Abstract
Background
Glenohumeral internal rotation (GIR) and total arc of motion (TAM) decrease, whereas external rotation (GER) may increase in throwing. Although decreased GIR has been documented after throwing, its time course for recovery and the effect of pitching role have not.
Questions/purposes
We therefore asked (1) how much rotational change occurs after a single throwing episode; (2) do these changes return to baseline by the next throwing episode; and (3) does pitching role affect the amount of change that occurs?
Methods
Forty-five pitchers, starters and relievers, were examined. GIR and GER measurements were taken at five time points (TP): before throwing (TP1); immediately after throwing (TP2); and 24 (TP3), 48 (TP4), and 72 (TP5) hours later. TAM was calculated as the combination of GIR and GER.
Results
GIR decreased from TP1 to TP5 and did not return to baseline. GER changed very little and TAM decreased at TP5. Relievers had greater GIR, GER, and TAM across all time points, but the amount of change over all time points was not different between groups.
Conclusions
GIR was most affected over one 4-day throwing cycle after an acute throwing episode and was less than baseline 72 hours later. Pitching role did not affect the short-term changes.
Clinical Relevance
GIR changes should be expected after an acute throwing episode and conditioning and recovery programs should be used to modify the changes. Because GIR is dynamic, studies on GIR should specifically state when during the pitching cycle the measurement was obtained.
Introduction
Effective pitching requires balanced internal and external glenohumeral rotation. The right balance of glenohumeral (GH) internal rotation (GIR) and external rotation (GER) minimizes translation of the humeral instant center of rotation on the glenoid [12] and maximizes concavity compression [16]. GIR also contributes to maximal hand and ball velocity [9, 13, 17] and decreases the valgus loads at the elbow [13, 20].
GIR and GER are dynamic and affected by the throwing motion: compared with the nondominant arm, GIR is decreased and GER is increased [1, 2, 5, 8, 18, 21, 27]. In most throwers, this increase and decrease cancel each other so that the total arc of motion (TAM, the sum of GIR and GER) is the same on both sides [27]. These adaptations, especially in GER, are believed to be advantageous for achieving the maximal arm position for cocking and creating maximum ball velocity [2, 24].
However, maladaptations in glenohumeral motion can also occur that alter the most effective ball and socket kinematics (ie, minimal translation) and may increase injury risk. GIR and TAM may be decreased compared with the nondominant shoulder, creating alterations in GH kinematics so the humeral instant center of rotation moves anterosuperiorly on the glenoid with forward flexion [1] and posterosuperiorly with external rotation and cocking [2, 11]. These alterations in motion have been associated with labral injury [2, 3, 15, 19] and elbow injuries [6] and reportedly predict increased injury incidence at the shoulder [26].
These maladaptive changes have been expressed as deficits (D) of GH motion compared with the nondominant arm—GIRD and TAMD. Since GIRD was first reported more than 20 years ago [4], multiple studies have described some of its parameters. GIRD increases from immediately before to immediately and 24 hours after a throwing exposure [22], from the beginning to the end of one season [10], and with years of throwing exposure [14, 23]. GIRD also differs in the amount of change over one season between starters and relievers [10].
Injury prevention strategies are focusing on identifying and modifying the factors that may produce GIRD and TAMD. Almost all pitchers pitch on a regular cycle of pitching, rest, and return to pitching. The length of the cycle is determined by the pitching role. Data regarding alterations in GIR, GER, and TAM for the entire pitching cycle either for starters or relievers during this cycle would be beneficial in understanding how these alterations develop and change over this cycle will suggest conditioning strategies to modify these alterations.
We therefore asked whether (1) GIR and TAM would change in response to a 4-day pitching cycle; (2) the change in GIR would be slow to return to baseline; and (3) rotation magnitude and duration would differ between starters and relievers.
