study, 43 patients (mean age=10.0±58.4 years; 82% male) participated. The frequency of risk factors for heart disease was as fallowed; hypertension=18 patients (47.3%), diabetes=13 patients (34.2%), dyslipidemia=14 patients (36.8%), and smoking=9 patients (23.6%).
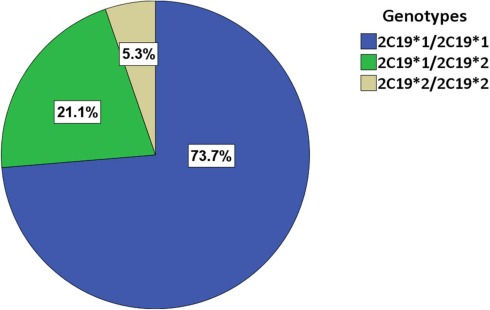
The prevalence of genotypes was as fallowed: CYP2C19*1/CYP2C19*1=31 patients (72.1%), CYP2C19*1/CYP2C19*2=10 patients (23.3%), and CYP2C19*2/CYP2C19*2=2 patients (4.7%) (Figure 1). So the relative frequency of CYP2C19*2 allele in the study sample was 27.9%.
Figure 1.
CYP2C19 genotypes in Iranian patients with CAD
Discussion
Polymorphisms of CYP2C19 and CYP2C19*2 allele are major determinants of prognosis after MI in patients treated with clopidogrel. According to studies, the incidence of CYP2C19*2 allele in East Asian societies is more than Western societies. For example, in a study conducted in Korea on 2,146 patients receiving DES, 47% had at least one CYP2C19*2 allele. Patients were followed for 12 months and results showed that deaths due to heart failure, MI, and stent thrombosis, were significantly higher in patients who were the carriers of CYP2C19*2 allele compared with non-carriers (2.0% vs. 0.8%).17 According to a study conducted in Lebanon, in healthy population, the relative frequency of alleles CYP2C19*2 and CYP2C19*3 were respectively 13% and 3%.18 In our study, the overall relative frequency of CYP2C19*2 alleles was 26.3% and the relative frequency of homozygous was 5.3% for this allele. In one study conducted in Tehran (Iran) by Zendehdel et al, on patients with gastroesophageal reflux disease under treatment with omeprazole, frequency of CYP2C19*2 alleles was 13.4% and the relative frequency of homozygous was 1.3% for this allele.19 In another study conducted on general healthy population of Tehran Zand et al reported the frequency of CYP2C19*2 allele as 25% and the relative frequency of homozygous as 3%.20 The difference among these studies could be due to difference in the studied populations as in our study and the study by Zand et al, the sample was from specific patients while in the other study sampling was done from the general population.20
Considering that the presence of non-functional CYP2C19 polymorphism determines the prognosis of response to the treatment with clopidogrel, some researchers recommended that treatment choice should be based on patient's genotype. However, according to the new review studies, the recommendation of treatment initially based on the CYP2C19 genotype is controversial.13,14,16 It is important to know that most of these studies have been done on western populations and the results of similar studies in Asian populations might be different. This issue is more important when other determining factors of response to treatment with clopidogrel such as drug interactions would be considered. While patients on clopidogrel-aspirin dual antiplatelet therapy usually require treatment with proton pump inhibitors (PPI), statins, and other medications, the drugs are to reduce the activity of CYP2C19. Thus, in the patients with reduced activity of the enzyme CYP2C19, because of being the carriers of CYP2C19*2 allele, selecting a drug with less interaction with this enzyme become more important.21 According to a large cohort study in French on 2744 patients who were using clopidogrel and PPI at the same time after MI, the results showed that the co-administration of clopidogrel and PPI did not increase the risk of cardiovascular events or mortality and the results did not change with regard to the type of PPI and CYP2C19 genotypes, though the results of this cohort study showed that the increased risk in patients carrying the two non-functional alleles cannot be ruled out.22 However, due to the higher prevalence of non-functional CYP2C19 alleles in East Asian populations, drug interactions in these communities may have a different effect. As the results of a large study in Taiwan showed, simultaneous use of clopidogrel and PPI is associated with increased mortality (hazard ratio=1.65).23
There are some studies on some strategies such as using higher doses of clopidogrel, adding or alternating the therapy with other antiplatelet drugs (e.g. ticagrelor and cilostazol),24 and using CYP2C19 enzyme inducers (e.g. St. John's wort)25 in patients with non-functional alleles of CYP2C19. According to Cuisset et al study, increasing the doses of clopidogrel in patients undergoing PCI, who had not responded appropriately to the drug was effective in those who had no CYP2C19*2 allele.26 In the study of Park et al, cilostazol was added to clopidogrel-aspirin regimen and significantly reduced platelet activity in patients carrying the non-functional allele.27 However, no single strategy for carrier patients is yet recommended. Also, in selecting a cost-benefit treatment strategy, the prevalence of non-functional alleles in each population should be considered.
