Abstract
Background
Several studies have identified risk factors for proximal junctional kyphosis (PJK) after instrumentation for scoliosis, but the relative risks are unclear.
Questions/purposes
We identified risk factors for PJK in idiopathic scoliosis and determined their relative risks in a predictive model.
Methods
We retrospectively reviewed the charts of all 249 patients with idiopathic scoliosis who underwent surgery from 1996 to 2008. We compared those who developed PJK to those who did not. We identified risk factors for PJK and performed univariate and multivariate analyses to determine independent risk factors. We then used a Cox proportional-hazards model to evaluate the time to the development of PJK. The minimum followup time was 1.5 years (mean, 4 years; range, 1.5–9 years).
Results
The incidence of PJK in our series of patients with idiopathic scoliosis was 17%. There was no difference in Scoliosis Research Society-22 scores between patients without and with junctional kyphosis. Independent risk factors included proximal fusion to T1 through T3 and sagittal sacral vertical line, while in the Cox model a combined anterior-posterior approach surgery was the most important risk factor.
Conclusions
Patients with a T1 through T3 upper instrumented level, combined anterior-posterior surgery, and increased sagittal sacral vertical line difference had a higher likelihood of developing PJK. Of these risk factors, anterior-posterior surgery was the strongest risk factor.
Level of Evidence
Level III, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Spinal arthrodesis reportedly prevents progressive deformity in idiopathic scoliosis [2, 3]. One of the complications that can occur after arthrodesis in spine fusion is proximal junctional kyphosis (PJK) [2–8, 10–13]. PJK is the progression of kyphosis at the proximal end of a construct greater than 10°, which can lead to progressive decompensation in the sagittal plane and, in some cases, neurologic compromise [2]. The reported incidence ranges between 10% and 40% [2, 5–13]. Reported risk factors for developing PJK include long rigid fusion constructs [2, 5], integrity of the posterior soft tissue tension band [2], instrumentation techniques [3, 7], magnitude of sagittal balance correction, and bone quality [12]. Some postulate PJK has a multifactorial etiology related to surgical and patient factors [2, 7, 12, 13]. However, the relative risks of these various factors and their interactions are unclear.
We therefore identified risk factors for PJK in idiopathic scoliosis and determined their relative risks in a predictive model.
Patients and Methods
We identified all 336 patients with idiopathic scoliosis treated with primary instrumentation and fusion from 1996 and 2008. We included patients from all age groups with the diagnosis of idiopathic scoliosis. Patients who did not have complete charts, including a preoperative dual-energy x-ray absorptiometry (DEXA), radiographs, and Scoliosis Research Society-22 (SRS-22) questionnaire scores [1] from the pre- and postoperative periods, were excluded from the study, leaving a total of 249 patients for our study. There were 214 females and 35 males with an average age of 35 years (range, 15–62 years) (Table 1). Forty-two of these patients (17%) developed PJK during the followup period. In the PJK group, the average age was 42 years. Eighteen of the 42 (43%) patients who developed PJK during followup did so within the first postoperative year (Fig. 1). The minimum followup was 1.5 years (mean, 4 years; range, 1.5–9 years). We lost no patients to followup and did not recall any patients specifically for this study; we obtained all data from medical records and radiographic studies.
Table 1.
Descriptive summary of patient cohort
| Descriptive parameter | Mean (SD) or number (%) |
|---|---|
| Total number of patients | 249 |
| No PJK group | 207 (83.1%) |
| PJK group | 42 (16.9%) |
| Female | 214 (85.9%) |
| Mean age (years) | 35 (19) |
| < 18 years | 91 (36.8%) |
| 19–29 years | 22 (8.1%) |
| 30–39 years | 25 (10.1%) |
| 40–49 years | 42 (17.0%) |
| > 50 years | 69 (27.7%) |
| Osteoporosis or osteopenia | |
| Normal | 156 (62.7%) |
| Osteopenia | 16 (6.4%) |
| Osteoporosis | 77 (30.9%) |
| Fusion to S1 | 57 (22.9%) |
| Thoracoplasty | 75 (30.1%) |
| Surgical approach | |
| Anterior only | 14 (5.6%) |
| Posterior only | 147 (59.0%) |
| Anterior-posterior | 88 (35.3%) |
| Instrumentation technique | |
| Hook/hybrid | 182 (73.1%) |
| Pedicle screw | 40 (16.1%) |
| Vertebral body screws (anterior) | 25 (10.0%) |
| Wires | 2 (0.8%)* |
| Upper instrumented level | |
| T1 to T3 | 83 (33.3%) |
| T4 to T12 | 163 (65.5%) |
| L1 or below | 3 (1.2%)* |
| Levels fused | 10.64 (3.13) |
| PJK angle | 3.36º (7.28º) |
| SSVL difference (mm) | −4.40 (40.45) |
| SRS score difference | 3.73 (0.53) |
| Followup (years) | 3.9 (2.3) |
* Excluded from data analysis due to low numbers; PJK = proximal junction kyphosis; SSVL = sacral sagittal vertical line difference between pre- and postoperative time; SRS = Scoliosis Research Society.
