Abstract
Background
Classic bone lengthening requires patients wear external fixation for the distraction and consolidation phases and there is fracture risk after frame removal. Our technique of lengthening with the Taylor Spatial FrameTM and then insertion of a locked plate allows earlier removal of the external fixator during consolidation. Plate insertion is accomplished through a clean pin-free zone avoiding contamination and before frame removal maintaining bone position.
Questions/purposes
We asked (1) whether lengthening and then plating (LAP) decrease the time for external fixation (2) how alignment and complications compare with those of the classic method.
Methods
We performed a retrospective case-matched comparison between LAP and the classic technique with 27 extremities in each group. We compared time wearing the frame, bone healing index, external fixation index, joint ROM, alignment, and complications.
Results
The time wearing the frame and external fixation index were lower in the LAP group (4.5 versus 6.2 months and 1.5 versus 2 months/cm). Deviation from normal alignment was observed in seven and six patients in the LAP and classic group, respectively. Varus malalignment in two patients in the LAP group was associated with plate breakage. The incidence of pin-tract infection was greater in the classic group (12 versus two). No deep infections occurred in the LAP group.
Conclusions
The LAP technique shortened the time patients wore the external fixator but was associated with a high incidence of varus deformity. Stronger plates may help prevent deformity and allow earlier removal of the frame.
Level of Evidence
Level III, therapeutic study (retrospective study). See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Distraction osteogenesis, initially described by Ilizarov [13], is a predictable technique for deformity correction, bone lengthening, and treatment of nonunion. However, it is associated with prolonged external fixation ranging from 1.3 to 2.4 months per centimeter of lengthening [4, 15]. In turn, this leads to increased risk of pin-site infection of 7.5% to 80% [16, 30], hardware breakage of 3% [16], need for lengthy narcotic use, and a 64% patient dissatisfaction rate [10]. There is also an 8% to 30% risk of refracture and deformity after frame removal [7, 21].
Distraction osteogenesis consists of two main phases: distraction and consolidation. Distraction is the lengthening phase which is best accomplished at a rate of 1.0 mm per day [12]. Once the desired length is achieved, the consolidation phase begins. At this time, conversion to internal fixation can be performed to shorten the duration of external fixation. Plates and screws may be inserted during the same surgery as external fixator removal [22]. Other hybrid techniques have been described such as lengthening and then nailing (LATN) [26], plating after lengthening [31], and lengthening over a nail (LON) [24].
Lengthening followed by plating was first described and popularized by Wagner in 1978 [32]. Variations of this technique have been described in a case report [1] and short case series [8, 14, 22, 31, 33]. These variations include using a circular external fixator instead of Wagner device [31, 33], lengthening over a locking plate [1, 14], external fixator removal before plate application [33], and using this approach for bone transport as opposed to traditional bone lengthening [1]. Concerns with these approaches are cross-contamination between external and internal hardware [14, 22, 31, 33], and loss of alignment when the external fixator is removed before plate application [33]. We introduced a new technique using a frame applied in a manner that keeps the approach for subsequent plating free of external fixation. The plating is performed after distraction and while the frame is still on to prevent any loss of position. After the bone is secured with the plate and screws, the external fixator is removed. The intention of the new approach is to minimize the risk of internal hardware contamination and preserve alignment achieved with the external fixator adjustments while minimizing the time patients wear the external fixator. The plate also may protect against refracture.
We therefore asked whether the LAP technique would (1) reduce the time the patient wears the external fixator (external fixation index [EFI]); (2) reduce the time to achieve bone healing (bone healing index [BHI]); (3) improve limb alignment; (4) maintain ROM of adjacent joints; and (5) reduce complications compared with classic lengthening.
Patients and Methods
We performed a retrospective case-matched comparison of patients who underwent LAP and those who underwent classic lengthening. From 2006 to 2009, we treated 25 patients (27 extremities) with the LAP technique. Proximal tibia lengthening was performed in 21 cases and distal femoral lengthening in six. In general, we perform LON for femoral lengthening and LATN for tibial lengthening. Indications for the LAP procedure were deformity about the knee requiring a metaphyseal osteotomy and any other problems precluding the use of an intramedullary nail, including, for example, a tight intramedullary canal. Contraindications were a history of osteomyelitis at the osteotomy site and poor skin condition at the proposed plate insertion site. From 2000 to 2010, we treated 87 patients with a classic approach. As controls, we identified 26 of these 87 patients (27 extremities) and matched them for etiology (Table 1), age, amount of lengthening (cm), mechanical axis deviation (MAD), and tibia/femur distribution (Table 2). The minimum followup was 28 months (mean, 45 months; range, 28–63 months) for the LAP group and 25 months (mean, 80 months; range, 25–140 months) for the classic group. No patients were lost to followup. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs.
Table 1.
