Abstract
Background
Superior labral anterior-posterior (SLAP) lesions are a common cause of pain and disability in athletes. Individual studies have suggested low patient satisfaction with SLAP repairs in throwing athletes in particular and it is unclear how frequently athletes return to their previous level of competetion.
Questions/purposes
We systematically reviewed the literature to determine (1) patient satisfaction and (2) return to play at previous level of competition among throwing athletes compared to all athletes who underwent repair of Type II SLAP tears using various types of fixation.
Methods
We searched databases for English-language articles in peer-reviewed journals from 1950 to 2010 reporting Type II SLAP repairs with 2-year followup for our systematic review. A total of 506 patients with Type II SLAP tears were reviewed from 14 studies; of these, 327 had SLAP lesions repaired by anchor, 169 by tacks, and 10 by staples. Of the 506 patients, 198 were overhead athletes with a pooled subset of 81 identified baseball players.
Results
For the entire patient population, 83% had “good-to-excellent” patient satisfaction and 73% returned to their previous level of play whereas only 63% of overhead athletes returned to their previous level of play. Anchor repair in overhead athletes resulted in a higher percentage of “good-to-excellent” patient satisfaction (88% versus 74%) and a slightly higher return to play rate (63% versus 57%) compared with tack repair.
Conclusions
Repair of Type II SLAP tears leads to a return to previous level of play in most patients. Overhead athletes appear to have a lower rate of return to level of previous of play. Anchor fixation appears to be the most favorable fixation in both subjective scores and return to previous level of play.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-012-2295-6) contains supplementary material, which is available to authorized users.
Introduction
The shoulder is a mobile ball-and-socket joint with both static and dynamic stabilizers, including the glenoid with its concave surface, labrum, capsule and its ligamentous thickenings, negative intraarticular pressure, and adhesion-cohesion of synovial fluid [18]. The glenoid labrum is a fibrocartilaginous tissue with the superior labrum primarily triangular in cross section, allowing for deeper seating of the humeral head relative to the glenoid socket [16]. Andrews et al. [4] first reported these superior labral injuries. They were labeled superior labrum anterior-to-posterior lesions (SLAP) by Snyder et al. [30, 31] in 1990 and grouped into four basic types. A Type I tear is the most common, comprised of a fraying and degeneration of the superior labrum without biceps detachment. Type II tears can be described as a detachment of the superior labrum (or biceps anchor) from the glenoid. Since these tears include detachment of both the labrum and biceps, they are amenable to surgical fixation. Type III tears are bucket handle in shape with an intact biceps anchor, while Type IV tears extend into the biceps tendon. The precise mechanism of superior labrum tears is still not completely understood; it has been hypothesized repetitive overhead throwing may cause undue stress on the structure [14].
Previous attempts to treat these injuries with débridement alone were ineffective [3]. Fixation devices have evolved through the years, ranging from metal staples [35] to bioabsorbable tacks [25] to modern suture anchors [20]. The main outcomes studied have included patient satisfaction as measured by multiple validated scales (including UCLA [10], American Shoulder and Elbow Society [ASES] [27], and L’Insalata [19] scores), which ranges from 40% to 94% “good-to-excellent” results [5, 7], and ability to return to sport at a similar level of competition, which ranges from 22% to 92% [7, 17]. Although early studies showed patient satisfaction of greater than 90% in all athletes [29], overhead throwing athletes appeared to have less satisfaction after SLAP repair. Overhead or throwing sports include baseball, tennis, handball, badminton, softball, swimming, volleyball, and squash.
We therefore systematically reviewed the literature to determine (1) patient satisfaction and (2) return to play at previous level of competition among throwing athletes compared to all athletes who underwent repair of Type II SLAP tears using various types of fixation.
Search Strategy and Criteria
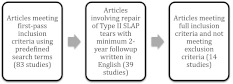
We conducted a systematic Internet search of PubMed, Ovid, and Cochrane database for Type II SLAP repairs between January 1, 1950, and December 31, 2010. Database search terms included “SLAP” OR “superior labrum anterior and posterior” OR “Type II SLAP” OR “SLAP outcome”. The initial search generated a total of 83 studies (Fig. 1). A supplemental hand search of American Journal of Sports Medicine, Arthroscopy, Journal of Shoulder and Elbow Surgery, Journal of Bone and Joint Surgery (American and British Volumes), and Clinical Orthopaedics and Related Research was performed.
Fig. 1.
A flowchart illustrates the method for selection of articles in this review.
