Abstract
Background and objective
The number of elderly persons in society is increasing, placing additional demands on the public health system. Extensive use of drugs is common in the elderly, and in patients with dementia this further increases their vulnerability. Since 1998 the municipality of Kalmar, Sweden, has worked with a dementia management programme that focuses on early intervention in order to identify the patient's help needs at an early stage. An important part of the programme aims at optimizing pharmacological treatment. The objective of the present study is to evaluate whether the dementia programme had a secondary effect on the use of psychotropic medication in the elderly population in general.
Design and setting
A retrospective, drug utilization study analysing the use of selected drug categories by the elderly (75 years and older) in the Kalmar municipality compared with the whole of Sweden.
Results and conclusions
The results suggest that the dementia programme contributed to an improvement in psychotropic drug use in the elderly as a secondary effect. Furthermore, the implementation of this programme did not require allocation of extra funding.
Key Words: Alzheimer's disease, dementia, dementia nurse, disease management programme, drug monitoring, general practitioner, health economics
Extensive use of drugs is common among the elderly. In patients with dementia the disease increases their vulnerability to drugs.
Dementia management programmes with multi modal components such as the one presented here appear to improve the management of psychotropic drug use in the elderly as a secondary effect.
Implementation of this programme has not required allocation of extra funding.
The elderly population is increasing worldwide [1]. This entails further need for health care support. In Sweden, people aged 75 and older comprise 9% of the population, yet they consume 38% of the total amount of drugs, half of which are prescribed by general practitioners (GPs) [2,3]. Drug-related problems are common in this population [4,5]. Adverse drug reactions are a significant cause of hospitalization in this age group [6]. The elderly are more vulnerable to adverse drug reactions due to age-related changes in pharmacokinetics and pharmacodynamics. Further, psychotropic drugs may impede cognitive functions in the elderly, especially in patients with dementia [7]. These facts form the rationale for monitoring drug use in patients at risk of developing dementia.
Dementia is widespread in the elderly population. The prevalence of dementia is 1% at the age of 60 and doubles every five years [8]. The increased intensity and variability of symptoms associated with dementia progression leads to an increase in the use of drugs with psychotropic action [9]. In addition, elderly individuals suffering from cognitive disturbances, such as dementia, are more vulnerable to anticholinergic agents and neuroleptics [10–13].
In the Swedish municipality of Kalmar, with a population of 60 000 inhabitants (less than 1% of the entire population of Sweden), a dementia management programme has been established, involving primary care and specialist health services and municipal elderly care organizations [14]. This programme was initially implemented stepwise in 1998. From 2004 its use was extended throughout the county (340 000 inhabitants), with no allocation of extra funding. The main focus of the programme was to identify the patient with dementia as early in the disease as possible. In the primary care centres, dementia nurses (n = six) and GPs (n = 30) gathered information necessary for a dementia diagnosis. An evaluation of the patient's medications was made, including medical indication, dosage, and potential drug–drug interactions [14]. During the study period from 2000 to 2005, 1294 patients were included in the dementia programme. The effect of the programme and further analyses of this are presented elsewhere [14,15].
The objective of the present study was to evaluate whether the dementia programme had a secondary effect on the use of psychotropic medication in the general population of the elderly. The elderly population of the Kalmar municipality was compared with the entire elderly population of Sweden.
Material and methods
This is a retrospective drug utilization study. Two different data sources were used: longitudinal drug sales data from Swedish pharmacies from 2000 to 2005 and cross-sectional data from the Swedish Prescribed Drug Register (SPDR) [16] from October to December 2005. The individual-based SPDR was introduced only in July 2005 and, hence, did not cover our whole study period (2000 to 2005).
Demographics of the Kalmar municipality and Sweden were provided by Statistics Sweden [17]. The proportion of the population over 65, 75, and 85 years of age was calculated for the period 2000 to 2005. In Kalmar, 5510 persons were 75 years and older in 2005. Of these, approximately 815 individuals participated in the dementia programme. Sweden had a total population of 796 799 aged 75 years and older in 2005.
The investigated drugs were chosen based on their frequency of use by the elderly and their potential to influence brain functions [10]. These include antidementia drugs (N06D), neuroleptics (N05A), anxiolytics (N05B), antidepressants (N06A), and selected drugs with anticholinergic properties. The classification of anticholinergic drugs (Table I) was based on the definition by the Swedish National Board of Health and Welfare [18] together with international consensus [10].
Table I.
