Abstract
Background
The benefits of postoperative mobilization include decreased incidence of pulmonary complications, pressure ulcers, and progression of deep vein thrombosis. However, the complexity of certain spinal reconstructions and the patient’s physiologic condition may preclude the possibility of early mobilization. Prolonged bed rest after spine surgery is controversial.
Questions/purposes
We evaluated the efficacy of prolonged bed rest after complex spine surgery to determine (1) patient characteristics that led to prescribing bed rest, (2) clinical and radiographic outcomes, (3) complications, and (4) estimated direct costs.
Methods
We retrospectively reviewed all 11 patients (median age, 50 years) who underwent complex spine surgery followed by prolonged bed rest between 2005 and 2010. All patients were deemed at high risk for developing pseudarthrosis or instrumentation failure without postoperative bed rest. One patient died of complications related to pulmonary tuberculosis at 4 months. The patients averaged 3 months of bed rest. Minimum followup was 24 months (median, 30 months; range, 4–52 months).
Results
All patients had (1) tenuous or limited fixation after correction of severe deformity, (2) previously failed spine reconstruction after early mobilization, or (3) limited treatment options if failure occurred again. No patient experienced pseudarthrosis, failure of instrumentation, thromboembolic disease, pressure ulcers, or pneumonia. One patient had a delayed union and one developed late urosepsis. The median cost of skilled nursing facilities during the period of bed rest was $16,702, while the median cost of home health nursing was $5712.
Conclusions
For patients with contraindications to early postoperative mobilization, prolonged bed rest may be useful to minimize the risk of complications that can occur with mobilization.
Level of Evidence
Level IV, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
The benefits of early mobilization after surgery are well documented. These benefits include reduced risk of pneumonia, pulmonary failure, cardiovascular complications, perioperative infection, pressure ulcers, and progression of deep vein thrombosis (DVT) [1, 20, 22]. Moreover, early spinal stabilization and mobilization have been associated with an almost eightfold decreased risk of complications related to prolonged recumbency [20]. These complications include pneumonia, respiratory failure, DVT, and pulmonary embolus. For example, compared to delayed spinal stabilization and mobilization, the rates of pneumonia have been reduced from 20% to 4% [20] and the rates of pulmonary failure have been reduced from 18% to 9% [20]. However, the complexity of a spinal reconstructive procedure and the overall physiologic condition of a particular patient (eg, bone quality, medical comorbidities, and the severity of the spinal deformity) may render early mobilization unfeasible and long-term postoperative bed rest a useful adjuvant therapy, as evidenced by improvement in physical function, decreased pain, and radiographic evidence of healing [16, 18].
Short-term bed rest is a well-documented primary and adjuvant method of treatment for spinal and musculoskeletal conditions. Two days of bed rest is usually sufficient for the treatment of acute low back pain [7]. Four weeks of postoperative bed rest reportedly improves the maintenance of sagittal alignment of patients with thoracolumbar burst fractures treated with spinal fusion and instrumentation [5] compared to spinal fusion and instrumentation with early mobilization. Moreover, some authors reported nonoperative treatment with 4 to 6 weeks of recumbence followed by mobilization with a brace was generally superior to surgical approaches in treating spinal injuries [23]. However, the potential benefits of more prolonged bed rest are unclear.
The adverse physiologic effects of prolonged bed rest on muscle and bone are also well documented. Muscle at complete rest can lose 10% to 15% of its strength per week of immobilization [9]. The muscles of the lower extremities are often the first to reveal signs of atrophy [3], but spinal muscle atrophy is also substantial: atrophy of the multifidus and erector spinae muscles may occur after 60 days of bed rest [3]. The cross-sectional area of the multifidus decreases after 8 weeks of bed rest, which may destabilize the spine [12]. In addition, there are structural changes in bone that are directly related to the duration of immobilization. These changes are consistent with other scenarios leading to disuse osteopenia and may cause substantial cortical thinning and trabecular bone loss [24]. The reduction in bone mass may, in turn, increase the risk for pseudarthrosis. In addition to causing long-term physiologic deterioration of muscle and bone, bed rest has been associated with other systemic complications. Insulin resistance, pressure ulcers, pneumonia, thromboembolic disease, cardiac atrophy with decreased stroke volume and orthostatic intolerance, and changes in microvascular structure have all been associated with prolonged immobilization [4, 6, 9, 12, 24, 26, 28].
We therefore investigated the efficacy of a controversial adjuvant treatment option: prolonged bed rest after major reconstructive spine surgery for patients at high risk for developing postoperative failure of spinal instrumentation, progressive deformity, pseudarthrosis, or life-threatening complications if further surgery is required to resolve these problems. Treatment efficacy was defined as successful, albeit delayed, upright mobilization without serious side effects during the period of prolonged bed rest. To determine the efficacy of prolonged postoperative bed rest as adjuvant therapy, we evaluated (1) the characteristics of the patients that led to prescribing prolonged bed rest after major reconstructive spine surgery; (2) clinical evidence of healing, ie, decreased pain and improved function; (3) radiographic evidence of healing on plain radiographs and CT scans; (4) associated complications; and (5) estimated direct costs.