Two authors (CCD, WMS) independently reviewed all abstracts. We included articles with the following criteria: (1) minimum 2-year followup, (2) reporting patient satisfaction and/or return-to-play rates, (3) Level IV or higher level of evidence per Centre for Evidence-Based Medicine criteria (CEBM) [24], (4) involving Type II SLAP tears without concomitant pathology, (5) English language, and (6) published in peer-reviewed journals. We excluded 69 articles that did not meet the inclusion criteria, leaving 14 studies [5–8, 11, 12, 15, 17, 20, 23, 25, 29, 35, 36] that met the inclusion criteria for this systematic review (Appendix 1; supplemental materials are available with the online version of CORR). The two reviewers were in complete agreement on the excluded and included studies. A total of 506 patients underwent arthroscopic fixation of Type II SLAP tears. Of these patients, 327 were fixed by anchors, 169 by tacks, and 10 by staples. A total of 198 overhead athletes and a subset of 81 baseball players were included in the studies.
Data extraction included type of fixation, patient subsets (specifically overhead athletes and baseball overhead athletes), patient satisfaction (graded as “good to excellent,” “fair,” or “poor” based on specific outcome scale used), and return to previous level of play (Table 1). The outcome measures used most often in these studies were the UCLA, ASES, and L’Insalata scores (Table 2). Levels of evidence were measured by two authors (CCD, WMS) using CEBM [24] (Table 2). We determined differences in patient satisfaction and percentage returning to previous level of play between types of athletes and types of fixation using Wilcoxon rank-sum test to compare these nonparametric continuous variables.
Table 1.
Results of 14 studies comparing patient satisfaction and return to play as subgrouped into overhead and baseball athletes
| Study | Year | Fixation | All patients | Overhead athletes | Baseball athletes | ||||
|---|---|---|---|---|---|---|---|---|---|
| Number | % “good-to-excellent” satisfaction | % returning to previous level of play | Number | % returning to previous level of play | Number | % returning to previous level of play | |||
| Morgan et al. [20] | 1998 | Anchor | 102 | 87 | NA | 53 | NA | 44 | 84 |
| Kim et al. [17] | 2002 | Anchor | 34 | 94 | 76 | 18 | 22 | NA | NA |
| Ide et al. [15] | 2005 | Anchor | 40 | 90 | 75 | 40 | 75 | 19 | 63 |
| Enad et al. [11] | 2007 | Anchor | 27 | 89 | 77 | NA | NA | NA | NA |
| Enad and Kurtz [12] | 2007 | Anchor | 36 | 92 | NA | NA | NA | NA | NA |
| Yung et al. [36] | 2008 | Anchor | 16 | 92 | 94 | 13 | NA | NA | NA |
| Brockmeier et al. [6] | 2009 | Anchor | 47 | 87 | 74 | 28 | 71 | 11 | 64 |
| Boileau et al. [5] | 2009 | Anchor | 25 | 40 | 20 | 15 | NA | NA | NA |
| Yoneda et al. [35] | 1991 | Staple | 10 | 80 | 50 | 10 | 50 | 7 | NA |
| Pagnani et al. [25] | 1995 | Tack | 22 | NA | NA | 13 | 92 | NA | NA |
| Samani et al. [29] | 2001 | Tack | 25 | 88 | 92 | NA | NA | NA | NA |
| O’Brien et al. [23] | 2002 | Tack | 31 | 74 | 52 | NA | NA | NA | NA |
| Cohen et al. [7] | 2006 | Tack | 41 | 69 | 48 | 8 | 38 | NA | NA |
| Coleman et al. [8] | 2007 | Tack | 50 | 70 | 93 | NA | NA | NA | NA |
| All studies | 506 | 83 | 73 | 198 | 63 | 81 | 76 | ||
NA = not available.
Table 2.
