Abstract
Background
New equipment and techniques often are used in clinical practice, occasionally without evidence of effectiveness and safety.
Questions/purposes
We asked whether the stage of introduction of an endoprosthesis model for TKA affected the risk of early revision.
Methods
We studied mandatory registry data from all centers in Finland (n = 69) that performed TKAs for primary osteoarthritis between 1998 and 2004. Of the total of 23,707 patients (28,760 TKAs), 22,551 patients (27,105 TKAs) had a followup of 5 years; we excluded longer followup from the analysis as subsequent revisions might result from wear rather than early technical failures. We used proportional hazards modeling for calculating the hazard ratios for the first 15 operations and subsequent increments of numbers of operations while adjusting for potentially confounding variables.
Results
For the first 15 operations with a new endoprosthesis, the risk was elevated (hazard ratio, 1.48; 95% confidence interval, 1.14–1.91). Absolute risk increase of early revision for the first 15 patients was 1.7% (95% confidence interval, 0.7–2.7). The risk was not increased as the numbers of TKAs incrementally performed increased.
Conclusions
Our data show an increased risk of early revision surgery for the first patients obtaining a knee endoprosthesis model previously unused in the hospital. Patients should be informed if there is a plan to introduce a new model of endoprosthesis in the hospital and offered the possibility to choose a conventional endoprosthesis instead. Although introducing potentially better endoprostheses is important, there is a need for managed introduction of new technology.
Level of Evidence
Level I, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
TKA is an established treatment for patients with severe osteoarthritis (OA) of the knee [1]. At this time, there are numerous brands and models of endoprostheses available on the market and new models are likely to emerge because of the drive for new technology and marketing, and the incidence of TKA is increasing [7, 13, 19, 22]. Hospital managers and orthopaedists make important decisions when choosing the implants and instruments to be used and these decisions carry consequences to patients’ health.
Based on comparisons of implant survival, the endoprosthesis has an effect on the risk for revision surgery [8, 21, 30, 32]. Although the principles of TKA are relatively constant, instrumentation of implants, like resecting guides and cutting blocks, differ and surgeons must be familiar with the particular instrumentation of each model he or she uses. When implementing computerized navigation or a minimally invasive technique in TKA, some studies have documented a learning curve effect [14, 16, 20, 23]. It could be expected that there would be a learning curve in conventional TKAs as well and that the learning process is related to every brand of endoprosthesis introduced for the first time in a hospital, not just to the first TKAs performed by the surgeon. However, no reliable scientific data exist to confirm this assumption.
We therefore asked whether the first patients operated on with any endoprosthesis type in a hospital have a higher revision rate than patients whose implants are conventional in the hospital. As a secondary analysis, the risk of early revision owing to characteristics related to the operation, patient, and hospital was assessed.
Patients and Methods
We identified all 23,707 patients, from the Finnish Arthroplasty Register (FAR), who underwent a total of 28,760 primary TKAs owing to OA between January 1, 1998, and December 31, 2004. The register contains information from all primary and revision TKAs performed in Finland since 1980 on joint level from every arthroplasty producer in the country. Reporting for entry in the implant and discharge register is mandatory. One thousand one hundred fifty-six patients (with 1655 operations) who underwent 28,760 TKAs and had missing data for endoprosthesis model (either femoral or tibial component model name missing) or fixation technique were excluded. These exclusions left 22,551 patients who had 27,105 TKAs in the data with 5 years of followup or who died before 5 years (Table 1). There were 1000 revisions in the data. Altogether 34 femoral and 27 tibial endoprosthesis models were introduced in the study population contributing to 34 compound introductions. In 66 of the total of 69 hospitals, there were 339 new endoprosthesis introductions between1998 and 2004. The followup was restricted to 5 years as later revisions more likely might be as a result of normal wear.
Table 1.