Etiology
| Etiology | LAP | Classic |
|---|---|---|
| Bilateral (short stature) | 2 | 2 |
| Malunion | 4 | 7 |
| Nonunion | 8 | 8 |
| Congenital | 2 | 4 |
| Polio | 3 | 1 |
| Growth arrest | 3 | 4 |
| Developmental | 3 | 1 |
| Other | 2 | 0 |
LAP = lengthening then plating.
Table 2.
Demographics
| Parameter | LAP | Classic |
|---|---|---|
| Age (years)* | 41.3 (35.9–46.8) | 41.1 (36.1–46.2) |
| Lengthening (cm)* | 3.6 (3.1–4.0) | 3.5 (2.9–4.1) |
| Number of extremities | 27 | 27 |
| Number of tibiae | 21 | 21 |
| Number of femora | 6 | 6 |
| Tibia lengthening (cm)* | 3.7 (3.1–4.3) | 3.6 (2.8–4.4) |
| Femur lengthening (cm)* | 3.1 (2.6–3.6) | 3.2 (2.5–3.8) |
* Mean and confidence interval; LAP = lengthening then plating.
The gender distribution in the two groups was similar (p = 0.1): 17 male patients in the classic group and 10 in the LAP group versus nine female patients in the classic group and 15 in the LAP group. The relative proportions of the sides also were similar (p = 0.4): 12 left sides in the classic group and 15 left sides in the LAP group.
We used a Taylor Spatial FrameTM (Smith and Nephew, Memphis, TN, USA) (FDA-approved) in all patients. Our typical external fixator application consisted of the following steps. We used a “rings first” [25] method for mounting the external fixator. We began with a fibular osteotomy. We used a lateral approach to the middle 1/3 of the fibula using the interval between the lateral and posterior compartments. Multiple drill holes were made, and the osteotomy was completed using an osteotome. The proximal tibia 2/3 (open) ring then was applied. This was our reference ring. We rotated the ring such that the open section was facing laterally, simplifying future lateral plate placement (Fig. 1). Bone fixation of the proximal ring consisted of three tapered, 6-mm hydroxyapatite-coated half-pins (Biomet, Warsaw, IN, USA). All pins were placed from the medial side to prevent contact with the area of future plate placement (Fig. 1). We used a medial half-pin to stabilize the proximal tibiofibular using a cannulated technique described by Green [11]. We fixed the distal tibiofibula syndesmosis at the ankle with one 4.5-mm quadricortical screw or a tensioned tibiofibular wire. Mounting parameters were obtained for the proximal ring [9] for later use with the Taylor Spatial FrameTM web-based software [28]. The distal ring then was attached at the midtibia level. This was done using a 1.8-mm medial face wire going anterolateral to posteromedial and two anteromedial half-pins. The six Taylor Spatial FrameTM struts were attached and their lengths were recorded. The struts then were detached from the proximal ring, and the tibial osteotomy was performed. This was done using a percutaneous technique under C-arm fluoroscopy. The Taylor Spatial FrameTM struts were reattached providing an anatomic reduction of the osteotomy. Next, mounting parameters were obtained intraoperatively using the C-arm as described previously [9].
Fig. 1A–D.
(A) Anteroposterior, (B) lateral, and (C) axial views of a plastic bone model of the external fixator configuration and lateral plate placement for proximal tibia lengthening are shown. (D) An intraoperative photograph shows a plate provisionally fixed to the tibia with the external fixator covered with blue towels.
The osteotomy and external fixator application were similar for patients in the classic group. The proximal tibia 2/3 ring in this group was applied in traditional fashion with the opening on the back for uninhibited knee flexion.
Postoperatively the patients were allowed to bear weight as tolerated on the affected extremity using crutches or a walker. A Taylor Spatial FrameTM strut adjustment schedule (using the total residual mode) was generated using the web-based software. The patients started their own adjustments on postoperative Day 7 at a rate of 1 mm/day. Postoperatively, the patients in both groups followed a routine protocol as described previously [27]. Knee and ankle ROM exercises were encouraged with supervision of a physical therapist three times per week for 1 hour. Patients also were given a daily 1-hour home therapy program. Patients with bilateral deformities had staged correction with surgery on the second-side typically at 6 to 8 weeks after the first side. ROM exercises of the knee and ankle were encouraged. A daily shower, including washing the pin sites with antibacterial soap, was encouraged. This was followed by daily pin care with half-strength hydrogen peroxide and then coverage of pin sites with a dry sterile gauze wrap. Patients were seen in the clinic every 10 to 14 days by the senior author (SRR) during the distraction phase. During each office visit the patients in both groups were examined clinically including inspection of the external fixator, pin sites, and ROM in adjacent joints. Neurovascular status also was assessed routinely to detect any neuropathy related to the distraction and deformity correction process. Anteroposterior and lateral radiographs were obtained at each visit and long leg radiographs were obtained on completion of the adjustment schedule.