The results of this study on an Iranian population with CAD who underwent PCI and received DES showed that the overall relative frequency of CYP2C19*2 alleles is high. These results, mostly follows other studies in Asian populations and shows the higher prevalence of alleles responsible for clopidogrel resistance in our population than western populations. Further cohort studies with larger sampling and on different races are required to determine the effects of this polymorphism on the prognosis of CAD patients in our population.
Limitations
There are some limitations to our study. The prevalence of other non-functional CYP2C19 alleles were not studied, though the CYP2C19*2 is the most important allele responsible for resistance to clopidogrel therapy. Also, the response to clopidogrel treatment and the final outcome was reported in this study, which is now undergoing by following-up the patients for one year.
Acknowledgments
This study was conducted with financial support of Isfahan University of Medical Sciences.
Conflict of Interests
Authors have no conflict of interests.
References
- 1.Bolognese L. Changing patterns of ST elevation myocardial infarction epidemiology. Am Heart J. 2010;160(6 Suppl):S1–3. doi: 10.1016/j.ahj.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 2.Abdallah M, Karrowni W, Shamseddeen W, Itani S, Kobeissi L, Ghazzal Z, et al. Acute coronary syndromes: clinical characteristics, management, and outcomes at the American University of Beirut Medical Center, 2002-2005. Clin Cardiol. 2010;33(1):E6–E13. doi: 10.1002/clc.20636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Donyavi T, Naieni KH, Nedjat S, Vahdaninia M, Najafi M, Montazeri A. Socioeconomic status and mortality after acute myocardial infarction: a study from Iran. Int J Equity Health. 2011;10(1):9. doi: 10.1186/1475-9276-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hatmi ZN, Tahvildari S, Gafarzadeh Motlag A, Sabouri Kashani A. Prevalence of coronary artery disease risk factors in Iran: a population based survey. BMC Cardiovasc Disord. 2007;7:32. doi: 10.1186/1471-2261-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Terkelsen CJ, Sorensen JT, Maeng M, Jensen LO, TH , Trautner S, et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304(7):763–71. doi: 10.1001/jama.2010.1139. [DOI] [PubMed] [Google Scholar]
- 6.Lambert L, Brown K, Segal E, Brophy J, Rodes-Cabau J, Bogaty P. Association between timeliness of reperfusion therapy and clinical outcomes in ST-elevation myocardial infarction. JAMA. 2010;303(21):2148–55. doi: 10.1001/jama.2010.712. [DOI] [PubMed] [Google Scholar]
- 7.Fischman DL, Leon MB, Baim DS, Schatz RA, Savage MP, Penn I, et al. A randomized comparison of coronary-stent placement and balloon angioplasty in the treatment of coronary artery disease. Stent Restenosis Study Investigators. N Engl J Med. 1994;331(8):496–501. doi: 10.1056/NEJM199408253310802. [DOI] [PubMed] [Google Scholar]