Shoulder outcome measures used and level of evidence for selected studies
| Study | Outcome measures | Study design/Level of evidence |
|---|---|---|
| Morgan et al. [20] | UCLA | Retrospective case series/Level IV |
| Kim et al. [17] | UCLA | Retrospective case series/Level IV |
| Ide et al. [15] | Rowe | Retrospective case series/Level IV |
| Enad et al. [11] | ASES, UCLA | Retrospective case series/Level IV |
| Enad and Kurtz [12] | UCLA | Retrospective case series/Level IV |
| Yung et al. [36] | UCLA | Prospective cohort/Level III |
| Brockmeier et al. [6] | ASES, L’Insalata | Retrospective case series/Level IV |
| Boileau et al. [5] | Constant-Murley | Prospective cohort/Level III |
| Yoneda et al. [35] | Tibone pain scale | Retrospective case series/Level IV |
| Pagnani et al. [25] | ASES | Retrospective case series/Level IV |
| Samani et al. [29] | ASES, UCLA | Retrospective case series/Level IV |
| O’Brien et al. [23] | ASES, L’Insalata | Retrospective case series/Level IV |
| Cohen et al. [7] | ASES, L’Insalata | Retrospective case series/Level IV |
| Coleman et al. [8] | ASES, L’Insalata | Retrospective case series/Level IV |
Results
With regard to patient satisfaction, 83% of all athletes had a “good-to-excellent” result on postoperative questionnaires (Table 1). Subset analysis revealed the “good-to-excellent” satisfaction rates were higher for anchor fixation (86%) than for tack fixation (74%) (p < 0.003) but not for staple fixation (80%) (p = 0.115). Anchor repair in overhead athletes resulted in a higher (p = 0.003) percentage of “good-to-excellent” patient satisfaction (88% versus 74%) compared with tack repair.
For all athletes, 73% were able to return to their previous level of play, whereas only 63% of overhead athletes returned to their previous level of play (Table 1). In comparing fixation devices for all athletes, there was no difference among anchors, staples, and tacks with regard to return to previous level of play. Anchor repair in overhead athletes resulted in a slightly higher (p > 0.05) return to previous level play rate (63% versus 57%) compared with tack repair.
Discussion
SLAP lesions are a common cause of pain and disability in the throwing athlete. Some studies [7, 17] have suggested low patient satisfaction with SLAP repairs in throwing athletes in particular. We therefore systematically reviewed the literature to determine (1) patient satisfaction and (2) return to play at previous level of competition among throwing athletes compared to all athletes who underwent repair of Type II SLAP tears using various types of fixation.
The literature and our specific review are subject to a number of limitations. First, the assessment of patient satisfaction via questionnaire and return to previous level of play are not sufficiently rigorous to definitively evaluate surgical fixation of Type II SLAP tears due to the heterogeneity of study outcome scales used (eg, UCLA, ASES, and L’Insalata scores). Patient questionnaires by definition are subjective and studies used different validated forms to generate an excellent/good/fair/poor outcome measure for ease of reporting. Combining the heterogeneous data of these studies in a systematic review introduces measurement bias, as the various scales measured patient satisfaction outcomes differently and do not have high intraobserver reliability [26]. Similarly, return to previous level of play as a surrogate outcome measure (as was used in the majority of reviewed studies) takes into account more than simply the successful repair of a labral tear. Concomitant pathology that was not identified and/or addressed during surgery would have obvious deleterious effects on an athlete’s recovery and return to sports, adding a different bias to the data. In addition, we did not perform testing to check for heterogeneity between the reviewed studies, nor did we utilize a standard measurement of study quality. These additional calculations could have led to stronger evidence and a better ability to extrapolate the data analyzed in this study.
We reviewed 14 studies regarding the repair of Type II SLAP tears in athletes. It appears overhead athletes have a more difficult time recovering from this lesion compared with other athletes. Although all 14 papers were retrospective in nature with small sample sizes, they were together fairly consistent in exemplifying difficulty with this subset of patients that needs to be addressed. The authors of these studies provided some explanations as to why overhead athletes seemingly did worse in comparison with their nonoverhead counterparts, including concomitant pathology and problems with throwing mechanics.
Recently, Neuman et al. [22] retrospectively analyzed 30 overhead athletes with Type II SLAP tears and followed them for an average of 3.5 years. Twenty-one of these athletes played baseball or softball, and nine athletes were in other overhead sports, such as tennis and javelin. The authors used the ASES scoring system [27], as did the majority of the studies included in our review. However, they also included the Kerlan-Jobe Orthopaedic Clinic Shoulder and Elbow score (KJOC), which has been proposed as a more specific score for overhead athletes [2]. The authors found 84% of patients were able to return to their previous level of play after an average of 11.7 months’ recovery, and 93% of patients believed they had “good-to-excellent” patient satisfaction. They found similar ASES and KJOC scores between baseball and other overhead athletes, but the baseball players had lower KJOC scores compared with the other overhead group. In subgroup analysis, the baseball players only had an 80% return to previous level of play compared with 94% for the other overhead athletes. The authors concluded, compared to the ASES score, the KJOC score is a more specific scoring system for throwing athletes and may more accurately document the struggles overhead athletes, particularly baseball players, have in returning to sport after a Type II SLAP repair.