The distraction phase was completed when the necessary length and desired alignment were achieved. We then performed the locking plate insertion and removal of the external fixator. A proximal tibia locking plate (Smith and Nephew) (FDA-approved) was used. The external fixator was prepared in the field, all of the pin sites were covered with Betadine® (Purdue Pharma LP, Stamford, CT, USA) -soaked gauze, and the external fixator was covered with sterile blue towels (Fig. 1). It was necessary to insert the plate with the external fixator still in place. The newly formed regenerate bone was not mature or rigid enough to maintain length at the time of plate insertion. The external fixator also served to maintain the bone in an ideal alignment during plate insertion. We inserted the in situ submuscular plate using a 4-cm lateral incision over the proximal tibia. The distal locking screws were inserted using an external targeting jig using small stab skin incisions and blunt dissection down to the plate. Contact between internal and external fixation was avoided. The external fixator was removed only after the plate stabilized the bone. Autologous bone marrow aspirate concentrate (BMACTM; Harvest Technologies, Plymouth, MA, USA) was injected into the regenerate in 15 extremities at the time of plating.
Postoperatively the patients remained toe-touch weightbearing for approximately 6 weeks until three of four cortices of bridging callus of the regenerate were observed. During this time the patients continued supervised physical therapy to maintain ROM in adjacent joints. The patients were seen in the clinic first 2 weeks after the surgery and every 4 to 6 weeks afterward. During each visit, all surgical wounds were inspected, neurovascular status was assessed, gross extremity alignment was noted, and adjacent joint ROM was documented. Anteroposterior, lateral, and long leg radiographs were obtained (Fig. 2). When deemed appropriate, gradual transition to full weightbearing was allowed during a period of 4 weeks.
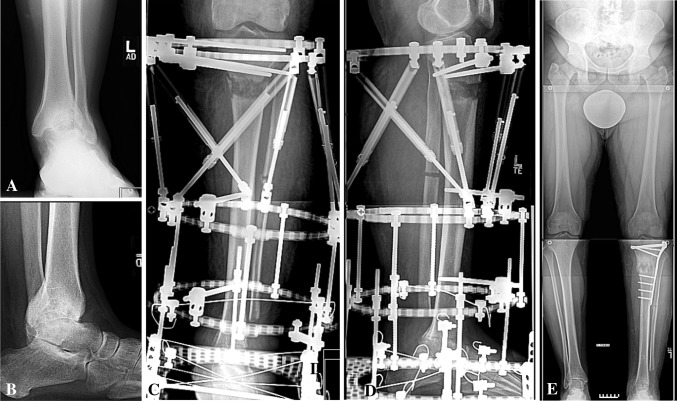
Fig. 2A–E.
(A) AP and (B) lateral radiographs of the left ankle of a 49-year-old man with advanced left ankle arthritis and varus deformity are shown. The patient was treated with ankle fusion and simultaneous proximal tibia lengthening. (C) AP and (D) lateral radiographs of his left tibia are shown. Using the LAP protocol in this case allowed us to remove the external fixator as soon as ankle fusion was achieved. To protect the proximal tibia regenerate, a lateral tibia plate was used. (E) A long leg standing radiograph shows equalization of leg length and good alignment.
Information regarding time wearing the frame, knee and ankle ROM, alignment, and complications were extracted from the medical records. We used the classification described by Paley [23] to define complications. According to that classification, true complications are all intraoperative injuries and all problems during lengthening that are not resolved by the end of the treatment. Even though pin-tract infection and cellulitis were not considered true complications according to this classification, they still were included in the analysis as we thought they could be relevant when comparing the LAP and classic groups.
All radiographs were evaluated by one observer (SRR). We used serial radiographs to determine the BHI. Bony union was determined by radiographs showing three of four cortices of bridging callus. Alignment was assessed by measuring the MAD on a 51-inch bipedal standing radiograph. MAD was considered normal within the range of 6 mm lateral to 17 mm medial. The same radiographs were used to assess leg length discrepancy. There were no missing radiographs. We computed BHI and EFI. BHI was defined as the time until bony union in months divided by the amount of lengthening in centimeters. EFI was defined as the time wearing the external fixator in months divided by the amount of lengthening in centimeters. Before taking radiographs, the leg length discrepancy was estimated clinically and appropriate height blocks were used under the foot of the short leg to level the patient’s pelvis and improve reliability of measurement of the discrepancy.
Using the classic group results, we examined data distribution for the EFI data. The mean was 2 months/cm and the median was 1.7 months/cm. Assuming a Mann-Whitney test, our power would be greater than 70% to detect a difference greater than 0.6 (18 days/cm difference between the two groups) with 27 extremities per group. This seemed to be an important clinical difference.
The Shapiro-Wilk test was used to check if outcome variables could be considered normally distributed. They could not. Therefore, Mann-Whitney analysis was used to determine outcome differences between the classic and LAP groups (EFI, BHI, and ROM). Considering the limited sample size, Fisher’s exact test was used to determine differences in the incidence of malalignment and complications. We used StatXact 8 (Cytel Inc, Cambridge, MA, USA) SYSTAT 12 and SYSTAT 13 (SYSTAT Software Inc, Chicago, IL, USA) and PASS (NCSS, Kaysville, UT, USA) for all analyses.