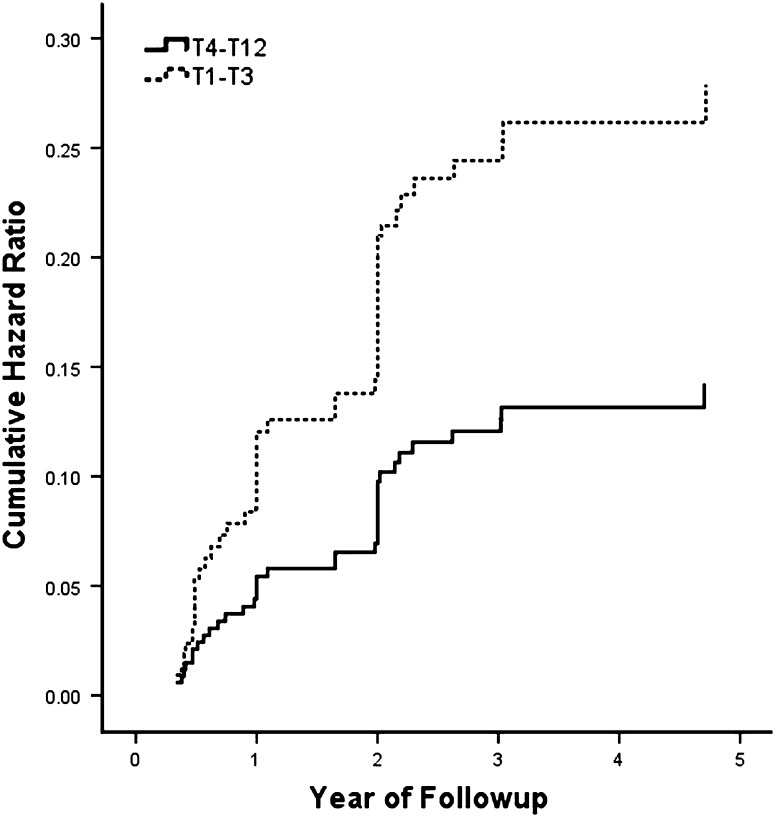
Fig. 1.
The graph shows a cumulative hazard plot for the development of PJK with stratification based on UIV. According to this model, those with proximal fusion levels ending at T1-T3 have a higher risk at all time points for developing PJK than those with fusions ending more distally in the T4-T12 region.
For DEXA, we defined normal patients as having a T-score of greater than −1.0, those with osteopenia as having a T-score of between −1.0 and −2.5, and those with osteoporosis as having a T-score of less than −2.5. We identified normal bone quality in 156 of 249 (63%) patients and observed abnormal bone quality in 93 of 249 (37%) patients: osteopenia in 16 of 249 (6%) and osteoporosis in 77 of 249 (31%).
All patients had a posterior or combined anterior-posterior arthrodesis of the spine with varied instrumentation techniques ranging from hooks, wires, pedicle screws, to cages. An average of 10.64 levels was fused in the whole group, and 57 of 249 (23%) patients had a fusion that included the S1 level.
Routine followup methodology included postoperative visits at 2 weeks, 6 to 10 weeks, 6 months, and 1 year after surgery. Subsequent followups were annual. Each followup appointment consisted of a SRS-22 questionnaire (including the pain and self-image subscales), radiographs, and a clinical evaluation. Radiographic followup included radiographs at three different time points: preoperative, immediate postoperative (first followup after surgery, usually 6 to 10 weeks postoperatively), and most recent followup. Patients stood naturally but with their shoulders flexed forward approximately 30° so that their vertebral bodies could be visualized on the lateral radiograph; we used a 91.4-cm-long cassette for both AP and lateral radiographs. We considered the most recent radiographs after the date of surgery to be our followup interval. If the radiographic images were poor enough that we could not make an accurate Cobb measurement, we did not include those patients in the study.