Agents with significant anticholinergic activity frequently used by the elderly in Sweden.
| ATC code | Class | Agent |
| G04BD | Urinary antispasmodics | Emeprone Oxybutynine Tolterodine |
| N05AA | Antipsychotics, low potency | Chlorpromazine Levomepromazine |
| N05AC02 | Antipsychotics, low potency | Thioridazine |
| N05AC03 | Antipsychotics, intermediate potency | Melperone |
| N05BB01 | Anxiolytics | Hydroxyzine |
| N06AA | Antidepressants, non-selective | Imipramine Chlomipramine Trimipramine Lofepramine Amitriptyline Nortriptyline Protriptyline Maprotiline |
The drug sales data from Swedish pharmacies associated with the use of drugs were analysed as DDD [2] per 1000 inhabitants and year for those 75 years and older. The DDD is the defined daily dose for a drug used for its main indication in adults [2]. The use of DDDs in this study enables us to assess trends in drug consumption and to make comparisons between population groups. From the year 2000 and onwards, the prescription data in Sweden are linked to the patient's address. Therefore data collection for this study starts in 2000. Along with drug use the costs of the target drugs were also analysed.
We additionally analysed cross-sectional data from the SPDR for individuals aged 75 years and older on 31 December 2005, based on the prescriptions filled during the three previous months. This method has been described in detail elsewhere [19].
Statistical analysis
We made descriptive analyses of DDDs and costs in the longitudinal drug sales data from Swedish pharmacies from 2000 to 2005, in Kalmar compared with Sweden as a whole. Further, logistic regression analysis for studies of the SPDR data was used, in order to analyse the use of neuroleptics, anxiolytics, sedatives, selective serotonin reuptake inhibitors (SSRIs), antidementia agents, and drugs with anticholinergic properties, during the last quarter of 2005. Adjustments were made for age, gender, and number of drugs. The relationships are expressed as odds ratios (ORs) with 95% confidence intervals (CIs).
Results
The populations of the Kalmar municipality and Sweden were similar in respect of age. There was, however, a slightly higher proportion of elderly women in Kalmar.
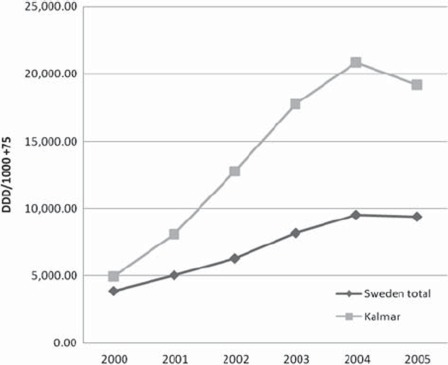
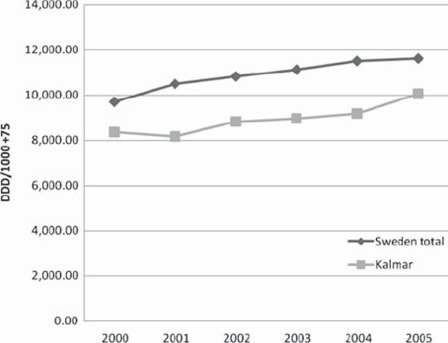
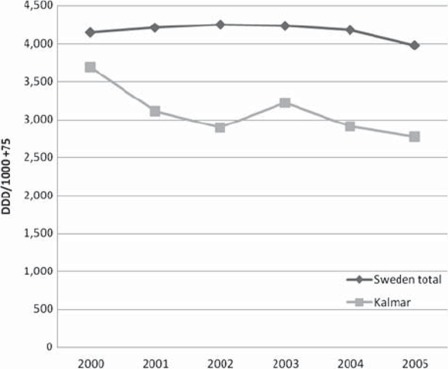
The sale of antidementia agents, mainly cholinesterase inhibitors, increased more in Kalmar compared with Sweden as a whole. During the introduction of the dementia programme, Kalmar increased its use by 289% and Sweden by 142% (Figure 1). The use of antidementia drugs was nearly twice as high in Kalmar as in the whole of Sweden in 2005. In Kalmar, the proportion of antidementia drugs prescribed by GPs increased from 42% to 86%. However, the amount prescribed by dementia specialists remained constant. Antidepressant drugs, mainly SSRI, were prescribed more often in the Kalmar municipality than in Sweden during the observation period but there was no increase in use compared with Sweden as a whole. The sale of anticholinergic drugs was lower in Kalmar (Figure 2). Furthermore, the sale of hypnotics decreased in Kalmar (−22%), along with the use of benzodiazepines (−15%). During the introduction of the dementia programme we did not see any difference in the sale of neuroleptics. However, when specifically analysing use in the elderly population, we observed a more pronounced decrease in the use of neuroleptics in Kalmar compared with the whole of Sweden (Figure 3). In Sweden, there was a 13% decrease in sales of neuroleptics from 2000 to 2005. However, in 2005, the use of neuroleptics by the elderly was 30% lower in Kalmar than in Sweden as a whole.