Materials and Methods
We recruited 45 professional baseball pitchers (age, 22.3 ± 2.6 years; height, 187.9 ± 6.2 cm; weight, 90.4 ± 9.1 kg) from one Major League Baseball organization (Houston Astros) for participation in this study during actual game situations as part of 2009 spring training. Subjects were identified by the organization as being either a starting (n = 22) or relief pitcher (n = 23). We used a repeated-measures design to assess change in rotation and total arc of motion after throwing. The independent variables were five time points (before throwing, immediately after throwing, and 24, 48, and 72 hours after throwing) and position (starter and reliever). The dependent variables were the measurements obtained from both dominant and nondominant arms for GER, GIR, and TAM. All measurements were taken during spring training at the start of interclub competition. A pitcher was excluded from the study if he had limitations such as pain, injury, or participation modifications preventing him from actively throwing. Per the baseball organization’s spring training classification of pitching role, a starting pitcher was defined as throwing 40 pitches during a competitive spring training game, whereas a relief pitcher threw 25 pitches during a game. The organization selected these limited parameters to acclimatize each player to his specific role and to limit the arm’s exposure to excessive work because of the lengthy baseball season. All subclassifications of relief pitchers (set-up, closer, etc) were combined into one group. A member of the research team explained the experimental procedures and any involved risks to each subject. The subject was then given an informed consent form to read and sign. General information, height, weight, dominant hand, age, and history of injury were obtained.
Each pitcher threw eight warm-up pitches from the mound at the start of each inning. Each starting pitcher threw a maximum of three innings, whereas each relief pitcher threw in a maximum of two innings, bringing the total number of pitches thrown in a game to 64 for starters and 41 for relievers. Once the pitch limit had been reached, the pitcher was removed from the game. In the event that the pitcher was in the middle of a batter and the pitch count was reached, the pitcher was allowed to finish throwing until the batter was either out or reached base. This occurred only six times with the extra pitch totals ranging from three to seven throws beyond the set pitch counts. A standardized daily pre- and postthrowing program was completed by each pitcher and included rotation measurements, team activities, and game and postgame measurements if indicated (Table 1).
Table 1.
Standardized pre- and postthrowing routine
| Game day (TP1–TP2) | 24 hours (TP3) | 48 hours (TP4) | 72 hours (TP5) |
|---|---|---|---|
| TP1 measurements obtained | TP3 measurements obtained | TP4 measurements obtained | |
| Team stretch and agilities | Team stretch and agilities | Team stretch and agilities | Team stretch and agilities |
| Long toss program* | Long toss program* | Long toss program* | Long toss program* |
| Fundamentals/baseball specific drills | Fundamentals/baseball specific drills | Fundamentals/baseball specific drills | Fundamentals/baseball specific drills |
| Performance enhancement program† | Performance enhancement program† | Performance enhancement program† | Performance enhancement program† |
| Batting practice (pitchers not throwing in daily games collect balls in outfield) | Batting practice (pitchers not throwing in daily games/side collect balls in outfield) | Batting practice (pitchers not throwing in daily games/side collect balls in outfield) | Batting practice (pitchers not throwing in daily games/side collect balls in outfield) |
| Lunch break | Side | ||
| Pregame warm-up | TP5 measurements obtained | ||
| Game | |||
| TP2 measurements obtained |
* All pitchers 60 tosses total up to a maximum of 90 feet; †series of eight exercises designed to warm up the rotator cuff and deltoid muscles performed with tubing and 3- to 5-lb free weights at one set of 10 repetitions; TP = time point.
One examiner (AS) measured glenohumeral internal and external rotation motions bilaterally by manual long-arm goniometry for all subjects. Both measurements were obtained at five time points: on arrival at the respective facility (before warm-up or stretching for the pitching exposure in an actual game situation) (time point [TP1]), immediately after the game day pitching exposure (TP2), and 24 (TP3), 48 (TP4), and 72 (TP5) hours later. TP5 was after the next time the pitcher had a throwing episode, a “side” in which the player threw in an abbreviated game simulation. Per the organization’s policy, no interventions such as ice, massage, or stretching were applied postthrowing; however, all pitchers aerobically conditioned under the direction of the strength and conditioning staff. The change in motions was defined as the change in each measure between TP1 and TP2–5. The ROM data gathered included GIR, GER, and TAM.
Each subject was placed in a supine position on a flat, level surface. A second examiner was positioned behind the athlete to properly stabilize the scapula during testing by applying stabilization to the coracoid and scapular body to ensure that scapular movement did not occur [28] (Fig. 1). This examiner also read and recorded the measurements obtained by the first examiner. The humerus was supported on the surface with the elbow placed at 90° and the arm on a bolster in the plane of the scapula. The following landmarks were identified before placing the goniometer: the fulcrum was set at the olecranon process of the elbow, the stationary arm perpendicular to the table as documented by the bubble on the goniometer, and the moving arm in line with the styloid process of the ulna. Each subject was then advised to relax while the humerus was passively moved into internal and external rotation. Internal rotation was taken to “tightness,” a point at which no more GH motion would occur unless the scapula would move. The humerus was then moved into an externally rotated position to “tightness.” The measure was recorded once the humeral motion stopped. The procedures were repeated bilaterally to obtain measurements from both the throwing and nonthrowing shoulders. The testing order of both rotation measurements and arm dominance was randomized through use of a randomization table.