Two of the authors (MY, HJK) conducted all radiographic measurements, including a senior spinal surgeon who was independent of the operative team. Radiographic analysis included Cobb angle measurements of the major curves on the preoperative, early postoperative (within 2 months), 2-year postoperative, and final followup radiographs of varying followup times up to 9 years. We presumed the Cobb angle to be reliably measured to within 5°. We measured global coronal balance as the distance between the C7 plumb line and the center sacral vertical line (CSVL). On the lateral radiographs, we measured global sagittal balance as the distance from the C7 plumb line to the perpendicular line drawn from the superior posterior endplate of S1 vertebral body (sagittal sacral vertical line [SSVL]). If the C7 plumb line fell behind the SSVL, global sagittal balance was negative. If the C7 plumb line fell in front of the SSVL, global sagittal balance was positive. If the C7 plumb line fell on the SSVL, global sagittal balance was zero. We measured thoracic kyphosis from the upper endplate of T5 to the lower endplate of T12 and measured the lumbar lordosis from the lower endplate of T12 to the upper endplate of S1.
We defined the proximal junctional angle as the caudal endplate of the upper instrumented vertebrae (UIV) to the cephalad endplate of two supraadjacent vertebrae above the UIV, as described by Glattes et al. [2]. Two disc spaces proximal to the UIV usually demonstrated the proximal junctional change. We defined abnormal PJK by two criteria as described in a previous study [2]: (1) proximal junction sagittal Cobb angle of 10° or greater and (2) proximal junction sagittal Cobb angle of at least 10° greater than the preoperative measurement. The presence of both criteria was necessary to be considered abnormal. Interobserver reliability of this method of measurement has a moderate to high reproducibility [10].
We assessed nine risk factors: sex, age, DEXA score, length of fusion, instrumentation technique, surgical approach, whether or not the patient had thoracoplasty, whether or not the patient had upper instrumented vertebrae, and the postoperative sagittal sacral vertical line difference.
We calculated overall summary statistics in terms of means and SDs for continuous variables and frequencies and percentages for categorical. After the descriptive analysis, we performed univariate comparisons for the independent associations between potential risk factors and the development of PJK. We evaluated group differences between those that developed PJK and those that did not using independent sample t-tests for continuous variables. We evaluated group differences for discrete variables using chi square or Fisher’s exact test. To assess the magnitude of the association, we calculated unadjusted odds ratios and their respective 95% CIs (Table 2). We then created a multivariable binary logistic regression model to evaluate the adjusted associations of each potential explanatory variable to predict the likelihood of development of PJK. To assess the risk factors for development of PJK as time passes, as well as to minimize confounding variables for a time period beyond the followup time, we used a Cox proportional-hazards regression model to estimate hazard ratios and their 95% CIs. For both regression models, we considered variables with a univariate significance level of 0.25 or less, or variables that we thought were clinically relevant to be eligible for inclusion in the analysis. Using a forward stepwise procedure, we removed variables that failed to achieve a p value of 0.15 or less from the final model. Due to the explanatory nature of this analyses, we chose p = 0.15 as the threshold for retention in the final model. For all regression models, we reported the adjusted odds or hazard ratios and their subsequent 95% CIs. We performed all analyses using SPSS® version 18.0 (SPSS®, an IBM® Company, Chicago, IL, USA).
Table 2.