Seven of the papers reviewed hypothesized concomitant pathology in the throwing athlete may be the reason for the poorer patient satisfaction generally identified in the overhead athletes. A number of papers suggested rotator cuff tears as a potential confounder. Franceschi et al. [13] performed a prospective randomized clinical trial focusing on patients older than 50 years with diagnosed Type II SLAP tears and a rotator cuff tear on arthroscopy. The authors randomized patients into a group for SLAP repair and rotator cuff repair and a group with long head of biceps tenodesis and rotator cuff repair. At minimum 2.9 years’ followup, there was no advantage in repairing the SLAP lesion when comparing groups using UCLA scores [10] and ROM measurements. The authors concluded, in the older population, the SLAP lesion may not be the major pain generator it is in younger throwing athletes, and biceps tenodesis works well for pain relief in this patient population.
Abbot et al. [1], in a study that did not meet our inclusion criteria, followed 48 patients with concomitant Type II SLAP tears and rotator cuff tears with an average age of 51.9 years. The authors intraoperatively randomized patients to subacromial decompression and rotator cuff repair with SLAP débridement versus repair. Using the Tegner and Lysholm [32] and UCLA shoulder scores, the group with SLAP débridement showed improved functional scores and pain relief compared with the repair group. However, 10 patients were lost to final followup in this study. In direct contrast, Voos et al. [34], in another study that did not meet our inclusion criteria, looked at a similar cohort of patients (average age, 47.8 years) with either a Bankart or SLAP lesion in addition to a rotator cuff tear. At a mean followup of 2.7 years, the authors found repairing both lesions resulted in 90% “good-to-excellent” patient satisfaction and a 77% (23 of 30 patients) return to previous level of play. Finally, Neri et al. [21], in a study that did not meet our inclusion criteria, reviewed 23 elite overhead athletes with the ASES and KJOC scores and found 96% “good-to-excellent” patient satisfaction on the ASES but only 52% “good-to-excellent” scores on the KJOC and a 57% return to previous level of play. Similar to the conclusions drawn by Neuman et al. [22], the authors state the KJOC score is more specific to overhead athletes in assessing their post-SLAP repair function and pain.
After systematically reviewing 14 articles on the results of arthroscopic repair of Type II SLAP tears, we conclude the generally recognized favorable patient satisfaction previously reported do not apply to the subset of overhead athletes in terms of pain relief or return to previous level of sport. The patient satisfaction measures in the overhead patient are variable and may be related to concomitant pathology, such as shoulder instability or rotator cuff tear. The data for overhead athletes with SLAP tears are inconclusive, and more research is required to find potential reasons why this patient population does not do as well after this surgery compared with nonthrowing athletes. The studies reviewed contained only Level III or IV evidence, and as such, large multicenter prospective trials will be necessary to clarify this problem for orthopaedists to best guide treatment for the overhead athletes with Type II SLAP tears.
Electronic supplementary material
Acknowledgments
We thank Dan O’Brien, BS, for his assistance in facilitating the editing process and Mitchell Malenfort, PhD, for his assistance with the statistical analysis.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Abbot AE, Li X, Busconi BD. Arthroscopic treatment of concomitant superior labral anterior posterior (SLAP) lesions and rotator cuff tears in patients over the age of 45 years. Am J Sports Med. 2009;37:1358–1362. doi: 10.1177/0363546509331940. [DOI] [PubMed] [Google Scholar]
