Abstract
Background
Repetitive overhead throwing motion causes motion adaptations at the glenohumeral joint that cause injury, decrease performance, and affect throwing mechanics. It is essential to define the typical range of motion (ROM) exhibited at the glenohumeral joint in the overhead thrower.
Questions/purposes
We (1) assessed the glenohumeral joint passive range of motion (PROM) characteristics in professional baseball pitchers; and (2) applied these findings clinically in a treatment program to restore normal PROM and assist in injury prevention.
Methods
From 2005 to 2010, we evaluated 369 professional baseball pitchers to assess ROM parameters, including bilateral passive shoulder external rotation (ER) at 45° of abduction, external and internal rotation (IR) at 90° abduction while in the scapular plane, and supine horizontal adduction.
Results
The mean ER was greater for the throwing and nonthrowing shoulders at 45° of abduction, 102° and 98°, respectively. The throwing shoulder ER at 90° of abduction was 132° compared with 127° on the nonthrowing shoulder. Also, the pitcher’s dominant IR PROM was 52° compared with 63° on the nondominant side. We found no statistically significant differences in total rotational motion between the sides.
Conclusions
Although we found side-to-side differences for rotational ROM and horizontal adduction, the total rotational ROM was similar.
Clinical Relevance
The clinician can use these PROM values, assessment techniques, and treatment guidelines to accurately examine and develop a treatment program for the overhead-throwing athlete.
Introduction
The throwing shoulder, especially in baseball pitchers, consistently demands considerable attention in the orthopaedic and sports medicine community because of the frequency with which it is injured [1, 2, 6, 17, 18, 21, 34, 36]. The pitcher exhibits unique ROM characteristics, which are often important to consider when evaluating and treating the thrower’s shoulder. Thus, the clinical and rehabilitation specialist should have an accurate understanding of the typical variations in motion and strength within the overhead thrower to prevent, evaluate, or treat the athlete.
The shoulder is frequently injured in the overhead-throwing athlete. Conte et al. [10] reported that 28% of all injuries sustained to professional baseball pitchers occur within the shoulder. McFarland and Wasik [23] reported that upper extremity injuries in collegiate baseball players accounted for 75% of the time lost from the sport as a result of injury. In fact, the pitcher was the most commonly injured position (69%), and rotator cuff tendonitis was the most common type of reported injury. Several investigations have documented that shoulder injuries are more common in pitchers than position players [10, 23].
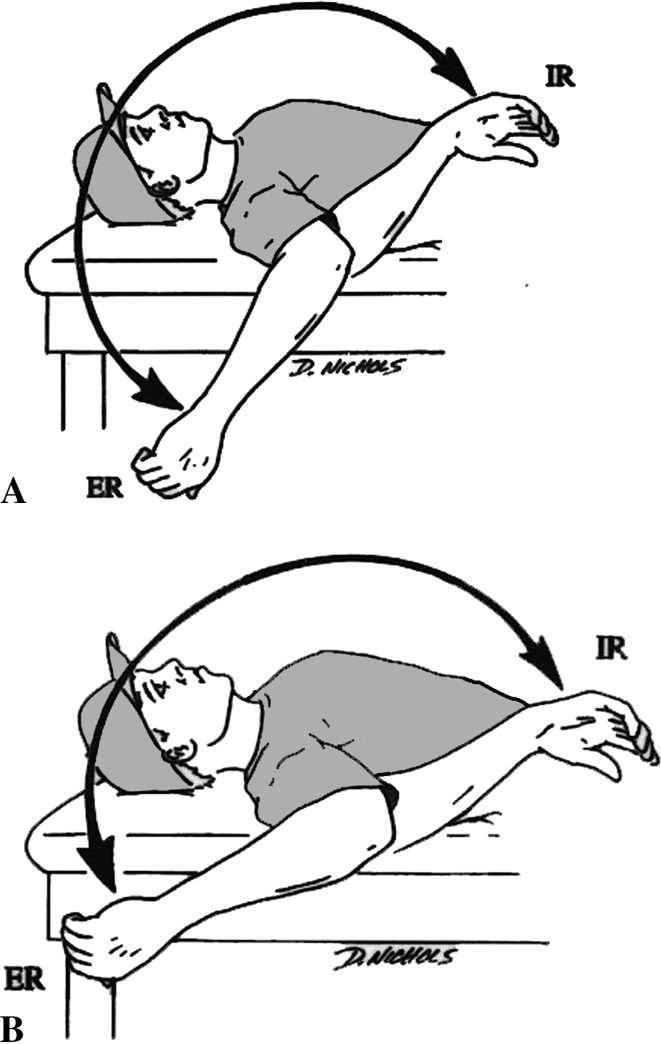
Numerous authors have documented a difference between internal rotation (IR) motion of the throwing and nonthrowing shoulders in throwing athletes [6, 8, 12, 15, 31] (Table 1). This disparity in internal rotation (IR) of the throwing shoulder when compared with the nonthrowing side has been referred to as glenohumeral joint internal rotation deficit (GIRD) [8]. GIRD, as defined by Burkhart et al. [7], occurs when there is a 20° or greater loss in IR measurements when the throwing shoulder is compared with the nonthrowing shoulder. Some clinicians [12, 24, 35] have suggested GIRD as a cause of specific shoulder injuries in throwing athletes. Wilk et al. [36] proposed the total rotational motion (TRM) concept of glenohumeral mobility in the throwing shoulder in which the amount of external rotation (ER) and IR measured at 90° of abduction are added together to calculate a total rotational arc of motion (Fig. 1). The authors reported that the TRM in the throwing shoulders of professional baseball pitchers should be within 5° of the nonthrowing shoulder, and a TRM arc greater than 5° may be a contributing factor to shoulder injuries in throwers [35, 36].