Univariate predictors of PJK after segmental spinal instrumentation and fusion
| Variable | Mean (SD) or number (%) | Odds ratio (95% CI) | p value | |
|---|---|---|---|---|
| No PJK | PJK | |||
| Total number of patients | 207 | 42 | ||
| Female | 175 (84.5%) | 39 (92.9%) | 2.38 (0.69, 8.16) | 0.223 |
| Mean age (years) | 34 (19) | 42 (20) | 0.011 | |
| < 18 years | 81 (39.5%) | 10 (23.8%) | Reference | |
| 19–29 years* | 16 (7.8%) | 4 (9.5%) | 2.03 (0.56, 7.27) | 0.276 |
| 30–39 years | 22 (10.7%) | 3 (7.1%) | 1.11 (0.28, 4.36) | > 0.999 |
| 40–49 years | 36 (17.6%) | 6 (14.3%) | 1.35 (0.46, 4.00) | 0.587 |
| > 50 years | 50 (24.4%) | 19 (45.2%) | 3.08 (1.33, 7.15) | 0.007 |
| Bone quality | ||||
| Normal | 137 (66.2%) | 19 (45.2%) | 2.37 (1.21, 4.64) | 0.011 |
| Osteopenia/osteoporosis | 70 (33.8%) | 23 (54.8%) | ||
| Fusion to S1 | 39 (18.8%) | 18 (42.9%) | 3.23 (1.60, 6.53) | 0.001 |
| Thoracoplasty | 65 (31.4%) | 10 (23.8%) | 0.68 (0.32, 1.47) | 0.328 |
| Surgical approach | ||||
| Anterior or posterior only | 144 (30.4%) | 17 (40.5%) | 3.36 (1.70, 6.66) | < 0.001 |
| Anterior-posterior | 63 (30.4%) | 25 (59.5%) | ||
| Instrumentation technique | ||||
| Hook/hybrid | 153 (74.6%) | 29 (69.0%) | Reference | |
| Pedicle screw | 32 (15.6%) | 8 (19.0%) | 1.32 (0.55, 3.15) | 0.532 |
| Vertebral body screws (anterior) | 20 (9.8%) | 5 (11.9%) | 1.32 (0.46, 3.80) | 0.607 |
| Upper instrumented level* | 175 (84.5%) | 39 (92.9%) | 2.38 (0.69, 8.16) | 0.223 |
| T1 to T3 | ||||
| T4 to T12 | ||||
| Levels fused | 10.56 (3.09) | 11.05 (3.31) | 0.358 | |
| PJK angle | 1.14° (5.00°) | 14.29° (6.92°) | < 0.001 | |
| SSVL difference (mm) | −1.03 (38.93) | −20.98 (44.12) | 0.004 | |
| SRS score difference | 3.75 (0.53) | 3.63 (0.54) | 0.196 | |
* For sum discrepancies, refer to Table 1 for excluded data; PJK = proximal junction kyphosis; SSVL = sacral sagittal vertical line difference between pre- and immediate postoperative time; SRS = Scoliosis Research Society.
Results
Of the 249 patients reviewed, the incidence of PJK was 42 of 249 (17%) patients (Table 2). Our data suggest there are many risk factors associated with PJK, including age of more than 50 years, osteopenia and osteoporosis, distal fusion to S1, surgical approach, and SSVL difference (Table 2).
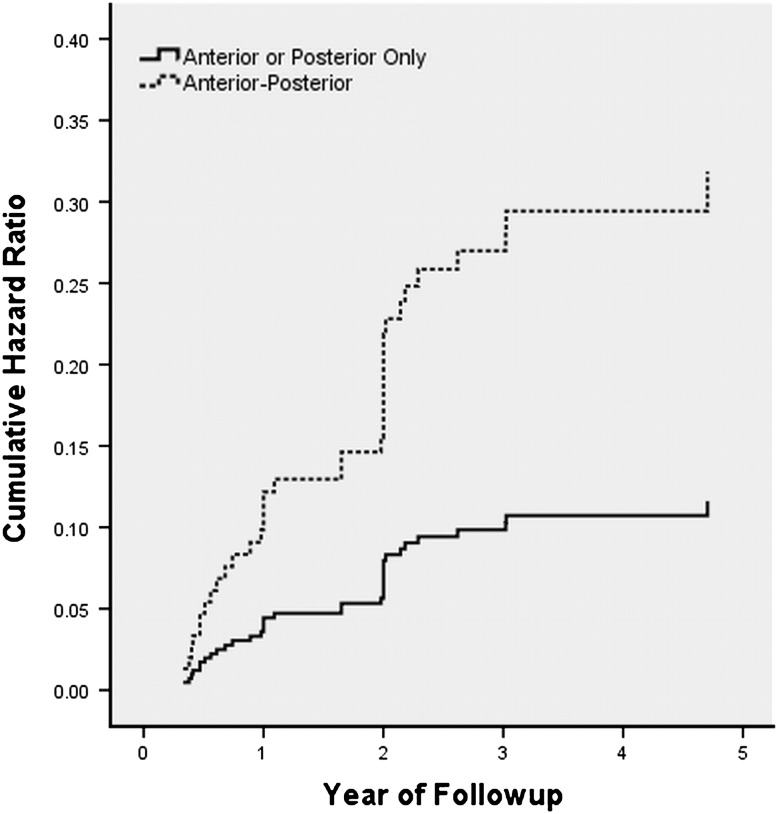
However, in our multivariate analysis, we found only two risk factors were independently associated with the development of PJK (Table 3). An anterior-posterior approach (odds ratio = 3.13; 95% CI = 1.08, 9.05) and UIV (odds ratio = 2.34; 95% CI = 1.07, 5.12) were the most significant independent risk factors for development of PJK (Table 3). Interestingly, osteopenia and osteoporosis, sex, age, and fusion to S1 were not independent risk factors identified in out multivariate analysis. The UIV (Fig. 1) and anterior-posterior approach (Fig. 2) predicted developing PJK in our hazard model. Subjects who had a UIV to T1 through T3 were almost twice as likely to develop a PJK compared to those who did not. Patients who underwent the anterior-posterior approach were three times more likely to develop a PJK. A greater difference in SSVL resulted in a minimal decrease in hazard risk (Table 4). We found no association (p = 0.25) between SSVL difference and surgical approach.
