Abstract
Background
Batter’s shoulder has been defined as posterior subluxation of the lead shoulder during the baseball swing. However, it is unclear whether or how frequently patients may return to play after treatment of this uncommon condition.
Questions/purposes
We therefore determined the rate of return to play after operative treatment for Batter’s shoulder and whether ROM was restored.
Methods
We retrospectively reviewed the records of 14 baseball players diagnosed with Batter’s shoulder. Four played professionally, six were in college, and four were in varsity high school. The average age was 20.3 years (range, 16–33 years). All had physical examinations and MRI findings consistent with posterior labral tears involving the lead shoulder. Treatment involved arthroscopic posterior labral repair (n = 10), débridement (n = 2), or rehabilitation (n = 2). The minimum followup was 18 months (average, 2.8 years; range, 18–64 months).
Results
Eleven of 12 surgically treated patients returned to their previous level of batting at an average of 5.9 months after surgery. The one patient who was unable to return to play also had an osteochondral lesion of the glenoid identified at surgery. Players typically returned to hitting off a tee at 3 months and to facing live pitching at 6 months postoperatively. All patients regained full internal and external ROM as compared with preoperative data.
Conclusions
Batter’s shoulder is an uncommon form of posterior instability in hitters affecting their lead shoulder. Most athletes are able to return to play at the same level after arthroscopic treatment of posterior capsulolabral lesions.
Level of Evidence
Level IV, case series. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Batter’s shoulder, posterior instability leading to episodic subluxation of the lead shoulder during the baseball swing [10], is an uncommon but often disabling type of posterior instability in baseball players. Subluxation in this scenario is an incomplete dislocation event that spontaneously reduces. Posterior shoulder instability is typically the result of a posteriorly directed load to the shoulder in a position of forward flexion, adduction, and internal rotation [3]. Posterior shoulder instability, including dislocation and subluxation, occurs much less frequently than anterior instability, accounting for only 2% to 12% of patients with shoulder instability [2]. The role of posterior shoulder instability as a cause of disability in the athletic population has become increasingly recognized [5, 12, 15].
Posterior instability in the athletic population more commonly arises from contact sports such as football and rugby and occurs from acute trauma [12, 15] or repetitive microtrauma [20]. In the case of batter’s shoulder, the major rotational forces about the shoulder are believed to be the cause of the instability [19]. Symptoms are often vague with posterior shoulder pain during batting or inability to generate power during the baseball swing [19].
During the four phases of the baseball swing, considerable energy is transferred from the lower extremity and core musculature to the upper body [23]. These forces translate into rotational velocities of 937°/second at the shoulder and 1160°/second at the arms with a resultant linear bat velocity of 31 m/s [26]. The combination of this rotational velocity along with the mass of the bat is believed to be the mechanism of injury in batter’s shoulder [19]. These forces are magnified in the case of a missed pitch as a result of the lack of counterforce to the dynamic posterior pulling force on the lead shoulder during batting [6]. A missed outside pitch may create more substantial injury because this increases the abduction angle of the shoulder and subsequently the shear forces across the glenohumeral joint [19].
Several studies suggest fewer athletes return to play after capsulolabral repair for posterior instability as compared with repair for anterior instability [22, 25]. The rate of return is reportedly lower in throwing athletes (55%) compared with nonthrowing athletes (71%) [22]. One study of surgery for posterior instability in athletes reported a failure rate of 40% [25]. However, it is unclear whether or how frequently patients may return to play after treatment of batter’s shoulder.
We therefore determined the rate of return to play after operative treatment for batter’s shoulder and whether ROM was restored.
