Abstract
Objective
To explore whether frequency and duration of sick-leave certification for acute airway infections differ between general practitioners (GPs) in Poland and Norway.
Design
Cross-sectional survey.
Setting
Educational courses for GPs.
Intervention
We used a questionnaire with four vignettes presenting patients with symptoms consistent with pneumonia, sinusitis, common cold, and exacerbation of chronic obstructive pulmonary disease (COPD), respectively. For each vignette GPs were asked whether they would offer a sick-leave note, and if so, for how many days.
Subjects
Convenience samples of GPs in Poland (n = 216) and Norway (n = 171).
Main outcome measures
Proportion of GPs offering a sick-leave certificate. Duration of sick-leave certification.
Results
In Poland 100%, 95%, 87%, and 94% of GPs would offer sick leave for pneumonia, sinusitis, common cold, and exacerbation of COPD, respectively. Corresponding figures in Norway were 97%, 83%, 60%, and 90%. Regression analysis adjusting for the GPs' sex, speciality, experience, and workload indicated that relative risks for offering sick leave (Poland versus Norway) were 1.16 (95% CI 1.07–1.26) for sinusitis and 1.50 (1.28–1.75) for common cold. Among GPs who offered sick leave for pneumonia, sinusitis, common cold, and exacerbation of COPD, mean duration was 8.9, 7.5, 5.1, and 6.9 days (Poland) versus 6.6, 4.3, 3.1, and 6.1 days (Norway), respectively. In regression analyses the differences between the Polish and Norwegian samples in duration of sick leave were statistically significant for all vignettes. A pattern of offering sick leave for three, five, seven, 10, or 14 days was observed in both countries.
Conclusion
In the Polish sample GPs were more likely to offer sick-leave notes for sinusitis and common cold. GPs in Poland offered sick leaves of longer duration for pneumonia, sinusitis, common colds, and exacerbation of COPD compared with GPs in the Norwegian sample.
Key Words: Family practice, general practice, respiratory tract infections, sick leave
Convenience samples of general practitioners (GPs) in Poland and Norway were presented with identical vignettes consistent with pneumonia, sinusitis, common cold, and exacerbation of chronic obstructive pulmonary disease, respectively.
Compared with Norwegian GPs, Polish GPs were more likely to offer sick-leave notes for sinusitis and common cold.
For all vignettes GPs in Poland offered sick leave notes of longer duration than GPs in Norway.
A characteristic and identical pattern of offering sick leave for three, five, seven, 10, or 14 days was observed in both countries.
Across Europe there is large variability in sickness certification rates [1]. Potential determinants of sick leave that have been explored empirically include patient-related factors such as age, sex, education [2], and self-reported health [3], and work-related factors such as physical working conditions, social support, job control and demand [4]. Furthermore, economic awards as well as general acceptance of sick leave in society may be important contributors to sickness absence [4]. Legislation pertaining to sick leave varies between European countries. In Norway workers have a right to self-certification for three or eight days of sick leave, depending on agreements between the employer and the National Social Insurance. Sick-listed persons are currently awarded full compensation from their employers for the first 16 days, and thereafter from the National Social Insurance. In Poland workers are obliged to present a sick-leave note from the physician from the first day of an absence. In most cases they receive 80% compensation from their employers for the first 30 days and from the National Social Insurance thereafter.
Although the impact of the physicians’ beliefs and attitudes towards sick listing relative to other determinants of sickness absence has not been clarified [4], government authorities and employers tend to emphasize that physicians should focus more on the patients’ work ability despite disease and illness. Consequently, guidelines for evaluation of work disability have emerged [5]. For example, Swedish guidelines recommend that sick leave for common cold and sinusitis should not exceed one week, whereas for pneumonia and exacerbation of chronic obstructive pulmonary disease (COPD) two weeks may be necessary (Table I) [6]. Disease-oriented guidelines have also been implemented in Germany and the Netherlands [5] and are currently being considered in Norway.
Table I.
Recommendations for sick leave by type of airway infection.1
| Disease | Duration of sick leave |
| Pneumonia | Usually up to two weeks |
| Sinusitis | Usually not beyond one week |
| Upper airway infection | Up to one week may be necessary |
| Exacerbation of COPD | Up to two weeks may be necessary |
Note: 1According to the Swedish National Board of Health and Welfare (6).