Characteristics of the primary TKAs
| Characteristic | Number of TKAs | % of TKAs | Characteristic | Number of TKAs | % of TKAs |
|---|---|---|---|---|---|
| Sex | Endoprosthesis ordinal number group | ||||
| Male | 7657 | 28.2% | Group A (operations 1 to 15) | 2006 | 7.4% |
| Female | 19,448 | 71.8% | Group B (16 to 30) | 1403 | 5.2% |
| Group C (31 to 50) | 1462 | 5.4% | |||
| Age | Group D (51 to 100) | 2926 | 10.8% | ||
| Median age, years (range) | 72 (median) | 32–97 (range) | Group E (over 101) | 19,308 | 71.2% |
| Morbidities | Endoprosthesis use and specialization | ||||
| Coronary disease (ICD-10: 120-125) | 4411 | 16.3% | Femoral models per 100 TKAs in hospital (average) | 4.6 (average) | |
| Chronic obstructive pulmonary disease and asthma (ICD-10: J44-J46) | 3074 | 11.3% | Arthroplasty share of all operations in hospital | 11.2% | |
| TKA share of arthroplasty operations in hospital | 41.1% | ||||
| Operation | |||||
| Bilateral | 2283 | 8.4% | Femoral model | ||
| Cemented | 25,452 | 93.9% | Duracon | 10,086 | 37.2% |
| Cementless | 560 | 2.1% | AGC V2 | 5945 | 21.9% |
| Hybrid | 1093 | 4.0% | PFC Sigma | 3527 | 13.0% |
| Patellar resurfacing | 8061 | 29.7% | Nexgen® CR | 1559 | 5.8% |
| Bone grafts | 308 | 1.1% | Arge | 1303 | 4.8% |
| Intravenous prophylactic antibiotics | 26,706 | 98.5% | Nexgen® LPS | 1290 | 4.8% |
| Length of stay, average (days) | 8.6 (average) | Maxim Primary | 854 | 3.2% | |
| PFC Sigma Stabilizer | 815 | 3.0% | |||
| Annual number of knee arthroplasties in hospital | Duracon Stabilizer Box | 349 | 1.3% | ||
| Less than 51 | 2127 | 7.8% | Genesis II | 165 | 0.6% |
| 51 to 150 | 11,879 | 43.8% | PFC | 147 | 0.5% |
| 151 to 300 | 8014 | 29.6% | Maxim PS | 135 | 0.5% |
| More than 300 | 5085 | 18.8% | AGC V2 Stabilizer | 121 | 0.4% |
| Search Evolution | 116 | 0.4% | |||
| Duracon Modular Total Stabilizer | 110 | 0.4% | |||
| Search | 109 | 0.4% | |||
| Other models | 474 | 1.7% |
ICD-10 = International Classification of Diseases, 10th Revision; Duracon, Stryker Howmedica, Mahwah, NJ, USA; PFC Sigma, DePuy, Warsaw, IN, USA; Nexgen®, Zimmer Inc, Warsaw, IN, USA; AGC V2, Biomet UK Ltd, South Glamorgan, UK; Arge, Implantcast GmbH, Buxtehude, Germany; Maxim, Biomet Orthopaedics, Warsaw, IN, USA; Genesis II, Smith & Nephew, Memphis, TN, USA; Search, Aesculap AG, Tuttlingen, Germany.
We linked individuals’ data in FAR from 1998 through 2009 and hospital discharge register from 1987 through 2009 using personal identification codes. The coverage and reliability of the registers are of a very high standard [10, 18, 29]. We also linked the Death Statistics of Statistics Finland to the data to take into consideration censoring of patients and special reimbursements (from the register of the Social Insurance Institution) of the patients from 1995 through 2004 to add information regarding their long-term medications to complete the medical histories. We used the discharge and arthroplasty registers to track all revisions performed. We obtained the number of every endoprosthesis model used between January 1, 1980, and December 31, 1997, for every hospital separately for femoral, tibial, and patellar components from the FAR. Using knee-specific data of the arthroplasty register from January 1, 1998, to December 31, 2004, for each knee arthroplasty in this period we defined the prostheses parts’ ordinal number in the operating hospital. We included only primary TKAs performed for primary OA in the final study data. Bicompartmental and tricompartmental primary TKAs are included. Neither minimally invasive techniques nor computer-assisted navigation techniques were used during the study period. The data are knee-specific.