- 8.Serruys PW, De Jaegere P, Kiemeneij F, Macaya C, Rutsch W, Heyndrickx G, et al. A comparison of balloon-expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. Benestent Study Group. N Engl J Med. 1994;331(8):489–95. doi: 10.1056/NEJM199408253310801. [DOI] [PubMed] [Google Scholar]
- 9.Sutton JM, Ellis SG, Roubin GS, Pinkerton CA, King SB, Raizner AE, et al. Major clinical events after coronary stenting. The multicenter registry of acute and elective Gianturco-Roubin stent placement. The Gianturco-Roubin Intracoronary Stent Investigator Group. Circulation. 1994;89(3):1126–37. doi: 10.1161/01.cir.89.3.1126. [DOI] [PubMed] [Google Scholar]
- 10.Cohen M. Antiplatelet therapy in percutaneous coronary intervention: a critical review of the 2007 AHA/ACC/SCAI guidelines and beyond. Catheter Cardiovasc Interv. 2009;74(4):579–97. doi: 10.1002/ccd.22021. [DOI] [PubMed] [Google Scholar]
- 11.American College of Cardiology, American Heart Association Task Force on Practice Guidelines. 2007 Focused update of the ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Catheter Cardiovasc Interv. 2008;71(1):E1–40. doi: 10.1002/ccd.21475. [DOI] [PubMed] [Google Scholar]
- 12.Ma TK, Lam YY, Tan VP, Yan BP. Variability in response to clopidogrel: how important are pharmacogenetics and drug interactions? Br J Clin Pharmacol. 2011 doi: 10.1111/j.1365-2125.2011.03949.x. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Price MJ, Tantry US, Gurbel PA. The influence of CYP2C19 polymorphisms on the pharmacokinetics, pharmacodynamics, and clinical effectiveness of P2Y (12) inhibitors. Rev Cardiovasc Med. 2011;12(1):1–12. doi: 10.3909/ricm0590. [DOI] [PubMed] [Google Scholar]
- 14.P2Y (12) inhibitors. Rev Cardiovasc Med. 2011;12(1):1–12. doi: 10.3909/ricm0590. [DOI] [PubMed] [Google Scholar]
- 15.Bauer T, Bouman HJ, Van Werkum JW, Ford NF, Ten Berg JM, Taubert D. Impact of CYP2C19 variant genotypes on clinical efficacy of antiplatelet treatment with clopidogrel: systematic review and meta-analysis. BMJ. 2011;343(d4588) doi: 10.1136/bmj.d4588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hulot JS, Collet JP, Silvain J, Pena A, Bellemain-Appaix A, Barthélémy O, et al. Cardiovascular risk in clopidogrel-treated patients according to cytochrome P450 2C19*2 loss-of-function allele or proton pump inhibitor coadministration: a systematic meta-analysis. J Am Coll Cardiol. 2010;56(2):134–43. doi: 10.1016/j.jacc.2009.12.071. [DOI] [PubMed] [Google Scholar]
- 17.Camilleri E, Jacquin L, Paganelli F, Bonello L. Personalized antiplatelet therapy: review of the latest clinical evidence. Curr Cardiol Rep. 2011;13(4):296–302. doi: 10.1007/s11886-011-0194-1. [DOI] [PubMed] [Google Scholar]
- 18.Oh IY, Park KW, Kang SH, Park JJ, Na SH, Kang HJ, et al. Association of cytochrome P450 2C19*2 polymorphism with clopidogrel response variability and cardiovascular events in Koreans treated with drug-eluting stents. Heart. 2011 doi: 10.1136/hrt.2011.227272. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 19.Djaffar Jureidini I, Chamseddine N, Keleshian S, Naoufal R, Zahed L, Hakime N. Prevalence of CYP2C19 polymorphisms in the Lebanese population. Mol Biol Rep. 2011 doi: 10.1007/s11033-011-0700-y. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 20.Zendehdel N, Biramijamal F, Hossein-Nezhad A, Zendehdel N, Sarie H, Doughaiemoghaddam M, et al. Role of cytochrome P450 2C19 genetic polymorphisms in the therapeutic efficacy of omeprazole in Iranian patients with erosive reflux esophagitis. Arch Iran Med. 2010;13(5):406–12. [PubMed] [Google Scholar]