In a recent study it was observed that of all sick-leave notes issued for acute cough, 36.9% and 5.6% were issued for more than one week in Poland and Norway, respectively [7]. In the present study we wanted to explore further whether frequency and duration of sick-leave certification for acute airways infections differ between Polish and Norwegian GPs.
Material and methods
In 2009 GPs attending continual medical educational (CME) courses and national meetings were approached and asked to participate in our survey. Norwegian GPs were recruited among participants in five CME courses, three in May and two in September/October. The content of the courses was unrelated to our study, but courses were chosen to ensure young as well as experienced participants. In June Polish GPs were recruited at a national meeting in the city of Bialystok. We obtained responses from 216 Polish and 171 Norwegian GPs, respectively. Compared with the Norwegian study arm there were significantly more women and more specialists among the Polish respondents (Table II). On average the Polish respondents had worked five years longer as physicians, and they reported seeing four more patients per hour (Table II).
Table II.
Characteristics of respondents in Poland and Norway: means, percentages, and 95% confidence intervals.
| Variable | Poland | Norway | p-value |
| Mean age, years | 46 (45–47) | 44 (42–45) | 0.06 |
| Women,% | 66 (59–72) | 45 (38–52) | <0.001 |
| Specialist in general practice,% | 78 (73–84) | 52 (45–60) | <0.001 |
| Time worked in general practice, years | 12 (11–13) | 12 (10–14) | 0.65 |
| Time worked as a physician, years | 20 (18–21) | 15 (13–16) | <0.001 |
| Average number of patients seen per hour | 7.5 (6.7–8.3) | 3.5 (3.4–3.7) | <0.001 |
For our study we developed a questionnaire presenting four hypothetical patients, each with a different kind of acute airway infection. No specific diagnoses were mentioned, but the four case descriptions provided clues pertinent to pneumonia, sinusitis, common cold, and exacerbation of COPD, respectively (see Appendix). We used symptoms as well as clinical findings as diagnostic triggers. In Norway c-reactive protein (CRP) is often used in the diagnostic work-up of acute airway infections, whereas in Poland this is unusual. Consequently, blood tests were not included in our vignettes. The questionnaire was piloted for face validity among a few Norwegian colleagues, which resulted in minor adjustments. Translation and back-translation was undertaken to resolve ambiguities and to the extent possible ensure that Polish and Norwegian GPs were presented with identical vignettes. For each vignette we asked whether the GP would offer a sick-leave note, and if so, for how many days. For other study purposes (not reported here) the GPs were asked about prescription of antibiotics and whether they would recommend restrictions, such as bed rest, staying indoors, or avoidance of physical activities. Finally we included questions about age, sex, speciality, years of professional experience, and workload.
For each of the four vignettes we tested the hypothesis that Norwegian and Polish GPs would differ with respect to frequency and duration of sick-leave certification. Consequently, the proportion of GPs that would offer a sick-leave note and duration of sick leave were our main outcome measures. The GPs’ country of residence was the main independent variable, whereas age, sex, speciality, number of years worked as a physician, number of years worked as a GP, and average number of patients seen per hour were included as secondary independent variables. These secondary variables were included as possible confounders of potential associations between country of residence and frequency and duration of sick listing, respectively.
Descriptive statistics (means, proportions) for duration and frequency of sick-leave notes, respectively, were calculated. We used log-Poisson regression with robust standard errors to calculate relative risks for offering a sick-leave note between the Polish and Norwegian samples. Ordinary least-squares regression was used to evaluate differences in mean duration of sick leave. We used robust variance estimates to account for non-normality of data. Bivariate and multivariate analyses were performed, but since the results were similar only the multivariate analyses are shown. The study was powered to detect a oneday difference in mean duration of sick leave assuming a standard deviation of 2.5 days. With 80% power and significance level 0.05 we would need at least 100 participants in each group. Since we did not expect all GPs to offer sick leave, we aimed for about 200 participants from each country. SPSS version 17.0 (SPSS, Chicago, Illinois) and STATA version 9.2 (Stata Corp., College Station, Texas) were used for data analysis; p-values < 0.05 were regarded as statistically significant.
