Abstract
Objective
To explore the influence of sociodemographic factors on access to appointments with physicians in primary, secondary, and tertiary health care in a publicly funded health care system.
Design
A population-based registry study.
Setting
Different health care settings in Västernorrland county, Sweden.
Subjects
All residents in the county at the end of 2006.
Main outcome measures
The number of people per 1000 residents who had at least one appointment with a physician in an average month in different health care settings.
Results
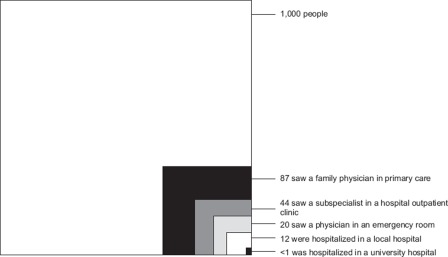
A total of 87 people had appointments with a physician in primary health care, 44 in outpatient clinics at a regional hospital, 20 in an emergency department, 14 in home care, and two in a university hospital outpatient clinic. Twelve were hospitalized at a regional hospital and <1 at the university hospital. Being young or elderly, female, divorced, widowed, and having a contractor as usual source of care were all independently associated with higher odds of receiving primary care.
Conclusions
The physician's office in primary care is the setting that has the potential to affect the largest number of people. The extent of the use of health care was independently influenced by all sociodemographic characteristics studied, which highlights the importance of individual factors in future resource allocation. Regarding availability the ecology model provides superior information as compared with the absolute number of physicians' appointments. The prerequisites in Sweden of high-quality registries and unique personal identification numbers encourage future research on the ecology model to optimize accessibility of health care.
Key Words: Delivery of health care, health services research, medical ecology, resource allocation
The medical ecology model has been used to assess health care use in private and mixed-finance systems but not in publicly funded systems. In the present study of a publicly funded health care system highly reliable population-based registers on an individual level were used.
The physician's office in primary care is the setting that has the potential to affect the largest number of people.
Sociodemographic characteristics influenced the proportion of physician appointments, which highlights the importance of individual factors in future resource allocation.
An ecological model of health care organization was shown to demonstrate a valid perspective of medical care use in the 1960s [1] in a model extended from general practice [2]. The model organizes complex relationships known to affect health care and the health of populations [3], with implications for the organization of health care, medical training, and research [4–6]. The model has also stated geo-demographic and socioeconomic status as factors influencing health care use [5,7]. Despite substantial changes in medicinal care, including improved techniques for data collection, a reassessment of health care use by the ecology model showed similar structures to those in the 1960s [7,8].
For several decades welfare policies in Sweden have provided a high level of social security protection to all residents, resulting in less income inequality and lower poverty rates, as compared with other European countries [9]. This includes health and medical care services that are financed primarily by taxation and to some extent by fees and government subsidies. At national level the county councils are responsible for management, including record keeping. This offers excellent opportunities to study health care use in the total population.
Previous studies in privately or mixed-finance systems using the ecology model have demonstrated two critical elements required for a balanced health care system: having health insurance and having a usual source of care [10]. No previous study has investigated health care use with the ecology model in a publicly funded system in a total population study.
The present study focuses on the influence of sociodemographic factors on access to appointments with physicians in primary, secondary, and tertiary health care in one publicly funded Swedish county.
Material and methods
The county of Västernorrland (LVN) is situated in central Sweden. During 2006 LVN ran three hospitals with one emergency department each and 36 primary healthcare centres including three emergency departments. The Umeå University Hospital is north of the county.
The Swedish Tax Office (STO) allocates to every citizen of Sweden a unique census registration number (CRN) that permits accurate record linkage between databases. Using the CRNs the County Census Bureau holds a population registry kept up to date by law, on date and country of birth, address, sex, and marital status. In addition, the LVN records every single contact in every health care setting in terms of date and type of health care contact, category of health care provider, diagnosis, and usual health care provider by the CRN of each person seeking health care. Its quality is regulated by standard operating procedures. Data on referrals to the Umeå University Hospital were recorded separately.