Results
The average amount of lengthening was similar between the two groups (3.6 cm in the LAP group versus 3.5 cm in the classic group [Table 2]). Time wearing the external fixator was shorter (p = 0.006) in the LAP group than in the classic group (4.5 months versus 6.2 months) (Table 3). The EFI also was lower (p < 0.001) in LAP group compared with the classic group (1.3 months/cm versus 2.0 months/cm). The BHI was similar (p = 0.6) in both groups (2.1 months/cm in the LAP group versus 2.2 months/cm in the classic group [Fig. 3]). Bone regenerate healing was not altered by insertion of the plate.
Table 3.
Clinical results
| Parameter | LAP | Classic | p value |
|---|---|---|---|
| Followup (months) | 45.0 (27.8–63.1) | 80.4 (25.2–140) | < 0.001 |
| Time wearing frame (months) | 4.5 (1.7–10.5) | 6.2 (3.4–11.8) | 0.006 |
| ED to frame removal interval (days) | 57.8 (0–233) | 123.3 (45–234) | < 0.001 |
| EFI (months/cm) | 1.3 (0.5–3.4) | 2.0 (1.0–4.0) | < 0.001 |
| BHI (months/cm) | 2.1 (0.9–5.5) | 2.2 (1.1–4.2) | 0.6 |
LAP = lengthening then plating; ED = end of distraction; EFI = external fixator index; BHI = bone healing index.
Fig. 3A–D.
Patient distributions are shown for the (A) time wearing the external fixator, (B) interval from the end of distraction to external fixator removal, (C) external fixation index (EFI), and (D) bone healing index (BHI). LAP = lengthening then plating; ED = end of distraction; ex fix = external fixator.
Ankle and knee ROM did not change with the treatment and was similar in both groups (Table 4). Knee stiffness developed in one patient undergoing femoral lengthening in the LAP group and in three undergoing femoral lengthening in the classic group.
Table 4.
Knee and ankle ROM
| ROM | LAP (degrees) | Classic (degrees) |
|---|---|---|
| Preoperative knee | ||
| Extension | −1.5 (−20–10) | −1.7 (−15–5) |
| Flexion | 124.1 (50–140) | 130.6 (125–140) |
| Postoperative knee | ||
| Extension | −0.8 (−10–0) | −1.0 (−10–0) |
| Flexion | 120.1 (45–130) | 127.0 (60–155) |
| Preoperative ankle | ||
| Dorsiflexion | 2.1 (−20–15) | 9.2 (−10–25) |
| Plantar flexion | 40.1 (0–90) | 46.0 (20–70) |
| Postoperative ankle | ||
| Dorsiflexion | 2.1 (0–10) | 11.8 (0–20) |
| Plantar flexion | 42.9 (20–65) | 42.8 (20–70) |
LAP = lengthening then plating.
In the LAP group, the mechanical axis shifted medially in seven patients, and in the classic group, the mechanical axis shifted laterally in six patients (Table 5). The medial MAD was associated with failure of the lateral plate in two patients. The plate fractured through one of the proximal holes in both patients which necessitated hardware removal and external fixator reapplication in one patient (Fig. 4). The other five patients with medial MAD shift had intact hardware but collapse of the medial regenerate. In one patient the collapse was addressed by removing the locking screw, correcting the deformity, unbending the plate, and reinserting the locking screws and by plate removal followed by reapplication of the Taylor Spatial FrameTM in the other patient. The magnitude of the deformity in the other five patients with varus malalignment was less substantial, and after appropriate discussion with the patients, this was accepted. Therefore, lateral plate insertion appeared to protect against valgus deformity but increased the risk for varus malalignment. After this was realized, we changed our protocol by delaying removal of the external fixator and plate insertion until farther into the consolidation period. Regenerate collapse into valgus in the classic group required deformity correction with plating in two patients.
Table 5.
Complications
| Complication | LAP | Classic | p value | ||
|---|---|---|---|---|---|
| Tibia | Femur | Tibia | Femur | ||
| Regenerate collapse | 7 (varus) | 0 | 5 (valgus) | 1 (valgus) | 1.0 |
| Broken plate | 2 | 0 | N/A | N/A | N/A |
| Reoperation for malalignment | 2 | 0 | 2 | 0 | 1.0 |
| Pin-site infection | 2 | 0 | 10 | 2 | 0.004 |
| Cellulitis | 2 | 0 | 2 | 0 | 1.0 |
| Deep infection | 0 | 0 | 1 | 0 | 1.0 |
| Nonunion | 0 | 0 | 0 | 0 | 1.0 |
| Knee stiffness | 0 | 1 | 0 | 3 | 0.61 |
LAP = lengthening then plating; N/A = not applicable.
Fig. 4A–C.