Patients and Methods
We retrospectively identified 588 patients using the International Classification of Diseases, 9th Revision [7] code 840.8 for sprain of other specified sites of the shoulder and upper arm for the period from April 2006 to December 2009. There is no specific code for posterior labral tear or posterior instability and 840.8 is typically the code used for these diagnoses. For this observational study we included patients who had a history of unidirectional, posterior instability related to batting. Any patients who may have had a traumatic event from a direct blow to the shoulder or may have had an injury from another sport were excluded. Additionally, we also excluded any patients with other shoulder pathology at the time of evaluation. Applying these criteria, we identified 14 players, all male; nine players were identified from the Kerlan Jobe database, whereas the remaining five were identified from the Hospital for Special Surgery. Four patients played professionally, six at the collegiate level, and four at the varsity level. The average age of the patients was 20.3 years (range, 16–33 years). The lead shoulder, which was also the nondominant shoulder, was involved in all cases. All 14 players identified experienced pain in the lead batting shoulder, which occurred during the batting swing. All patients had localized pain to the posterior shoulder. The minimum followup was 18 months (average, 2.3 years; range, 18–64 months). No patients were lost to followup. All data were obtained from patients’ medical records, with the exception of the latest clinical followup, which was evaluated through a telephone interview.
From the records we extracted demographic data including age, gender, position, level of competition, throwing arm, and length of followup. Clinical evaluation for all patients included assessment of active and passive ROM, strength testing, instability testing, and provocative maneuvers. We performed strength testing using manual muscle testing with a standardized six-point scale with 5 representing normal or full strength and 0 representing the absence of muscle contraction [14]. We examined instability by performing a modified load and shift test in the supine position [24]. The degree of instability was quantified based on the degree of subluxation with Grade 0 indicating no translation, Grade 1+ indicating translation to the glenoid rim, Grade 2+ translation beyond the glenoid rim with spontaneous reduction, and Grade 3+ translation beyond without spontaneous reduction [1]. Other provocative tests included the O’Brien’s test, Apprehension Test, Neer, and Hawkins impingement tests. On physical examination, 12 of 14 patients had a positive O’Brien’s sign, specifically pain elicited with resisted forward elevation with the shoulder positioned in adduction and internal rotation [18]. Seven of 14 had 1+ laxity on examination, and 50% had 2+ laxity on the affected shoulder (Table 1). The unaffected shoulder had Grade 1+ or less translation on examination.
Table 1.
Demographic data and preoperative findings
| Patient number | Age (years) | Level of play | Affected shoulder | Post laxity | Unaffected shoulder | MRI findings |
|---|---|---|---|---|---|---|
| 1 | 22 | Professional | Left | 1+ | 1+ | Post labral tear, reverse Hill Sachs |
| 2 | 16 | High school | Left | 1+ | 0 | Post labral tear |
| 3 | 17 | High school | Left | 1+ | 1+ | Post labral tear, reverse Hill Sachs |
| 4 | 22 | Professional | Left | 2+ | 1+ | Post labral tear |
| 5 | 33 | Professional | Right | 1+ | 0 | Post labral tear |
| Osteochondral defect | ||||||
| 6 | 17 | High school | Right | 1+ | 0 | Post labral tear |
| 7 | 20 | College | Left | 2+ | 1+ | Post labral tear |
| 8 | 19 | College | Left | 2+ | 0 | Post labral tear |
| 9 | 17 | High school | Left | 1+ | 0 | Post labral tear |
| 10 | 20 | College | Right | 1+ | 0 | Post labral tear |
| 11 | 21 | College | Left | 2+ | 1+ | Post labral tear |
| 12 | 24 | Professional | Left | 1+ | 1+ | Post labral tear |
Radiographic evaluation included three views of the shoulder, AP, axillary, and scapular Y. We obtained MR arthrograms for all patients using a shoulder coil with standard sequencing techniques. All 14 patients had MR arthrograms that were read by a musculoskeletal-trained radiologist (SK). Twelve of the 14 had evidence of posterior labral tears. One patient had a negative MRI, whereas the remaining patient had an irregularity in the posteroinferior glenohumeral ligament without an overt tear.