Figure 1.
Yearly sales of antidementia drugs (N06D) expressed as DDD/1000 persons 75 years and older in Kalmar and Sweden from 2000 to 2005 (Kalmar n = 5510 and the whole of Sweden n = 796, 799).
Figure 2.
Yearly sales of the major drugs with anticholinergic activity (G04BD, N05AA, N05AC02, N05BB01, N06AA) DDD/1000 persons 75 years and older in Kalmar and Sweden (Kalmar n = 5510 and the whole of Sweden n = 796, 799).
Figure 3.
Yearly sales of neuroleptic drugs (N05A) DDD/1000 persons 75 years and older in Kalmar and Sweden (Kalmar n = 5510 and the whole of Sweden n = 796, 799). Author(s):Jedenius, Johnell, Fast-bom, Strömqvist, Winblad, Andreasen
Table II shows a comparison of drug use based on data from the SPDR. These individual-based data confirm the above comparisons based on DDDs. Thus, antidementia drugs and SSRIs were used to a higher and neuroleptics to a lower extent in Kalmar than in Sweden as a whole.
Table II.
Number and proportion of persons (%) using neuroleptics, benzodiazepines, sleeping agents, SSRIs, antidementia agents, and drugs with anticholinergic properties among those 75 years and older in Kalmar and Sweden, 2005.1
| Kalmar (n = 5036) | Sweden total (n = 732230) | OR (95% CI) | |
| Neuroleptics (N05A) | 148 (2.9%) | 3.3071 (4.5%) | 0.71 (0.60–0.84) |
| Benzodiazepines (N05B) | 384 (7.6%) | 6.8644 (9.4%) | 0.90 (0.81–1.01) |
| Sleeping agents (N05C) | 1032 (20.5%) | 16.7338 (22.9%) | 0.95 (0.88–1.02) |
| SSRI antidepressants (N06AB) | 577 (11.5%) | 82.957 (11.3%) | 1.15 (1.05–1.26) |
| Antidementia agents (N06D) | 271 (5.4%) | 20.481 (2.8%) | 2.14 (1.89–2.43) |
| Drugs with anticholinergic properties | 270 (5.4%) | 42.007 (5.7%) | 1.05 (0.92–1.19) |
1The difference between Kalmar community and Sweden is expressed as an odds ratio (OR) controlled for age, gender, and number of drugs.
At the start of the programme the total cost of the target drugs was higher in Kalmar than in Sweden. During the beginning of the dementia programme the cost of antidementia drugs increased. This was more pronounced in Kalmar than in Sweden. Further, the sum of all target drugs in Sweden increased by 26% as compared with 1% in Kalmar during the observation period. As a result, the total cost of target drugs was equal in Kalmar and Sweden at the end of the study.
Discussion
From 2000 to 2005 the sales associated with the use of antidementia drugs increased in Kalmar, to a level twice as high as in the whole of Sweden. The question may be raised as to whether this is, in fact, excessive. However, even after the increase, the use of antidementia drugs only corresponded to about 40% of patients with Alzheimer's disease, i.e. those that may benefit from this treatment. We also observed a somewhat higher use of SSRI in Kalmar. The use of SSRI is recommended for depression, a condition frequently seen in elderly patients, especially in dementia [20]. Therefore, this finding may be regarded as positive, but needs to be further explored.
Neuroleptics [13,21], anxiolytics, sedatives-hypnotics, and drugs with anticholinergic properties are drugs that may cause serious side effects in the elderly [10,22]. In Kalmar, we observed that these drugs were used to a lesser extent from 2000 to 2005, compared with Sweden as a whole. Notably, the rate of decrease of neuroleptics was most prominent during the introduction of the dementia programme. Recently, there has been a debate in Sweden on the use of neuroleptics in the elderly [23], but our study was performed before this discussion. It has previously been shown that the elderly in Kalmar use three or more psychotropics to a lesser extent than the Swedish elderly in general [24]. One explanation could be regional difference in age distribution [25]. However, Kalmar's age distribution is similar to that for Sweden as a whole. Local therapy traditions may play a role, but this needs further investigation.