A 57-year-old man had ankle fusion for a right distal tibia nonunion with bone loss which resulted in 3.6 cm shortening. This was addressed by proximal tibia lengthening using the LAP protocol. The external fixator was removed at 4.8 months and the patient was advised to be toe-touch weightbearing. However, (A) progressive regenerate collapse into varus that eventually resulted in plate breakage was observed on a followup radiograph. The proximal hardware was removed, the external fixator was reapplied, and a proximal tibia osteotomy was performed. (B) The deformity was gradually corrected and alignment was fully restored. (C) The external fixator was removed in 4 months after reliable healing of the osteotomy was confirmed. The alignment remained unchanged at subsequent followups.
The incidence of pin-tract infection was greater (p = 0.004) in the classic group (12 of 27 extremities) versus the LAP group (two of 27 extremities). Deep infection occurred in one patient in the classic group and was treated with intravenous antibiotics. Two patients in each group had cellulitis. In the LAP group both cases resolved completely with intravenous antibiotics. Subsequent plating and external fixator removal were performed as one procedure, without a deviation in the protocol. There were no cases of deep infection in the LAP group.
Discussion
We describe a new hybrid technique of limb lengthening and a retrospective case-matched comparison of the outcomes of this technique versus the classic approach. The overall goal of a hybrid approach to bony lengthening is to shorten the duration of wearing an external fixator by safely converting to internal hardware as soon as the distraction phase is completed. The LATN technique was described previously [26]. However, there are situations in limb lengthening when replacing an external fixator with a plate is preferable to an intramedullary nail. We asked how the LAP compares with traditional lengthening with external fixation with respect to: (1) the time needed wearing an external fixator; (2) bone healing; (3) limb alignment; (4) ROM of adjacent joints; and (5) complications.
We note limitations of our study. First, it was not randomized. However, we believe that selection bias was minimized in this study as most of our patients who underwent metaphyseal lengthening from 2006 to 2009 underwent LAP unless it was contraindicated or the patient elected the classic protocol. Second, we were unable to completely match the patients in the classic and LAP groups with respect to etiology. The sample number in our study is limited, and our primary parameters in case matching were amount of lengthening, tibia and femur distribution, and patient age. These are not such common procedures that we could match in all respects. We believe that incomplete etiologic matching would not have a substantial impact on our study variables. Another aspect of incomplete matching of the two groups was bone marrow aspirate injections in 15 patients in the LAP group only. There are no data in the current literature regarding whether a bone marrow injection has impact on bone regenerate maturation. Although we realize that this a limitation of our study, we suspect that bone marrow injections may not cause a substantial effect in this instance as BHI calculations in our LAP group were not different from those for the classic group where bone marrow injections were not used. Third, we realize limitations of our approach to defining bony union. According to the literature, there is considerable interobserver variability in assessing fracture healing, particularly early [19]. Moreover, there is no consensus in the current literature for the definition of bony healing for fractures [3, 6], let alone bone regenerate healing in distraction osteogenesis. Perhaps owing to the limitations of our approach, we tended to overestimate healing of the regenerate and allowed for earlier weightbearing which led to a relatively high rate of malalignment in both groups.
The EFI for the LAP group was higher than previously reported (Table 6). This might be attributable to the differences in patient population between our study (mostly adults) and previous studies (children and adolescents). The EFI for the classic group was similar to those previously reported (Table 7).
Table 6.
Literature summary of lengthening and plating
| Study | Population | Design | Anatomic location | Type of external fixator | External fixator index | Final alignment | Reported complications | Technique details |
|---|---|---|---|---|---|---|---|---|
| Apivatthakakul & Arpornchayanon [1] | Two adolescents | Case report | Femur | Wagner lengthening device | 0.31 and 0.37 month/cm | Mild posterior angulations and varus of distal femur. | Knee stiffness in one patient | Bone transport cases for severely comminuted open distal femur fractures |
| Endo et al. [8] | Five adolescents | Retrospective | Femur | Monolateral external fixator | 24.6 days/cm | No change in alignment noted. | No infection reported. One patient had knee stiffness develop but almost full motion was regained after surgical release. | External fixator applied anterolaterally to avoid contact with the laterally inserted plate |
| Iobst & Dahl [14] | Six children | Case series | Femur (5) and tibia (1) | Ilizarov external fixator | 0.42 month/cm | Procurvatum deformity in 3 patients, one corrected with osteotomy | One pin-tract infection, transient knee stiffness, premature consolidation, fracture at the edge of the plate | Plating was done at the time of external fixator application |
| Oh et al. [22] | Eight children | Case series | Femur (3) and tibia (5) | Ilizarov ring fixator and monolateral external fixator | 26.93 days/cm | N/A | One pin-tract infection | Four lengthening and four bone transport series |
| Uysal et al. [31] | Five adults | Case series | Femur (1) and tibia (4) | Ilizarov external fixator | 20 days/cm | N/A | Three pin-tract infections, 2 delayed consolidations, 1 knee contracture | Anteromedial plating for tibia and lateral for femur |
| Wu et al. [33] | 18 adults | Case series (non-union with shortening) | Tibia | Ilizarov external fixator | Not reported | No malalignment noted | N/A | After external fixator removal, lamina spreader was used to maintain the length. Iliac crest autologous bone graft used in all cases. |
| Current study | 26 adults and one adolescent | Retrospective | Femur (6) and tibia (21) | Taylor Spatial FrameTM | 1.3 months/cm | Medial MAD in 7 patients | Two cases of pin-tract infection, 2 cases of cellulitis, 2 plates broke, 1 knee stiffness. | Taylor Spatial FrameTM was applied in such a fashion that lateral plating was done later without any contact with the external fixator. External fixator was removed after completion of plate application to prevent loss of alignment. |
MAD = medial axial deviation; N/A = not available; Taylor Spatial FrameTM (Smith and Nephew, Memphis, TN, USA).