Patients and Methods
After institutional review board approval was obtained, we retrospectively reviewed the surgical records of a single fellowship-trained spine surgeon (RAWM) to identify all 11 patients treated with prolonged bed rest in the postoperative course of their therapy during the years 2005 to 2010. Prolonged (at least 2 months) postoperative bed rest was prescribed. The median age of the patients (five men, six women) was 50 years (range, 27–73 years). All patients had a minimum followup of 24 months except one patient who died of complications related to his pulmonary tuberculosis. Median followup was 30 months (range, 4–52 months). All 11 patients presented with multiple diagnoses, and six of 11 presented with neurologic deficits (Table 1).
Table 1.
Patient characteristics, diagnoses, and surgical approaches to complex spine deficiencies
| Patient | Sex | Age (years) | Diagnoses | Number of previous surgeries | Neurologic symptoms | Surgical approach |
|---|---|---|---|---|---|---|
| 1 | Male | 65 | Positive sagittal imbalance; L5-S1 pseudarthrosis | 2 | None | Staged PSF T10-pelvis |
| 2 | Male | 70 | L4-5 MRSA osteomyelitis and discitis; fractured instrumentation | 2 | None | Instrumented PSF L3-pelvis |
| 3 | Female | 42 | AIS; sagittal imbalance; coronal imbalance; osteomyelitis; pseudarthrosis; fractured instrumentation | 4 | None | ASF L2-3, 3-4, revision PSF T2-pelvis |
| 4 | Female | 27 | L5-S1 kyphosis; L5-S1 spondylolisthesis; chondrosarcoma (previously treated with hemipelvectomy) | 1 | None | L2-pelvis revision PSF |
| 5 | Female | 50 | Pseudarthrosis; positive sagittal imbalance | 2 | None | T4-pelvis revision PSF |
| 6 | Male | 73 | Spinal tuberculosis involving the L1-2 spinal segment; spinal cord compression; paraparesis | 0 | Progressive paraparesis | Staged ASF with L1-2 corpectomy and T10-L5 PSF |
| 7 | Female | 63 | Osteomyelitis L3 and L4 vertebral bodies; L3-4 discitis | 0 | Progressive paraparesis | ASF L2-5 |
| 8 | Male | 48 | L5 and S1 osteomyelitis; quadriplegia | 1 | Quadriplegia | ASF with L5 corpectomy, L3-pelvis PSF |
| 9 | Female | 49 | AIS; positive sagittal imbalance; coronal imbalance; pseudoarthrosis L3-4; fractured instrumentation | 4 | Bilateral lower-extremity radicular symptoms | Staged T12-pelvis, L4 PSO |
| 10 | Female | 55 | Failed back syndrome; lumbar scoliosis; positive sagittal imbalance; S1-2 fracture; osteoporosis | 5 | Bilateral lower-extremity radicular symptoms | Staged T4-L4 PSF revision L5-S1 PSF, L2-4 ASF L3 corpectomy |
| 11 | Male | 27 | Neurofibromatosis; dural ectasia L3, L4, L5, S1, S2 | 0 | Left lower-extremity radicular symptoms | T12-pelvis with myocutaneous flap closure |
MRSA = methicillin-resistant Staphylococcus aureus; AIS = adolescent idiopathic scoliosis; PSF = posterior spinal fusion; ASF = anterior spinal fusion; PSO = pedicle subtraction osteotomy.
We evaluated the total number of previous spine operations, neurologic status, duration of bed rest, and complications. All patients were at high risk for developing progressive deformity, failure of instrumentation, or pseudarthrosis if early upright mobilization was instituted.
Seven patients were treated with a planned staged surgical approach with stages separated by a median of 4 days (range, 3–21 days) (Table 1). Six patients underwent a posterior spinal fusion with instrumentation with a combination of transverse and pedicle subtraction osteotomies. Five patients underwent a combined anterior and posterior instrumented fusion; of these five patients, four had a corpectomy during the anterior portion.
Bed rest was instituted immediately postoperatively. Occupational and physical therapy consultations were obtained during the period of acute postoperative hospitalization. All patients were transferred to skilled nursing facilities or in-home assisted living at a mean of 6 days (range, 2–11 days) for the duration of the prolonged bed rest. Patients were deemed clinically stable when they had normal vital signs, electrolytes, and hemoglobin without clinical signs of wound or systemic complications. Patients (as well as their caregivers) were advised to avoid supine positioning during the initial 4 weeks to decrease direct pressure on the posterior wound. Use of strict log-rolling technique was prescribed; patients were allowed to raise the head of bed up to 40° during meals; and bedpans and urinals were used. To help prevent the patients’ twisting and pulling with the upper extremities, overhead trapezes were prohibited.
Throughout the bed rest period, each patient received mechanical DVT prophylaxis, which consisted of the use of thromboembolic deterrent (TED) hose and thigh-high sequential compression devices while in the hospital and TED hose after discharge. Venous duplex ultrasonography was ordered for all patients on Postoperative Days 3 and 14; in none of the 11 patients was DVT detected by the procedure. Three patients elected to have an inferior vena cava (IVC) filter placed postoperatively, while one patient had an IVC filter placed preoperatively. None of the patients developed symptomatic pulmonary emboli. Chemical thromboembolic prophylaxis was not routinely used. However, one patient received prophylactic warfarin (Coumadin®; Bristol-Myers Squibb, New York, NY, USA) and one patient received prophylactic, subcutaneous low-molecular-weight heparin during the bed rest period. After spine surgery, the patients were treated with a median of 3 months (range, 2–6 months) of bed rest.