Fig. 1.

Internal and external rotation measurements were obtained using a two-person measurement technique.
The reliability of a single examiner (AS) was calculated a priori by testing 10 nonthrowing subjects using a standard long-arm goniometer. The intraclass coefficient (ICC), standard error of measurement (SEM), and minimal detectable change (MDC) for internal rotation were: ICC (2, 1) = 0.975, SEM = 1.9°, and MDC = 2.6°, whereas the values for external rotation were: ICC (2, 1) = 0.984, SEM = 1.5°, and MDC = 2.2°. We considered a meaningful change as 3° or greater because this measurement was beyond the examiner’s SEM and MDC. The numerical dial was covered on one side to prevent bias from the examiner obtaining the measurements while the second examiner recorded the resultant values.
To examine motion in the throwing arm, separate two (position; ie, starter or reliever) by five (time, ie, time points 1–5) repeated-measures analysis of variance (RM ANOVA) for GIR, GER, and TAM and separate two (position) by four (time) RM ANOVAs for percent change from TP1 for GIR, GER, and TAM were performed. Additionally, a three (motion) by four (time) RM ANOVA was performed to compare differences in percent change among GIR, GER, and TAM. A least significant difference post hoc analysis was performed when appropriate. Percent change was calculated for each followup measure (TP2–TP5) relative to baseline (TP1) and was calculated as (followup − TP1)/TP1*100. SPSS for Windows, Version 19.0 (SPSS, Inc, Chicago, IL, USA) was used for all statistical analyses.
Results
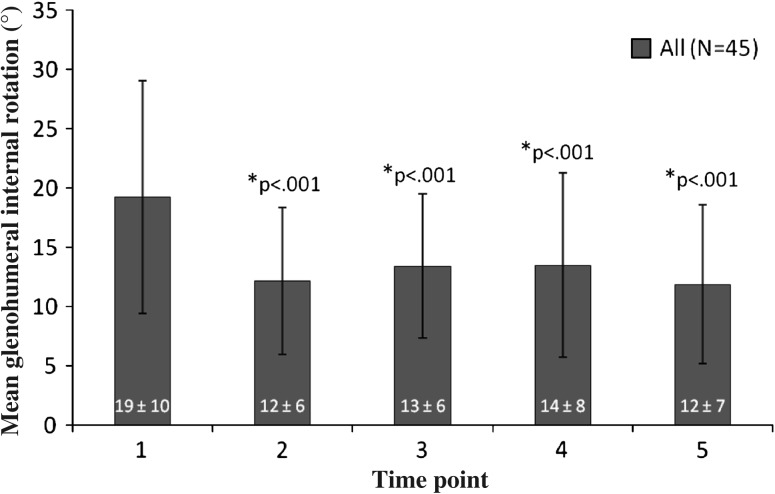
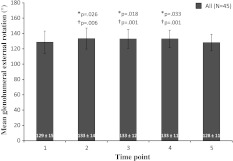
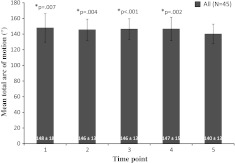
Across all subjects, mean GIR at TP1 (19°) was greater (p ≤ 0.001) than mean GIR at each of the followup time points (range, 12°–14°) (Fig. 2). These changes were larger than the SEM and MDC; therefore, the changes were considered meaningful. All values of GIR did not return to baseline across TP2–TP5. Additionally, mean GER was 133° at TP2, TP3, and TP4, which was greater (p ≤ 0.03) than TP1 (129°) and TP5 (128°) (Fig. 3). These changes were larger than the SEM and MDC; therefore, the changes were considered meaningful. Mean TAM at TP5 (140°) was less (p ≤ 0.007) than mean TAM at each of the other time points (range, 146°–148°) (Fig. 4).
Fig. 2.
The bar graph shows the measurements of GIR for the entire group at each time point. Mean GIR values were decreased across time points TP2–TP5 after an acute throwing episode. The asterisk indicates significantly less GIR than TP1. Mean ± SD is provided at the base of each bar in the graph.