Results
The proportion of GPs that would offer a sick leave note varied by disease scenario, i.e. 98%, 92%, 89%, and 75% for pneumonia, COPD exacerbation, sinusitis, and common cold, respectively. The crude proportions offering a sick-leave note were higher among Polish GPs for all scenarios, but confidence intervals overlapped for pneumonia and COPD (Table III). After adjustment for possible confounders, statistically significant differences in sickness certification frequency between the Polish and Norwegian samples of GPs remained for sinusitis and common cold (Table III). Among the GPs that would offer sick leave, the mean duration varied by disease scenario in a similar pattern, i.e. from eight days for pneumonia to about 4.5 days for common cold. In all vignettes the Polish GPs tended to sick list the patient for a longer time than the Norwegian GPs. However, a duration of seven days was most frequent in both countries for pneumonia, 36% in Poland and 45% in Norway. Corresponding figures for COPD exacerbations were 38% and 41%, respectively.
Table III.
Proportion of general practitioners in Poland and Norway that would offer a sick leave note for respiratory tract diseases.
| Disease | Poland (n = 216) %, 95% CI | Norway (n = 171) %, 95% CI | Adjusted relative risks1 95% CI |
| Female, age 30 Pneumonia | 99.5 (98.6–100) | 97.1 (94.5–99.6) | 1.02 (0.99–1.04) |
| Male, age 50 Sinusitis | 94.9 (92.0–97.9) | 82.5 (76.7–88.2) | 1.16 (1.07–1.26) |
| Female, age 45 Common cold | 86.6 (82.0–91.1) | 60.2 (52.9–67.7) | 1.50 (1.28–1.75) |
| Male, age 55 Exacerbation of COPD | 93.5 (90.2–96.8) | 89.5 (84.8–94.1) | 1.05 (0.98–1.13) |
Note: 1Relative risk for offering a sick-leave note in Poland versus Norway, adjusted for sex, speciality, number of years worked as a physician, and average number of patients seen per hour, using multivariate log-Poisson regression with robust standard errors.
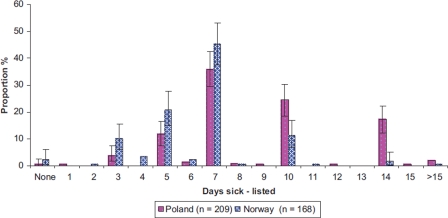
The adjusted difference in mean duration between Polish and Norwegian GPs varied from less than one day for COPD exacerbation to three days for sinusitis, and the difference was statistically significant for all scenarios (Table IV). For each vignette there was considerable variability in duration of sick listing, but very few outliers beyond 14 days in the Polish as well as in the Norwegian sample (see Figure 1 for an example). The proposed duration of sick leave for pneumonia showed a characteristic 3, five, seven, 10 or 14 days pattern (Figure 1). For the other vignettes the pattern was similar.
Table IV.
General practitioners' proposed duration of sick leave for respiratory tract diseases in Poland and Norway.
| Disease | Poland, days, 95% CI | Norway, days, 95% CI | Adjusted difference1, days 95% CI |
| Female, age 30 Pneumonia | 8.9 (8.4–9.4) | 6.6 (6.2–7.0) | 2.2 (1.4–3.0) |
| Male, age 50 Sinusitis | 7.5 (7.1–7.9) | 4.3 (4.0–4.6) | 3.0 (2.4–3.5) |
| Female, age 45 Common cold | 5.1 (4.9–5.4) | 3.1 (2.9–3.4) | 2.0 (1.5–2.5) |
| Male, age 55 Exacerbation of COPD | 6.9 (6.5–7.3) | 6.2 (5.8–6.5) | 0.7 (0.1–1.3) |
Note: 1Difference in proposed duration of sick leave adjusted for sex, speciality, number of years worked as a physician, and average number of patients seen per hour, using ordinary least-squares regression with robust variances to account for non-normal distributions.
Figure 1.
General practitioners' proposed duration of sick leave for a 30-year-old female with pneumonia in Poland and Norway. 95% CI bars are shown for the most frequent durations.