All patients were instructed to proceed with upright mobilization after completing the prescribed period of bed rest: progressive periods of prolonged sitting for patients who could only be mobilized using a wheelchair and progressive periods of sitting, standing, and walking for patients who were ambulatory.
After discharge from the hospital, patients were seen at 6 weeks, 3 months, 6 months, 12 months, and 24 months postoperatively. Plain radiographs were obtained at each visit to evaluate for evidence of instrumentation failure or failure of fixation, and CT scans were performed within a week of surgery to evaluate the placement of the instrumentation and before mobilizing to detect any evidence of fusion. An interbody was considered fused if there was trabecular bone in continuity bridging between the adjacent vertebral endplates as described by Wang et al. [29]. Posterolateral fusion was determined using the classification described by Lenke et al. [15]. Patients were allowed to mobilize when either interbody fusion was identified or solid big trabeculated bilateral fusion masses (Grade A) or a unilateral large fusion mass with contralateral small fusion mass (Grade B) was identified posterolaterally. All radiographs and CT scans were independently reviewed by two of us (RAWM, RMS).
From the charts, we extracted the total number of previous spine operations, neurologic status, length of bed rest, and complications. Complications were assessed based on the classification of surgical complications as outlined by Dindo et al. [8]. We used a 10-point VAS to assess pain [18, 30], whole-body pain diagrams [21], and patient questionnaire [18, 30] to assess functional outcomes related to pain, narcotic use, symptoms of depression, and work status. Patients were also asked to evaluate their functional status at their latest followup compared to their preoperative levels.
We used a t-test (SPSS® Version 18; IBM Corp, Chicago, IL, USA) to determine differences in VAS pain score from preoperatively to last followup.
Results
All patients treated with prolonged bed rest after complex spine surgery had one or more of the following characteristics: (1) tenuous or limited fixation after correction of severe sagittal or coronal imbalance (Fig. 1), (2) previously failed complex spine reconstruction with instrumentation and attempted early mobilization, or (3) limited treatment options if failure of complex spine reconstruction occurred (Fig. 2). All 11 patients were at high risk for developing progressive deformity, failure of instrumentation, or pseudarthrosis if early upright mobilization had been instituted (Table 2).
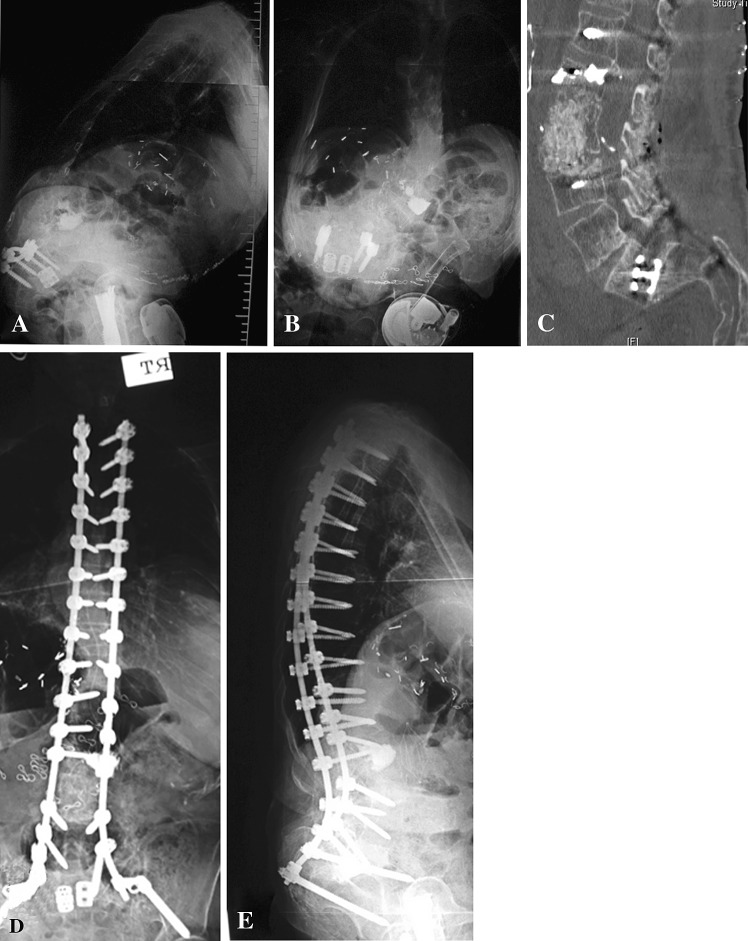
Fig. 1A–E.
(A) A lateral radiograph shows the spine of a 55-year-old woman who presented with progressive back pain, osteoporosis, and severe sagittal imbalance after multiple previous operations on her spine. (B) An AP radiograph demonstrates scoliosis and coronal imbalance. (C) A sagittal CT scan shows the spine after a decancellation procedure at L2. (D) An AP radiograph shows the spine after posterior, anterior, posterior spinal fusion and instrumentation to the pelvis. Twelve weeks of prophylactic bed rest was prescribed because of her high likelihood to develop failure of her tenuous fixation and limited treatment options in the event of failure of this procedure. (E) A lateral radiograph at last followup demonstrates adequate sagittal alignment.
Fig. 2A–E.