Table 1.
Literature review on ROM characteristics in the overhead athlete
| Author | Mean glenohumeral external rotation at 90° abduction dominant shoulder | Mean glenohumeral internal rotation at 90° abduction dominant shoulder | Total rotational motion (TRM) dominant shoulder | Mean glenohumeral external rotation at 90° abduction nondominant shoulder | Mean glenohumeral internal rotation at 90° abduction nondominant shoulder | Total rotational motion (TRM) nondominant shoulder | Conclusion |
|---|---|---|---|---|---|---|---|
| Borsa et al. [4] | 135.5° ± 9.5° | 59.7° ± 7.0° | 195.2° ± 12.1° | 130.4° ± 10.7° | 68.2° ± 8.6° | 198.6° ± 26.6° | External rotation was found to be significantly increased and internal rotation was found to be significantly decreased in a pitcher’s dominant shoulder |
| Borsa et al. [5] | 134.8° ± 10.2° | 68.6° ± 9.2° | 203.4° ± 9.7° | 125.8° ± 8.7° | 78.3° ± 10.6° | 204.1° ± 9.7° | There is no correlation between glenohumeral translation and passive internal and external rotation in a thrower’s shoulder |
| Chant et al. [9] | 114° ± 9.8° | 57.1° ± 8.7° | 171.1° ± 12.5° | 104.1° ± 7.4° | 73.5° ± 9.6° | 177.6° ± 11.0° | The increased external rotation and decreased internal rotation in baseball player’s dominant shoulder can be explained by both soft tissue changes and increased humeral retroversion |
| Crockett et al. [11] | 128° ± 9.2° | 62° ± 7.4° | 189° ± 12.6° | 119° ± 7.2° | 71° ± 9.3° | 189° ± 12.7° | There is a correlation between increased external rotation and decreased internal rotation in a thrower’s dominant shoulder and humeral retroversion |
| Dwelly et al. [14] | Pre-fall: 96.2° ± 12.7° Pre-spring: 104° ± 17.0° Post-spring: 106.9° ± 19.9° |
Pre-fall: 45.5° ± 11.1° Pre-spring: 47.5° ± 8.5° Post-spring: 45.8° ± 10.0° |
Pre-fall: 141.7° ± 15.0° Pre-spring: 151.4° ± 16.9° Post-spring:152.4° ± 19.9° |
Pre-fall: 92.0° ± 10.0° Pre-spring: 101.7° ± 15.2° Post-spring: 104.4° ± 17.8° |
Pre-fall: 52.7° ± 11.8° Pre-spring: 52.6° ± 10.2° Post-spring: 52.2° ± 11.3° |
Pre-fall: 144.7° ± 14.4° Pre-spring: 145.3° ± 15.0° Post-spring: 156.6° ± 17.3° |
Baseball and Softball players exhibited an increase in external ROM and TROM during the course of a season, but did not exhibit changes in internal rotation |
| Ellenbecker et al. [15] | 103.2° ± 9.1° | 42.2° ± 15.8° | 145.7° ± 18.0° | 94.5° ± 8.1° | 52.4° ± 16.4° | 146.9° ± 17.5° | There was no significant difference in total ROM between extremities in baseball players |
| Freehill et al. [16] | Start of season: 124.8° ± 19.5° End of season: 126.3° ± 21.6° |
Start of season: 70.9° ± 11.8° End of season: 73.6° ± 13.2° |
Start of season: 196.5° ± 22.1° End of season: 199.9° ± 26.0° |
Start of season: 116.3° ± 12.7° End of season: 119.0° ± 16.4° |
Start of season: 76.3° ± 12.4° End of season: 81.4° ± 10.4° |
Start of season: 193.6° ± 19.9° End of season: 200.4° ± 22.0° |
There were no significant changes in shoulder internal and external rotation during the course of a season. Relief pitchers exhibited a greater increase in glenohumeral internal rotation deficit over the season |
| Laudner et al. [19] | Pretest: 118.6° ± 10.9° Posttest: 119.2° ± 11.0° |
Pretest: 43.8° ± 9.5° Posttest: 46.9° ± 9.8° |
Pretest: 162.4° Posttest: 166.1° |