The STO registry that included 243 978 inhabitants of LVN at 31 December 2006, the LVN registry of the >1 200 000 physician appointments in 2006, and the registry of referred care at the University Hospital were merged by CRN. The discharge date was used for hospital stays and we assumed that similar numbers of people moved to and from the county. To guarantee confidentiality all CRNs were replaced with a random 20-digit number before data extraction by the computer program AVID® (Technology Nexus Inc. Omaha, NE).
Variables
The dependent variable “person-month” [1] was defined as the number of people per 1000 inhabitants who, in an average month, had an appointment with a physician at least once during 2006 in any of the following settings: (1) primary health care centres; (2) hospital outpatient departments, (3) hospital inpatient departments; (4) emergency departments; (5) their own home; (6) university hospital outpatient departments; and (7) university hospital inpatient departments. The “person-month” variable reflects use or non-use by an individual and not the absolute number of health care contacts per person.
Family physicians/general practitioners (GPs) conducted the service at primary health care centres and subspecialist physicians (e.g. cardiologist, gastroenterologist, surgeon) in the other settings except at emergency departments and patients' homes where both categories could conduct the service. We used the budgeting site code as a unique identifier for each health care provider unit.
The following variables were categorized and used as predictor variables: (1) age, in completed years at the end of 2006: <5, 5–17, 18–24, 25–44, 45–65, or >65 years; (2) sex: male or female; (3) marital status: married, unmarried, widowed, or divorced; (4) country of birth: Sweden, other Nordic countries, other European country, or non-European country; (5) residence location: a city zone with >4000 inhabitants (urban), other parishes (rural); (6) care provider's funding: LVN or contractor.
Statistical analyses
Descriptive analyses were performed using the person-month concept. The value record was set to”0” if a person had no contact with any setting and to “1” if the person had at least one appointment with a physician. The monthly person-month value records for each person were totalled and divided by 12 to obtain an estimate of the use of services in a typical month. We then multiplied this by 1000 and divided the product by the number of people who had seen a physician in each setting.
To estimate the independent effects on the person-month variable the individual characteristics were entered into a logistic regression analysis to derive adjusted odds ratios (ORs). The reference category was the largest one for each characteristic.
Statistical analysis was performed using SAS program package version 9.1 (SAS Institute, Cary, NC, USA) [11].
Results
The number of people per 1000 residents who had at least one appointment with a physician in an average month by the different health care settings is shown in Figure 1.
Figure 1.
Number of people per 1000 inhabitants who had at least one appointment with a physician in an average month by the different health care settings.
Table I shows these proportions stratified by sociodemographic characteristics. A wide distribution effect on the appointments was exerted in virtually all settings by age, marital status, country of birth, in primary care and hospital outpatient department by sex, and at the university hospital appointments by care provider's funding. Place of residence showed small effects.
Table I.
Number of people per 1000 inhabitants, stratified by sociodemographic characteristics, who had at least one appointment with a physician in an average month by the different health care settings.