All patients underwent an initial course of nonoperative management. The indications for surgery were: (1) the inability to return to play at the same level; (2) failure to respond to at least 3 months of conservative treatment including cessation of batting and physical therapy; (3) evidence of posterior instability on examination; and (4) radiographic evidence of posterior capsulolabral pathology. The contraindications for surgery were: (1) multidirectional instability; (2) habitual or voluntary subluxation; or (3) osseous abnormalities.
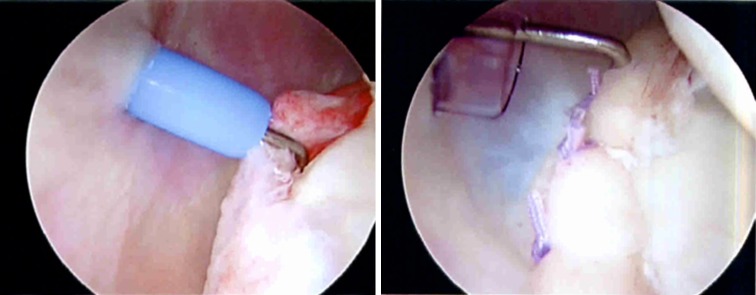
Patients indicated for surgery underwent an examination under anesthesia before the start of the procedure. Surgery was performed in the lateral decubitus position using a beanbag to position the patient. The operative arm was placed in 45° of abduction and 20° of forward flexion with 10 pounds of traction applied. The posterior portal was created slightly inferior to the standard posterior portal. An anterior portal was established within the rotator interval under and was used as the viewing portal in cases requiring capsulolabral repair. When possible, repairs were performed through the posterior portal using a penetrator. In cases in which the desired area could not be reached by the posterior portal, an accessory low posterolateral was created under spinal needle localization [17]. Posterior labral tears were classified based on arthroscopic findings according to the classification of Kim et al. [13] in which a Type I lesion demonstrates incomplete stripping, Type II a marginal crack, Type III chondrolabral erosion, and Type IV a flap tear. Two players had Type I posterior labral tears without detachment. These patients underwent labral débridement only. The remaining 10 players had Type III posterior labral tears with chondral labral disruption. These patients underwent arthroscopic posterior capsulolabral repair with suture anchors (Fig. 1). For the repairs, an average of 2.2 anchors (range, 1–3) was used (Table 2).
Fig. 1.
A probe demonstrating posterior labral tear before and after repair.
Table 2.
Surgical treatment and average time to return to play
| Patient number | Age (years) | Level of play | Treatment | Return to batting | Return to play | Last followup |
|---|---|---|---|---|---|---|
| 1 | 22 | Professional | 3 anchor repair | 5 months | 6 months | 36 months |
| 2 | 16 | High school | Débridement | 6 months | 7 months | 35 months |
| 3 | 17 | High school | 2 anchor repair | 5 months | 6 months | 37 months |
| 4 | 22 | Professional | 2 anchor repair | 6 months | 7 months | 50 months |
| 5 | 33 | Professional | 1 anchor repair | 12 months | No | 64 months |
| Débridement chondral lesion | ||||||
| 6 | 17 | High school | Débridement | 6 months | 7 months | 48 months |
| 7 | 20 | College | 2 anchor repair | 6 months | 7 months | 28 months |
| 8 | 19 | College | 3 anchor repair | 4 months | 6 months | 18 months |
| 9 | 17 | High school | 2 anchor repair | 5 months | 7 months | 24 months |
| 10 | 20 | College | 2 anchor repair | 5 months | 6 months | 25 months |
| 11 | 21 | College | 3 anchor repair | 5 months | 6 months | 20 months |
| 12 | 24 | Professional | 2 anchor repair | 6 months | 7 months | 20 months |
Postoperatively, patients undergoing repair were placed in a sling for 2 weeks and were then started on a physical therapy program focusing on passive ROM for 6 weeks. Active ROM was started thereafter with strengthening delayed until 12 weeks postoperatively. Hitting off a tee was permitted at 12 weeks postoperatively, and players were permitted to take live pitches at 6 months postoperatively.