There was a significant increase in glenohumeral internal rotation and posterior shoulder flexibility after performing the sleeper stretch | |||
| Lintner et al. [20] | Stretching group: 142.7° Nonstretching group: 138.9° |
Stretching group: 74.3° Nonstretching group: 55.2° |
Stretching group: 216.98° Nonstretching group: 194.2° |
Participation in an internal rotation stretching program significantly improved glenohumeral internal rotation and TROM | |||
| Myers et al. [24] | Impingement group: 125.8° ± 13.1° Nonimpingement group: 121.1° ± 8.7° |
Impingement group: 42.5 ° ± 12.1° Nonimpingement group: 51.1° ± 14.4° |
Impingement group: 168.3° Nonimpingement group: 172.2° |
Impingement group: 117.5° ± 16.7° Nonimpingement group: 116° ± 10.3° |
Impingement group: 62.2° ± 16.9° Nonimpingement group: 62.2° ± 13.7° |
Impingement group: 179.7° Nonimpingement group: 178.2° |
Throwers with impingement exhibited greater internal rotation deficits and posterior shoulder tightness |
| Osbahr et al. [26] | 126.8° ± 12.0° | 79.3° ± 13.3° | 206.1° | 114.5° ± 9.1° | 91.4° ± 13.6° | 205.9° | Increased external rotation and decreased internal rotation in a thrower’s shoulder is due to both soft tissue changes as well as an increase in humeral retroversion |
| Reagan et al. [27] | 116.3° ± 11.4° | 43.0° ± 7.4° | 159.5° ± 12.4° | 106.6° ± 11.2° | 51.2° ± 7.3° | 157.8° ± 11.5° | An increase in glenohumeral external rotation and a decrease in glenohumeral internal rotation correlates to an increase in humeral retroversion in throwers |
| Thomas et al. [30] | Baseball players with greater than 15° of glenohumeral internal rotation deficit (GIRD) exhibit significantly more scapular protraction and significantly less scapular upward rotation than baseball players with less than 15° of GIRD | ||||||
| Wilk et al. [35] | 136.1° ± 11.2° | 47.5° ± 10.6° | 183.7° ± 14.5° | 128.6° ± 11.0° | 59.1° ± 11.0° | 187.7° ± 14.5° | Pitchers with GIRD were twice as likely to get injured |
| Wilk et al. [36] | 132° | 52° | 184° | 127° | 63° | 190° | External rotation was found to be significantly increased and internal rotation was found to be significantly decreased in a pitcher’s dominant shoulder |
Fig. 1.
Total rotational motion (TRM) concept to assess ER and IR at 90° of abduction (ER + IR = TRM) in the overhead athlete.
Our purposes are to (1) provide ROM data in a large group of professional baseball pitchers to improve the evaluation and treatment of these athletes through the following manner; (2) assess ER and IR passive ROM (PROM) in the throwing shoulder in comparison to the nonthrowing shoulder; and (3) evaluate horizontal adduction and compare this motion bilaterally and correlate these motions to ER/IR PROM.
Methods and Materials
We studied all 369 professional baseball pitchers who presented during six consecutive spring training seasons (2005–2010) for one professional baseball team. Two examiners consistently made all measurements, one to position the extremity (KEW) and one to align and read the goniometer (LCM). Subjects were positioned in the supine position with a towel roll placed between the arm and the table to maintain the plane of the scapula. The examiner positioning the extremity was blinded to the results of the measurement.