| Demographic characteristic | Primary care | Hospital outpatient | Hospital inpatient | Emergency department | Home care | University hospital outpatient | University hospital inpatient |
| Age (years) | |||||||
| <5 | 137.4 | 36.6 | 8.8 | 31.5 | 11.7 | 1.2 | 0.6 |
| 5–17 | 55.0 | 31.3 | 3.7 | 17.9 | 0.9 | 1.3 | 0.3 |
| 18–24 | 57.8 | 28.9 | 7.2 | 20.0 | 1.4 | 2.6 | 0.3 |
| 25–44 | 69.9 | 30.4 | 10.4 | 15.6 | 2.3 | 1.8 | 0.3 |
| 45–64 | 88.4 | 45.4 | 9.1 | 16.0 | 5.7 | 2.7 | 0.8 |
| ≥65 | 126.1 | 72.6 | 25.4 | 31.1 | 55.4 | 0.9 | 2.4 |
| Sex | |||||||
| Male | 71.7 | 39.6 | 10.4 | 20.2 | 10.6 | 2.1 | 0.5 |
| Female | 101.9 | 47.5 | 13.1 | 20.6 | 17.9 | 2.1 | 0.6 |
| Marital status | |||||||
| Unmarried | 95.5 | 50.8 | 12.8 | 18.3 | 11.8 | 2.6 | 0.7 |
| Married | 71.3 | 33.3 | 7.9 | 19.0 | 6.0 | 1.8 | 0.4 |
| Divorced | 141.2 | 69.5 | 29.2 | 35.8 | 85.3 | 1.7 | 0.6 |
| Widowed | 105.2 | 54.0 | 16.6 | 24.7 | 17.6 | 2.6 | 1.0 |
| Country of birth | |||||||
| Sweden | 87.3 | 43.7 | 11.8 | 20.4 | 14.6 | 2.1 | 0.6 |
| Other Nordic | 79.8 | 43.8 | 14.1 | 24.1 | 8.5 | 2.4 | 0.6 |
| Other Europe | 56.2 | 29.0 | 6.8 | 14.0 | 3.9 | 1.9 | 0.5 |
| Non-Europe | 73.2 | 38.0 | 10.2 | 19.2 | 5.3 | 1.0 | 0.3 |
| Residence location | |||||||
| Urban | 86.3 | 43.9 | 11.8 | 21.7 | 12.9 | 2.1 | 0.5 |
| Rural | 88.0 | 42.8 | 11.8 | 17.4 | 17.4 | 2.1 | 0.6 |
| Primary care provider's funding | |||||||
| County council | 85.1 | 44.8 | 11.9 | 20.4 | 14.7 | 2.3 | 0.6 |
| Contractor | 95.3 | 37.5 | 11.1 | 20.4 | 12.5 | 1.1 | 0.4 |
The proportion of appointments with physicians adjusted for sociodemographic characteristics in the different settings (Table II) was statistically significantly sensitive to virtually all sociodemographic characteristics in the model in all health care settings. The most striking effects were exerted by age, marital status, and primary care provider's funding. Place of residence displayed the least effect. Having a contracted primary care provider increased the likelihood of having one's appointment there, and decreased the likelihood of going to the hospital outpatient department and of being referred to the University Hospital.
Table II.
Odds ratios for the number of people per 1000 inhabitants who had an appointment with a physician in the health care system adjusted by sociodemographic characteristics at the different health care settings.
| Demographic characteristic | Primary care | Hospital outpatient | Hospital inpatient | Emergency department | Home care | University hosp. outpatient | University hosp. inpatient |
| Age (years) | |||||||
| <5 | 2.66 (2.55–2.79)*** | 0.95 (0.91–0.99)* | 1.23 (1.15–1.33)*** | 2.27 (2.13–2.39)*** | 3.76 (3.47–4.08)*** | 0.63 (0.51–0.77)*** | 0.78 (0.58–1.10) |
| 5–17 | 0.78 (0.76–0.81)*** | 0.76 (0.73–0.79)*** | 0.49 (0.46–0.52)*** | 1.31 (1.25–1.36)*** | 0.19 (0.17–0.22)*** | 0.68 (0.59–0.78)*** | 0.51 (0.39–0.66)*** |
| 18–24 | 0.74 (0.71–0.77)*** | 0.71 (0.68–0.74)*** | 0.93 (0.86–0.99)* | 1.38 (1.31–1.45)*** | 0.25 (0.21–0.29)*** | 1.27 (1.10–1.46)*** | 0.54 (0.39–0.74)*** |
| 25–44 | 0.79 (0.77–0.81)*** | 0.71 (0.69–0.73)*** | 1.37 (1.31–1.43)*** | 1.04 (1.00–1.07)* | 0.46 (0.42–0.50)*** | 0.83 (0.75–0.92)*** | 0.51 (0.42–0.62)*** |
| 45–64 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ≥65 | 1.92 (1.87–1.97)*** | 1.75 (1.70–1.79)*** | 2.54 (2.45–2.64)*** | 1.75 (1.69–1.80)*** | 7.85 (7.42–8.31)*** | 1.08 (0.98–1.18) | 1.21 (1.04–1.40)* |
| Sex | |||||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Female | 1.50 (1.48–1.53)*** | 1.23 (1.20–1.25)*** | 1.19 (1.16–1.23)*** | 0.94 (0.92–0.96)*** | 1.27 (1.23–1.32)*** | 0.99 (0.93–1.06) | 1.09 (0.97–1.23) |
| Marital status | |||||||