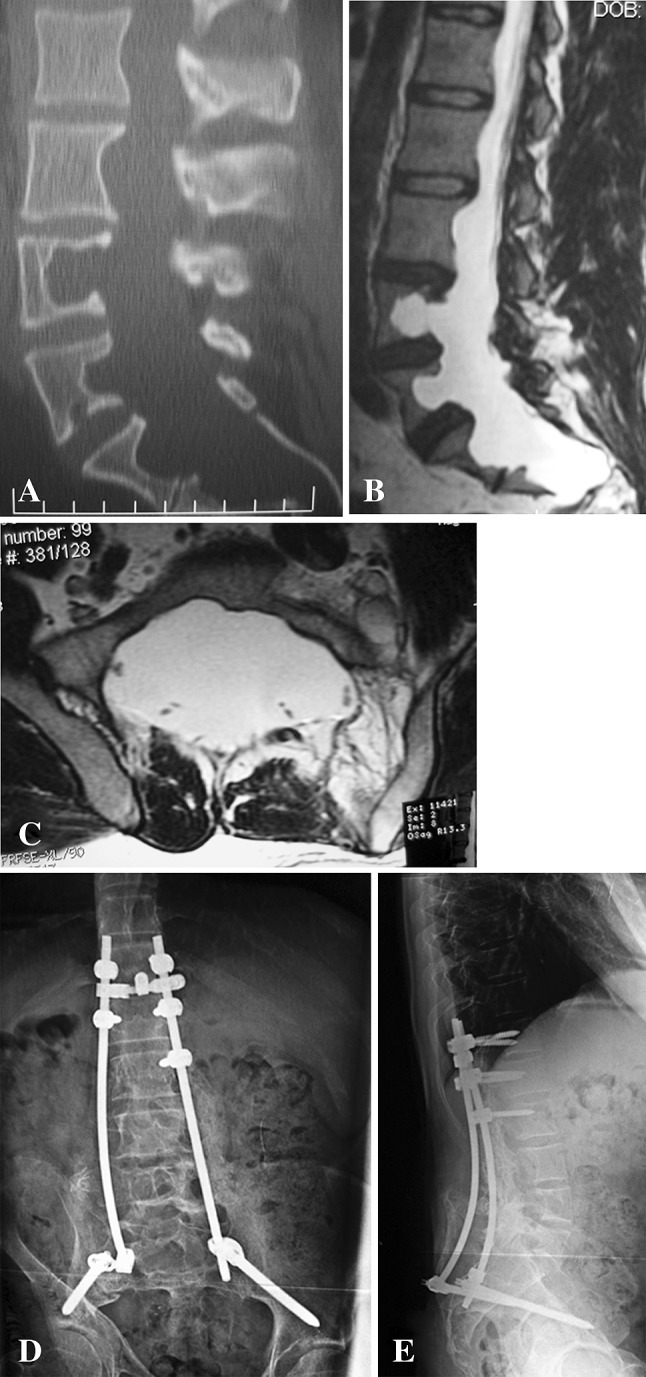
(A) A sagittal CT scan shows the spine of a 29-year-old man with neurofibromatosis and multilevel duralectasia who had presented with severe disabling pain with ambulation. (B) A sagittal T2-weighted MR image demonstrates duralectasia with erosion of the middle column of the L3, L4, L5, S1, and S2 vertebral bodies. (C) An axial T2-weighted MR image at S1 demonstrates severe duralectasia. (D) An AP plain radiograph shows the spine after posterior spinal fusion with instrumentation from T12 to the pelvis. Postoperative prophylactic bed rest was prescribed for 3 months due to the limited fixation, high risk of pseudarthrosis, and limited treatment options in the event of failure of this procedure. (E) A lateral plain radiograph at last followup when he was ambulating without assistive devices and plain radiographs showed maintenance of alignment without fractures of the bone, failure of instrumentation, or failure of fixation of the instrumentation.
Table 2.
Bed rest parameters and treatment results
| Patient | Reason for bed rest* | Bed rest duration (days) | Complications of bed rest | Followup (months) | Change in pain | Change in function | Radiographic evidence of healing |
|---|---|---|---|---|---|---|---|
| 1 | 2, 3 | 126 | Delayed union | 24 | Decreased | Increased | Yes |
| 2 | 1, 3 | 84 | None | 24 | Decreased | Increased | Yes |
| 3 | 2 | 84 | None | 41 | Decreased | Increased | Yes |
| 4 | 1, 3 | 84 | None | 32 | Decreased | Increased | Yes |
| 5 | 3 | 112 | None | 30 | Decreased | Increased | Yes |
| 6 | 3 | 56 | None | 4 | Decreased | Decreased | Yes |
| 7 | 2, 3 | 280 | Late urosepsis and adjacent-level infection | 24 | Decreased | Increased | Yes |
| 8 | 1, 3 | 168 | None | 52 | Decreased | Increased | Yes |
| 9 | 2, 3 | 112 | None | 30 | Decreased | Increased | Yes |
| 10 | 1, 2, 3 | 84 | None | 48 | Decreased | Increased | Yes |
| 11 | 1, 3 | 84 | None | 52 | Decreased | Increased | Yes |
* 1 = tenuous or limited fixation after correction of severe sagittal or coronal imbalance; 2 = previously failed complex spine reconstruction with attempted early mobilization; 3 = limited treatment options if failure of complex spine reconstruction had occurred.
The mean pain level decreased (p < 0.001) at last followup compared to preoperatively: VAS 4 versus 8, respectively. At last followup, 10 of the 11 patients reported decreased pain and improved function. Nine of the 11 patients were unemployed before surgery and all nine of these patients remain unemployed. One of the patients employed preoperatively returned to work, while one patient became unemployed. All 11 patients had radiographic evidence of healing at last followup, and all maintained coronal and sagittal alignment. No patient developed failure of instrumentation or instrument fixation.