Table 7.
Literature summary of classic lengthening
| Study | Population | Design | Anatomic location | Type of external fixator | External fixation index | Technique details |
|---|---|---|---|---|---|---|
| Aston et al. [2] | 27 children and adolescents | Case series | Femur | One Taylor Spatial FrameTM, the rest were classic Ilizarov frames | 39.97 days/cm | Seven lengthenings were done over the Ruch nail |
| Blondel et al. [4] | 36 children and adolescents | Prospective study | Tibia (26), femur (6), other (4) | All Taylor Spatial FramesTM | 38.2 days/cm | 67 deformities in three spatial planes also were corrected |
| Catagni et al. [5] | 54 adults | Case series | Tibia | Hybrid (half-pins and wires) Ilizarov external fixator | 40.7 days/cm | Bifocal tibia lengthening was performed |
| Kristiansen et al. [15] | 47 children and adults | Retrospective | Tibia | 20 patients treated with Taylor Spatial FrameTM, 27treated with Ilizarov fixator | 2.4 months/cm for Taylor Spatial FrameTM, 1.8 months/cm for Ilizarov fixator | Proximal and distal tibia osteotomies were used |
| Lie & Chow [17] | Eight children and adults | Retrospective | Femur (5), tibia (9) | Ilizarov and monolateral external fixators | 48 days/cm | |
| Matsubara et al. [18] | 28 children and adults | Retrospective | Tibia (17), femur (17) | Ilizarov fixator (21) and Taylor Spatial FrameTM (7) | 58.6 days/cm with acute deformity correction and 42.5 days/cm for gradual deformity correction | A group that underwent acute deformity correction after lengthening was compared with a group that had gradual correction and lengthening |
| Nakase et al. [20] | 10 children and adults | Case series | Tibia (6), femur (4) | Taylor Spatial FrameTM | 57.8 days/cm | |
| Song et al. [29] | 14 children and adults | Retrospective | Tibia | Ilizarov external fixator | 1.8 months/cm for classic group and 2.0 months/cm for nail group | Lengthening over a nail in three cases and classic lengthening in 11 |
Taylor Spatial FrameTM (Smith and Nephew, Memphis, TN, USA).
Considering the abovementioned difficulties of defining bone healing, it would be difficult to compare our BHI data with that in the literature. The same approach in determining BHI was used in a study of LATN, another hybrid technique [26]. The LATN protocol led to substantial acceleration of regenerate healing with a BHI of 0.8 versus 1.9 for the classic group. The BHI for the LAP group was 2.1 months/cm. Based on these findings we recommend LATN over LAP whenever possible.
Only one patient undergoing femoral lengthening in the LAP group had knee stiffness develop. This complication also was recorded in four of six previous studies (Table 6).
Malalignment after using a hybrid technique for lengthening is not a new finding. In one study of femoral lengthening with submuscular plate stabilization it was as much as 50% [14]. We observed a 27% incidence of varus malalignment in the LAP group. We realize that this is rather high rate of malalignment after lengthening. We analyzed all cases of varus malalignment in the LAP group and concluded that it occurred owing to conversion to internal fixation too early at the beginning of the consolidation phase, and the standard lateral tibia locking fracture plate is not strong enough to support an immature regenerate. Therefore, we improved stability of the plate by increasing the width and thickness of the standard plate by 2 mm. In addition, the plate holes were removed at the level of the regenerate where we observed metal fatigue failure in two patients. We have used this new custom-made plate on one patient with a good outcome. To prevent varus collapse we postponed the timing of conversion to internal fixation, allowing for some regenerate maturation. This delay in plating led to the only modest decrease in EFI compared with the classic technique. In addition, we now prohibit progression to full weightbearing on the plate until after solid healing is observed on radiographs.
Analysis of complications in both cohorts showed a lower incidence of pin-tract infection in the LAP group, similar to the incidence in the LATN study [26]. In another study, it was as much as 60% [31]. The most obvious explanation for the lower pin-tract infection rate in our study is the shorter duration of external fixation in the LAP cohort led to less infection. Despite the concern of deep infection, there were no cases noted in the LAP group. We feel that this is related to the meticulous separation between internal and external fixation.