We numbered the chronological sequence of insertion (ie, ordinal numbers) of femoral, tibial, and patellar components for all knee arthroplasties in each hospital separately, but in the analysis, patellar component ordinals were not taken into account. Usually, the femoral and tibial components define each other and components rarely are mixed. The compound ordinal number used in the model is the minimum of the femoral and tibial component ordinals (less used in hospital). This reflects our view that the less used component defines the unfamiliarity associated with the prostheses during the operation and initiates the learning curve.
The personal identification number enables the accrual of the followup data for each individual from the registers and tracking of all revisions that occurred in 5 years from the primary TKA. Revisions are reliably recorded in registers and they are an accepted outcome measure in register-based TKA research [31, 33]. In this study, insertion of a patellar component after the primary operation is considered to be a revision.
We classified the operations with respect to the ordinal number into five classes: Group A (Operations 1–15), Group B (16–30), Group C (31–50), Group D (51–100), and Group E (over 100). We compared the cases in Group A to D with those in Group E. We used Cox’s proportional hazard model [5] to compare the groups so censoring because of deaths and timing of the revision could be taken into account. Because we knew the dates of the primary and revision surgeries, we used the time in days from the primary surgery to revision or censoring as the dependent variable. Censoring happened when 5 years of followups ended or the patient died, whichever came first.
We extensively adjusted for potentially confounding factors. In the final model, the patient’s gender, age, and comorbid diseases (coronary disease, chronic obstructive pulmonary disease [COPD], and asthma) were included. As operation-related variables, we included cementing, patellar component insertion, bone graft use, intravenous antibiotic prophylaxis, bilaterality, femoral model (if at least 100 operations with the model in the data; models with less than 100 operations in the data were placed in ‘other models’), ordinal number group, and the length of stay. In addition, for each calendar year, hospital-level variables that possibly affect the outcome of primary surgery (TKA share of hospital arthroplasty volume, hospital’s femoral title use per 100 TKAs, average length of stay after TKA, hospital knee arthroplasty volume) were constructed. All regressors in the model were fixed, ie, considered time-independent. The final model was stratified on gender and classified age (younger than 50, 51–60, 61–70, 71–80, and older than 80 years) to allow men and women of different ages a different baseline hazard function. The proportional hazard assumption was investigated by testing for a nonzero slope in a generalized linear regression of the scaled Schoenfeld residuals on functions of time [11]. The global test of proportionality was nonsignificant (p = 0.0759).
Results
The first 15 implementations (in Group A) had a 1.48-fold risk (p = 0.003) for revision surgery when compared with Group E (Table 2) after adjusting for all baseline characteristics. The learning curve smoothed quickly: the revision hazard was not increased for Groups B to D. The absolute risk for revision in Group A was 5.3% and in Group E, 3.6%. Thus, the absolute risk increase was 1.7% (95% confidence interval, 0.7%–2.7%), and number needed to harm is 59 (ie, 1/0.017).
Table 2.
Risk for revision surgery in the four stages of endoprosthesis introduction
| Stage of introduction | Hazard ratio* | 95% confidence interval |
|---|---|---|
| Group A (operations 1–15) | 1.48 | 1.14–1.91 |
| Group B (16–30) | 0.97 | 0.71–1.33 |
| Group C (31–50) | 0.85 | 0.61–1.17 |
| Group D (51–100) | 1.14 | 0.93–1.40 |
| Group E (over 100) | 1.00 |
* Adjusted with all factors that are listed in Table 1.
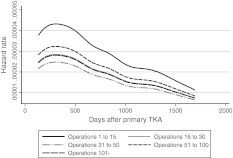
The smoothed hazard functions of the different stages of introduction show that the hazard for early revision of the knee is elevated for the first 15 operations with a new endoprosthesis model in a hospital (Fig. 1). Overall, the risk for early revision is greatest during the first 2 years after the primary TKA. Also, the difference in hazard for early revision between the stages of introduction is greatest during the early years of the followup.