Discussion
We observed that when presented with clinical case descriptions of acute airway infections, the Polish GPs were more likely to offer a sick-leave note for sinusitis and common cold, and the mean duration of sick listing was longer for all airway infections under study compared with the Norwegian GPs. Furthermore, there was considerable within-country variation in the proposed duration of sick-leave certification. A characteristic and identical pattern of offering sick leave for three, five, seven, 10, or 14 days was observed in both countries.
Sick-leave certification is a complex phenomenon in which patients, physicians, workplace [8], and society as a whole play significant roles. When this phenomenon is approached scientifically, practice variation is a prominent finding. A recent review found considerable variability in sickness certification rates across European countries [1], whereas others have found large variation in how long physicians would sick list similar patients for [9]. Practice variation by physician characteristics such as age, gender, speciality, length of professional experience, and part-time versus full-time work has been studied [10–12], often with conflicting results. Typically, data have been collected using questionnaires, and, as in our study, case vignettes [9]. Other studies using vignette techniques suggest that sick-listing practices may vary by type of clinical problem (physical versus psychological [13], pregnancy with and without risk factors [14]), how the patient presented his/her problem [12], and the form used for work assessment [15]. Physicians may experience difficulty with issuing sick-leave notes [16–19], especially for long-term sickness absence [20]. Assessing functional ability [21] and work capacity, handling conflicts [17,18,22], and, notably, determining the optimal degree and duration of sickness absence are some of the issues physicians may find difficult [23].
Our finding of between-country differences is consistent with the hypothesis that societal and cultural factors such as legislation, working conditions, and patient expectations may contribute to variation in sick-listing practice. In many European countries GPs are expected to act in their patients’ best interest, but also as gatekeepers for access to specialized health care and welfare benefits [4,24–27]. One might hypothesize that Polish and Norwegian GPs balance these opposing interests differently, perhaps due to different expectations from the professional society, government authorities, or employers. Prior to and during the study period measures to reduce sickness absence were heavily debated in Norway, which may have influenced the Norwegian GPs in their answers to the questionnaire. Notably, only a small minority of GPs in either country would offer sick leave notes beyond two weeks for pneumonia and COPD exacerbation, or beyond one week for sinusitis and common cold. This is in accordance with current disease-oriented guidelines for sick listing (see Table I).
Another crucial issue is whether the between-country differences in sick-leave certification could be attributed to differences in self-certifying rights. Neither the vignettes nor the questions to the GPs included any reference to such rights. Since these exist in Norway, it is conceivable that Norwegian GPs took them into account when considering sick-leave certification. That many Norwegian GPs said no to sick-leave certification for common cold is consistent with this hypothesis.
Furthermore, it is conceivable that Polish and Norwegian GPs had different perceptions of patient needs or expectations. A previous study suggests that patients may have prominent influence on the GPs’ sick-listing practice [28]. In our vignettes information concerning working conditions was sparse, and it is conceivable that the GPs used their general experience to determine patient needs when responding to the questionnaire.
The very much identical pattern of issuing sick notes for three, five, seven, 10 or 14 days in the Polish and Norwegian samples is intriguing. There was nothing in the vignettes to suggest that these durations of inability to work were more likely than others. The observed pattern could be attributed to digit preferences, i.e. a human inclination to prefer some digits over others. Findings consistent with this phenomenon have been observed in studies of blood pressure measurements [29] as well as in studies of pure guessing [30,31]. Whether national guidelines will erase or enforce such patterns for short-term sickness absence has not yet been established. Introduction of more generous self-certification schemes, however, has been associated with shortening of sickness absence spells [32,33].
To our knowledge, no previous study has explored sick-listing decisions for different acute airway infections. The vignette technique ensured that all GPs responded to the same clinical information. Thereby our study is among the first to compare sickness certification decisions among GPs in different countries using standardized measurements. However, we realize that our study has several limitations. First, we used convenience samples of Polish and Norwegian GPs. Therefore our results may not be representative of Polish and Norwegian GPs in general. Furthermore, although the observed between-country differences were adjusted for several physician characteristics, the possibility of unmeasured confounders remains. Whether decisions on hypothetical case scenarios are representative of real-life decisions is a longstanding concern pertaining to the vignette technique [34], but empirical evidence in support of its validity exists. Using the standardized patient technique as a gold standard, clinical vignettes measured physician performance about equally well across different types of diseases and case complexities, and measures based on vignettes compared favourably with those based on patient chart abstracts [35]. Based on a literature review, Veloski et al. concluded that vignettes compare favourably with analysis of claims data sets in studying physicians’ decision-making while controlling for case mix [36].