Early conversion of external fixation to a plate after completion of the distraction phase allows for shortening of the duration of external fixation for lengthening. The Taylor Spatial FrameTM can be used effectively for this protocol. Unlike the LATN hybrid technique, bone healing is not accelerated by the LAP method. We suggest using the LATN technique, if possible, for tibial lengthening. The injection of bone marrow aspirate into the regenerate to speed the healing process requires additional study. Nonweightbearing, delayed conversion from external fixation to plating, and use of a customized, stronger plate may help decrease high varus malunion rate and hardware failure seen in the LAP group. Patients who have classic lengthening may benefit from more time wearing the frame and avoid an approximately 25% chance of valgus malunion associated with that technique. At the last followup, joint ROM was not affected by either technique. There was no increased rate of infection with conversion to internal fixation despite the prolonged use of an external fixator. A lower rate of knee stiffness is another possible advantage of LAP.
Although LAP did decrease the time for external fixation, the improvement was modest and there was a high incidence of varus deformity. We think that the use of a stronger custom-made plate will improve these shortcomings. Further study is needed.
Acknowledgments
We thank Margaret Peterson PhD for assistance with the statistical analysis.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution has approved the reporting of these cases, that all investigations were conducted inconformity with ethical principles of research, and that informed consent for participating in the study was obtained.
References
- 1.Apivatthakakul T, Arpornchayanon O. Minimally invasive plate osteosynthesis (MIPO) combined with distraction osteogenesis in the treatment of bone defects: a new technique of bone transport. A report of two cases. Injury. 2002;33:460–465. doi: 10.1016/S0020-1383(02)00010-4. [DOI] [PubMed] [Google Scholar]
- 2.Aston WJ, Calder PR, Baker D, Hartley J, Hill RA. Lengthening of the congenital short femur using the Ilizarov technique: a single-surgeon series. J Bone Joint Surg Br. 2009;91:962–967. doi: 10.1302/0301-620X.91B7.21304. [DOI] [PubMed] [Google Scholar]
- 3.Bhandari M, Guyatt GH, Swiontkowski MF, Tornetta P, 3rd, Sprague S, Schemitsch EH. A lack of consensus in the assessment of fracture healing among orthopaedic surgeons. J Orthop Trauma. 2002;16:562–566. doi: 10.1097/00005131-200209000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Blondel B, Launay F, Glard Y, Jacopin S, Jouve JL, Bollini G. Limb lengthening and deformity correction in children using hexapodal external fixation: preliminary results for 36 cases. Orthop Traumatol Surg Res. 2009;95:425–430. doi: 10.1016/j.otsr.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Catagni MA, Lovisetti L, Guerreschi F, Combi A, Ottaviani G. Cosmetic bilateral leg lengthening: experience of 54 cases. J Bone Joint Surg Br. 2005;87:1402–1405. doi: 10.1302/0301-620X.87B10.16468. [DOI] [PubMed] [Google Scholar]
- 6.Corrales LA, Morshed S, Bhandari M, Miclau T., 3rd Variability in the assessment of fracture-healing in orthopaedic trauma studies. J Bone Joint Surg Am. 2008;90:1862–1868. doi: 10.2106/JBJS.G.01580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Danziger MB, Kumar A, DeWeese J. Fractures after femoral lengthening using the Ilizarov method. J Pediatr Orthop. 1995;15:220–223. [PubMed] [Google Scholar]
- 8.Endo H, Asaumi K, Mitani S, Noda T, Minagawa H, Tetsunaga T, Ozaki T. The minimally invasive plate osteosynthesis (MIPO) technique with a locking compression plate for femoral lengthening. Acta Med Okayama. 2008;62:333–339. doi: 10.18926/AMO/30972. [DOI] [PubMed] [Google Scholar]
- 9.Gantsoudes GD, Fragomen AT, Rozbruch SR. Intraoperative measurement of mounting parameters for the Taylor Spatial Frame. J Orthop Trauma. 2010;24:258–262. doi: 10.1097/BOT.0b013e3181c2f7f0. [DOI] [PubMed] [Google Scholar]
- 10.Gereli A, Nalbantoglu U, Kocaoglu B, Turkmen M. Comparison of palmar locking plate and K-wire augmented external fixation for intra-articular and comminuted distal radius fractures. Acta Orthop Traumatol Turc. 2010;44:212–219. doi: 10.3944/AOTT.2010.2325. [DOI] [PubMed] [Google Scholar]
- 11.Green SA. Pin and wire technique for external fixation. Instr Course Lect. 1995;44:487–493. [PubMed] [Google Scholar]
- 12.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res. 1989;239:263–285. [PubMed] [Google Scholar]