Two patients developed complications during the period of prolonged bed rest. Patient 1 had delayed union (Grade 1), and Patient 7 developed urosepsis (Grade 4). Patient 1 had a previous attempt to repair a pseudarthrosis at L5-S1 and a positive sagittal balance of 35 cm. Despite complete surgical correction of his sagittal imbalance, prolonged bed rest was prescribed because the patient previously failed complex spine reconstruction with attempted early mobilization, and there were limited treatment options if reconstruction failed again. Additionally, the potential for normal healing in this patient appeared diminished because the L5 and S1 endplates were extremely sclerotic despite aggressive endplate preparation. CT scan demonstrated delayed union of the L5-S1 anterior fusion at the 12-month followup evaluation but ultimately demonstrated fusion on CT scan at the 24-month followup. Patient 7 was initially treated with 6 months of bed rest. She developed urosepsis 11 months after her operation and subsequently developed an infection at a level adjacent to her anterior construct. This patient had progressive paraparesis and osteomyelitis secondary to methicillin-resistant Staphylococcus aureus at the time of her initial presentation. She underwent a two-level corpectomy, with titanium mesh reconstruction and single-rod anterior spinal instrumentation from L2 to L5, and had been scheduled to then undergo a posterior spinal fusion and instrumentation. However, she sustained a hypotensive episode upon positioning in the prone position, perhaps due to volume shifting to her massive pannus protruding through the frame of the Jackson table. The hypotension resolved after the patient was returned to the supine position. Postoperative bed rest was prescribed due to the limited fixation and limited treatment options if failure of the anterior spinal fusion had occurred. This patient mobilized to a wheelchair after 6 months of bed rest. A Pseudomonas urosepsis infection then seeded the L2-3 disc space 11 months after the index operation. Anterior débridement of L2-3 and anterior spinal fusion without instrumentation were followed by posterior spinal fusion and instrumentation from T10 to the pelvis. The patient who had been followed for 4 months before he died had succumbed to complications related to an underlying tuberculosis infection. There were no documented reports of superficial or deep wound infections, DVTs, pressure ulcers, wound breakdown, or hospital-acquired pneumonia throughout the prolonged period of bed rest. One patient developed symptoms of depression during bed rest, and one had symptoms of depression preoperatively and throughout the bed rest period. Both of these patients denied symptoms of depression at last followup.
The average daily rate for a private nursing home in our region is $164 per day, while the average hourly rate for home health nursing is $34 per hour. Six of our patients completed the period of bed rest in a skilled nursing facility at an estimated median cost of $16,702; four completed it at home with the assistance of home health nursing at an estimated median cost of $5712; and one completed it at home without home health nursing.
Discussion
Prolonged bed rest has been used to treat patients with thoracolumbar fractures, scoliosis, spondylolisthesis, and tuberculosis [2, 17, 30, 31]. The use of modern spinal instrumentation has reportedly reduced the recumbency time and complications after surgery [13]. Early mobilization has also been associated with decreased likelihood of developing minor and major complications after spine surgery [20]. However, the complexity of certain spinal reconstructions and the overall physiologic condition of the patient may preclude the possibility of early mobilization. To determine the efficacy of prolonged postoperative bed rest after complex spine surgery, we evaluated (1) the characteristics of the patients that led to prescribing prolonged bed rest after major reconstructive spine surgery; (2) clinical evidence of healing, ie, decreased pain and improved function; (3) radiographic evidence of healing on plain radiographs and CT scans; (4) associated complications; and (5) estimated direct costs.
We acknowledge the limitations of our study. First is the lack of a comparable cohort of patients treated with early postoperative mobilization. It is thus impossible to determine whether prolonged bed rest provides improved fusion or decreased instrumentation failure, compared to early postoperative mobilization for this select group of patients. It is possible these patients may have had similar clinical improvement in function and radiographic evidence of healing if early mobilization was instituted. However, every patient in this study was deemed to be at high risk for failure of instrumentation or fusion because of the complex spinal surgery required to correct the underlying deformity or infection, combined with severe osteoporosis or poor fixation. Moreover, several patients had no other reasonable treatment options in the event of failure of this final attempt at spine reconstruction. Direct comparison of a cohort of patients treated with early postoperative mobilization seems imprudent, since the potential risks of reoperation and failure of fixation or fusion appear to greatly outweigh the potential risks of bed rest in patients who meet the inclusion criteria for postoperative prolonged bed rest. Second, we had limited methods to assess function. We used a VAS for pain, whole-body pain diagrams, and patient questionnaires to assess functional outcomes related to pain, narcotic use, symptoms of depression, and work status. However, more rigorous methodology for assessing function was not performed, which complicates direct comparison of our results to other studies. Third was the controversial use of CT scan evidence of healing before allowing mobilization. It is possible enough healing could have occurred to allow these patients to mobilize earlier; however, we believed it was prudent to continue bed rest until some evidence of bone healing was noted before mobilization.