Given the findings and the limitations of the present study, several suggestions for further research come to mind. First, studies to validate the vignette technique against other methods in the domain of sick-listing practices might be worthwhile. Second, exploring whether the duration of short-term sick-leave notes in actual clinical practice is influenced by digit preferences would be interesting. Third, further studies of cultural and societal determinants of sick-leave practices are needed to deepen our understanding. Determinants with potential to change through interventions, such as physicians’ workload or legislation, should perhaps have priority.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Appendix: Four case scenarios presented to Norwegian and Polish GPs
Female patient. 30 years old. No history of previous diseases. No regular use of prescribed drugs. She has been smoking for 15 years, and is now smoking 15 cigarettes per day. Works full time in a grocery store. Married, two children aged 3 and 5 who go to kindergarten. She comes to the doctor's office on Monday morning after 3 days of having a temperature up to 39.7 degrees C, shaking chills, night sweats, and cough with green sputum. On examination basal inspiratory crackles are heard over the left lung and also a dull percussion sound in the same area. There is no heart murmur and the heart rate is 95. No enlarged lymph nodes can be found on examination of the neck and the tonsils are neither enlarged nor inflamed. She has a temperature of 39 degrees C.
Male patient. 50 years old. No history of previous diseases. No regular use of prescribed drugs. He has been smoking for approximately 30 years, and is now smoking 10 cigarettes per day. Works full time as a carpenter. He is not married and has no children. He has had the common cold for a week. Two days ago he also developed a temperature up to 38.5 degrees C, experienced pain over both maxillary sinuses, which worsened when bending forwards, and he had purulent and smelly secretion from his nose. On examination there is pain on percussion over both his maxillary sinuses. The mucous membranes of his nose are red and irritated, and there is some purulent secretion. In his throat there are red and irritated mucous membranes, but no enlarged tonsils. On his neck there are several lightly enlarged and somewhat tender lymph nodes. Otoscopy as well as auscultation of the heart and the lungs are normal. Temperature 38.5 degrees C.
Female patient. 45 years old. She has no history of previous diseases. No regular use of prescribed drugs. She is a non-smoker. She works part time (80%) as a nurse at a nursing home. Married. One child aged 16 years. For the last four days she has experienced an annoying non-productive cough which disrupts her sleep and she has a constant running nose. The temperature has not been raised. Her throat is sore. She does not feel comfortable about going to work in this condition. On examination there is normal otoscopy, and no pain on percussion of her sinuses. There are red mucous membranes in her throat, but no enlarged tonsils, and no enlarges lymph nodes on her neck. Normal lung sounds. Temperature 37.4 degrees C.
Male patient, 55 years old. He has COPD, and is treated with inhaled ipratropium bromide and salbutamol on demand. No regular use of other prescribed drugs, and no other known diseases. He used to smoke 20 cigarettes a day for 30 years, but quit 2 years ago. He works full time as a bus driver. He lives with his girlfriend. No children are living at home any more. For the last four days he has suffered from the common cold, but now he consults you because of dyspnoea both on exertion and at rest, and he has a non-productive cough. Cardiac and respiratory pain is absent. When you examine him you find expiratory wheezes, no crackling sounds, and no dullness on percussion, but there is a hyper-resonant percussion sound over both lungs. There is no heart murmur, his pulse is 85 and regular. Neck/throat is normal. Temperature 38 degrees C.