Measurements of bilateral passive shoulder ER at 45° of abduction, ER (Fig. 2) and IR (Fig. 3) at 90° abduction and in the scapular plane (10° of horizontal adduction from the coronal plane), and supine horizontal adduction were performed on all patients. The order of extremity and measurement performed was randomized before data collection.
Fig. 2.

Passive assessment of glenohumeral external rotation ROM at 90° abduction and 10° of horizontal adduction (scapular plane) is measured with a bubble goniometer.
Fig. 3.

Assessment of glenohumeral internal rotation ROM performed with stabilization to the scapula. The scapular’s coracoid process is palpated by the thumb while the fingers are placed over the body of the scapula posteriorly.
The examiner passively moved the extremity to the end ROM and the position was held as the bubble goniometer was aligned and read. ER and IR were performed supine with the table stabilizing the scapula. For shoulder ER at 45° and 90° of abduction, the motion was stopped at the subject’s end of available ROM when full capsular or bony end feel was achieved. For shoulder IR, the scapular stabilization technique was used as described by Wilk et al. [37]. A combination of end feel and scapular motion was used to determine the end of ROM. The extremity was moved until the examiner could feel the scapula beginning to anteriorly rotate. The humeral head was not manually stabilized to avoid altering the normal glenohumeral arthrokinematics during measurement. Passive horizontal adduction was performed with the lateral border of the scapular stabilized by the examiner as a cross-body motion was performed with pressure applied to the olecranon tip (Fig. 4). ROM was determined when the lateral border of the scapula began to move and a capsular-like end feel was noted by the examiner. We determined the mean horizontal adduction measurements for the throwing and nonthrowing shoulders.
Fig. 4.

Measurement technique of passive horizontal adduction to assess the flexibility of the posterior musculature.
A standard goniometer was used with an attached, customized bubble inclinometer to assure proper perpendicular alignment and measurement. For shoulder measurement, the axis of the goniometer was positioned over the olecranon process with one arm of the device perpendicular to the ground and the other arm aligned along the ulnar to the ulnar styloid process [25]. Measurements were initially taken before the performance of any warm-up, exercise, or throwing program to remove the influence of these confounding on the ROM data. For each of the four measurements (ER at 45° of abduction, ER at 90° abduction, IR at 90° abduction, and horizontal adduction), a paired t-test was used to compare throwing and nonthrowing shoulders. Differences were considered significant when p < 0.05.
A pilot study was previously performed to assess the test-retest intratester reliability of the goniometric methodology of this study [37]. Intraclass correlation coefficients (ICC3,1) were calculated on shoulder ER, shoulder IR, elbow flexion, and elbow extension. Single-measure intraclass correlation results were 0.81 for shoulder IR, 0.87 for shoulder ER, 0.91 for elbow flexion, and 0.97 for elbow extension. Intratester measurements were performed because the clinicians performing the measurements remained the same throughout the duration of the study. Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) (Version 11.5; Chicago, IL, USA).
Results
The mean ER at 45° of abduction was significantly greater (p < 0.001) for the throwing compared with the nonthrowing shoulder: 102° and 98°, respectively. The mean ER at 90° of abduction was 132°, whereas the nonthrowing shoulder displayed less (p < 0.001) ER with the mean being 127°. When the scapula was stabilized, the pitcher’s throwing shoulder mean IR PROM was lower (p < 0.001) than that on the nondominant shoulder: 52° versus 63°, respectively. Although the mean TRM was lower (p < 0.001) on the throwing than the nonthrowing shoulders (184° versus 190°, respectively) (Table 2), a difference of 6° may not be clinically relevant.
Table 2.
ROM characteristics*
| ROM characteristic | Dominant | Nondominant | Significance |
|---|---|---|---|
| External rotation at 45° | 102 ± 12 | 98 ± 12 | < 0.001 |
| External rotation at 90° | 132 ± 11 | 127 ± 11 | < 0.001 |
| Internal rotation at 90° | 52 ± 12 | 63 ± 12 | < 0.001 |
| Total rotational motion | 184 | 190 | < 0.001 |
| Horizontal adduction | 42 ± 8 | 44 ± 8 | 0.001 |
* Mean in degrees.
The mean horizontal adduction on the throwing side was less (p = 0.001) than that of the nonthrowing side (42° ± 8° versus 44° ± 8°, respectively) but 2° is within the measurement error of goniometry and may not be important [25]. The throwing side IR had a low correlation (r = 0.12; p < 0.001) with throwing side horizontal adduction.
