Abstract
Background
The direct anterior approach in THA requires no detachment of muscle insertions. However, damage to the short external rotator muscles may occur when attempting to elevate the femur for exposure. Although the anatomic insertions of these muscles are approximately known, there are no quantitative data regarding their locations.
Questions/purposes
We therefore asked where and how the tendons attach to the inner aspect of the greater trochanter.
Methods
In 20 cadaveric hips we identified the attachments of the short external rotator tendons on the medial aspect of the greater trochanter. Mapping of the attachment site was performed by defining coordinate axes; the total width and height of the greater trochanter represented 100% and distances of the attachment from the anteroinferior reference point were given.
Results
The mean anterior border location of the conjoined tendon (obturator internus, gemellus superior, and gemellus inferior) attachment was located at 29% (13 mm from the anteroinferior reference point), its posterior border at 53% (23 mm), its mean superior border at 70% (15 mm), and its mean inferior border at 24% (5 mm). The mean anterior border of the piriformis tendon attachment was located at 57% (25 mm), its mean posterior border at 78% (34 mm), its mean superior border at 64% (17 mm), and its inferior border at 55% (12 mm). There was considerable variation in these attachment sites among individuals.
Conclusions
The insertion of the conjoined tendon extends to the anterosuperior aspect of the greater trochanter. Together with the considerable variation of the attachment site, external rotator muscles remain at risk of being damaged during the capsular release.
Introduction
Minimally invasive THA (MIS-THA) that minimizes soft tissue dissection reportedly reduces blood loss [3], does not increase complication rates [3, 6, 13], and improves early walking ability compared with conventional THA [3, 4]. Among the MIS-THA methods, the direct anterior approach (DAA) was modified from the Smith-Petersen approach and has become one of the standard procedures for primary THA [5, 13]. The DAA, which uses an intermuscular plane among the sartorius, rectus femoris, and tensor fasciae latae, does not dissect muscles around the hip and conserves the posterior tissue to a large extent, leading to improved stability and a reduced postoperative dislocation rate [6, 8, 11–13]. As a consequence, reduction of the dislocation rate and early postoperative functional recovery can be expected [10].
When performing DAA, detachment of the joint capsule at appropriate sites is indispensable to obtain a clearer visual field during surgery [8, 11]. However, despite careful capsular release and rasping, damage to muscles may occur [9], possibly eliminating one of the advantages of the approach. Furthermore, because of the limited surgical visual field in MIS-THA, there is a risk of prolonged operation time, unexpected soft tissue injury, unfavorable implant placement position, and fracture [1]. Anterior elevation of the proximal femur for a clearer visual field and femoral rasping may minimize these complications, and releasing of the posterolateral capsule or superior capsule has been advocated [7, 11]. However, such capsular dissection and femoral rasping may pose a risk of damaging the short external rotators. Therefore it is essential for surgeons to have detailed anatomic knowledge of the muscle attachment sites to minimize soft tissue damage during the anterior approach. Although the anatomy of the short external rotator muscles is approximately known [15], there is no detailed quantitative information regarding the location of their tendon insertions.
We therefore asked where and how the tendons attach to the inner aspect of the greater trochanter on defined horizontal and vertical axes.
Materials and Methods
We obtained 20 hips (11 right hips and nine left hips) from 16 embalmed cadavers (11 males and five females) donated for medical education and research. The cadaver specimens had a mean age of 84 years (range, 61–100 years) at the time of death and had no history of hip disease. Details of the antemortem weight and mobility status were not available, but the estimated height was 168 ± 8 cm for the male and 149 ± 6 cm for the female cadavers. Measured collodiaphyseal angle and neck anteversion were 126.0° ± 6.0° and 12.3° ± 5.1°, respectively. We removed the skin, fat, and soft tissues until only the gluteus medius, gluteus minimus, piriformis, obturator internus, obturator externus, gemellus superior, gemellus inferior, and capsular structures remained. After arthrotomy around the acetabular rim, the femur was disarticulated and the muscles were dissected so as to leave sufficient structures at the femoral insertion (Fig. 1). We then dissected the gluteus medius, obturator internus, gemellus superior, gemellus inferior, obturator externus, and remaining capsule with special attention to the connection between the tendons (Fig. 2A). When the tendons were integrated close to the insertion sites, the tendons were identified and separated bluntly based on their fiber orientation down to the attachment on the greater trochanter or trochanteric fossa. Subsequently, we partially cut the tendons with scissors to identify their footprints at the insertion and their peripheries were carefully marked with a pen. Osteotomy of the femoral neck at the saddle then was done (Fig. 2B-C).