References
- 1.Wynne-Jones G, Mallen CD, Welsh V, Dunn KM. Rates of sickness certification in European primary care: A systematic review. Eur J Gen Pract. 2009:1–10. doi: 10.1080/13814780802687521. [DOI] [PubMed] [Google Scholar]
- 2.Dekkers-Sanchez PM, Hoving JL, Sluiter JK, Frings-Dresen MH. Factors associated with long-term sick leave in sick-listed employees: a systematic review. Occup Environ Med. 2008;65:153–7. doi: 10.1136/oem.2007.034983. [DOI] [PubMed] [Google Scholar]
- 3.Eriksson HG, von Celsing AS, Wahlstrom R, Janson L, Zander V, Wallman T. Sickness absence and self-reported health a population-based study of 43,600 individuals in central Sweden. BMC Public Health. 2008;8:426. doi: 10.1186/1471-2458-8-426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Werner EL, Cote P. Low back pain and determinants of sickness absence. Eur J Gen Pract. 2009;15:74–9. doi: 10.1080/13814780903051866. [DOI] [PubMed] [Google Scholar]
- 5.De Boer WE, Bruinvels DJ, Rijkenberg AM, Donceel P, Anema JR. Evidence-based guidelines in the evaluation of work disability: An international survey and a comparison of quality of development. BMC.Public Health. 2009;9:349. doi: 10.1186/1471-2458-9-349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. http://www.socialstyrelsen.se/riktlinjer/forsakringsmedicin sktbeslutsstod. (accessed March 14, 2010)
- 7.Godycki-Cwirko M, Nocun M, Butler C, Muras M, Fleten N, Melbye H. Sickness certification for patients with acute cough/LRTI in primary care in Poland and Norway. Scand J Prim Health Care. 2010 doi: 10.3109/02813432.2010.544898. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Norrmen G, Svardsudd K, Andersson DK. The association of patient's family, leisure time, and work situation with sickness certification in primary care in Sweden. Scand J Prim Health Care. 2010;28:76–81. doi: 10.3109/02813431003765265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soderberg E, Alexanderson K. Sickness certification practices of physicians: A review of the literature. Scand J Public Health. 2003;31:460–74. doi: 10.1080/14034940310005367. [DOI] [PubMed] [Google Scholar]
- 10.Bollag U, Rajeswaran A, Ruffieux C, Burnand B. Sickness certification in primary care: The physician's role. Swiss Med Wkly. 2007;137:341–6. doi: 10.4414/smw.2007.11865. [DOI] [PubMed] [Google Scholar]
- 11.Norrmen G, Svardsudd K, Andersson D. Impact of physician-related factors on sickness certification in primary health care. Scand J Prim Health Care. 2006;24:104–9. doi: 10.1080/02813430500525433. [DOI] [PubMed] [Google Scholar]
- 12.Englund L, Tibblin G, Svardsudd K. Variations in sick-listing practice among male and female physicians of different specialities based on case vignettes. Scand J Prim Health Care. 2000;18:48–52. doi: 10.1080/02813430050202569. [DOI] [PubMed] [Google Scholar]
- 13.Campbell A, Ogden J. Why do doctors issue sick notes? An experimental questionnaire study in primary care. Fam Pract. 2006;23:125–30. doi: 10.1093/fampra/cmi099. [DOI] [PubMed] [Google Scholar]
- 14.Frazier LM, Ho HL, Molgaard CA. Variability in physician management of employment during pregnancy. Women Health. 2001;34:51–63. doi: 10.1300/J013v34n04_04. [DOI] [PubMed] [Google Scholar]
- 15.Sallis A, Birkin R, Munir F. Working towards a “fit note”: An experimental vignette survey of GPs. Br J Gen Pract. 2010;60:245–50. doi: 10.3399/bjgp10X483896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Engblom M, Alexanderson K, Englund L, Norrmen G, Rudebeck CE. When physicians get stuck in sick-listing consultations: A qualitative study of categories of sick-listing dilemmas. Work. 2010;35:137–42. doi: 10.3233/WOR-2010-0965. [DOI] [PubMed] [Google Scholar]