The cost of dementia drugs in Sweden increased by 32% and the corresponding cost in Kalmar by 50% during the study period. Despite this, the total cost of the targeted drugs in Kalmar was unchanged while increasing by 26% in Sweden as a whole. In addition, the dementia programme was implemented without any extra resource allocations. Moreover, it is worth noting that the cost for dementia drugs accounts for only 1% of the total cost for dementia care in Sweden [26].
A pertinent question is whether the dementia programme has played any role in the change of drug use seen in this analysis, and if so, in what way? One part of the programme focuses on optimizing pharmacological treatment, even though this is not the main goal in a dementia investigation. It is reasonable to assume that local education and caregiver support groups, in addition to the dementia programme, had an effect on drug use. In the literature, there are some dementia management programmes that describe changes in other areas such as time to nursing home placement [27–29]. However, to our knowledge, no dementia or elderly management programme has yet been presented in the literature, suggesting changes in long-term [30] prescribing patterns.
As a result of the dementia programme (2000–2005), 1294 cognitively impaired patients were identified in primary care [14], corresponding to over 10% of 65 and nearly 15% of 75-year-olds in the municipality. All of these patients were evaluated regarding their drug use. The demographic characteristics of the elderly population in Kalmar are comparable to those of the rest of Sweden. It was therefore possible to use Sweden as a comparative population in this study. Moreover, the organization of care is essentially similar throughout Sweden, which suggests that the findings can be generalized to the rest of Sweden.
Some limitations of this study should be mentioned. There was no information available on diagnoses, including dementia, or indications for the prescriptions. Thus, the present analyses do not focus on dementia patients but include all the elderly. Also, we do not know what the change in drug use means in terms of treatment of dementia and psychiatric disorders in the elderly. The use of two different drug data sources also has implications for our results. The individual-based SPDR was introduced in July 2005 and, thus, did not cover our whole study period of 2000 to 2005. We would have preferred to rely only on individual-based data but, due to this time restraint, we also had to analyse drug sales data. Future longitudinal studies of individual-based data are needed to investigate direct effects of management programmes. Moreover, it may be problematic to use all of Sweden as a comparison, as similar (activities) management programmes might be used elsewhere. However, to the best of our knowledge only one comparable project was ongoing at that time in one municipality in northern Sweden (Båtsman S, personal communication).
Our results indicate improvements in the use of psychotropic drugs in the elderly as a secondary effect of the implementation of a dementia management programme in primary care. In the drug sales data analyses, drugs with possible harmful effects on cognition (neuroleptics, anxiolytics, sedatives-hypnotics, and drugs with anticholinergic properties) were used to a lesser extent. This was confirmed regarding neuroleptics in the analyses of the SPDR. Moreover, drugs with possible benefits for patients with dementia, such as antidementia drugs and SSRIs, were used to a higher extent in Kalmar (supported by both drug sales data and the SPDR). Future analysis with a prospective approach is needed to compare different health care programmes aimed at specific groups of patients, in order to evaluate which approach is the most effective, in both health and economic terms. Nevertheless, the dementia management programme in Kalmar was implemented without extra funding, suggesting economic benefits in favour of this programme.
Acknowledgements
Many thanks are offered to all patients and primary care staff in the Kalmar Municipality. Special thanks go to Maud Löfström, Margareta Johansson, Kristian Aranäs, Anneli Adolfsson, Marianne Jakobsson, Helen Holmström Ann-Christen Arvidsson, Katarina Jervelind, Janet Mosén, Lena Rundgren, Thomas Johansson, and Gunvor Adolfsson. Statistical support and advice from Gunnar Edman. Finally, the authors would like to thank Gunilla Johansson and Roberta Boson for linguistic support.
Ethical approval
The study was approved by the Ethical Committees at Linköping University (Dnr. 03-494) and Karolinska Institutet, Stockholm (Dnr 2006/948-31).
Funding
The Swedish Alzheimer Association and the Foundation for the Memory of Ragnhild and Einar Lundströms.
Potential conflict of interests
The main author, E. Jedenius, is also medical adviser at Janssen Pharmaceutica in Sweden.