- 2.Alberta FG, El Attrache NS, Bissell S, Mohr K, Browdy J, Yocum L, Jobe F. The development and validation of a functional assessment tool for the upper extremity in the overhead athlete. Am J Sports Med. 2010;38:903–911. doi: 10.1177/0363546509355642. [DOI] [PubMed] [Google Scholar]
- 3.Altchek DW, Warren RF, Wickiewicz TL, Ortiz G. Arthroscopic labral debridement: a three-year follow-up study. Am J Sports Med. 1992;20:702–706. doi: 10.1177/036354659202000611. [DOI] [PubMed] [Google Scholar]
- 4.Andrews JR, Carson WG, Jr, McLeod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13:337–341. doi: 10.1177/036354658501300508. [DOI] [PubMed] [Google Scholar]
- 5.Boileau P, Parratte S, Chuinard C, Roussanne Y, Shia D, Bicknell R. Arthroscopic treatment of isolated Type II SLAP lesions: biceps tenodesis as an alternative to reinsertion. Am J Sports Med. 2009;37:929–936. doi: 10.1177/0363546508330127. [DOI] [PubMed] [Google Scholar]
- 6.Brockmeier SF, Voos JE, Williams RJ, 3rd, Altchek DW, Cordasco FA, Allen AA. Outcomes after arthroscopic repair of Type-II SLAP lesions. J Bone Joint Surg Am. 2009;91:1595–1603. doi: 10.2106/JBJS.H.00205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen DB, Coleman S, Drakos MC, Allen AA, O’Brien SJ, Altchek DW, Warren RF. Outcomes of isolated Type II SLAP lesions treated with arthroscopic fixation using a bioabsorbable tack. Arthroscopy. 2006;22(2):136–142. doi: 10.1016/j.arthro.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 8.Coleman SH, Cohen DB, Drakos MC, Allen AA, Williams RJ, O’Brien SJ, Altchek DW, Warren RF. Arthroscopic repair of Type II superior labral anterior posterior lesions with and without acromioplasty: a clinical analysis of 50 patients. Am J Sports Med. 2007;35:749–753. doi: 10.1177/0363546506296735. [DOI] [PubMed] [Google Scholar]
- 9.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 10.Ellman H. Arthroscopic subacromial decompression: analysis of one- to three-year results. Arthroscopy. 1987;3:173–181. doi: 10.1016/S0749-8063(87)80061-0. [DOI] [PubMed] [Google Scholar]
- 11.Enad JG, Gaines RJ, White SM, Kurtz CA. Arthroscopic superior labrum anterior-posterior repair in military patients. J Shoulder Elbow Surg. 2007;16:300–305. doi: 10.1016/j.jse.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 12.Enad JG, Kurtz CA. Isolated and combined Type II SLAP repairs in a military population. Knee Surg Sports Traumatol Arthrosc. 2007;15:1382–1389. doi: 10.1007/s00167-007-0334-8. [DOI] [PubMed] [Google Scholar]
- 13.Franceschi F, Longo UG, Ruzzini L, Rizzello G, Maffulli N, Denaro V. No advantages in repairing a Type II superior labrum anterior and posterior (SLAP) lesion when associated with rotator cuff repair in patients over age 50. Am J Sports Med. 2008;36:247–253. doi: 10.1177/0363546507308194. [DOI] [PubMed] [Google Scholar]
- 14.Grossman MG, Tibone JE, McGarry MH, Schneider DJ, Veneziani S, Lee TQ. A cadaveric model of the throwing shoulder: a possible etiology of superior labrum anterior-to-posterior lesions. J Bone Joint Surg Am. 2005;87:824–831. doi: 10.2106/JBJS.D.01972. [DOI] [PubMed] [Google Scholar]
- 15.Ide J, Maeda S, Takagi K. Sports activity after arthroscopic superior labral repair using suture anchors in overhead-throwing athletes. Am J Sports Med. 2005;33:507–514. doi: 10.1177/0363546504269255. [DOI] [PubMed] [Google Scholar]
- 16.Keener JD, Brophy RH. Superior labral tears of the shoulder: pathogenesis, evaluation, and treatment. J Am Acad Orthop Surg. 2009;17:627–637. doi: 10.5435/00124635-200910000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Kim SH, Ha KI, Kim SH, Choi HJ. Results of arthroscopic treatment of superior labral lesions. J Bone Joint Surg Am. 2002;84:981–985. doi: 10.1302/0301-620X.84B7.12587. [DOI] [PubMed] [Google Scholar]
- 18.Lee SB, Kim KJ, O’Driscoll SW, Morrey BF, An KN. Dynamic glenohumeral stability provided by the rotator cuff muscles in the mid-range and end-range of motion: a study in cadavera. J Bone Joint Surg Am. 2000;82:849–857. doi: 10.2106/00004623-200006000-00012. [DOI] [PubMed] [Google Scholar]