| Unmarried | 0.83 (0.81–0.85)*** | 0.88 (0.86–0.91)*** | 0.99 (0.95–1.03) | 1.00 (0.98–1.04) | 1.99 (1.87–2.11)*** | 0.85 (0.77–0.94)** | 0.81 (0.68–0.96)* |
| Married | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Divorced | 1.07 (1.04–1.10)*** | 1.07 (1.03–1.10)*** | 1.21 (1.16–1.27)*** | 1.32 (1.27–1.37)*** | 1.52 (1.43–1.62)*** | 1.02 (0.91–1.14) | 1.22 (1.02–1.46)* |
| Widowed | 1.07 (1.03–1.12)*** | 0.98 (0.94–1.01) | 1.41 (1.35–1.48)*** | 1.47 (1.41–1.54)*** | 3.15 (2.99–3.30)*** | 0.67 (0.57–0.78)*** | 0.73 (0.58–0.93)** |
| Country of birth | |||||||
| Sweden | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Other Nordic | 0.86 (0.78–0.94)*** | 0.99 (0.90–1.09) | 1.24 (1.08–1.43)** | 1.06 (0.95–1.19) | 0.77 (0.61–0.99)* | 1.17 (0.84–1.64) | 1.20 (0.68–2.12) |
| Other Europe | 0.62 (0.54–0.70)*** | 0.74 (0.64–0.87)*** | 0.71 (0.55–0.91)** | 0.74 (0.62–0.89)** | 0.93 (0.62–1.38) | 1.04 (0.64–1.71) | 0.72 (0.23–2.24) |
| Non-Europe | 0.88 (0.83–0.93)*** | 1.12 (1.05–1.20)*** | 1.28 (1.16–1.40)*** | 1.02 (0.95–1.10) | 1.92 (1.64–2.23)*** | 0.58 (0.43–0.79)*** | 0.89 (0.54–1.47) |
| Residence location | |||||||
| Urban | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Rural | 1.07 (1.05–1.09)*** | 0.94 (0.92–0.95)*** | 1.02 (0.99–1.06) | 0.80 (0.79–0.82)*** | 1.23 (1.18–1.28)*** | 0.93 (0.86–0.99)* | 0.97 (0.86–1.10) |
| Primary care provider's funding | |||||||
| County | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Contractor | 1.20 (1.17–1.22)*** | 0.87 (0.85–0.89)*** | 0.99 (0.95–1.03) | 1.02 (0.99–1.05) | 0.97 (0.93–1.02) | 0.54 (0.49–0.61)*** | 0.65 (0.55–0.78)*** |
Notes: *p<0.05; **p<0.01; ***p<0.001.
Discussion
The GP's office was the setting in which the most people had appointments with a physician in a typical month. Therefore this is the setting that has the potential to affect the largest number of people of relevance for implementation strategies, education, and research. The proportion of appointments with physicians was sensitive to virtually all sociodemographic characteristics, which highlights the importance of individual factors for future resource allocation.
The strength of the study was the use of high-quality registries for all physician appointments on the individual level in the county's population. This assured high reliability of the results including the multiple regression analyses, prevented recall and selection bias, prevented the sociodemographic variables from acting as confounders for each other, and decreased the probability of contradictory events [12,13].
The present study had several limitations, the most important of which was the absence of certain socioeconomic variables. Data on self-perceived health problems and patient ailments would have been useful, as previously proposed [10]. There was no recent assessment of the quality of the medical registries used.
This is the first study, to the best of our knowledge, using the classic ecology model in a publicly funded health care system with population-based registry data. In previous studies survey data were used in privately or mixed-finance health care systems [5,7,8,14–17]. Overall, in LVN the proportion of residents who consulted a physician appears to be smaller, and the dispersion to the alternative settings was different, as compared with previous studies [5,7,8]. Previous ecology model studies demonstrated that women, young people, and elderly people were most likely to make use of health care resources [5,7,8]. In the present study, marital status, country of birth, and health care source also significantly affected health care use. Living in a rural area in LVN increased the likelihood of having an appointment with a GP and decreased the probability of having an appointment with a subspecialist.