Discussion
Numerous authors have described abnormalities in the pitcher’s ROM, particularly GIRD, that may predispose the pitcher to shoulder and/or elbow injury. Careful and proper evaluation techniques to assess glenohumeral joint motion are critical in the assessment of this type of athlete. We believe the assessment of shoulder ROM is critical to properly evaluate the overhead thrower. We therefore (1) provide ROM data in a large group of professional baseball pitchers to improve the evaluation and treatment of these athletes through the following manner; (2) assess external and internal rotation PROM in the throwing shoulder in comparison to the nonthrowing shoulder; and (3) evaluate horizontal adduction and compare this motion bilaterally and correlate these motions to ER/IR PROM.
Several limitations to this study may include (1) the use of healthy pitchers in determining PROM characteristics; (2) an assessment of pitchers from a single professional baseball organization; and (3) an evaluation that was isolated to the first day of spring training before any throwing during the same season. All of these factors have the potential to impose variations on PROM measurements and the ability to extrapolate these findings to injured and in-season pitchers. Our study’s goal of obtaining normal PROM measurements will help the clinical and rehabilitation specialist determine baseline values for comparison for in-season rehabilitative efforts for the overhead-throwing athlete.
Our findings are similar to other investigators regarding the disparity in side-to-side differences in ER and IR ROM. Although all authors agree that these differences exist, the actual values vary greatly depending on measurement techniques. For example, Osbahr et al. [26] reported an IR value of 79°, whereas a study by Reagan et al. [27] reported an IR value of 43°. Both investigators assessed motion at 90° of abduction and used a standard goniometer. In the present study, we report a value of 52° in the thrower’s dominant shoulder. The differences in the IR ROM measured at 90° of abduction are probably the result of the technique in assessing the motion. In this study, we have used a technique that stabilizes the scapular. In a previous study, [37] we reported that the most reliable method of assessing IR PROM in the throwing shoulder occurs when the scapular is stabilized at the coracoid process and the body of the scapular posteriorly. The clinician should be aware of the most accurate and normal values for ER and IR PROM in the baseball pitcher.
We believe the pitcher’s dominant shoulder IR ROM is approximately 52° and the nondominant is 63°. This represents an 11° bilateral difference in IR ROM when measured at 90° of abduction. Because of the high forces generated during the throwing motion and the repetitive nature of pitching, the overhead thrower exhibits substantial adaptations. One obvious adaptation is the disparity in ER and IR ROM. Investigators have proposed several reasons for the motion adaptations, including osseous adaptations (increased retroversion) [9, 11, 13, 26, 27], posterior musculature tightness [5, 28, 36], posterior capsular tightness [6–8, 32], and even scapular position [3, 31]. Several investigators [9, 26, 27] reported an increase in humeral head retroversion of 10° compared with the contralateral, nonthrowing side. Pieper reported a 9° difference in humeral head retroversion in his cohort, whereas Whiteley et al. [33] reported a 12° difference. We are aware of only one study [11] reporting humeral head retroversion greater than 12° in overhead athletes and that study reported a difference of 17°. If we consider the five studies that reported approximately 10° to 12° difference in retroversion, then these figures match closely with the 11° difference in goniometric IR ROM. Thus, we believe a difference of approximately 12° is likely the result of humeral head retroversion changes. Therefore, when the IR value exceeds 12°, then perhaps other structures are involved in limiting IR ROM and need to be carefully assessed to decrease the susceptibility to injury.
Recently, Wilk et al. [35] prospectively studied pitchers’ ROM and correlated their ROM to injuries sustained during a 3-year period. They determined that the throwers with a side-to-side TRM difference of greater than 5° were more susceptible to injury. Of the injured players assessed, the mean loss of IR was approximately 12°. This is represented by the findings that the difference in TRM was not statistically significant between the dominant and nondominant throwing shoulders.
Thus, we believe the repetitive nature of throwing results in shoulder adaptations. The change in ER and IR ROM is initially the result of the osseous adaptations, which represents a change in side-to-side ROM by approximately 12°. Other factors such as muscular tightness [5, 28, 36], posterior capsular tightness [6–8, 29, 32], and scapular position [3, 31] are superimposed onto the osseous adaptations and may contribute to an injury. Further research is needed to determine the exact risk factors for shoulder injuries in the thrower and the other structures that contribute to the loss of shoulder IR and the increase in ER.