Fig. 1.
The smoothed hazard function of early revision after primary TKA in different stages of endoprosthesis introduction during the 5 years of followup in a population-based study of 27,105 TKAs as shown.
Characteristics of the patients being among the first 15 in a hospital (Group A) to get a new endoprosthesis model and the patients operated on with an endoprosthesis that had been used at least 100 times in the hospital (Group E) differed. The patients in Group A were slightly older (71.1 versus 70.5 years; p < 0.001) and there were relatively fewer males (25.3% versus 28.7%; p = 0.001) than in Group E. A same-day bilateral operation was less common in Group A (5.4% versus 9.0%; p < 0.001) as was the insertion of a patellar component (25.0% versus 30.4%; p < 0.001).
None of the operation-related explanatory variables were statistically significantly related to early revision (Table 3). Of the femoral models, two models (PFC Sigma; DePuy, Warsaw, IN, USA) (Nexgen CR; Zimmer Inc, Warsaw, IN, USA) had lower and two models (Duracon Stabilizer Box; Stryker Howmedica, Mahwah, NJ, USA) (Search, Aesculap AG, Tuttlingen, Germany) had higher overall hazard for early revision than the reference model (Duracon). Coronary artery disease and COPD or asthma were associated with an increased hazard for early revision surgery (Table 4). The longer the patient’s length of stay in the surgical department, the greater the risk of early revision. The higher the TKA share of total arthroplasty volume in a hospital, the lower the early revision risk.
Table 3.
Results of the Cox proportional hazards model
| Variable (reference) | Hazard ratio* | 95% CI |
|---|---|---|
| Bilateral operation (unilateral) | 0.94 | 0.75–1.18 |
| Cementless (cemented) | 0.86 | 0.50–1.48 |
| Hybrid (cemented) | 1.21 | 0.89–1.63 |
| Patellar resurfacing (no patellar resurfacing) | 0.92 | 0.79–1.06 |
| Antibiotic prophylaxis (no intravenous antibiotic prophylaxis) | 0.78 | 0.49–1.23 |
| Bone grafts (no bone grafts) | 0.96 | 0.54–1.71 |
| Femoral model, manufacturer [years when introductions in hospitals] | ||
| Duracon, Stryker [1998–2004] (reference model) | 1.00 | |
| AGC V2, Biomet [1998–2004] | 0.94 | 0.80–1.11 |
| PFC Sigma, DePuy [1998, 1999, 2001–2004] | 0.66 | 0.52–0.84 |
| Nexgen® CR, Zimmer [1998–2004] | 0.54 | 0.37–0.78 |
| Arge, Implant Cast [1998–2002] | 0.86 | 0.60–1.24 |
| Nexgen LPS, Zimmer [1999–2004] | 0.89 | 0.63–1.27 |
| Maxim Primary, Biomet [1998–2000, 2002, 2004] | 0.92 | 0.64–1.33 |
| PFC Sigma Stabilized, DePuy [1998–2004] | 0.68 | 0.42–1.09 |
| Duracon Stabilizer Box, Stryker [1998–2004] | 1.85 | 1.22–2.81 |
| Genesis II, Smith & Nephew [1998–2004] | 0.26 | 0.06–1.05 |
| PFC, DePuy [1998] | 0.89 | 0.40–2.02 |
| Maxim PS, Smith & Nephew [1998, 2001, 2004] | 1.47 | 0.72–3.02 |
| AGC V2 Stabilized, Biomet [1998–2004] | 1.25 | 0.53–2.97 |
| Search Evolution, Aesculap AG [2001, 2002] | 0.20 | 0.03–1.52 |
| Duracon Modular TS, Stryker [1998–2004] | 2.06 | 0.98–4.36 |
| Search, Aesculap AG [1998] | 2.51 | 1.20–5.24 |
| Other models | 0.94 | 0.59–1.52 |
* Adjusted with all factors listed in Table 1.