Patients were seen within 1 week after surgery for removal of stitches. Subsequent followup visits were at 6 weeks, 3 months, 6 months, and 1 year unless patients were not able to return to play at the same level by that time. ROM was assessed at each followup visit, whereas the modified load-shift, O’Brien’s, and apprehension tests were delayed until 3 months postoperatively. Final followup was conducted by telephone interview, and patients were evaluated using a modification of the scale proposed by Conway et al. [8]. Outcomes were evaluated based on whether patients were able to return to the same level of play, a lower level of play, a recreational level of play, or an inability to play.
Results
Eleven of 12 patients undergoing surgery returned to play at the same level at last followup; none of these 11 patients had any other shoulder pathology requiring treatment. The operatively treated payers returned to batting at an average of 5.9 months (range, 4–12 months) postoperatively with an average return to play at 6.5 months (range, 6–7 months) (Table 2). The remaining patient did not return to batting. At the time of surgery, the patient had an osteochondral lesion of the glenoid in addition to a calcification of the posteroinferior glenoid labrum. There were no complications. Two players responded to nonoperative treatment and were the two who had no evidence of posterior labral tears on MRI. These two players were ultimately able to return to play at the same level after 1 month of rehabilitation.
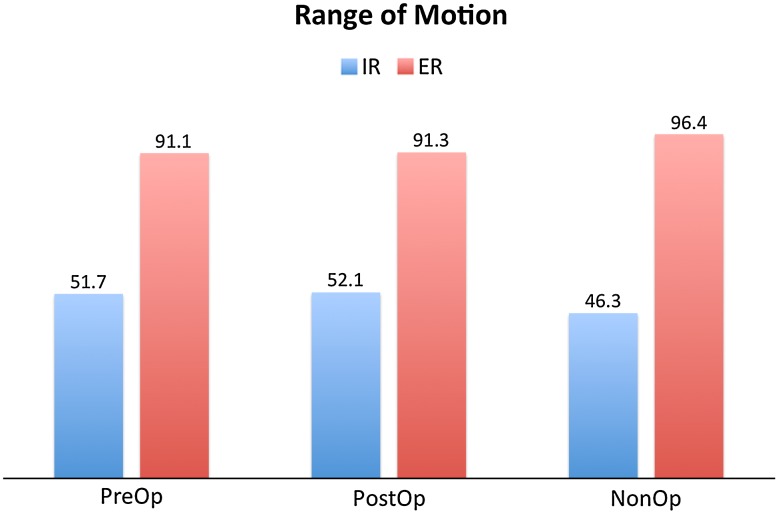
At last followup, all patients had regained full internal and external ROM as compared with preoperative data. The average postoperative external rotation was 91.3° and internal rotation was 52.1° versus the nonoperative arm, which demonstrated average external and internal rotation of 96.4° and 46.3°, respectively (Fig. 2). Shoulder stability was restored to the same degree as the unaffected side in all cases.
Fig. 2.
Average preoperative and postoperative ROM is demonstrated. IR = internal rotation; ER = external rotation.
Discussion
Posterior shoulder instability is an uncommon but disabling condition increasingly recognized in the athletic population. Batter’s shoulder is a recently described type of posterior instability affecting the lead shoulder during the baseball swing [10]. Given the relatively low rate of return to play after surgical treatment of posterior instability, we examined whether players were able to return to the same level of play in this uncommon form of posterior instability and whether the motion was restored.