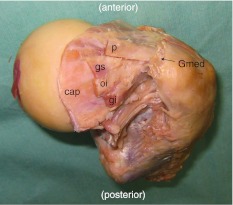
Fig. 1.
A posterosuperior view of the cadaveric dissection of the right hip shows the short external rotator muscles. p = piriformis; gs = gemellus superior; oi = obturator internus; gi = gemellus inferior; Gmed = gluteus medius; cap = capsule.
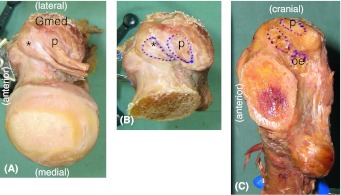
Fig. 2A–C.
The attachment site of the short external rotator muscles indicates their relative localization. (A) A superior view, (B) superior view and footprint of the tendon insertion, and (C) mediolateral view and footprint of the tendon insertion are shown. *Conjoined tendon of the gemellus superior, obturator internus, and gemellus inferior; p = piriformis; oe = obturator externus; Gmed = gluteus medius.
We measured the major and minor axes of the elliptical or scaphoid-shaped footprint of the tendon attachment using calipers. We then took high-resolution scaled digital photographs of each dissected specimen in a mediolateral direction from 50 cm away at a right angle to the femoral shaft. We determined eight points (anterior, posterior, superior, inferior, and midpoints between each of them) on the contour of the attachment footprint and recorded them using Adobe Photoshop CS2 software (Adobe Systems Inc, San Jose, CA, USA). In the mediolateral view of the femur, the proximal shaft axis was defined as the proximal femoral axis (Fig. 3A). At the level of the femoral neck saddle, an axis perpendicular to the proximal femoral axis was defined as the X-axis (AP axis). We defined an axis at the anterior border of the greater trochanter on the saddle level, parallel to the proximal femoral axis, as the Y-axis (vertical axis) (Fig. 3B). Their intersection was defined as 0. For mapping of the tendon attachment, the AP position was expressed in percentages with the anterior border as 0% and the posterior border as 100%. The vertical position of the tendon attachment was expressed with the saddle height as 0% and the vertex of the greater trochanter as 100% (Fig. 3B). The distance of each border in millimeters from the 0 reference point also was measured and the value was standardized with the mean width and height of the greater trochanter of the cadavers.
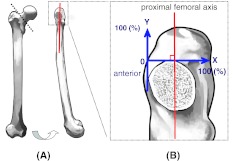
Fig. 3A–B.
The femoral axis and coordinate axis used for measurement are shown. In the mediolateral view of the femur, the anterior border of the greater trochanter parallel to the proximal femoral axis was defined as the Y-axis and its perpendicular axis at the saddle level was defined as the X-axis. (A) An AP view of the right femur is shown on the left and a mediolateral view is shown on the right. (B) The coordinate axis for measurement of tendon attachment is shown.
We used Spearman’s rank correlation to identify relationships among the anterior border of the tendon attachment site, neck anteversion angle, and the width and height of the greater trochanter.