Fig. 3.
The bar graph shows the measurements of GER for the entire group at each time point. Mean GER values were greater at TP2–TP4 compared with TP1 and TP5 after an acute throwing episode. The asterisk indicates significantly greater GER than TP1. The dagger indicates significantly greater GER than TP5. Mean ± SD is provided at the base of each bar in the graph.
Fig. 4.
The bar graph shows the measurements of TAM for the entire group at each time point. The mean TAM value at TP5 was decreased compared with preceding time points TP1, TP2, TP3, and TP4 after an acute throwing episode. The asterisk indicates significantly greater TAM than TP5. Mean ± SD is provided at the base of each bar in the graph.
Across all subjects, the percent change from baseline in GIR was variable at TP2–TP5 (range, −19% to −31%) (p > 0.05). Across all subjects, the percent change from baseline in GER at TP2–TP4 (4%) was greater than the percent change from baseline at TP5 (1%) (p ≤ 0.009) (Table 2). The percent change from baseline in TAM at TP5 (−4%) was greater (p ≤ 0.004) than the percent change from baseline at TP2 (−1%), TP3 (0%), and TP4 (0%) (Table 2). Across all time points, percent change in GIR (−26%), GER (3%), and TAM (−1%) were each different from one another (p < 0.001).
Table 2.
Rotation measures of starters and relievers reported as mean and SD of percent change (%Δ) for consecutive time points
| Motion | Position | Time point 2 | Time point 3 | Time point 4 | Time point 5 | Mean across all time points | Differences between time points |
|---|---|---|---|---|---|---|---|
| Internal rotation | Starter | −32 ± 34 | −21 ± 37 | −13 ± 67 | −22 ± 48 | −22 | |
| Reliever | −31 ± 28 | −24 ± 26 | −24 ± 32 | −37 ± 31 | −29 | ||
| Total | −31 ± 30 | −22 ± 32 | −19 ± 52 | −30 ± 41 | −26* | ||
| External rotation | Starter | 6 ± 11 | 3 ± 11 | 4 ± 12 | −1 ± 12 | 3 | |
| Reliever | 3 ± 12 | 5 ± 7 | 5 ± 9 | 2 ± 10 | 4 | ||
| Total | 4 ± 12 | 4 ± 9 | 4 ± 10 | 1 ± 11 | 3† | %Δ TP2, %Δ TP3, and %Δ TP4 < %Δ TP5 (p ≤ 0.009) | |
| Total arc of motion | Starter | 1 ± 10 | −1 ± 10 | 0 ± 13 | −5 ± 10 | −1 | |
| Reliever | −2 ± 12 | 0 ± 9 | 0 ± 11 | −4 ± 12 | −2 | ||
| Total | −1 ± 11 | 0 ± 9 | 0 ± 12 | −4 ± 11 | −1‡ | %Δ TP5 < %Δ TP2, %Δ TP3, and %Δ TP4 (p ≤ 0.004) |
* Significantly different compared with external rotation and total arc of motion; †significantly different compared with internal rotation and total arc of motion; ‡significantly different compared with internal rotation and external rotation; TP = time point.
When collapsing across all time points, relievers demonstrated more GIR (16° ± 5° versus 12° ± 5°, p = 0.03), GER (134° ± 10° versus 128° ± 10°, p = 0.06), and TAM (150° ± 10° versus 141° ± 10°, p = 0.004) than starters.
Discussion
The baseball throwing motion requires balanced glenohumeral rotation to minimize the translation of the glenohumeral instant center of rotation on the glenoid [12] and maximize concavity-compression [16]. GIR, GER, and TAM change in response to long-term throwing exposure [14, 23], to acute exposure from before to immediately after a throwing exposure [22], and to the type of pitching role—starter versus reliever [10]. Changes in GIR and TAM have been associated with shoulder injury [2, 3, 15, 19] and may be predictive of shoulder injury [26]. We asked whether (1) GIR and TAM would change in response to a 4-day pitching cycle; (2) the change in GIR would be slow to return to baseline; and (3) rotation magnitude and duration would differ between starters and relievers.