Table 3.
Unadjusted and adjusted odds ratios for PJK following segmental spinal instrumentation and fusion
| Variable | Unadjusted odds ratio (95% CI) | p value | Adjusted odds ratio (95% CI) | p value |
|---|---|---|---|---|
| Female | 2.38 (0.69, 8.16) | 0.223 | 2.53 (0.67, 9.65) | 0.173 |
| Age | 1.02 (1.01, 1.04) | 0.013 | 0.99 (0.95, 1.03) | 0.582 |
| Osteopenia/osteoporosis | 2.37 (1.21, 4.64) | 0.011 | 1.75 (0.68, 4.46) | 0.244 |
| Upper instrumented level (T1-T3) | 2.38 (0.69, 8.16) | 0.223 | 2.34 (1.07, 5.12) | 0.034* |
| Anterior-posterior approach | 3.36 (1.70, 6.66) | 0.001 | 3.13 (1.08, 9.05) | 0.035* |
| Fusion to S1 | 3.23 (1.60, 6.53) | 0.001 | 1.52 (0.55, 4.16) | 0.419 |
| SSVL difference (mm) | 0.99 (0.98, 1.00) | 0.006 | 0.99 (0.98, 1.00) | 0.004* |
* Variable retained in final model; PJK = proximal junctional kyphosis; SSVL = sacral sagittal vertical line.
Fig. 2.
The graph shows a cumulative hazard plot for development of PJK with stratification based on surgical approach. In this model, those with anterior-posterior combined surgery are approximately three times more likely to develop PJK at 2 years after surgery than those who received only posterior surgery.
Table 4.
Hazard ratio for PJK after segmental spinal instrumentation and fusion
| Variable | Hazard ratio (95% CI) | p value |
|---|---|---|
| Female | 2.36 (0.72, 7.81) | 0.159 |
| Osteopenia/osteoporosis | 1.86 (0.98, 3.55) | 0.058 |
| Upper instrumented level (T1-T3) | 1.98 (1.05, 3.72) | 0.034 |
| Anterior-posterior approach | 3.04 (1.56, 5.93) | 0.001 |
| SSVL difference (mm) | 0.99 (0.98, 1.00) | 0.001 |
PJK = proximal junction kyphosis; SSVL = sacral sagittal vertical line.
Discussion
Risk factors for developing PJK include long, rigid, fusion constructs [2, 5], integrity of the posterior soft tissue tension band [2], instrumentation techniques [3, 7], magnitude of sagittal balance correction, and bone quality [12]. Some postulate PJK has a multifactorial etiology related to surgical and patient factors [2, 7, 12, 13]. However, the relative risks of these various factors have never been quantified. Our data suggest a combined anterior-posterior approach and a UIV from T1 through T3 increases the risk of developing PJK by three and two times, respectively. Additionally, our survival analysis, by way of the Cox proportional-hazards model, reveals only UIV (Fig. 2) and the anterior-posterior approach (Fig. 1) to be associated with an increased risk for developing PJK. These risk factors are also associated with an increased risk over time.