Previous studies using the ecology model highlighted the fact that the focus of medical education activities is at the care-providing sites that handle the major load of care contacts [1,4]. These settings are the most conducive to healthcare education, preventive counselling, chronic disease care, and activities dependent on a sustained partnership between clinicians and patients. This was also supported by the results of the present study and suggests that more time should be spent on training physicians and physicians-to-be outside the hospitals.
The variable “person-month” is less sensitive as a measure of the use of health care services than the absolute number of appointments, since the latter includes repeated appointments for medical reasons. This is shown by the official statistics for appointments with family physicians in LVN in 2006 [18]: the absolute number was 295 795 corresponding to 101 appointments with a family physician per 1000 residents per month (1000*[(295795/243978)/12]), which is 16.1% (14/87) more than the rate of use of such services based on a person-month variable (87/1000). This is even more evident for appointments with subspecialists at the hospital outpatient departments: the absolute number of appointments was 229 265, corresponding to 78 appointments with the subspecialist per 1000 residents per month (1000*[(229265/243978)/12]), which is 77% (34/44) more than the corresponding person-month parameter (44/1000).
Interestingly, in the present study there was a large discrepancy between contracted and public primary care offices concerning the proportion of physician appointments in primary care, hospital outpatient care, and university hospital care. This could be explained by the greater density of physicians, greater confidence or accessibility to the care unit, or organizational differences of contracted offices. In any case, it points out a condition of great importance since access to health care has a role in generating inequalities in hard end-points such as mortality, even in high-income countries [19,20].
In 2006 the proportion of females in LVN and the whole country was 50.1 and 50.4, respectively, and the population distribution (%) by age groups 0–17, 18–64 and 65– in LVN and the whole country were: 20.2, 59.4, 20.4 and 21.2, 61.4 and 17.4, respectively [21]. In addition, the number of GPs per 100 000 inhabitants in 2006 in the northern region of Sweden was 62 as compared with 60 for the whole country [22]. From this perspective, the results in the present study might be representative of other Swedish counties.
The present study shows how registry data in Scandinavian health care can be used on aggregated levels to generate important knowledge for the health care organization in general and for primary care and general practice in particular. The prerequisites of high-quality registries and unique identification numbers encourage future research on the ecology model to optimize accessibility of health care.
Conclusions
The GP's office is the setting that has the potential to affect the largest number of people. The proportion of appointments with physician was independently influenced by all the sociodemographic characteristics, which highlights the importance of individual factors in future resource allocation. Regarding availability the ecology model provides superior information as compared with the absolute number of physician's appointments.
Acknowledgements
The regional ethics review board of the University of Umeå had no objections to the study on 6 May 2008 (reference number 08-014M). The authors would like to thank Anna Bostedt for help merging the databases.
Funding
The study was supported by grants from LVN. The researchers were fully independent of the funders regarding the present work.
Conflict of interest
The authors have no conflicts of interest.