Based on the previously mentioned articles, we believe it is necessary to perform stretching and ROM exercises on pitchers who exhibit ROM characteristics, which may predispose them to injury. The ROM values that make the thrower more susceptible to injury are the following: (1) side-to-side TRM differences greater than 5°; and (2) GIRD of 12° or more compared with the contralateral shoulder. Several authors have reported a stretching program in college players [19] and in professional baseball pitchers [20], which were effective in maintaining or improving shoulder IR ROM. Based on these observations, we developed a stretching program for the posterior shoulder soft tissues. These stretches include the sleeper stretch (Fig. 5), sleeper stretch with a lift (Fig. 6), and supine horizontal adduction (cross-body stretch with IR) (Fig. 7) that can be performed alone or with a rehabilitation specialist [22]. We also incorporate a horizontal adduction stretch with the patient assisting in IR (Fig. 8). The stretches are performed to improve the flexibility of the posterior musculature, which may become tight as a result of the high eccentric muscle contractions and forces (repetitive microtrauma) during the deceleration phase of the throwing motion. The ultimate goal of stretching is to restore IR PROM within approximately 10° to 12° of the nondominant side. Also, the clinical and rehabilitation specialist should consider regaining TROM within 5° of the opposite shoulder. Another structure to consider when improving IR in the baseball pitcher is the posterior capsule. Although we rarely find this structure to become excessively tight on clinical examination, it should be noted as a possible limitation to shoulder IR in some individuals. The rehabilitation technique we use to improve the posterior capsular mobility is joint mobilization. It is important that the rehabilitation specialist performs the glide in a posterolateral direction that is perpendicular to the glenoid face to avoid abutting the humeral head with the glenoid rim (Fig. 9).
Fig. 5.

Self stretch, known as the “sleeper stretch,” is used for the posterior musculature of the glenohumeral joint.
Fig. 6.

Modified “sleeper stretch with a lift” to alter the stretch to the posterior musculature; this technique pretensions posterior structures before IR motion; thus, less IR is required.
Fig. 7.

Horizontal adduction stretch performed by the rehabilitation specialist to improve posterior shoulder flexibility. To further enhance the IR stretch, the rehabilitation specialist pushes on the dorsum of the distal forearm after getting into end ROM, thus enhancing the IR stretch.
Fig. 8.

Horizontal adduction stretch modification to include the athlete applying gentle overpressure into IR as the rehabilitation specialist performs horizontal adduction with the lateral scapular border stabilized.
Fig. 9.

Posterior capsular mobilization performed by the rehabilitation specialist in a posterolateral direction.
The overhead thrower is a unique athlete with unique physical demands and injury risks. Restoring glenohumeral PROM in the overhead athlete appears critical in preventing future injury and the potential need for surgery. The clinical and rehabilitation specialists should have a clear understanding of proper measurement and treatment techniques in the overhead-throwing athlete. In fact, the rehabilitation efforts should attempt to maximize results in the thrower through the following goals: (1) IR of the dominant arm within 12° of the opposite arm; (2) TRM within 5° of the opposite side; and (3) postural correction exercises to stretch tight structures and strengthen the weak scapula stabilizers. The authors believe these critical factors can decrease the risk of injury in overhead throwers.
Acknowledgments
We thank Glenn S. Fleisig, PhD, and his staff at The American Sports Medicine Institute for the statistical analysis. Also, a special thank you to Ron Porterfield, ATC, and the Tampa Bay Rays baseball organization for allowing us access to their players, facilities, and staff during the data collection process.