There are several limitations in this study. First, being a retrospective study, there is the potential for selection bias. However, all identified subjects were included, thus minimizing this potential error. Second, the sample size was small, limiting the power of the study and making it difficult to generalize the rate of return to play we found in our study. Despite the small number, our findings are comparable to other studies. Third, there were also variations in surgery with  of patients undergoing débridement and the remainder undergoing capsulolabral repair. Consequently, this limits the support for any specific surgical technique. Finally, there were no validated outcome scores used. We relied on a modified Conway scale, which has been used in other peer-reviewed articles as an objective measure of outcome based on the rate and duration of return to play [4, 8, 9].
of patients undergoing débridement and the remainder undergoing capsulolabral repair. Consequently, this limits the support for any specific surgical technique. Finally, there were no validated outcome scores used. We relied on a modified Conway scale, which has been used in other peer-reviewed articles as an objective measure of outcome based on the rate and duration of return to play [4, 8, 9].
In our series, 11 of 12 patients undergoing surgical management were able to return to play at the same level at a minimum followup of 18 months with only one patient unable to return to play at any level. The findings in our series are similar to those reported in the literature for arthroscopic treatment of posterior instability. The overall rate of return to play at the same level in the literature ranges from 75% to 91% [5, 13, 20, 27, 28]. When the subset of overhead athletes is examined, the success rate is substantially lower. In one of the few studies focusing on overhead athletes, we found only 55% of throwers undergoing arthroscopic posterior stabilization were able to return to the same level of play [22]. Fortunately, in the case of batter’s shoulder, the lead shoulder is typically the nondominant arm except in the case of switch hitters. Thus, the throwing arm is typically unaffected and allows for a quicker return to play and is likely the reason why the rate of return is higher in our series than reported for overhead athletes [22].
Although shoulder stability was restored to the same level as the contralateral shoulder in all cases, this did not correlate with clinical outcome. Furthermore, three of 12 players did not demonstrate a clinically detectable difference in posterior stability before surgery. In the setting of batter’s shoulder, most patients do not have overt posterior instability, but rather pain resulting from labral pathology and subclinical instability. As such, clinical assessments of shoulder stability are not as important as overall functional improvement.
One of the difficulties in evaluating and comparing the outcomes of posterior instability is the variability of surgical techniques used. Techniques include débridement, capsular plication, and chondrolabral repair. The trend has been to move toward chondrolabral repair with suture anchors, which is our preferred method of treatment [21]. The poor quality of the posterior capsule makes it difficult to achieve adequate repair with suture plication alone. This may be another reason why the outcomes of posterior stabilization have been inferior to anterior stabilization.
On examination, 12 of 14 players had a positive O’Brien’s or active compression test. O’Brien’s test was classically described for the diagnosis of SLAP tears [18], but recent studies suggest it is useful for identifying labral pathology in general in conjunction with other provocative tests [11, 16]. O’Brien’s test is believed to produce pain by applying tension across the biceps labral complex and by tensioning the capsule again an unstable labrum [18]. Internal rotation of the shoulder preferentially tightens the posterior capsular applying pressure to the posterior labrum, which may explain the high rate of positive O’Brien’s test in our series.
Although the exact mechanism of injury in batter’s shoulder is unknown, the condition is believed to be the result of repetitive microtrauma, which is greatest with a missed, outside pitch. During a missed pitch, it is presumed there is no counterforce to the momentum from the baseball swing leading to overdynamics in the shoulder and an excessive pulling force [10]. In a preliminary study, Philips et al. [19] found an average shoulder abduction angle of 105° for outside pitches versus 90° for inside pitches. The American Sports Medicine Institute (ASMI) group suggested the increased shoulder abduction angle may increase shear forces across the joint [10]. There has also been a trend toward one-handed follow-through during the baseball swing, which has also been presumed to increase the microtrauma across the posterior labrum and capsule.
Batter’s shoulder is a unique form of posterior shoulder instability believed to be the result of repetitive microtrauma on the posterior capsulolabral complex during the follow-through phase of batting. In our limited series, 11 of 12 patients undergoing surgical treatment of batter’s shoulder were able to return to play at the same level at an average of 6.5 months. Larger, prospective studies are needed to corroborate these preliminary findings.