References
- 1.Fratiglioni L, De Ronchi D, Aguero-Torres H. Worldwide prevalence and incidence of dementia. Drugs Aging. 1999;15:365–75. doi: 10.2165/00002512-199915050-00004. [DOI] [PubMed] [Google Scholar]
- 2.WHO. WHO Collaborating Centre for Drug Statistics Methodology. 2008. [cited 2007]; available from: http://www.whocc.no/atcddd/
- 3.Pehrsson Å, Lindström E, Kohl E, Jarnehammar K, Hirsch C, Lönnebo M, et al. Report No. 6504–02. Stockholm: Norra Stockholms läkemedelskommité; 2002 May 2002. Läkemedelsgenomgångar på Kungsholmen och Norrmalm. [Drug revue in Kungsholmen and Norrmalm. Report No. 6504-02. Stockholm: Northern Stockholm Pharmaceutical Committee] [Google Scholar]
- 4.Hajjar ER, Hanlon JT, Artz MB, Lindblad CI, Pieper CF, Sloane RJ, et al. Adverse drug reaction risk factors in older outpatients. Am J Geriatr Pharmacother. 2003;1:82–9. doi: 10.1016/s1543-5946(03)90004-3. [DOI] [PubMed] [Google Scholar]
- 5.Hanlon JT, Lindblad CI, Hajjar ER, McCarthy TC. Update on drug-related problems in the elderly. Am J Geriatr Pharmacother. 2003;1:38–43. doi: 10.1016/s1543-5946(03)80014-4. [DOI] [PubMed] [Google Scholar]
- 6.Onder G, Pedone C, Landi F, Cesari M, Della Vedova C, Bernabei R, et al. Adverse drug reactions as cause of hospital admissions: Results from the Italian Group of Pharmacoepidemiology in the Elderly (GIFA) J Am Geriatr Soc. 2002;50:1962–8. doi: 10.1046/j.1532-5415.2002.50607.x. [DOI] [PubMed] [Google Scholar]
- 7.Turnheim K. Drug therapy in the elderly. Exp Gerontol. 2004;39:1731–8. doi: 10.1016/j.exger.2004.05.011. [DOI] [PubMed] [Google Scholar]
- 8.Jorm AF, Korten AE, Henderson AS. The prevalence of dementia: A quantitative integration of the literature. Acta Psychiatr Scand. 1987;76:465–79. doi: 10.1111/j.1600-0447.1987.tb02906.x. [DOI] [PubMed] [Google Scholar]
- 9.Giron MS, Wang HX, Bernsten C, Thorslund M, Winblad B, Fastbom J. The appropriateness of drug use in an older nondemented and demented population. J Am Geriatr Soc. 2001;49:277–83. doi: 10.1046/j.1532-5415.2001.4930277.x. [DOI] [PubMed] [Google Scholar]
- 10.Björkman IK, Fastbom J, Schmidt IK, Bernsten CB. Pharmaceutical Care of the Elderly in Europe Research (PEER) Group, Drug–drug interactions in the elderly. Ann Pharmacother. 2002;36:1675–81. doi: 10.1345/aph.1A484. [DOI] [PubMed] [Google Scholar]
- 11.Hosia-Randell HM, Muurinen SM, Pitkala KH. Exposure to potentially inappropriate drugs and drug–drug interac-tions in elderly nursing home residents in Helsinki, Finland: A cross-sectional study. Drugs Aging. 2008;25:683–92. doi: 10.2165/00002512-200825080-00005. [DOI] [PubMed] [Google Scholar]
- 12.Pitkala KH, Laurila JV, Strandberg TE, Tilvis RS. Behavioral symptoms and the administration of psychotropic drugs to aged patients with dementia in nursing homes and in acute geriatric wards. Int Psychogeriatrics/IPA. 2004r;16:61–74. doi: 10.1017/s1041610204000079. [DOI] [PubMed] [Google Scholar]
- 13.Raivio MM, Laurila JV, Strandberg TE, Tilvis RS, Pitkala KH. Neither atypical nor conventional antipsychotics increase mortality or hospital admissions among elderly patients with dementia: A two-year prospective study. Am J Geriatr Psychiatry. 2007 Feb 9; doi: 10.1097/JGP.0b013e31802d0b00. [DOI] [PubMed] [Google Scholar]
- 14.Jedenius E, Wimo A, Stromqvist J, Andreasen N. A Swedish programme for dementia diagnostics in primary healthcare. Scand J Prim Health Care. 2008;26:235–40. doi: 10.1080/02813430802358236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jedenius E, Wimo A, Stromqvist J, Jonsson L, Andreasen N. The cost of diagnosing dementia in a community setting. Int J Geriatric Psychiatry. 2009 Aug 14; doi: 10.1002/gps.2365. [DOI] [PubMed] [Google Scholar]