Results
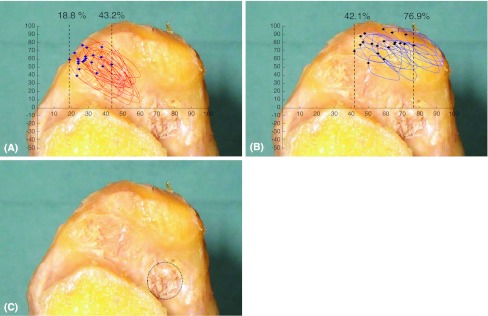
Three muscles of the short external rotators, obturator internus, gemellus superior, and gemellus inferior, formed a conjoined tendon and attached anteriorly of the medial aspect of the greater trochanter. On the coordinate axes, the anterior border of the conjoined tendon attachment site ranged from 19% (9 mm) to 43% (23 mm), the posterior border ranged from 39% (18 mm) to 60% (30 mm), the superior border ranged from 48% (8 mm) to 86% (21 mm), and the inferior border ranged from 4% (1 mm) to 40% (9 mm) (Table 1). The footprint of the conjoined tendon insertion was elliptical or scaphoid-shaped with a mean size of 12.8 (± 2.5) mm × 4.3 (± 1.2) mm. As shown in the superimposed drawing of the attachment site of each specimen (Fig. 4A), there was variation in the position of the conjoined tendon attachment in the horizontal and vertical directions. The attachment site of the piriformis was posterosuperior to that of the conjoined tendon. On the coordinate axes, the anterior border of the piriformis attachment site ranged from 42% (16 mm) to 77% (36 mm), the posterior border ranged from 59% (23 mm) to 97% (46 mm), the superior border ranged from 65% (10 mm) to 99% (24 mm), and the inferior border ranged from 34% (7 mm) to 79% (17 mm) (Table 1). The size of the attachment footprint was 10.3 (± 1.6) mm × 4.7 (± 1.1) mm and the superimposed attachment sites indicated the degree of their variation (Fig. 4B). The obturator externus attached independently to a fossa located posteroinferior to the other short external rotator muscles (Fig. 4C). Its attachment site was relatively constant; on the coordinate axes, the anterior border ranged from 49% (20 mm) to 70% (34 mm), the posterior border ranged from 66% (23 mm) to 83% (39 mm), the superior border ranged from −19% (−2 mm) to 33% (7 mm), and the inferior border ranged from −59% (−7 mm) to 6% (1 mm) (Table 1).
Table 1.
Mapping of attachment sites
| Tendon | Attachment border | Mean ± SD (range) (%) | |
|---|---|---|---|
| Conjoined tendon* | X axis | Anterior | 29.1 ± 6.4 (18.8–43.2) |
| Posterior | 52.8 ± 5.1 (38.9–59.9) | ||
| Y axis | Superior | 70.2 ± 8.4 (48.1–85.7) | |
| Inferior | 24.3 ± 10.1 (3.8–40.2) | ||
| Piriformis | X axis | Anterior | 57.4 ± 10.2 (42.1–76.9) |
| Posterior | 78.4 ± 11.9 (59.4–97.3) | ||
| Y axis | Superior | 64.3 ± 9.4 (64.9–98.5) | |
| Inferior | 55.1 ± 11.3 (34.3–74.8) | ||
| Obturator externus | X axis | Anterior | 61.3 ± 6.5 (48.6–70.1) |
| Posterior | 75.9 ± 5.8 (65.6–83.0) | ||
| Y axis | Superior | 10.6 ± 12.7 (−19.0–33.3) | |
| Inferior | −18.7 ± 18.6 (−59.0–6.3) | ||
* Obturator internus, gemellus superior, and gemellus inferior.
Fig. 4A–C.
Superimposed footprints of the attachment of the short external rotator muscles on the inner aspect of the greater trochanter are shown. (A) The attachment of the conjoined tendon (obturator internus, gemellus superior, and gemellus inferior) for 20 hips is shown. The plot highlights the most anterior part of the attachment in each specimen to show its variation of 18.8% to 43.2% from the anterior border of the greater trochanter. (B) The attachment of the piriformis for 20 hips is shown. The plot highlights the most anterior part of the attachment in each specimen. (C) The dotted line indicates the attachment site of the obturator externus to a fossa.
No significant correlation was found between the anterior border (X value) of the conjoined tendon attachment and neck anteversion angle (p = 0.12), the width of the greater trochanter (p = 0.25), or the height of the greater trochanter (p = 0.82). In addition, the anterior border (X value) of the piriformis attachment did not show significant correlation with neck anteversion angles (p = 0.73), the width of the greater trochanter (p = 0.74), or the height of the greater trochanter (p = 0.36).
Discussion
Detailed knowledge of the anatomy of tendon attachment is a prerequisite for less invasive THA and attempts should be made to preserve soft tissue, including the short external rotator muscles. MIS-THA using an intermuscular approach has been reported [2, 13]. However, unless capsular dissection and femoral rasping are performed carefully, the short external rotators might be injured. It therefore is important to have improved knowledge of the anatomic positions of the tendon attachment sites.