- 21.Zand N, Tajik N, Moghaddam AS, Milanian I. Genetic polymorphisms of cytochrome P450 enzymes 2C9 and 2C19 in a healthy Iranian population. Clin Exp Pharmacol Physiol. 2007;34(1-2):102–5. doi: 10.1111/j.1440-1681.2007.04538.x. [DOI] [PubMed] [Google Scholar]
- 22.Bates ER, Lau WC, Angiolillo DJ. Clopidogrel-drug interactions. J Am Coll Cardiol. 2011;57(11):1251–63. doi: 10.1016/j.jacc.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 23.Simon T, Steg PG, Gilard M, Blanchard D, Bonello L, Hanssen M, et al. Clinical events as a function of proton pump inhibitor use, clopidogrel use, and cytochrome P450 2C19 genotype in a large nationwide cohort of acute myocardial infarction: results from the French Registry of Acute ST-Elevation and Non-ST-Elevation Myocardial Infarction (FAST-MI) registry. Circulation. 2011;123(5):474–82. doi: 10.1161/CIRCULATIONAHA.110.965640. [DOI] [PubMed] [Google Scholar]
- 24.Huang CC, Chen YC, Leu HB, Chen TJ, Lin SJ, Chan WL, et al. Risk of adverse outcomes in Taiwan associated with concomitant use of clopidogrel and proton pump inhibitors in patients who received percutaneous coronary intervention. Am J Cardiol. 2010;105(12):1705–9. doi: 10.1016/j.amjcard.2010.01.348. [DOI] [PubMed] [Google Scholar]
- 25.Tantry US, Bliden KP, Wei C, Storey RF, Armstrong M, Butler K, et al. First analysis of the relation between CYP2C19 genotype and pharmacodynamics in patients treated with ticagrelor versus clopidogrel: the ONSET/OFFSET and RESPOND genotype studies. Circ Cardiovasc Genet. 2010;3(6):556–66. doi: 10.1161/CIRCGENETICS.110.958561. [DOI] [PubMed] [Google Scholar]
- 26.Lau WC, Welch TD, Shields T, Rubenfire M, Tantry US, Gurbel PA. The effect of St John's Wort on the pharmacodynamic response of clopidogrel in hyporesponsive volunteers and patients: increased platelet inhibition by enhancement of CYP3A4 metabolic activity. J Cardiovasc Pharmacol. 2011;57(1):86–93. doi: 10.1097/FJC.0b013e3181ffe8d0. [DOI] [PubMed] [Google Scholar]
- 27.Cuisset T, Quilici J, Cohen W, Fourcade L, Saut N, Pankert M, et al. Usefulness of High Clopidogrel Maintenance Dose According to CYP2C19 Genotypes in Clopidogrel Low Responders Undergoing Coronary Stenting for Non ST Elevation Acute Coronary Syndrome. Am J Cardiol. 2011 doi: 10.1016/j.amjcard.2011.05.045. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 28.Park KW, Park JJ, Lee SP, Oh IY, Suh JW, Yang HM, et al. Cilostazol attenuates on-treatment platelet reactivity in patients with CYP2C19 loss of function alleles receiving dual antiplatelet therapy: a genetic substudy of the CILON-T randomised controlled trial. Heart. 2011;89(7):641–7. doi: 10.1136/hrt.2010.216499. [DOI] [PubMed] [Google Scholar]