- 19.L’Insalata JC, Warren RF, Cohen SB, Altchek DW, Peterson MG. A self-administered questionnaire for the assessment of symptoms and function of the shoulder. J Bone Joint Surg Am. 1997;79:738–748. doi: 10.1302/0301-620X.79B5.7345. [DOI] [PubMed] [Google Scholar]
- 20.Morgan CD, Burkhart SS, Palmeri M, Gillespie M. Type II SLAP lesions: three subtypes and their relationships to superior instability and rotator cuff tears. Arthroscopy. 1998;14(6):553–565. doi: 10.1016/S0749-8063(98)70049-0. [DOI] [PubMed] [Google Scholar]
- 21.Neri BR, Attrache NS, Owsley KC, Mohr K, Yocum LA. Outcome of Type II superior labral anterior posterior repairs in elite overhead athletes. Am J Sports Med. 2011;39:114–120. doi: 10.1177/0363546510379971. [DOI] [PubMed] [Google Scholar]
- 22.Neuman B, Boisvert CB, Reiter B, Lawson K, Ciccotti MG, Cohen SB. Results of arthroscopic repair of Type II SLAP lesions in overhead athletes: assessment of return to pre-injury playing level and satisfaction. Am J Sports Med. 2011;39:1883–1888. doi: 10.1177/0363546511412317. [DOI] [PubMed] [Google Scholar]
- 23.O’Brien SJ, Allen AA, Coleman SH, Drakos MC. The trans-rotator cuff approach to SLAP lesions: technical aspects for repair and a clinical follow-up of 31 patients at a minimum of 2 years. Arthroscopy. 2002;18:372–377. doi: 10.1053/jars.2002.30646. [DOI] [PubMed] [Google Scholar]
- 24.Oxford Centre for Evidence-Based Medicine Levels of Evidence Working Group. The Oxford 2011 Levels of Evidence. Available at: http://www.cebm.net/index.aspx?o=5653. Accessed January 31, 2012.
- 25.Pagnani MJ, Speer KP, Altchek DW, Warren RF, Dines DM. Arthroscopic fixation of superior labral lesions using a biodegradable implant: a preliminary report. Arthroscopy. 1995;11:194–198. doi: 10.1016/0749-8063(95)90066-7. [DOI] [PubMed] [Google Scholar]
- 26.Placzek JD, Lukens SC, Badalanmenti S, Roubal PJ, Freeman DC, Walleman KM, Parrot A, Wiater JM. Shoulder outcome measures: a comparison of 6 functional tests. Am J Sports Med. 2004;32:1270–1277. doi: 10.1177/0363546503262193. [DOI] [PubMed] [Google Scholar]
- 27.Richards RR, An KN, Bigliani LU, Friedman RJ, Gartsman GM, Gristina AG. A self-administered questionnaire for the assessment of symptoms and function of the shoulder. J Shoulder Elbow Surg. 1994;3:347–351. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- 28.Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am. 1978;60:1–16. [PubMed] [Google Scholar]
- 29.Samani JE, Marston SB, Buss DD. Arthroscopic stabilization of Type II SLAP lesions using an absorbable tack. Arthroscopy. 2001;17:19–24. doi: 10.1053/jars.2001.19652. [DOI] [PubMed] [Google Scholar]
- 30.Snyder SJ, Banas MP, Karzel RP. An analysis of 140 injuries to the superior glenoid labrum. J Shoulder Elbow Surg. 1995;4:243–248. doi: 10.1016/S1058-2746(05)80015-1. [DOI] [PubMed] [Google Scholar]
- 31.Snyder SJ, Karzel RP, Pizzo W, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthroscopy. 1990;6:274–279. doi: 10.1016/0749-8063(90)90056-J. [DOI] [PubMed] [Google Scholar]
- 32.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 33.Tibone JE, Jobe FW, Kerlan RK, Carter VS, Shields CL, Lombardo SJ, Yocum LA. Shoulder impingement syndrome in athletes treated by an anterior acromioplasty. Clin Orthop Relat Res. 1985;198:134–140. [PubMed] [Google Scholar]
- 34.Voos JE, Pearle AD, Mattern CJ, Cordasco FA, Allen AA, Warren RF. Outcomes of combined arthroscopic rotator cuff and labral repair. Am J Sports Med. 2007;35:1174–1179. doi: 10.1177/0363546507300062. [DOI] [PubMed] [Google Scholar]
- 35.Yoneda M, Hirooka A, Saito S, Yamamoto T, Ochi T, Shino K. Arthroscopic stapling for detached superior glenoid labrum. J Bone Joint Surg Br. 1991;73:746–750. doi: 10.1302/0301-620X.73B5.1894660. [DOI] [PubMed] [Google Scholar]
- 36.Yung PS, Fong DT, Kong MF, Lo CK, Fung KY, Ho EP, Chan DK, Chan KM. Arthroscopic repair of isolated Type II superior labrum anterior-posterior lesion. Knee Surg Sports Traumatol Arthrosc. 2008;16:1151–1157. doi: 10.1007/s00167-008-0629-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.