Readers should know the limitations of our study. First, our study was limited by sample size as a result of the difficulty in obtaining a large number of embalmed cadavers. Second, we did not have detailed information regarding body size and could not correlate quantitative anatomy with body size. However, the position of the tendon attachment site, when shown as a relative value on the coordinate axes, apparently was not influenced by skeletal size difference. Third, with a smaller sample size of female and bilateral hip cadavers, our study was underpowered to analyze possible gender differences or intraspecimen variance. Additional study is needed to investigate such variance, if any. Fourth, the study is limited to the measurement of morphologic hip features in Japanese subjects. It is possible that ethnic difference in bony geometry may be associated with variation of the tendon attachment. However, we believe these quantitative data supplement what generally is known about the locations of the short external rotator muscle attachments.
The general gross anatomy and approximate insertion of the short external rotator muscles to the greater trochanter have been approximately known, but detailed quantitative locations of the attachment sites are not known. Standard anatomy textbooks only indicate the insertion to be the upper medial side of the greater trochanter [15] and do not provide specific information regarding the attachment site. Windisch et al. [17] provided details regarding the anatomy of the musculotendinous junction and fusion of short external rotator muscles. Solomon et al. [14] reported that the piriformis inserted onto the greater trochanter through a conjoint tendon with the obturator internus. Nevertheless, the location of the attachment of each tendon on the inner aspect of the greater trochanter still remained obscure. Our observations show the accurate location of the greater trochanteric attachments of the short external rotator muscles (a conjoined tendon, piriformis, and obturator externus) and their positional relation for the first time.
We found both attachment sites of the conjoined tendon and piriformis were considerably more variable among individuals than had been thought. Based on the mapping data, the conjoined tendon of the short external rotators may attach as anteriorly as 19% (or 9 mm from the anteroinferior reference point) of the horizontal width of the greater trochanter and as low as 4% (1 mm) of the medical height of the greater trochanter from the saddle in certain individuals. These observations suggest preservation of the short external rotator muscles may not always be possible during capsular release in the DAA. The piriformis also can be damaged depending on its attachment variation during capsular release or femoral rasping. This is consistent with the study of Meneghini et al. [9] that showed the need for transection of the piriformis or the conjoined tendon of the obturator internus and gemelli in 50% of the cases during the anterior Smith-Petersen approach.
Thus, the short external rotators, especially the conjoined tendon, are at a high risk of being damaged and their detachment might be inevitable during the superior and/or posterior capsular release that is necessary to mobilize the femur during DAA in certain cases. The importance of preservation of the short external rotators for postoperative hip stability has been documented for other approaches such as the posterior approach [16]. The question remains whether a partial release of the short external rotator muscle during DAA would affect the postoperative stability of the hip. In addition, further study is needed to see the potential influence of morphologic features of a diseased hip, such as coxa vara and valga, on alteration of anatomic tendon attachment.
We report the quantitative locations of the anatomic attachment of the short external rotators of the hip. We showed that the tendons are at a risk of being damaged during capsular release. Improved anatomic knowledge of the short external rotators will assist surgeons in accurately locating these structures.