Table 4.
Results of the Cox proportional hazards model
| Variable (reference) | Hazard ratio* | 95% CI |
|---|---|---|
| Patient specific | ||
| Coronary disease (no coronary disease) | 1.27 | 1.07–1.50 |
| COPD and asthma (no COPD or asthma) | 1.27 | 1.06–1.51 |
| Length of stay | 1.06 | 1.04–1.07 |
| Hospital specific | ||
| TKA share of arthroplasty ops | 0.42 | 0.19–0.97 |
| Femoral models per 100 TKAs | 0.99 | 0.97–1.01 |
| Length of stay, average | 0.98 | 0.94–1.03 |
| Less than 51 total knee arthroplasties per year | 1.25 | 0.86–1.80 |
| 51 to 150 total knee arthroplasties per year | 1.23 | 0.97–1.57 |
| 151 to 300 total knee arthroplasties per year | 1.25 | 0.98–1.58 |
| Over 300 total knee arthroplasties per year | 1.00 | |
* Adjusted with all factors that are listed in Table 1; COPD = chronic obstructive pulmonary disease.
Discussion
Based on comparisons of implant survival, the endoprosthesis model has an effect on the risk for revision surgery [8, 21, 30, 32]. Although the principles of TKA are relatively constant, instrumentation of implants, like resecting guides and cutting blocks, differ and surgeons must be familiar with the particular instrumentation of each model he or she uses. At this time, there are numerous endoprosthesis brands and models available on the market and new models are likely to emerge because of the drive for new technology and its marketing, and because the incidence of TKA is increasing [7, 13, 19, 22]. Hospital managers and orthopaedists make important decisions when choosing the implants and instruments to be used and these decisions carry consequences to patients’ health. There might be a learning curve that is related to every endoprosthesis brand introduced for the first time in a hospital, not just to the first TKAs performed by the surgeon. However, no reliable scientific data exist. The ability to identify the stage of introduction of an endoprosthesis model for each patient in a nationwide population provides unique data. The personal identification number allows linking of hospital discharge register data with implant register data individually for patient comorbidities, operation details, and outcome. We therefore asked whether the first patients operated on with any endoprosthesis type in a hospital have a higher revision rate than patients whose implants are conventional in the hospital and, secondarily, whether the characteristics related to the operation, patient, and hospital were associated with risk of early revision.
There are some limitations that need to be considered. First, because there usually was more than one model in use in each hospital, we could not quantify the true amount of technical change linked to the introduction of a particular endoprosthesis. That is, a new implant could be substantially similar to the previously used implants but not reflect essential changes in technology or surgical difficulty. Thus, our data might underestimate the risk for early revision regarding major changes in the surgical technique. However, the 7-year study covers an entire population of patients with OA undergoing TKAs and the findings reflect ordinary healthcare practice. Further, the analysis was performed on a large number of operations and variety of endoprostheses. The register-based approach enables accurate followup of the patients with a minimal number of dropouts. The findings are plausible given the learning curve in surgery and probably are generalizable to any setting. Second, the degree of pain relief and disability varies after TKA [3, 6, 12, 28], and our data might underestimate the harmful effects of introducing an endoprosthesis model, ie, there might be patients who still have pain and disability after failed TKAs but not enough to warrant revision surgery. The most common causes for TKA revision surgery are aseptic loosening, wear, instability, infection, fracture, and malalignment [4, 12]. These postoperative problems induce pain and disability. Most of the revisions in our data were performed during the first 2 