- 16.Wettermark B, Hammar N, Fored CM. The new Swedish Prescribed Drug Register: Opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf. 2007;16:726–35. doi: 10.1002/pds.1294. [DOI] [PubMed] [Google Scholar]
- 17.Sweden SS. Description of the population in Sweden. SCB. Stockholm: Statistics Sweden; 2008. Population statistics 2000–5. [Google Scholar]
- 18.Fastbom J. [Increased consumption of drugs among the elderly results in greater risk of problems] Lakartidningen. 2001;98:1674–9. [PubMed] [Google Scholar]
- 19.Johnell K, Fastbom J, Rosen M, Leimanis A. Inappropriate drug use in the elderly: A nationwide register-based study. Ann Pharmacother. 2007;41:1243–8. doi: 10.1345/aph.1K154. [DOI] [PubMed] [Google Scholar]
- 20.Jost BC, Grossberg GT. The evolution of psychiatric symptoms in Alzheimer's disease: A natural history study. J Am Geriatr Soc. 1996;44:1078–81. doi: 10.1111/j.1532-5415.1996.tb02942.x. [DOI] [PubMed] [Google Scholar]
- 21.Klarin I, Fastbom J, Wimo A. A population-based study of drug use in the very old living in a rural district of Sweden, with focus on cardiovascular drug consumption: Comparison with an urban cohort. Pharmacoepidemiol Drug Saf. 2003;12:669–78. doi: 10.1002/pds.878. [DOI] [PubMed] [Google Scholar]
- 22.Rognstad S, Brekke M, Fetveit A, Spigset O, Wyller TB, Straand J. The Norwegian General Practice (NORGEP)criteria for assessing potentially inappropriate prescriptions to elderly patients: A modified Delphi study. Scand J Prim Health Care. 2009;27:153–9. doi: 10.1080/02813430902992215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Läkemedelsverket. Läkemedelsbehandling och bemötande vid Beteendemässiga och Psykiska Symtom vid Demenssjukdom – BPSD Swe MPA. 2008. [Dementia societal cost and the number of people with dementia in Sweden 2005. Stockholm: National Board of Health and Welfare; 2007] [Google Scholar]
- 24.Johnell K, Fastbom J, Rosen M, Leimanis A. Low quality of drug use among the elderly: An analysis based on the national drug registry shows regional differences. Lakartidningen. 2007;104:2158–62. [PubMed] [Google Scholar]
- 25.Hovstadius B, Astrand B, Petersson G. Assessment of regional variation in polypharmacy. Pharmacoepidemiol Drug Saf. 2010;19:375–83. doi: 10.1002/pds.1921. [DOI] [PubMed] [Google Scholar]
- 26.Wimo A, Jonsson L, Johansson L. Demenssjukdomarnas samhällskostnader och antalet dementa i Sverige 2005. Stockholm: National Board of Health and Welfare; 2007. [Google Scholar]
- 27.Andren S, Elmstahl S. Effective psychosocial intervention for family caregivers lengthens time elapsed before nursing home placement of individuals with dementia: A five-year follow-up study. Int Psychogeriatrics/IPA. 2008:1–16. doi: 10.1017/S1041610208007503. [DOI] [PubMed] [Google Scholar]
- 28.Brodaty H, Green A, Koschera A. Meta-analysis of psychosocial interventions for caregivers of people with dementia. J Am Geriatr Soc. 2003;51:657–64. doi: 10.1034/j.1600-0579.2003.00210.x. [DOI] [PubMed] [Google Scholar]
- 29.Eloniemi-Sulkava U, Notkola IL, Hentinen M, Kivela SL, Sivenius J, Sulkava R. Effects of supporting community-living demented patients and their caregivers: A randomized trial. J Am Geriatr Socy. 2001;49:1282–7. doi: 10.1046/j.1532-5415.2001.49255.x. [DOI] [PubMed] [Google Scholar]
- 30.Pitkala KH, Strandberg TE, Tilvis RS. Is it possible to reduce polypharmacy in the elderly? A randomised, controlled trial. Drugs Aging. 2001;18:143–9. doi: 10.2165/00002512-200118020-00007. [DOI] [PubMed] [Google Scholar]