Acknowledgments
We thank Drs David M. Dines and Ralph A. Gambradella for allowing us to include their patients in this study. We thank Dr Scott Kingston for his help in reviewing the radiographic studies.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the reporting of this investigation and that all investigations were conducted in conformity with ethical principles of research.
This study was conducted at the Kerlan Jobe Orthopaedic Clinic, Los Angeles, CA, USA and the Hospital for Special Surgery, New York, NY, USA.
References
- 1.Altchek DW, Warren RF, Skyhar MJ, Ortiz G. T-plasty modification of the Bankart procedure for multidirectional instability of the anterior and inferior types. J Bone Joint Surg Am. 1991;73:105–112. [PubMed] [Google Scholar]
- 2.Antoniou J, Harryman DT., 2nd Posterior instability. Orthop Clin North Am. 2001;32:463–473. doi: 10.1016/S0030-5898(05)70215-7. [DOI] [PubMed] [Google Scholar]
- 3.Bottoni CR, Franks BR, Moore JH, DeBerardino TM, Taylor DC, Arciero RA. Operative stabilization of posterior shoulder instability. Am J Sports Med. 2005;33:996–1002. doi: 10.1177/0363546504271509. [DOI] [PubMed] [Google Scholar]
- 4.Bowers AL, Dines JS, Dines DM, Altchek DW. Elbow medial ulnar collateral ligament reconstruction: clinical relevance and the docking technique. J Shoulder Elbow Surg. 2010;19:110–117. doi: 10.1016/j.jse.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 5.Bradley JP, Baker CL, 3rd, Kline AJ, Armfield DR, Chhabra A. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 100 shoulders. Am J Sports Med. 2006;34:1061–1071. doi: 10.1177/0363546505285585. [DOI] [PubMed] [Google Scholar]
- 6.Bradley JP, Tejwani SG. Arthroscopic management of posterior instability. Orthop Clin North Am. 2010;41:339–356. doi: 10.1016/j.ocl.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 7.Buck CJ, American Medical Association. 2011 ICD-9-CM, Volumes 1 & 2 for Physicians. St Louis, MO, Chicago, IL, USA: Elsevier/Saunders; American Medical Association; 2011.
- 8.Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992;74:67–83. [PubMed] [Google Scholar]
- 9.Dines JS, ElAttrache NS, Conway JE, Smith W, Ahmad CS. Clinical outcomes of the DANE TJ technique to treat ulnar collateral ligament insufficiency of the elbow. Am J Sports Med. 2007;35:2039–2044. doi: 10.1177/0363546507305802. [DOI] [PubMed] [Google Scholar]
- 10.Fleisig GS, Dun S, Kingsley D. Biomechanics of the shoulder during sports. In: Wilk KE, Reinold MM, Andrews JR, editors. The Athlete’s Shoulder. Philadelphia, PA, USA: Churchill Livingstone; 2009. p. 380. [Google Scholar]
- 11.Guanche CA, Jones DC. Clinical testing for tears of the glenoid labrum. Arthroscopy. 2003;19:517–523. doi: 10.1053/jars.2003.50104. [DOI] [PubMed] [Google Scholar]
- 12.Kaplan LD, Flanigan DC, Norwig J, Jost P, Bradley J. Prevalence and variance of shoulder injuries in elite collegiate football players. Am J Sports Med. 2005;33:1142–1146. doi: 10.1177/0363546505274718. [DOI] [PubMed] [Google Scholar]
- 13.Kim SH, Ha KI, Park JH, Kim YM, Lee YS, Lee JY, Yoo JC. Arthroscopic posterior labral repair and capsular shift for traumatic unidirectional recurrent posterior subluxation of the shoulder. J Bone Joint Surg Am. 2003;85:1479–1487. doi: 10.1302/0301-620X.85B2.13289. [DOI] [PubMed] [Google Scholar]