- 17.Arrelov B, Alexanderson K, Hagberg J, Lofgren A, Nilsson G, Ponzer S. Dealing with sickness certification: A survey of problems and strategies among general practitioners and orthopaedic surgeons. BMC Public Health. 2007;7:273. doi: 10.1186/1471-2458-7-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lofgren A, Hagberg J, Arrelov B, Ponzer S, Alexanderson K. Frequency and nature of problems associated with sickness certification tasks: A cross-sectional questionnaire study of 5455 physicians. Scand J Prim Health Care. 2007;25:178–85. doi: 10.1080/02813430701430854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gulbrandsen P, Hofoss D, Nylenna M, Saltyte-Benth J, Aasland OG. General practitioners’ relationship to sickness certification. Scand J Prim Health Care. 2007;25:20–6. doi: 10.1080/02813430600879680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Engblom M, Alexanderson K, Rudebeck CE. Characteristics of sick-listing cases that physicians consider problematic: Analyses of written case reports. Scand J Prim Health Care. 2009;27:250–5. doi: 10.3109/02813430903286286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krohne K, Brage S. New rules meet established sickness certification practice: A focus-group study on the introduction of functional assessments in Norwegian primary care. Scand J Prim Health Care. 2007;25:172–7. doi: 10.1080/02813430701267421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wynne-Jones G, Mallen CD, Main CJ, Dunn KM. What do GPs feel about sickness certification? A systematic search and narrative review. Scand J Prim Health Care. 2010;28:67–75. doi: 10.3109/02813431003696189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lofgren A, Hagberg J, Alexanderson K. What physicians want to learn about sickness certification: Analyses of questionnaire data from 4019 physicians. BMC Public Health. 2010;10:61. doi: 10.1186/1471-2458-10-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Swartling M, Peterson S, Wahlstrom R. Views on sick-listing practice among Swedish General Practitioners: A phenomenographic study. BMC Fam Pract. 2007;8:44. doi: 10.1186/1471-2296-8-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carlsen B, Norheim OF. Introduction of the patient-list system in general practice: Changes in Norwegian physicians’ perception of their gatekeeper role. Scand J Prim Health Care. 2003;21:209–13. doi: 10.1080/02813430310004155. [DOI] [PubMed] [Google Scholar]
- 26.Delnoij D, Van MG, Paulus A, Groenewegen P. Does general practitioner gatekeeping curb health care expenditure? J Health Serv Res Policy. 2000;5:22–6. doi: 10.1177/135581960000500107. [DOI] [PubMed] [Google Scholar]
- 27.Bohlert I, Adam I, Robra BP. [The Swiss gatekeeper system: A model for improving capacity development and economic effectiveness] Gesundheitswesen. 1997;59:488–94. [PubMed] [Google Scholar]
- 28.Englund L, Svardsudd K. Sick-listing habits among general practitioners in a Swedish county. Scand J Prim Health Care. 2000;18:81–6. doi: 10.1080/028134300750018954. [DOI] [PubMed] [Google Scholar]
- 29.Burnier M, Gasser UE. End-digit preference in general practice: A comparison of the conventional auscultatory and electronic oscillometric methods. Blood Press. 2008;17:104–9. doi: 10.1080/08037050801972881. [DOI] [PubMed] [Google Scholar]
- 30.Hill TP. Random-number guessing and the 1st digit phenomenon. Psychol Rep. 1988;62:967–71. [Google Scholar]
- 31.Sanford EC. On the guessing of numbers. Am J Psychol. 1903;14:647–65. [Google Scholar]
- 32.Taylor PJ. Self-certification for brief spells of sickness absence. BMJ. 1969;1:144–7. doi: 10.1136/bmj.1.5637.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fleten N, Krane L, Johnsen R. Extended self-certification: A step towards more appropriate sickness absence? Nor J Epidemiol. 2009;19:223–8. [Google Scholar]
- 34.Jones TV, Gerrity MS, Earp J. Written case simulations: Do they predict physicians’ behavior? J Clin Epidemiol. 1990;43:805–15. doi: 10.1016/0895-4356(90)90241-g. [DOI] [PubMed] [Google Scholar]
- 35.Peabody JW, Luck J, Glassman P, Jain S, Hansen J, Spell M, et al. Measuring the quality of physician practice by using clinical vignettes: A prospective validation study. Ann Intern Med. 2004;141:771–80. doi: 10.7326/0003-4819-141-10-200411160-00008. [DOI] [PubMed] [Google Scholar]
- 36.Veloski J, Tai S, Evans AS, Nash DB. Clinical vignette-based surveys: A tool for assessing physician practice variation. Am J Med Qual. 2005;20:151–7. doi: 10.1177/1062860605274520. [DOI] [PubMed] [Google Scholar]