Ordinarily, the use of spinal instrumentation should provide enough stability to allow patients to mobilize early while maintaining alignment and achieving acceptable fusion rates. The initial intent of our treatment was early postoperative mobilization. However, three primary factors contributed to our belief that early mobilization would lead to failure of the instrumentation or fusion: (1) tenuous or limited fixation after correction of severe sagittal or coronal imbalance, (2) previous failure of complex spine reconstruction with instrumentation and attempted early mobilization, and (3) limited treatment options if complex spine reconstruction failed again. All patients had one or more of these risk factors. Early mobilization after the planned complex reconstruction of the spine would have dramatically increased the likelihood of these patients developing progressive deformity, failure of instrumentation, or pseudarthrosis. For these reasons, the potential benefits of prolonged bed rest appeared to greatly outweigh the potential risks for these 11 patients. Similarly, patients with unstable fractures, high-grade spondylolisthesis, and severe tuberculosis-related kyphosis who are treated without instrumentation are more likely to develop progressive deformity, neurologic deficits, or pseudarthrosis if early mobilization is prescribed [2, 11, 13, 14, 17–19, 27, 30, 31]. The addition of modern instrumentation to the surgical treatment of these disorders has allowed us to employ early mobilization postoperatively for most patients with these disorders. However, unlike the patients in our study, most patients with these disorders have sufficient, satisfactory bone for screw purchase and sufficient fixation above and below the area of instability. Additionally, most of these patients have not experienced previous failure of surgical intervention. For these reasons, we believe our patients are different from patients previously described in the literature.
After a median of 3 months of postoperative bed rest, 10 of the 11 patients reported decreased pain and improved function at last followup. Similarly, Weinstein et al. [30] and Mumford et al. [18] reported satisfactory pain control based on VAS scores after bed rest for treatment of thoracolumbar burst fractures (Table 3). Mumford et al. [18] also reported 32 of 41 patients (78%) were working before treatment, while 26 of 32 patients (81%) returned to work after treatment with bed rest. However, only two of 11 patients in our study were working before surgery, and only one of these patients returned to work after surgery. These data may reflect the more complex and disabling nature of the underlying problems treated in our patients compared to patients with thoracolumbar burst fractures. The radiographic outcomes of our patients demonstrated maintenance of coronal and sagittal alignment in all 11 patients. In contrast, several authors reported the development of progressive deformity of greater than 5° of kyphosis or scoliosis after bed rest for the treatment of scoliosis, thoracolumbar fractures, and spondylolisthesis [2, 14, 18, 19, 27, 31]. All of our patients were treated with spinal fusion with instrumentation, correction of deformity, and bed rest, which may have contributed to the maintenance of postoperative alignment in these patients compared to patients in other studies who were treated with bed rest alone.
Table 3.
Summary of bed rest studies
| Study | Number of patients | Sex | Diagnosis | Treatment | Fusion | Cast | Instrumentation | Median length of bed rest (months) | Complications |
|---|---|---|---|---|---|---|---|---|---|
| Current study | 11 | 5 male, 6 female | See Table 1 | Spinal fusion and instrumentation | Yes | No | Yes | 3 | 1 delayed union, 1 late urosepsis |
| Mumford et al. [18] (1993) | 41 | 27 male, 14 female | Thoracolumbar burst fracture | Bed rest | No | No | No | 1 | 4 transient urinary retention, 4 urinary tract infections, 16 progressive deformity |
| Weinstein et al. [30] (1988) | 42 | 31 male, 11 female | Thoracolumbar burst fracture | Cast and bed rest | No | Yes | No | 0–3 | None |
| Tezer et al. [27] (2005) | 6 | 2 male, 4 female | Thoracolumbar compression fracture | Bed rest | No | No | No | 3 | 2 progressive deformity |
| Oner et al. [19] (2002) | 24 | 13 male, 11 female | Unstable thoracolumbar fracture | Cast and bed rest | No | Yes | No | 1–1.5 | 14 unsatisfactory outcomes with more than occasional pain and progressive deformity |
| Medical Research Council [17] (1978) | 55 | 33 male, 22 female | Tuberculosis of the spine | Radical resection and fusion | Yes | No | No | 1–3 | 1 intraoperative death, 12 nonunion |
| Jacobs et al. [13] (1980) | 34 | Thoracolumbar fracture | Bed rest | No | No | No | 2.25 | 2 pulmonary emboli, 1 pneumonia, 1 phlebitis, 2 pressure ulcers | |
| Jacobs et al. [13] (1980) | 51 | Thoracolumbar fracture | Spinal fusion and instrumentation | Yes | No | Yes | 1 | 2 pulmonary emboli, 1 infection, 1 failure of fixation | |
| Frankel et al. [11] (1969) | 612 | Cervical, thoracic, and lumbar fractures | Bed rest | No | No | No | 2.75 | None | |
| Kinoshita et al. [14] (1993) | 23 | Thoracolumbar burst fracture | Bed rest | No | No | No | 2–2.5 | 1 delayed union, 1 progressive deformity | |
| Wiltse et al. [31] (1968) | 3 | Pediatric spondylolisthesis | Fusion and bed rest | Yes | No | No | 2 | None | |
| Arkin [2] (1964) | 6 | 2 male, 4 female | Juvenile and neuromuscular scoliosis | Corrective casting and bed rest | No | Yes | No | 16 | 6 progression of deformity, rib deformities, emotional problems, difficulty in school |
Despite the well-known adverse effects of immobilization [2–7, 9–14, 16–19, 21, 23–28, 30, 31], only a few postoperative complications were identified. One patient had radiographic evidence of delayed union, whereas four of 11 patients had preoperatively documented pseudarthrosis. All patients demonstrated radiographic evidence of healing at last followup. None of our patients experienced failure of instrumentation or failure of fixation. These findings are particularly important in view of the high risk for failure of the fixation or fusion if early upright mobilization had been instituted. These results compare favorably to the 22% (12 of 55) incidence of pseudarthrosis after radical resection, fusion, and bed rest for patients with tuberculosis as reported by the Medical Research Council [17]. Throughout the bed rest period, each patient received mechanical DVT prophylaxis, which consisted of the use of TED hose and sequential compression devices while in the hospital and TED hose after discharge. No thromboembolic events were reported in this series. However, if prolonged bed rest is planned and the patient has other underlying risk factors for thromboembolic disease, an IVC filter or chemical prophylaxis may be helpful in decreasing the risk of pulmonary emboli. In addition, no patient developed pressure ulcers or wound breakdown during the period of bed rest. This complication is avoidable if special care is taken to limit the time a patient lies directly on his or her back. The psychologic effects of prolonged bed rest are potentially detrimental to the patient’s mental state. Patient 11 developed depression during the 6 months of bed rest. Although we did not identify any other reports of the development of depression during bed rest for the treatment of spinal disorders, Arkin [2] cited emotional problems and difficulty in school as two of the reasons he no longer recommends prolonged recumbency for his patients with scoliosis.