years of the followup, a phenomenon also found by Sharkey et al. [34]. Third, we considered insertion of a patellar component after the primary TKA to be a revision. This is justified, although it is not uncommon to attempt to solve postoperative pain resulting from TKA component malpositioning by inserting a patellar component. We do not have reliable data for the reasons for revisions. However, it is probable that the main finding of our study is the result of the learning curve effect of implementation of endoprostheses. We consider it unlikely that deficiencies in the quality of the hardware (quality or design of the endoprostheses) biased the study because we adjusted for the models. Fourth, some patient characteristics were unavailable in the register, like BMI and physical activity. In a systematic review by Gillespie and Porteous [9], there was some evidence for an increased risk for early implant failure among obese subjects. However, in a study of 9735 patients undergoing TKAs, no such risk was found [2]. Furthermore, in clinical practice, we believe it is improbable that obesity is a decisive factor when choosing between endoprosthesis models. There is some evidence of no correlation between physical activity and early revision [15, 26]. It is unlikely that physical activity would bias our estimates, because age and physical activity are correlated and age was adjusted for in our model. The characteristics of the patients operated on with a recently implemented endoprosthesis differed slightly from the characteristics of the patients operated on with a model that had been used in the hospital more than 100 times. We think that these small differences have no clinical importance. Adjusting for endoprosthesis model was essential to control for patient-related factors that were not available in register data (ie, degree of arthrosis, preoperative malalignment). The 5-year revision hazards of models shown in Table 3 may reflect patient-related need for specific endoprosthesis type and differences in learning curve. We are aware that the models might have different learning curves, but were not able to analyze the learning curve individually for each endoprosthesis model. Fifth, hospital arthroplasty volume, surgical expertise, and annual surgeon’s caseload might decrease revision risk, but the evidence is inconclusive [17, 24, 25, 27, 35, 36]. We controlled for hospital arthroplasty volumes in the analyses. The register data do not show who operated on each patient. Sixth, we could not analyze the effect of different operative techniques. Surgeons differ in their skills and caseloads, and this could have an effect on revision risk. For instance, in the case of an experienced surgeon moving to another hospital, he or she might begin in the new hospital with the old and familiar prostheses for him- or herself but not used at the new hospital and by its team. However, this might shift the revision risk of introductions downward.
Our data confirm that introduction of an endoprosthesis model in a hospital puts the first patients at greater risk of revision surgery. The effect is substantial for the first 15 patients (Group A) who are operated on with implantation of a new endoprosthesis model because their adjusted relative risk is 1.48 times greater than that of patients having implantation of a conventional model (Group E).
Our data show there is an increased risk of early revision surgery for the first patients obtaining a knee endoprosthesis model previously unused in a hospital. Patients should be informed if there is a plan to introduce a new model and offered the possibility to choose a conventional endoprosthesis instead. Surgeons should be aware of the risks and preferably practice beforehand with the new model using, eg, cadavers or plastic bone models. Units performing arthroplasties might consider introducing endoprosthesis models. Although introducing potentially better endoprosthesis models is important, there is a need for managed uptake of new technology.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the National Institute of Health and Welfare, Helsinki, Finland.