Footnotes
Each author certifies that he has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
References
- 1.Andrews JR, Casey PJ. Internal impingement. In: Krishnan SG, Hawkins RJ, Warren RF, editors. The Shoulder and the Overhead Athlete. Philadelphia: Lippincott Williams and Wilkins; 2004. pp. 125–134. [Google Scholar]
- 2.Bigliani LU, Codd TP, Connor PM, Levine WN, Littlefield MA, Hershon SJ. Shoulder motion and laxity in the professional baseball player. Am J Sports Med. 1997;25:609–613. doi: 10.1177/036354659702500504. [DOI] [PubMed] [Google Scholar]
- 3.Borich MR, Bright JM, Lorello DJ, Cieminski CJ, Buisman T, Ludewig PM. Scapular angular positioning at end range internal rotation in cases of glenohumeral internal rotation deficit. J Orthop Sports Phys Ther. 2006;36:926–934. doi: 10.2519/jospt.2006.2241. [DOI] [PubMed] [Google Scholar]
- 4.Borsa PA, Dover GC, Wilk KE, Reinold MM. Glenohumeral range of motion and stiffness in professional baseball pitchers. Med Sci Sports Exerc. 2006;38:21–26. [DOI] [PubMed]
- 5.Borsa PA, Wilk KE, Jacobson JA, Scibek JS, Dover GC, Reinold MM, Andrews JR. Correlation of range of motion and glenohumeral translation in professional baseball pitchers. Am J Sports Med. 2005;33:1392–1399. doi: 10.1177/0363546504273490. [DOI] [PubMed] [Google Scholar]
- 6.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part I: pathoanatomy and biomechanics. Arthroscopy. 2003;19:404–420. doi: 10.1053/jars.2003.50128. [DOI] [PubMed] [Google Scholar]
- 7.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19:641–661. doi: 10.1016/S0749-8063(03)00389-X. [DOI] [PubMed] [Google Scholar]
- 8.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part II: evaluation and treatment of SLAP lesions in throwers. Arthroscopy. 2003;19:531–539. doi: 10.1053/jars.2003.50139. [DOI] [PubMed] [Google Scholar]
- 9.Chant CB, Litchfield R, Griffin S, Thain LM. Humeral head retroversion in competitive baseball players and its relationship to glenohumeral rotation range of motion. J Orthop Sports Phys Ther. 2007;37:514–520. doi: 10.2519/jospt.2007.2449. [DOI] [PubMed] [Google Scholar]
- 10.Conte S, Requa RK, Garrick JG. Disability days in major league baseball. Am J Sports Med. 2001;29:431–436. doi: 10.1177/03635465010290040801. [DOI] [PubMed] [Google Scholar]
- 11.Crockett HC, Gross LB, Wilk KE, Schwartz ML, Reed J, O’Mara J, Reilly MT, Dugas JR, Meister K, Lyman S, Andrews JR. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002;30:20–26. doi: 10.1177/03635465020300011701. [DOI] [PubMed] [Google Scholar]
- 12.Dines JS, Frank JB, Akerman M, Yocum LA. Glenohumeral internal rotation deficits in baseball players with ulnar collateral ligament insufficiency. Am J Sports Med. 2009;37:566–570. doi: 10.1177/0363546508326712. [DOI] [PubMed] [Google Scholar]
- 13.Drakos MC, Rudzki JR, Allen AA, Potter HG, Altchek DW. Internal impingement of the shoulder in the overhead athlete. J Bone Joint Surg Am. 2009;91:2719–2728. doi: 10.2106/JBJS.I.00409. [DOI] [PubMed] [Google Scholar]
- 14.Dwelly PM, Tripp BL, Tripp PA, Eberman LE, Gorin S. Glenohumeral rotational range of motion in collegiate overhead-throwing athletes during an athletic season. J Athl Train. 2009;44:611–616. [DOI] [PMC free article] [PubMed]
- 15.Ellenbecker TS, Roetert EP, Bailie DS, Davies GJ, Brown SW. Glenohumeral joint total rotation range of motion in elite tennis players and baseball pitchers. Med Sci Sports Exerc. 2002;34:2052–2056. doi: 10.1097/00005768-200212000-00028. [DOI] [PubMed] [Google Scholar]
- 16.Freehill MT, Ebel BG, Archer KR, Bancells RL, Wilckens JH, McFarland EG, Cosgarea AJ. Glenohumeral range of motion in major league pitchers: changes over the playing season. Sports Health Journal. 2011;3:97–104. [DOI] [PMC free article] [PubMed]
- 17.Jazrawi LM, McCluskey GM, 3rd, Andrews JR. Superior labral anterior and posterior lesions and internal impingement in the overhead athlete. Instr Course Lect. 2003;52:43–63. [PubMed] [Google Scholar]
- 18.Kibler WB. Role of the scapula in the overhead throwing motion. Contemp Orthop. 1991;22:525–532. [Google Scholar]