- 13.Ilizarov GA. Transosseous Osteosynthesis: Theoretical and Clinical Aspects of the Regeneration and Growth of Tissue. New York, NY: Springer-Verlag; 1992. [Google Scholar]
- 14.Iobst CA, Dahl MT. Limb lengthening with submuscular plate stabilization: a case series and description of the technique. J Pediatr Orthop. 2007;27:504–509. doi: 10.1097/01.bpb.0000279020.96375.88. [DOI] [PubMed] [Google Scholar]
- 15.Kristiansen LP, Steen H, Reikeras O. No difference in tibial lengthening index by use of Taylor spatial frame or Ilizarov external fixator. Acta Orthop. 2006;77:772–777. doi: 10.1080/17453670610012971. [DOI] [PubMed] [Google Scholar]
- 16.Lerner A, Chezar A, Haddad M, Kaufman H, Rozen N, Stein H. Complications encountered while using thin-wire-hybrid-external fixation modular frames for fracture fixation: a retrospective clinical analysis and possible support for “Damage Control Orthopaedic Surgery”. Injury. 2005;36:590–598. doi: 10.1016/j.injury.2004.08.035. [DOI] [PubMed] [Google Scholar]
- 17.Lie CW, Chow W. Limb lengthening in short-stature patients using monolateral and circular external fixators. Hong Kong Med J. 2009;15:280–284. [PubMed] [Google Scholar]
- 18.Matsubara H, Tsuchiya H, Sakurakichi K, Watanabe K, Tomita K. Deformity correction and lengthening of lower legs with an external fixator. Int Orthop. 2006;30:550–554. doi: 10.1007/s00264-006-0133-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McClelland D, Thomas PB, Bancroft G, Moorcraft CI. Fracture healing assessment comparing stiffness measurements using radiographs. Clin Orthop Relat Res. 2007;457:214–219. doi: 10.1097/BLO.0b013e31802f80a8. [DOI] [PubMed] [Google Scholar]
- 20.Nakase T, Kitano M, Kawai H, Ueda T, Higuchi C, Hamada M, Yoshikawa H. Distraction osteogenesis for correction of three-dimensional deformities with shortening of lower limbs by Taylor Spatial Frame. Arch Orthop Trauma Surg. 2009;129:1197–1201. doi: 10.1007/s00402-008-0702-y. [DOI] [PubMed] [Google Scholar]
- 21.O’Carrigan T, Paley D, Herzenberg JE. Obstacles in limb lengthening: fractures. In: Rozbruch SR, Ilizarov S, editors. Limb Lengthening and Reconstruction Surgery. New York, NY: Informa Healthcare; 2007. pp. 675–679. [Google Scholar]
- 22.Oh CW, Shetty GM, Song HR, Kyung HS, Oh JK, Min WK, Lee BW, Park BC. Submuscular plating after distraction osteogenesis in children. J Pediatr Orthop B. 2008;17:265–269. doi: 10.1097/BPB.0b013e32830688d8. [DOI] [PubMed] [Google Scholar]
- 23.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 24.Paley D, Herzenberg JE, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail: a matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am. 1997;79:1464–1480. doi: 10.2106/00004623-199710000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Rozbruch SR, Fragomen AT, Ilizarov S. Correction of tibial deformity with use of the Ilizarov-Taylor spatial frame. J Bone Joint Surg Am. 2006;88(suppl 4):156–174. doi: 10.2106/JBJS.F.00745. [DOI] [PubMed] [Google Scholar]
- 26.Rozbruch SR, Kleinman D, Fragomen AT, Ilizarov S. Limb lengthening and then insertion of an intramedullary nail: a case-matched comparison. Clin Orthop Relat Res. 2008;466:2923–2932. doi: 10.1007/s11999-008-0509-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rozbruch SR, Segal K, Ilizarov S, Fragomen AT, Ilizarov G. Does the Taylor Spatial Frame accurately correct tibial deformities? Clin Orthop Relat Res. 2010;468:1352–1361. doi: 10.1007/s11999-009-1161-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith & Nephew Inc. Taylor Spatial FrameTM Software. Available at: www.spatialframe.com. Accessed October 19, 2011.
- 29.Song HR, Myrboh V, Oh CW, Lee ST, Lee SH. Tibial lengthening and concomitant foot deformity correction in 14 patients with permanent deformity after poliomyelitis. Acta Orthop. 2005;76:261–269. doi: 10.1080/00016470510030670. [DOI] [PubMed] [Google Scholar]
- 30.Temple J, Santy J. Pin site care for preventing infections associated with external bone fixators and pins. Cochrane Database Syst Rev. 2004;1:CD004551. [DOI] [PubMed]
- 31.Uysal M, Akpinar S, Cesur N, Hersekli MA, Tandogan RN. Plating after lengthening (PAL): technical notes and preliminary clinical experiences. Arch Orthop Trauma Surg. 2007;127:889–893. doi: 10.1007/s00402-007-0442-4. [DOI] [PubMed] [Google Scholar]
- 32.Wagner H. Operative lengthening of the femur. Clin Orthop Relat Res. 1978;136:125–142. [PubMed] [Google Scholar]
- 33.Wu CC, Lee ZL, Wu CC, Lee ZL. Speeded gradual lengthening and secondary angled blade plate stabilisation for proximal tibial shaft non-union with shortening. Int Orthop. 2008;32:693–696. doi: 10.1007/s00264-007-0370-5. [DOI] [PMC free article] [PubMed] [Google Scholar]