References
- 1.Bellemans J, Vandenneucker H, Vanlauwe J. Total knee replacement. Curr Orthop. 2005;19:446–452. doi: 10.1016/j.cuor.2005.09.007. [DOI] [Google Scholar]
- 2.Bordini B, Stea S, Cremonini S, Viceconti M, Palma R, Toni A. Relationship between obesity and early failure of total knee prostheses. BMC Musculoskelet Disord. 2009;10:29. doi: 10.1186/1471-2474-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bourne RB, McCalden RW, MacDonald SJ, Mokete L, Guerin J. Influence of patient factors on TKA outcomes at 5 to 11 years followup. Clin Orthop Relat Res. 2007;464:27–31. doi: 10.1097/BLO.0b013e318159c5ff. [DOI] [PubMed] [Google Scholar]
- 4.Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010;468:45–51. doi: 10.1007/s11999-009-0945-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cox DR. Regression models and life-tables. J R Stat Soc Ser B. 1972;34:187–220. [Google Scholar]
- 6.Cushnaghan J, Bennett J, Reading I, Croft P, Byng P, Cox K, Dieppe P, Coggon D, Cooper C. Long-term outcome following total knee arthroplasty: a controlled longitudinal study. Ann Rheum Dis. 2009;68:642–647. doi: 10.1136/ard.2008.093229. [DOI] [PubMed] [Google Scholar]
- 7.Dixon T, Shaw M, Ebrahim S, Dieppe P. Trends in hip and knee joint replacement: socioeconomic inequalities and projections of need. Ann Rheum Dis. 2004;63:825–830. doi: 10.1136/ard.2003.012724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Furnes O, Espehaug B, Lie SA, Vollset SE, Engesaeter LB, Havelin LI. Early failures among 7, 174 primary total knee replacements: a follow-up study from the Norwegian Arthroplasty Register 1994–2000. Acta Orthop Scand. 2002;73:117–129. doi: 10.1080/000164702753671678. [DOI] [PubMed] [Google Scholar]
- 9.Gillespie GN, Porteous AJ. Obesity and knee arthroplasty. Knee. 2007;14:81–86. doi: 10.1016/j.knee.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Gissler M, Haukka J. Finnish health and social welfare registers in epidemiological research. Norsk Epidemiol. 2004;14:113–120. [Google Scholar]
- 11.Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81:515–526. doi: 10.1093/biomet/81.3.515. [DOI] [Google Scholar]
- 12.Hossain F, Patel S, Haddad FS. Midterm assessment of causes and results of revision total knee arthroplasty. Clin Orthop Relat Res. 2010;468:1221–1228. doi: 10.1007/s11999-009-1204-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jain NB, Higgins LD, Ozumba D, Guller U, Cronin M, Pietrobon R, Katz JN. Trends in epidemiology of knee arthroplasty in the United States, 1990–2000. Arthritis Rheum. 2005;52:3928–3933. doi: 10.1002/art.21420. [DOI] [PubMed] [Google Scholar]
- 14.Jenny JY, Miehlke RK, Giurea A. Learning curve in navigated total knee replacement: a multi-centre study comparing experienced and beginner centres. Knee. 2008;15:80–84. doi: 10.1016/j.knee.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 15.Jones DL, Cauley JA, Kriska AM, Wisniewski SR, Irrgang JJ, Heck DA, Kwoh CK, Crossett LS. Physical activity and risk of revision total knee arthroplasty in individuals with knee osteoarthritis: a matched case-control study. J Rheumatol. 2004;31:1384–1390. [PubMed] [Google Scholar]
- 16.Kashyap SN, Ommeren JW, Shankar S. Minimally invasive surgical technique in total knee arthroplasty: a learning curve. Surg Innov. 2009;16:55–62. doi: 10.1177/1553350609331396. [DOI] [PubMed] [Google Scholar]
- 17.Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am. 2004;86:1909–1916. doi: 10.1302/0301-620X.86B7.14358. [DOI] [PubMed] [Google Scholar]
- 18.Keskimäki I, Aro S. Accuracy of data on diagnoses, procedures and accidents in the Finnish Hospital Discharge Register. Int J Health Sci. 1991;2:15–21. [Google Scholar]
- 19.Kim S. Changes in surgical loads and economic burden of hip and knee replacements in the US: 1997–2004. Arthritis Care Res. 2008;59:481–488. doi: 10.1002/art.23525. [DOI] [PubMed] [Google Scholar]