There are several limitations in this study that should be considered. First, data collection took place during spring training when the shoulders had little prior exposure to throwing. Further measurements during the season could establish curves of response after multiple exposures to throwing. Second, we did not examine the effect of less controlled pitching exposures such as repetitive warming up times or higher pitch counts. Again, in-season measurements would be ideal. Third, the data reflect the response in this particular population. Other groups such as high school or college pitchers or injured players may have different curves of response. These specific variables need to be considered in any further investigations. Third, we acknowledge that our rotation values are lower compared with previously reported values in baseball pitchers likely as a result of inconsistencies between past work regarding stabilization and instrumentation (Table 3). The authors attempted to capture glenohumeral rotation without the influence of surrounding anatomical structures allowing excessive degrees of freedom. We selected the method of stabilization because it reportedly allows determination reliable passive internal and external rotation of the glenohumeral joint without compromising natural rotary motion [28]. Fourth, this study only evaluated changes in GIR, GER, and TAM in the throwing shoulder to delineate the acute changes as a result of the throwing episode. Side-to-side differences were not calculated.
Table 3.
Summarization of reported humeral rotation values, applied instrumentation, and stabilization techniques for baseball players
| Manuscript | Study design | Subjects | Time of measurement | Internal rotation (°) | External rotation (°) | Instrument | Stabilization |
|---|---|---|---|---|---|---|---|
| Dwelly et al. [7] | Prospective | 29 collegiate pitchers and position players | Pre- and post-Spring | Pre: 48 ± 9 Post: 46 ± 10 |
Pre: 104 ± 17 Post: 107 ± 20 |
Inclinometer | Table stabilized scapula and visual inspection |
| Freehill et al. [10] | Retrospective | 21 professional baseball pitchers | First 2 weeks of spring training and final home stand of regular season | Pre: 71 ± 12 Post: 74 ± 13 |
Pre: 125 ± 20 Post: 126 ± 22 |
Bubble goniometer | Posterior-directed force to anterior shoulder and visual inspection |
| Reinold et al. [22] | Prospective | 67 professional baseball pitchers | First 2 days of spring training (pre-, postthrow, and 24 hours later) | Pre: 54 ± 11 Post: 45 ± 12 24 hours: 47 ± 10 |
Pre: 137 ± 10 Post: 135 ± 9 24 hours: 137 ± 9 |
Bubble goniometer | Table stabilized scapula and visual inspection |
| Wilk et al. [26] | Retrospective | 122 professional baseball pitchers | Spring training physical examinations | 48 ± 11 | 136 ± 11 | Bubble goniometer | Coracoid and scapular body |
| Current study | Prospective | 45 professional baseball pitchers | 5 weeks into spring training during exhibition competition (pre-, postthrow, 24–72 hours later) | Pre: 19 ± 10 Post: 12 ± 6 24 hours: 13 ± 6 48 hours: 14 ± 8 72 hours: 12 ± 7 |
Pre: 129 ± 15 Post: 133 ± 14 24 hours: 133 ± 13 48 hours: 133 ± 11 72 hours: 128 ± 11 |
Bubble goniometer | Coracoid and scapular body |
We found there are clinically meaningful changes in GIR in response to an acute throwing episode over the entire time of a common pitching cycle. These data confirm the findings from other studies that document altered GIR in throwing and serving athletes [10, 14, 22, 23, 26] and supplies additional data concerning the key timeframe of the entire pitching cycle. The early changes, from TP1 to TP3, are consistent with a previous study [22] and the changes from TP3 to TP5 show a continued decline not previously reported. They also show that the decrease in GIR does not return to baseline during the entire pitching cycle. Repetition of these short-term changes could form the basis for developing the documented long-term changes seen in pitchers. These changes have been associated with alterations in glenohumeral kinematics in cocking [2, 11] and follow-through [12] and with shoulder injury [25]. In addition, the absolute values of GIR are below the advocated values of acceptable GIR [2]. These findings indicate conditioning programs should be developed to modify the changes that occur during this time period.
GER does not appear to be meaningfully altered. This is consistent with other studies (Table 3). However, TAM is reduced from TP1-TP5. The amount of change is not clinically important over this short time period but if continued over the entire season could become meaningful.
In contrast to a previous study [10], we did not find any substantial differences between starters and relievers over this pitching time cycle. This difference probably relates to the more controlled environment of regulated pitch counts during spring training compared with the effect of repetitive exposures over the entire season.
We found GIR is dynamic and varies over time depending on the time from pitching exposure. This evidence of a muscular response in which GIR changed over a short timeframe after throwing and failed to return to baseline measurement suggests interventions such as eccentric conditioning programs and stretching programs could be helpful in improving fitness and recovery.