- 14.Lovett RW, Martin EG. Certain aspects of infantile paralysis (with a descrition of a method of muscle testing) JAMA. 1916;66:729–733. doi: 10.1001/jama.1916.02580360031009. [DOI] [Google Scholar]
- 15.Mair SD, Zarzour RH, Speer KP. Posterior labral injury in contact athletes. Am J Sports Med. 1998;26:753–758. doi: 10.1177/03635465980260060301. [DOI] [PubMed] [Google Scholar]
- 16.Meserve BB, Cleland JA, Boucher TR. A meta-analysis examining clinical test utility for assessing superior labral anterior posterior lesions. Am J Sports Med. 2009;37:2252–2258. doi: 10.1177/0363546508325153. [DOI] [PubMed] [Google Scholar]
- 17.Nord KD, Brady PC, Yazdani RS, Burkhart SS. The anatomy and function of the low posterolateral portal in addressing posterior labral pathology. Arthroscopy. 2007;23:999–1005. doi: 10.1016/j.arthro.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 18.O’Brien SJ, Pagnani MJ, Fealy S, McGlynn SR, Wilson JB. The active compression test: a new and effective test for diagnosing labral tears and acromioclavicular joint abnormality. Am J Sports Med. 1998;26:610–613. doi: 10.1177/03635465980260050201. [DOI] [PubMed] [Google Scholar]
- 19.Philips BB, Andrews JR, Fleisig GS. Batter’s Shoulder: Posterior Instability of the Lead Shoulder, A Biomechanical Evaluation. Birmingham, AL, USA: Alabama Sports Medicine and Orthopaedic Center; 2000. [Google Scholar]
- 20.Provencher MT, Bell SJ, Menzel KA, Mologne TS. Arthroscopic treatment of posterior shoulder instability: results in 33 patients. Am J Sports Med. 2005;33:1463–1471. doi: 10.1177/0363546505278301. [DOI] [PubMed] [Google Scholar]
- 21.Provencher MT, Leclere LE, King S, Frank RM, Mologne TS, Ghodadra NS, Romeo AA. Posterior instability of the shoulder: diagnosis and management. Am J Sports Med. 2011;39:874–886. doi: 10.1177/0363546510384232. [DOI] [PubMed] [Google Scholar]
- 22.Radkowski CA, Chhabra A, Baker CL, Tejwani SG, Bradley JP. Arthroscopic capsulolabral repair for posterior shoulder instability in throwing athletes compared with nonthrowing athletes. Am J Sports Med. 2008;36:693–699. doi: 10.1177/0363546508314426. [DOI] [PubMed] [Google Scholar]
- 23.Shaffer B, Jobe FW, Pink M, Perry J. Baseball batting. An electromyographic study. Clin Orthop Relat Res. 1993;292:285–293. [PubMed] [Google Scholar]
- 24.Silliman JF, Hawkins RJ. Classification and physical diagnosis of instability of the shoulder. Clin Orthop Relat Res. 1993;291:7–19. [PubMed] [Google Scholar]
- 25.Tibone JE, Bradley JP. The treatment of posterior subluxation in athletes. Clin Orthop Relat Res. 1993;291:124–137. [PubMed] [Google Scholar]
- 26.Welch CM, Banks SA, Cook FF, Draovitch P. Hitting a baseball: a biomechanical description. J Orthop Sports Phys Ther. 1995;22:193–201. doi: 10.2519/jospt.1995.22.5.193. [DOI] [PubMed] [Google Scholar]
- 27.Williams RJ, 3rd, Strickland S, Cohen M, Altchek DW, Warren RF. Arthroscopic repair for traumatic posterior shoulder instability. Am J Sports Med. 2003;31:203–209. doi: 10.1177/03635465030310020801. [DOI] [PubMed] [Google Scholar]
- 28.Wolf EM, Eakin CL. Arthroscopic capsular plication for posterior shoulder instability. Arthroscopy. 1998;14:153–163. doi: 10.1016/S0749-8063(98)70034-9. [DOI] [PubMed] [Google Scholar]