We recognize limitations of our study. First, our retrospective study design precludes us from making any strong conclusions based on the independent risk factors we identified. However, our Cox proportional-hazards model was based on our multivariate analysis for a relatively large series of patients, and in the surgical literature, this is often the most feasible method for risk factor identification and quantification because randomized controlled trials are often not possible. Second, the incidence for PJK in our series is limited to patients with idiopathic scoliosis. PJK is a complication that can occur in all types of spine pathology after undergoing multiple level fusions; therefore, we cannot report our incidence as an accurate assessment for all spine surgeries. Our incidence of 17% is similar to the ranges of 10% to 40% reported in the literature [2–8, 10–13], which address adult [2, 5, 12] and adolescent [3, 4, 6, 7] populations (Table 5). To our knowledge, there are no studies available in the literature that address the comparison between PJK in degenerative versus deformity conditions.
Table 5.
Risk factors identified in other studies on PJK
| Study | Year of publication | Study population | Total number of patients | PJK incidence | Risk factor |
|---|---|---|---|---|---|
| Glattes et al. [2] | 2005 | Adults | 81 | 26% | T3 UIV |
| Hollenbeck et al. [4] | 2008 | Adolescents | 174 | 9% | None |
| Kim et al. [5] | 2008 | Adults | 161 | 39% | Age > 55 years, combined anterior-posterior surgery |
| Kim et al. [6] | 2005 | Adolescents | 193 | 26% | Thoracoplasty, preoperative thoracic hyperkyphosis (T5-T12 > 40), hybrid instrumentation |
| Kim et al. [7] | 2007 | Adolescents | 410 | 27% | Male, thoracoplasty, preoperative thoracic hyperkyphosis (T5-T12 > 40) |
| Wang et al. [11] | 2010 | Adolescents | 150 | 28% | Fusion below L2, use of pedicle screw at top of construct, thoracoplasty |
| Yagi et al. [12] | 2011 | Adults | 157 | 20% | Fusion to S1, posterior segmental instrumentation, abnormal global sagittal alignment, CSVL correction > 5 cm |
PJK = proximal junction kyphosis; UIV = upper instrumented vertebrae; CSVL = center sacral vertical line.
Many studies identify risk factors associated with PJK (Table 5). In our study, we identified multiple factors, including age of greater than 50 years, poor bone quality, distal fusion to S1, surgical approach, and SSVL difference (Table 2). However, many of these factors were not independently associated with PJK. This is a particularly important finding because other studies do not perform multivariate analyses on their data, and it is possible there are confounding variables inherent to the risk factors. The explanation for this may be the relationship that many of the risk factors have with each other, such as SSVL difference and distal fusion to S1. One can argue a greater correction in sagittal imbalance is achieved with a distal fusion level incorporating the sacrum and pelvis. Similarly, combined anterior-posterior fusion may be associated with a greater SSVL because of the anterior release, allowing for greater correction. The same can be said for bone quality and age. Due to these inherent relationships between the variables, relying on univariate analysis may lead to significant associations that do not exist once confounding variables are isolated. Although we identified five variables associated with PJK, multivariate analysis revealed only three risk factors to be independently related to PJK, and furthermore, only two risk factors led to a significant quantitative risk for developing PJK in the predictive model. To date, there is no study that provides a quantitative risk for PJK development based on independent variables. Specifically identified in our Cox proportional-hazards model were surgical approach and large SSVL difference as independent risk factors for the development of PJK (Table 4). Combined anterior-posterior spine surgeries reportedly allow a greater correction in the sagittal plane; therefore, SSVL and surgical approach are inherently related [9]. However, we do not find this in our data analysis, suggesting surgical approach and SSVL difference were independently involved in the increased PJK risk in our patients. It is unclear why combined anterior-posterior surgery leads to an increased risk for PJK independent of SSVL. Intuitively, these risk factors can lead to increased stress concentrations at the proximal end of the fusion and theoretically increase the risk for developing PJK [5, 11]. A recent study also identified combined anterior-posterior spine surgery affecting PJK development [5], but this finding has not been uniform in studies assessing risk factors for PJK development [11, 12].