In summary, GIR is a dynamic number, decreasing in response to an acute throwing episode and not returning to baseline before another acute throwing episode. The magnitude and direction of the changes suggest a role in the development of GIRD and its implications for injury and point to the need to develop conditioning programs to modify the changes during the pitching cycle.
Acknowledgments
We thank the Houston Astros Baseball Organization including the coaches, players, team physicians, and athletic training staff for granting us permission to perform the data collection necessary to execute this study.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
Data collection was performed at the Houston Astros Baseball Organization Spring Training Facilities, Kissimmee, FL, USA.
References
- 1.Bigliani LU, Codd TP, Connor PM, Levine WN, Littlefield MA, Herson SJ. Shoulder motion and laxity in the professional baseball player. Am J Sports Med. 1997;25:609–613. doi: 10.1177/036354659702500504. [DOI] [PubMed] [Google Scholar]
- 2.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part I: Pathoanatomy and biomechanics. Arthroscopy. 2003;19:404–420. doi: 10.1053/jars.2003.50128. [DOI] [PubMed] [Google Scholar]
- 3.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part II: Evaluation and treatment of SLAP lesions in throwers. Arthroscopy. 2003;19:531–539. doi: 10.1053/jars.2003.50139. [DOI] [PubMed] [Google Scholar]
- 4.Chandler TJ, Kibler WB, Uhl TL, Wooten B, Kiser A, Stone E. Flexibility comparisons of junior elite tennis players to other athletes. Am J Sports Med. 1990;18:134–136. doi: 10.1177/036354659001800204. [DOI] [PubMed] [Google Scholar]
- 5.Crockett HC, Gross LB, Wilk KE, Schwartz ML, Reed J, O’Mara J, Reilly MT, Dugas JR, Meister K, Lyman S, Andrews JR. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002;30:20–26. doi: 10.1177/03635465020300011701. [DOI] [PubMed] [Google Scholar]
- 6.Dines JS, Frank JB, Akerman M, Yocum LA. Glenohumeral internal rotation deficits in baseball players with ulnar collateral ligament insufficiency. Am J Sports Med. 2009;37:566–570. doi: 10.1177/0363546508326712. [DOI] [PubMed] [Google Scholar]
- 7.Dwelly PM, Tripp BL, Tripp PA, Eberman LE, Gorin S. Glenohumeral rotational range of motion in collegiate overhead-throwing athletes during an athletic season. J Ath Train. 2009;44:611–616. doi: 10.4085/1062-6050-44.6.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ellenbecker TS, Roetert EP, Bailie DS, Davies GJ, Brown SW. Glenohumeral joint total range of motion in elite tennis players and baseball pitchers. Med Sci Sports Exerc. 2002;34:2052–2056. doi: 10.1097/00005768-200212000-00028. [DOI] [PubMed] [Google Scholar]
- 9.Fleisig G, Barrentine SW, Escamilla RF, Andrews JR. Biomechanics of overhand throwing with implications for injuries. Sports Med. 1996;21:421–437. doi: 10.2165/00007256-199621060-00004. [DOI] [PubMed] [Google Scholar]
- 10.Freehill MT, Ebel BG, Archer KR, Bancells RL, Wilckens JH, McFarland EG, Cosgarea AJ. Glenohumeral range of motion in major league pitchers: changes over the playing season. Sports Health. 2011;3:97–104. doi: 10.1177/1941738110374627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grossman MG, Tibone JE, McGarry MH, Schneider DJ, Veneziani S, Lee TQ. A cadaveric model of the throwing shoulder: a possible etiology of superior labrum anterior-to-posterior lesions. J Bone Joint Surg Am. 2005;87:824–831. doi: 10.2106/JBJS.D.01972. [DOI] [PubMed] [Google Scholar]
- 12.Harryman DT, II, Sidles JA, Clark JM, McQuade KJ, Gibb TD, Matsen FA., III Translation of the humeral head on the glenoid with passive glenohumeral motion. J Bone Joint Surg Am. 1990;72:1334–1343. [PubMed] [Google Scholar]