The direct costs of prolonged bed rest ranged from an estimated median cost of $16,702 for a skilled nursing facility to an estimated median cost of $5712 for home health nursing. Two of our 11 patients were employed before instituting bed rest. One of these patients remains unemployed 52 months after surgery. The other patient lost 3 months of work during the bed rest period and now works part-time.
Bed rest can be a useful adjunct to complex reconstructive spine surgery in carefully selected patients who are at high risk for failure of instrumentation with early mobilization and who have limited treatment options after such surgery. Further studies would be helpful in formulating a protocol to help reduce the potential complications associated with postoperative immobilization.
Footnotes
One of the authors (RAWM) is a consultant for Synthes Spine (West Chester, PA, USA) and DePuy Spine (Raynham, MA, USA) and is on the Speakers’ Bureau of DePuy Spine.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Allman RM, Goode PS, Patrick MM, Burst N, Bartolucci AA. Pressure ulcer risk factors among hospitalized patients with activity limitation. J Am Med Assoc. 1995;273:865–870. doi: 10.1001/jama.1995.03520350047027. [DOI] [PubMed] [Google Scholar]
- 2.Arkin AM. Correction of structural changes in scoliosis by corrective plaster jackets and prolonged recumbency. J Bone Joint Surg Am. 1964;46:33–52. [PubMed] [Google Scholar]
- 3.Belavý DL, Miokovic T, Armbrecht G, Richardson CA, Rittweger J, Felsenberg D. Differential atrophy of the lower-limb musculature during prolonged bed-rest. Eur J Appl Physiol. 2009;107:489–499. doi: 10.1007/s00421-009-1136-0. [DOI] [PubMed] [Google Scholar]
- 4.Bleeker MW, Groot PC, Rongen GA, Rittweger J, Felsenberg D, Smits P, Hopman MT. Vascular adaptation to deconditioning and the effect of an exercise countermeasure: results of the Berlin Bed Rest Study. J Appl Physiol. 2005;99:1293–1300. doi: 10.1152/japplphysiol.00118.2005. [DOI] [PubMed] [Google Scholar]
- 5.Dang Y, Yen D, Hopman W. Postoperative bed rest improves the alignment of thoracolumbar burst fractures treated with the AO spinal fixator. Can J Surg. 2009;52:215–220. [PMC free article] [PubMed] [Google Scholar]
- 6.Demiot C, Dignat-George F, Fortrat JO, Sabatier F, Gharib C, Larina I, Gauquelin-Koch G, Hughson R, Custaud MA. WISE 2005: chronic bed rest impairs microcirculatory endothelium in women. Am J Physiol Heart Circ Physiol. 2007;293:H3159–H3164. doi: 10.1152/ajpheart.00591.2007. [DOI] [PubMed] [Google Scholar]
- 7.Deyo RA, Diehl AK, Rosenthal M. How many days of bed rest for acute low back pain? A randomized clinical trial. N Engl J Med. 1986;315:1064–1070. doi: 10.1056/NEJM198610233151705. [DOI] [PubMed] [Google Scholar]
- 8.Dindo D, Demartines N, Clavien P. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dittmer DK, Teasell R. Complications of immobilization and bed rest. Part 1. Musculoskeletal and cardiovascular complications. Can Fam Physician. 1993;39:1428–1432. [PMC free article] [PubMed] [Google Scholar]
- 10.Dorfman TA, Levine BD, Tillery T, Peshock RM, Hastings JL, Schneider SM, Macias BR, Biolo G, Hargens AR. Cardiac atrophy in women following bed rest. J Appl Physiol. 2007;103:8–16. doi: 10.1152/japplphysiol.01162.2006. [DOI] [PubMed] [Google Scholar]
- 11.Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH, Vernon JD, Walsh JJ. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Part I. Paraplegia. 1969;7:179–192. doi: 10.1038/sc.1969.30. [DOI] [PubMed] [Google Scholar]
- 12.Hides JA, Belavý DL, Stanton W, Wilson SJ, Rittweger J, Felsenberg D, Richardson CA. MRI assessment of trunk muscles during prolonged bed rest. Spine (Phila Pa 1976) 2007;32:1687–1692. doi: 10.1097/BRS.0b013e318074c386. [DOI] [PubMed] [Google Scholar]
- 13.Jacobs RR, Asher MA, Snider RK. Thoracolumbar spinal injuries: a comparative study of recumbent and operative treatment in 100 patients. Spine (Phila Pa 1976) 1980;5:463–477. doi: 10.1097/00007632-198009000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Kinoshita H, Nagata Y, Ueda H, Kishi K. Conservative treatment of burst fractures of the thoracolumbar and lumbar spine. Paraplegia. 1993;31:58–67. doi: 10.1038/sc.1993.9. [DOI] [PubMed] [Google Scholar]