Our findings suggest uncertainty in the etiology of PJK. Various studies have proposed the development of PJK is related to a combination of patient- and surgery-related factors [2–8, 10–13]. Of these, the integrity of the soft tissue tension band [2], rigidity of the construct (stress concentration) [5], bone quality [12], instrumentation type [3], and amount of sagittal plane correction [5, 11, 12] are all implicated as contributing to PJK development. Although this may be true, our analysis suggests only surgical approach, UIV, and SSVL are independently associated with PJK development. While we identified risk factors similar to those in the literature, they did not independently predict PJK. It remains unclear whether PJK results from iatrogenic or patient-related causes, but our data suggest those with UIV between T1 and T3, a combined approach, and large SSVL differences should be monitored closely for the development of PJK because they are not only at risk but their risk seems to increase with time.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Asher M, Min Lai S, Burton D, Manna B. The reliability and concurrent validity of the Scoliosis Research Society-22 patient questionnaire for idiopathic scoliosis. Spine (Phila Pa 1976) 2003;28:63–69. doi: 10.1097/00007632-200301010-00015. [DOI] [PubMed] [Google Scholar]
- 2.Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C., 2nd Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 2005;30:1643–1649. doi: 10.1097/01.brs.0000169451.76359.49. [DOI] [PubMed] [Google Scholar]
- 3.Helgeson MD, Shah SA, Newton PO, Clements DH, 3rd, Betz RR, Marks MC, Bastrom T, Harms Study Group Evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Spine (Phila Pa 1976) 2010;35:177–181. doi: 10.1097/BRS.0b013e3181c77f8c. [DOI] [PubMed] [Google Scholar]
- 4.Hollenbeck SM, Glattes RC, Asher MA, Lai SM, Burton DC. The prevalence of increased proximal junctional flexion following posterior instrumentation and arthrodesis for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2008;33:1675–1681. doi: 10.1097/BRS.0b013e31817b5bea. [DOI] [PubMed] [Google Scholar]
- 5.Kim YJ, Bridwell KH, Lenke LG, Glattes CR, Rhim S, Cheh G. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976) 2008;30:2179–2184. doi: 10.1097/BRS.0b013e31817c0428. [DOI] [PubMed] [Google Scholar]
- 6.Kim YJ, Bridwell KH, Lenke LG, Kim J, Cho SK. Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976) 2005;30:2045–2050. doi: 10.1097/01.brs.0000179084.45839.ad. [DOI] [PubMed] [Google Scholar]
- 7.Kim YJ, Lenke LG, Bridwell KH, Kim J, Cho SK, Cheh G, Yoon J. Proximal junctional kyphosis in adolescent idiopathic scoliosis after three different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine (Phila Pa 1976) 2007;32:2731–2738. doi: 10.1097/BRS.0b013e31815a7ead. [DOI] [PubMed] [Google Scholar]
- 8.Lee GA, Betz RR, Clements DH, III, Huss GK. Proximal kyphosis after posterior spinal fusion in patients with idiopathic scoliosis. Spine (Phila Pa) 1999;24:795–799. doi: 10.1097/00007632-199904150-00011. [DOI] [PubMed] [Google Scholar]
- 9.Lonner BS, Newton P, Betz R, Scharf C, O’Brien M, Sponseller P, Lenke L, Crawford A, Lowe T, Letko L, Harms J, Shufflebarger H. Operative management of Scheuermann’s kyphosis in 78 patients: radiographic outcomes, complications, and technique. Spine (Phila Pa 1976) 2007;32:2644–2652. doi: 10.1097/BRS.0b013e31815a5238. [DOI] [PubMed] [Google Scholar]
- 10.Sacramento-Dominguez C, Vayas-Diez R, Coll-Mesa L, Parrilla AP, Machado-Calvo M, Pinilla JA, Sosa AJ, Lopez Gde L. Reproducibility measuring the angle of proximal junctional kyphosis using the first or the second vertebra above the upper instrumented vertebrae in patients surgically treated for scoliosis. Spine (Phila Pa 1976) 2009;34:2787–2791. doi: 10.1097/BRS.0b013e3181b61955. [DOI] [PubMed] [Google Scholar]
- 11.Wang J, Zhao Y, Shen B, Wang C, Li M. Risk factor analysis of proximal junctional kyphosis after posterior fusion in patients with idiopathic scoliosis. Injury. 2010;41:415–420. doi: 10.1016/j.injury.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 12.Yagi M, Akilah KB, Boachie-Adjei O. Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine (Phila Pa 1976) 2011;36:E60–E68. doi: 10.1097/BRS.0b013e3181eeaee2. [DOI] [PubMed] [Google Scholar]
- 13.Yang SH, Chen PQ. Proximal kyphosis after short posterior fusion for thoracolumbar scoliosis. Clin Orthop Relat Res. 2003;411:152–158. doi: 10.1097/01.blo.0000069885.72909.bb. [DOI] [PubMed] [Google Scholar]