- 13.Hirashima M, Yamane K, Nakamura Y, Ohtsuki T. Kinetic chain of overarm throwing in terms of joint rotations revealed by induced acceleration analysis. J Biomech. 2008;41:2874–2883. doi: 10.1016/j.jbiomech.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 14.Kibler WB, Chandler TJ, Livingston B, Roetert EP. Shoulder range of motion in elite tennis players. Am J Sports Med. 1996;24:279–285. doi: 10.1177/036354659602400306. [DOI] [PubMed] [Google Scholar]
- 15.Laudner KG, Myers JB, Pasquale MR, Bradley JP, Lephart SM. Scapular dysfunction in throwers with pathologic internal impingement. J Orthop Sports Phys Ther. 2006;36:485–494. doi: 10.2519/jospt.2006.2146. [DOI] [PubMed] [Google Scholar]
- 16.Lippitt S, Vanderhooft JE, Harris SL, Sidles JA, Harryman DT, II, Matsen FA., III Glenohumeral stability from concavity-compression: a quantitative analysis. J Shoulder Elbow Surg. 1993;2:27–35. doi: 10.1016/S1058-2746(09)80134-1. [DOI] [PubMed] [Google Scholar]
- 17.Marshall R, Elliott BC. Long axis rotation: the missing link in proximal to distal segment sequencing. J Sports Sci. 2000;18:247–254. doi: 10.1080/026404100364983. [DOI] [PubMed] [Google Scholar]
- 18.Meister K, Day T, Horodyski M, Kaminski TW, Wasik MP, Tillman S. Rotation motion changes in the glenohumeral joint of the adolescent/Little League baseball player. Am J Sports Med. 2005;33:693–698. doi: 10.1177/0363546504269936. [DOI] [PubMed] [Google Scholar]
- 19.Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am J Sports Med. 2006;34:385–391. doi: 10.1177/0363546505281804. [DOI] [PubMed] [Google Scholar]
- 20.Putnam CA. Sequential motions of body segments in striking and throwing skills: descriptions and explanations. J Biomech. 1993;26(Suppl 1):125–135. doi: 10.1016/0021-9290(93)90084-R. [DOI] [PubMed] [Google Scholar]
- 21.Reagan KM, Meister K, Horodyski M, Werner DW, Carruthers C, Wilk KE. Humeral retroversion and its relationship to glenohumeral rotation in the shoulder of college baseball players. Am J Sports Med. 2002;30:354–360. doi: 10.1177/03635465020300030901. [DOI] [PubMed] [Google Scholar]
- 22.Reinhold MM, Wilk KE, Macrina LC, Reinhold MM, Wilk KE, Macrina LC. Changes in shoulder and elbow passive range of motion after pitching in professional baseball players. Am J Sports Med. 2008;36:523–527. doi: 10.1177/0363546507308935. [DOI] [PubMed] [Google Scholar]
- 23.Roetert EP, Ellenbecker TS, Brown SW. Shoulder internal and external rotation range of motion in nationally ranked junior tennis players: a longitudinal analysis. J Strength Cond Res. 2000;14:140–143. [Google Scholar]
- 24.Werner SL, Gill TJ, Murray TA, Cook TD, Hawkins RJ. Relationships between throwing mechanics and shoulder distraction in professional baseball pitchers. Am J Sports Med. 2001;29:354–358. doi: 10.1177/03635465010290031701. [DOI] [PubMed] [Google Scholar]
- 25.Whitehead NP, Weerakkody NS, Gregory JE, Morgan DL, Proske U. Changes in passive tension of muscle in humans and animals after eccentric exercise. J Physiol. 2001;533:593–604. doi: 10.1111/j.1469-7793.2001.0593a.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilk KE, Macrina LC, Fleisig GS, Porterfield R, Simpson CD, 2nd, Harker P, Paparesta N, Andrews JR. Loss of internal rotation and the correlation to shoulder injuries in professional baseball pitchers. Am J Sports Med. 2011;39:329–335. doi: 10.1177/0363546510384223. [DOI] [PubMed] [Google Scholar]
- 27.Wilk KE, Meister K, Andrews JR. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med. 2002;30:136–151. doi: 10.1177/03635465020300011201. [DOI] [PubMed] [Google Scholar]
- 28.Wilk KE, Reinold MM, Macrina LC, Porterfield R, Devine KM, Suarez K, Andrews JR. Glenohumeral internal rotation measurements differ depending on stabilization technique. Sports Health. 2009;1:131–136. doi: 10.1177/1941738108331201. [DOI] [PMC free article] [PubMed] [Google Scholar]