Acknowledgments
We thank Dr Ryuich Gejo, Dr Kazuhito Sugimori, and Dr Hiraku Motomura for their assistance and contribution in data collection and analysis. We also thank Dr Osamu Ohtani for help during anatomic analysis.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution either has waived or does not require approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Berry DJ. ‘Minimally invasive’ total hip arthroplasty. J Bone Joint Surg Am. 2005;87:699–700. doi: 10.2106/JBJS.E.00126. [DOI] [PubMed] [Google Scholar]
- 2.Bertin KC, Rottinger H. Anterolateral mini-incision hip replacement surgery: a modified Watson-Jones approach. Clin Orthop Relat Res. 2004;429:248–255. doi: 10.1097/01.blo.0000150294.81825.8c. [DOI] [PubMed] [Google Scholar]
- 3.Chimento GF, Pavone V, Sharrock N, Kahn B, Cahill J, Sculco TP. Minimally invasive total hip arthroplasty: a prospective randomized study. J Arthroplasty. 2005;20:139–144. doi: 10.1016/j.arth.2004.09.061. [DOI] [PubMed] [Google Scholar]
- 4.DiGioia AM, 3rd, Plakseychuk AY, Levison TJ, Jaramaz B. Mini-incision technique for total hip arthroplasty with navigation. J Arthroplasty. 2003;18:123–128. doi: 10.1054/arth.2003.50025. [DOI] [PubMed] [Google Scholar]
- 5.Judet J, Judet H. Anterior approach in total hip arthroplasty] [in French. Presse Med. 1985;14:1031–1033. [PubMed] [Google Scholar]
- 6.Kennon RE, Keggi JM, Wetmore RS, Zatorski LE, Huo MH, Keggi KJ. Total hip arthroplasty through a minimally invasive anterior surgical approach. J Bone Joint Surg Am. 2003;85(suppl 4):39–48. doi: 10.2106/00004623-200300004-00005. [DOI] [PubMed] [Google Scholar]
- 7.Matsuura M, Ohashi H, Okamoto Y, Inori F, Okajima Y. Elevation of the femur in THA through a direct anterior approach: cadaver and clinical studies. Clin Orthop Relat Res. 2010;468:3201–3206. doi: 10.1007/s11999-010-1349-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matta JM, Shahrdar C, Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res. 2005;441:115–124. doi: 10.1097/01.blo.0000194309.70518.cb. [DOI] [PubMed] [Google Scholar]
- 9.Meneghini RM, Pagnano MW, Trousdale RT, Hozack WJ. Muscle damage during MIS total hip arthroplasty: Smith-Petersen versus posterior approach. Clin Orthop Relat Res. 2006;453:293–298. doi: 10.1097/01.blo.0000238859.46615.34. [DOI] [PubMed] [Google Scholar]
- 10.Nakata K, Nishikawa M, Yamamoto K, Hirota S, Yoshikawa H. A clinical comparative study of the direct anterior with mini-posterior approach: two consecutive series. J Arthroplasty. 2009;24:698–704. doi: 10.1016/j.arth.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 11.Nogler M, Krismer M, Hozack WJ, Merritt P, Rachbauer F, Mayr E. A double offset broach handle for preparation of the femoral cavity in minimally invasive direct anterior total hip arthroplasty. J Arthroplasty. 2006;21:1206–1208. doi: 10.1016/j.arth.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 12.Oinuma K, Eingartner C, Saito Y, Shiratsuchi H. Total hip arthroplasty by a minimally invasive, direct anterior approach. Oper Orthop Traumatol. 2007;19:310–326. doi: 10.1007/s00064-007-1209-3. [DOI] [PubMed] [Google Scholar]
- 13.Siguier T, Siguier M, Brumpt B. Mini-incision anterior approach does not increase dislocation rate: a study of 1037 total hip replacements. Clin Orthop Relat Res. 2004;426:164–173. doi: 10.1097/01.blo.0000136651.21191.9f. [DOI] [PubMed] [Google Scholar]
- 14.Solomon LB, Lee YC, Callary SA, Beck M, Howie DW. Anatomy of piriformis, obturator internus and obtrator externus: implications for the posterior surgical approach to the hip. J Bone Joint Surg Br. 2010;92:1317–1324. doi: 10.1302/0301-620X.92B9.23893. [DOI] [PubMed] [Google Scholar]
- 15.Standring S. Gray’s Anatomy: The Anatomical Basis of Clinical Practice. Edinburgh, UK: Churchill Livingstone; 2008. [Google Scholar]
- 16.White RE, Jr, Forness TJ, Allman JK, Junick DW. Effect of posterior capsular repair on early dislocation in primary total hip replacement. Clin Orthop Relat Res. 2001;393:163–167. doi: 10.1097/00003086-200112000-00019. [DOI] [PubMed] [Google Scholar]
- 17.Windisch G, Braun EM, Anderhuber F. Piriformis muscle: clinical anatomy and consideration of the piriformis syndrome. Surg Radiol Anat. 2007;29:37–45. doi: 10.1007/s00276-006-0169-x. [DOI] [PubMed] [Google Scholar]