References
- 1.White KL, Williams TF, Greenberg BG. The ecology of medical care. N Engl J Med. 1961;265:885–92. doi: 10.1056/NEJM196111022651805. [DOI] [PubMed] [Google Scholar]
- 2.Horder J, Horder E. Illness in general practice. The Practitioner. 1954;173:177–87. [PubMed] [Google Scholar]
- 3.Alcock P, Glennerster H, Oakley A, Sinfield A. Welfare and wellbeing. Bristol, UK: Policy Press; 2001. [Google Scholar]
- 4.White KL. The ecology of medical care: Origins and implications for population-based healthcare research. Health Serv Res. 1997;32:11–21. [PMC free article] [PubMed] [Google Scholar]
- 5.Fryer GE, Jr., Green LA, Dovey SM, Yawn BP, Phillips RL, Lanier D. Variation in the ecology of medical care [see comment] Ann Fam Med. 2003;1:81–9. doi: 10.1370/afm.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dovey SM, Green LA, Phillips RL, Fryer GE. The ecology of medical care for children in the United States: A new application of an old model reveals inequities that can be corrected. Am Fam Phys. 2003;68:2310. [PubMed] [Google Scholar]
- 7.Dovey S, Weitzman M, Fryer G, Green L, Yawn B, Lanier D, et al. The ecology of medical care for children in the United States. Pediatrics. 2003;111:1024–9. doi: 10.1542/peds.111.5.1024. [DOI] [PubMed] [Google Scholar]
- 8.Green LA, Fryer GE, Jr., Yawn BP, Lanier D, Dovey SM. The ecology of medical care revisited [see comment] N Engl J Med. 2001;344:2021–5. doi: 10.1056/NEJM200106283442611. [DOI] [PubMed] [Google Scholar]
- 9.Fritzell J. Still different? Income distribution in the Nordic countries in a European comparison. In: Kautto M, Fritzell J, Hvinden B, Kvist J, Uusitalo H, editors. Nordic welfare state in the European context. London: Routledge; 2001. pp. 18–41. [Google Scholar]
- 10.White KL. Two cheers for ecology. Ann Fam Med. 2003;1:67–9. doi: 10.1370/afm.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cary, NC: SAS Institute; Statistical Analysis System. http://www.sas.com/technologies/analytics/statistics. [Google Scholar]
- 12.Morgenstern H. Ecologic studies in epidemiology: Concepts, principles, and methods. Annu Rev Public Health. 1995;16:61–81. doi: 10.1146/annurev.pu.16.050195.000425. [DOI] [PubMed] [Google Scholar]
- 13.Wamala S, Merlo J, Bostrom G, Hogstedt C. Perceived discrimination, socioeconomic disadvantage and refraining from seeking medical treatment in Sweden. J Epidemiol Community Health. 2007;61:409–15. doi: 10.1136/jech.2006.049999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bliss EB, Meyers DS, Phillips RL, Jr, Fryer GE, Dovey SM, Green LA. Variation in participation in health care settings associated with race and ethnicity [see comment] J Gen Intern Med. 2004:931–6. doi: 10.1007/s11606-004-0008-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yawn BP, Fryer GE, Phillips RL, Dovey SM, Lanier D, Green LA. Using the ecology model to describe the impact of asthma on patterns of health care. BMC Pulmonary Med. 2005;5:7. doi: 10.1186/1471-2466-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tondo L, Albert MJ, Baldessarini RJ. Suicide rates in relation to health care access in the United States: An ecological study. J Clin Psychiatry. 2006;67:517–23. doi: 10.4088/jcp.v67n0402. [DOI] [PubMed] [Google Scholar]
- 17.Leung GM, Wong IO, Chan WS, Choi S, Lo SV. The ecology of health care in Hong Kong. Soc Sci Med. 2005;61:577–90. doi: 10.1016/j.socscimed.2004.12.029. [DOI] [PubMed] [Google Scholar]
- 18.Söderberg E, Ekström S. Årsredovisning 2006. 2006 [cited 2011 25 January]; Available from: www.lvn.se/Demokrati-och-insyn/Sa-styrs-landstinget/Landstingsplanen/Arsredovisning.
- 19.Ezzati M, Hoorn SV, Rodgers A, Lopez AD, Mathers CD, Murray CJ. Estimates of global and regional potential health gains from reducing multiple major risk factors. Lancet. 2003;362:271–80. doi: 10.1016/s0140-6736(03)13968-2. [DOI] [PubMed] [Google Scholar]
- 20.Mackenbach JP, Stirbu I, Roskam AJ, Schaap MM, Menvielle G, Leinsalu M, et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. 2008;358:2468–81. doi: 10.1056/NEJMsa0707519. [DOI] [PubMed] [Google Scholar]
- 21.Statistics_Sweden. Population statistics 2006. 2007 2007-12-14 [cited 2011 13 January]; Available from: http://www.scb.se/Pages/TableAndChart____193256.aspx.
- 22.Hansell C, Schwarz H, Eriksson B. Labour supply in Sweden: Midwives, doctors, dental hygienists and dentists 2006. 2008 [cited 2011 14 January]; Available from: http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/8724/2008–125–4_20081254_rev.pdf.