- 19.Laudner KG, Sipes RC, Wilson JT. The acute effects of sleeper stretches on shoulder range of motion. Journal of Athletic Training. 2008;43:359–363. doi: 10.4085/1062-6050-43.4.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lintner D, Mayol M, Uzodinma O, Jones R, Labossiere D. Glenohumeral internal rotation deficits in professional pitchers enrolled in an internal rotation stretching program. Am J Sports Med. 2007;35:617–621. doi: 10.1177/0363546506296736. [DOI] [PubMed] [Google Scholar]
- 21.Litchfield R, Hawkins R, Dillman CJ, Atkins J, Hagerman G. Rehabilitation for the overhead athlete. J Orthop Sports Phys Ther. 1993;18:433–441. doi: 10.2519/jospt.1993.18.2.433. [DOI] [PubMed] [Google Scholar]
- 22.McClure P, Balaicuis J, Heiland D, Broersma ME, Thorndike CK, Wood A. A randomized controlled comparison of stretching procedures for posterior shoulder tightness. J Orthop Sports Phys Ther. 2007;37:108–114. doi: 10.2519/jospt.2007.2337. [DOI] [PubMed] [Google Scholar]
- 23.McFarland EG, Wasik M. Epidemiology of collegiate baseball injuries. Clin J Sport Med. 1998;8:10–13. doi: 10.1097/00042752-199801000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am J Sports Med. 2006;34:385–391. doi: 10.1177/0363546505281804. [DOI] [PubMed] [Google Scholar]
- 25.Norkin CC, White DJ. Measurement of Joint Motion: A Guide to Goniometry. Philadelphia, PA, USA: FA Davis; 2003. [Google Scholar]
- 26.Osbahr DC, Cannon DL, Speer KP. Retroversion of the humerus in the throwing shoulder of college baseball pitchers. Am J Sports Med. 2002;30:347–353. doi: 10.1177/03635465020300030801. [DOI] [PubMed] [Google Scholar]
- 27.Reagan KM, Meister K, Horodyski MB, Werner DW, Carruthers C, Wilk K. Humeral retroversion and its relationship to glenohumeral rotation in the shoulder of college baseball players. Am J Sports Med. 2002;30:354–360. doi: 10.1177/03635465020300030901. [DOI] [PubMed] [Google Scholar]
- 28.Reinold MM, Wilk KE, Macrina LC, Sheheane C, Dun S, Fleisig GS, Crenshaw K, Andrews JR. Changes in shoulder and elbow passive range of motion after pitching in professional baseball players. Am J Sports Med. 2008;36:523–527. doi: 10.1177/0363546507308935. [DOI] [PubMed] [Google Scholar]
- 29.Tehranzadeh AD, Fronek J, Resnick D. Posterior capsular fibrosis in professional baseball pitchers: case series of MR arthrographic findings in six patients with glenohumeral internal rotational deficit. Clin Imaging. 2007;31:343–348. doi: 10.1016/j.clinimag.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 30.Thomas SJ, Swanik KA, Swanik CB, Kelly JDt. Internal rotation deficits affect scapular positioning in baseball players. Clin Orthop Relat Res. 2010;468:1551–1557. doi: 10.1007/s11999-009-1124-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Torres RR, Gomes JL. Measurement of glenohumeral internal rotation in asymptomatic tennis players and swimmers. Am J Sports Med. 2009;37:1017–1023. doi: 10.1177/0363546508329544. [DOI] [PubMed] [Google Scholar]
- 32.Tyler TF, Nicholas SJ, Roy T, Gleim GW. Quantification of posterior capsule tightness and motion loss in patients with shoulder impingement. Am J Sports Med. 2000;28:668–673. doi: 10.1177/03635465000280050801. [DOI] [PubMed] [Google Scholar]
- 33.Whiteley RJ, Ginn KA, Nicholson LL, Adams RD. Sports participation and humeral torsion. J Orthop Sports Phys Ther. 2009;39:256–263. doi: 10.2519/jospt.2009.2821. [DOI] [PubMed] [Google Scholar]
- 34.Wilk KE, Arrigo C. Current concepts in the rehabilitation of the athletic shoulder. J Orthop Sports Phys Ther. 1993;18:365–378. doi: 10.2519/jospt.1993.18.1.365. [DOI] [PubMed] [Google Scholar]
- 35.Wilk KE, Macrina LC, Fleisig GS, Porterfield R, Simpson CD, 2nd, Harker P, Paparesta N, Andrews JR. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am J Sports Med. 2011;39:329–335. doi: 10.1177/0363546510384223. [DOI] [PubMed] [Google Scholar]
- 36.Wilk KE, Meister K, Andrews JR. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med. 2002;30:136–151. doi: 10.1177/03635465020300011201. [DOI] [PubMed] [Google Scholar]
- 37.Wilk KE, Reinold MM, Macrina LC, Porterfield R, Devine KM, Suarez K, Andrews JR. Glenohumeral internal rotation measurements differ depending on stabilization techniques. Sports Health Journal. 2009;1:131–136. doi: 10.1177/1941738108331201. [DOI] [PMC free article] [PubMed] [Google Scholar]