- 20.King J, Stamper DL, Schaad DC, Leopold SS. Minimally invasive total knee arthroplasty compared with traditional total knee arthroplasty: assessment of the learning curve and the postoperative recuperative period. J Bone Joint Surg Am. 2007;89:1497–1503. doi: 10.2106/JBJS.F.00867. [DOI] [PubMed] [Google Scholar]
- 21.Koskinen E, Eskelinen A, Paavolainen P, Pulkkinen P, Remes V. Comparison of survival and cost-effectiveness between unicondylar arthroplasty and total knee arthroplasty in patients with primary osteoarthritis: a follow-up study of 50, 493 knee replacements from the Finnish Arthroplasty Register. Acta Orthop. 2008;79:499–507. doi: 10.1080/17453670710015490. [DOI] [PubMed] [Google Scholar]
- 22.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 23.Lubowitz JH, Sahasrabudhe A, Appleby D. Minimally invasive surgery in total knee arthroplasty: the learning curve. Orthopedics. 2007;30(8 suppl):80–82. [PubMed] [Google Scholar]
- 24.Mahaluxmivala J, Bankes MJ, Nicolai P, Aldam CH, Allen PW. The effect of surgeon experience on component positioning in 673 Press Fit Condylar posterior cruciate-sacrificing total knee arthroplasties. J Arthroplasty. 2001;16:635–640. doi: 10.1054/arth.2001.23569. [DOI] [PubMed] [Google Scholar]
- 25.Manley M, Ong K, Lau E, Kurtz SM. Total knee arthroplasty survivorship in the United States Medicare population: effect of hospital and surgeon procedure volume. J Arthroplasty. 2009;24:1061–1067. doi: 10.1016/j.arth.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 26.Mont MA, Marker DR, Seyler TM, Gordon N, Hungerford DS, Jones LC. Knee arthroplasties have similar results in high- and low-activity patients. Clin Orthop Relat Res. 2007;460:165–173. doi: 10.1097/BLO.0b013e318042b5e7. [DOI] [PubMed] [Google Scholar]
- 27.Palan J, Gulati A, Andrew JG, Murray DW, Beard DJ, the EPOS study group The trainer, the trainee and the surgeons’ assistant: clinical outcomes following total hip replacement. J Bone Joint Surg Br. 2009;91:928–934. doi: 10.1302/0301-620X.91B7.22021. [DOI] [PubMed] [Google Scholar]
- 28.Price AJ, Rees JL, Beard D, Juszczak E, Carter S, White S, Steiger R, Dodd CA, Gibbons M, McLardy-Smith P, Goodfellow JW, Murray DW. A mobile-bearing total knee prosthesis compared with a fixed-bearing prosthesis: a multicentre single-blind randomised controlled trial. J Bone Joint Surg Br. 2003;85:62–67. doi: 10.1302/0301-620X.85B1.13233. [DOI] [PubMed] [Google Scholar]
- 29.Puolakka TJS, Pajamäki KJJ, Halonen PJ, Pulkkinen PO, Paavolainen P, Nevalainen JK. The Finnish Arthroplasty Register: report of the hip register. Acta Orthop Scand. 2001;72:433–441. doi: 10.1080/000164701753606608. [DOI] [PubMed] [Google Scholar]
- 30.Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg Am. 2003;85:259–265. doi: 10.2106/00004623-200302000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Robertsson O. Knee arthroplasty registers. J Bone Joint Surg Br. 2007;89:1–4. doi: 10.1302/0301-620X.89B1.18327. [DOI] [PubMed] [Google Scholar]
- 32.Robertsson O, Knutson K, Lewold S, Lidgren L. The Swedish Knee Arthroplasty Register 1975–1997: an update with special emphasis on 41, 223 knees operated on in 1988–1997. Acta Orthop Scand. 2001;72:503–513. doi: 10.1080/000164701753532853. [DOI] [PubMed] [Google Scholar]
- 33.Serra-Sutton V, Allepuz A, Espallargues M, Labek G, Pons JM. Arthroplasty registers: a review of international experiences. Int J Technol Assess Health Care. 2009;25:63–72. doi: 10.1017/S0266462309090096. [DOI] [PubMed] [Google Scholar]
- 34.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby S. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Shervin N, Rubash H, Katz JN. Orthopaedic procedure volume and patient outcomes: a systematic literature review. Clin Orthop Relat Res. 2007;457:35–41. doi: 10.1097/BLO.0b013e3180375514. [DOI] [PubMed] [Google Scholar]
- 36.SooHoo NF, Zingmond DS, Lieberman JR, Ko CY. Primary total knee arthroplasty in California 1991 to 2001: does hospital volume affect outcomes? J Arthroplasty. 2006;21:199–205. doi: 10.1016/j.arth.2005.03.027. [DOI] [PubMed] [Google Scholar]