- 15.Lenke LG, Bridwell KH, Bullis D, Betz RR, Baldus C, Schoenecker PL. Results of in situ fusion for isthmic spondylolisthesis. J Spinal Disord. 1992;5:433–442. doi: 10.1097/00002517-199212000-00008. [DOI] [PubMed] [Google Scholar]
- 16.McEvoy RD, Bradford DS. The management of burst fractures of the thoracic and lumbar spine: experience in 53 patients. Spine (Phila Pa 1976) 1985;10:631–637. doi: 10.1097/00007632-198509000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Medical Research Council Working Party on Tuberculosis of the Spine A controlled trial of anterior spinal fusion and débridement in the surgical management of tuberculosis of the spine in patients on standard chemotherapy: a study in two centres in South Africa. Seventh Report of the Medical Research Council Working Party on Tuberculosis of the Spine. Tubercle. 1978;59:79–105. doi: 10.1016/0041-3879(78)90012-0. [DOI] [PubMed] [Google Scholar]
- 18.Mumford J, Weinstein JN, Spratt KF, Goel VK. Thoracolumbar burst fractures: the clinical efficacy and outcome of nonoperative management. Spine (Phila Pa 1976) 1993;18:955–970. doi: 10.1097/00007632-199306150-00003. [DOI] [PubMed] [Google Scholar]
- 19.Oner FC, Gils AP, Faber JA, Dhert WJ, Verbout AJ. Some complications of common treatment schemes of thoracolumbar spine fractures can be predicted with magnetic resonance imaging: prospective study of 53 patients with 71 fractures. Spine (Phila Pa 1976) 2002;27:629–636. doi: 10.1097/00007632-200203150-00012. [DOI] [PubMed] [Google Scholar]
- 20.Pakzad H, Roffey DM, Knight H, Dagenais S, Yelle J, Wai EK. Delay in operative stabilization of spine fractures in multitrauma patients without neurologic injuries: effects on outcomes. Can J Surg. 2011;54:270–276. doi: 10.1503/cjs.008810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parker H, Wood P, Main C. The use of pain drawing as a screening measure to predict psychological distress in chronic low back. Spine (Phila Pa 1976) 1995;20:236–243. doi: 10.1097/00007632-199501150-00022. [DOI] [PubMed] [Google Scholar]
- 22.Partsch H. Bed rest versus ambulation in the initial treatment of patients with proximal deep vein thrombosis. Curr Opin Pulm Med. 2002;8:389–393. doi: 10.1097/00063198-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Rechtine GR. Nonoperative management and treatment of spinal injuries. Spine (Phila Pa 1976) 2006;31(11 suppl):S22–S27. doi: 10.1097/01.brs.0000217947.43730.a6. [DOI] [PubMed] [Google Scholar]
- 24.Sievanen H. Immobilization and bone structure in humans. Arch Biochem Biophys. 2010;503:146–152. doi: 10.1016/j.abb.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 25.Slipman CW, Lipetz JS, Jackson HB, Vresilovic EJ. Deep venous thrombosis and pulmonary embolism as a complication of bed rest for low back pain. Arch Phys Med Rehabil. 2000;81:127–129. doi: 10.1016/s0003-9993(00)90233-8. [DOI] [PubMed] [Google Scholar]
- 26.Teasell R, Dittmer DK. Complications of immobilization and bed rest. Part 2. Other complications. Can Fam Physician. 1993;39:1440–1446. [PMC free article] [PubMed] [Google Scholar]
- 27.Tezer M, Erturer RE, Ozturk C, Ozturk I, Kuzgun U. Conservative treatment of fractures of the thoracolumbar spine. Int Orthop. 2005;29:78–82. doi: 10.1007/s00264-004-0619-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duijnhoven NT, Bleeker MW, Groot PC, Thijssen DH, Felsenberg D, Rittweger J, Hopman MT. The effect of bed rest and an exercise countermeasure on leg venous function. Eur J Appl Physiol. 2008;104:991–998. doi: 10.1007/s00421-008-0854-z. [DOI] [PubMed] [Google Scholar]
- 29.Wang T, Zeng B, Xu J, Chen H, Zhang T. Radiographic evaluation of selective anterior thoracolumbar or lumbar fusion for adolescent idiopathic scoliosis. Eur Spine J. 2008;17:1012–1018. doi: 10.1007/s00586-007-0510-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weinstein JN, Collalto P, Lehmann TR. Thoracolumbar “burst” fractures treated conservatively: a long-term follow-up. Spine (Phila Pa 1976) 1988;13:33–38. doi: 10.1097/00007632-198801000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Wiltse LL, Bateman G, Hutchinson RH, Nelson WE. The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Joint Surg Am. 1968;50:919–926. [PubMed] [Google Scholar]