Abstract
Very little is known about predictors of subjective health status among African American adolescents. This study was designed to determine whether selected anthropometric, psychological, lifestyle behavioral, and structural variables predicted poor self-rated general health in a cross-sectional non-clinical sample of 310 female African American adolescents, 14 to 18 years old. The odds of reporting poor self-rated health were 2 to 3 times greater for African American teens from lower socioeconomic households when compared to teens residing in higher socioeconomic households and for those reporting infrequent participation in activities that promote spiritual well-being compared to those who participate more frequently in activities that enhance spiritual health. Findings indicate that socioeconomic level and engagement in behaviors that enhance healthy spirituality appear to be the most salient predictors of self-rated health. In addition to biodiversity considerations that influence perceptions of health status, culturally focused interventions should integrate variables shown to influence self-rated health among African American teens. These inclusions may inform a more integrated understanding of health, health outcomes, and health disparities in this vulnerable population.
Keywords: African Americans, adolescents, health status, obesity
Self-rated health (SRH) is a widely used global indicator of future health outcomes. Recognized as a broad summary measure of general well-being, SRH is most frequently measured using a single question that asks respondents to rate their overall health on a scale from excellent to poor. The resulting responses are often dichotomized as poor versus the remaining groupings. SRH is generally accepted as a highly reliable and valid predictive of population health and has been used in large-scale surveillance studies of health status (Liao et al., 2011). An extensive body of evidence documents that even after adjustment for other measured health related covariates, individuals who perceive their health negatively demonstrate significantly increased odds for morbidity, all-cause mortality and disability than their counterparts reporting excellent or good health (DeSalvo, Bloser, Reynolds, He, & Muntner, 2006; Gander et al., 2011; Idler & Benyamini, 1997).
Recently researchers have also documented associations between poor SRH and several cardio-metabolic and immunologic disease trait biomarkers (Nakata, Takahashi, Otsuka, & Swanson, 2010; Tomten & Hostmark, 2007). Based on the strengths of findings in the extant literature, measures of SRH have been recommended for use in population health monitoring by domestic and international public health organizations including the Centers for Disease Control and Prevention (CDC), European Union, and World Health Organization (de Bruin, Picavet, & Nossikov, 1996; Hennessy, Moriarty, Zack, Scherr, & Brackbill, 1994; Kramers, 2003). Moreover, a 2009 report by The Institute of Medicine (2009) highlighted the importance of perceived health status by endorsing the use of “poor” SRH as a benchmark for tracking health evolution in the United States.
A number of previous researchers have identified measured anthropometric trait variables as potential predictive risk parameters for poor SRH. Chief among these characteristics is body mass index (BMI). BMI is generally considered to be a reliable, indirect indicator for body fatness and is commonly used to define normal weight, overweight and obesity among adults and children. Increasing BMI has been linked with self-reporting reduced health in several ethnically diverse adult populations. A comparative overview of the SRH-related literature found that in some instances the odds of an overweight adult reporting poor health were three times greater than for adults who were not overweight (Okosun, Choi, Matamoros, & Dever, 2001; Phillips, Hammock, & Blanton, 2005; Prosper, Moczulski, & Qureshi, 2009).
Among adolescent populations, however, the science addressing the relationship between BMI and SRH is not well established. Although earlier researchers have documented a link between increasing BMI and a poor SRH status among youth (Swallen, Reither, Haas, & Meier, 2005; Vingilis, Wade, & Seeley, 2002), more recently divergent, even contradictory findings regarding the impact of BMI on SRH among young people have been identified. For example, using data collected from a representative sample of U.S. high school students, Foti and Eaton (2010) were unable to support a pattern of association between BMI and SRH. Darviri, Artemiadis, Tigani, and Alexopoulos (2011) reported similar findings with a Greek sample that included adolescent participants 15–19 years of age.
Similar to the potential influence of BMI on SRH reporting, evidence suggests that low global self-esteem may also contribute to reporting low self-ratings of health. Global self-esteem is generally defined as the way one characteristically feels about oneself (Harter, 1999, 2003). Within the general population low global self-esteem has been found to co-occur with several mental and physical health risk factors including substance abuse, depression and obesity. (DiClemente et al., 2005; Donnellan, Trzesniewski, Robins, Moffitt, & Caspi, 2005; Wang, Wild, Kipp, Kuhle, & Veugelers, 2009). In a limited number of studies, these risk vulnerabilities have, in turn, been shown to exert an effect on an individuals’ perception of both their current and future health status (Axelsson & Ejlertsson, 2002; Hasson, Arnetz, Theorell, & Anderberg, 2006). In an even smaller number of studies, consisting largely of adults, co-occurring global self-esteem and obesity have shown some function as a contributory factor to perception of wellness and scorings of SRH (Rohrer & Young, 2004). To promote a more robust understanding of the global self-esteem-SRH phenomena additional study is needed in this area with a variety of populations.
In addition to the risk that psychological variables such as lowered global self-esteem may pose to SRH, lifestyle risk behaviors such as physical inactivity have increasingly been linked with poor SRH in both domestic and international populations. It has been well documented that regular physical activity is a fundamental component to a first-class health status. Researchers have found that at similar levels of physical functioning, individuals who participated less frequently in physical activity tended to report lower SRH. Using Greek and Swedish cohorts in cross-sectional and longitudinal studies, Darviri et al., (2011) and Elinder, Sundblom, and Rosendahl (2011) reported significant associations between poor SRH and low physical activity. Lower participatory frequency in physical activity was also found to correlate with a lower perception of SRH in a sample of Spanish adults (Galan, Meseguer, Herruzo, & Rodriguez-Artalejo, 2010).
Literature that currently informs knowledge about African American adolescents’ SRH is sparse. However, an extensive body of medical research has shown that decreased physical activity has significant direct and indirect health risks among adolescents. Reciprocally, these lifestyle risk behaviors may have major implications for SRH among youth. Furthermore, national surveillance data using self-report indices of physical activity levels showed that female African American adolescents had a higher prevalence of physical inactivity than their European American counterparts (CDC, 2011; Thompson & Barksdale, 2010, Whitt-Glover et al., 2009). In the absence of targeted research, the documented relationship between physical activity and morbidity risk would support the postulation of a link between physical activity and SRH among members of this population subgroup.
Low levels of participation in lifestyle behaviors that promote spiritual well-being have also demonstrated risk potential for reporting lower ratings of health. A plethora of literature has identified spiritual involvement as a major component of health and well-being among African Americans (Carter, 2002; Dessio, Wade, Chao, Kronenberg, Cushman, & Kalmuss, 2004; Musgrave, Allen, & Allen, 2002). Spirituality is often conceptually viewed as a multidimensional construct that is both personal and intangible (Coyle, 2002; Turner-Musa & Lipscomb, 2007). Outward expressions of spirituality among African Americans are seen in activities such as prayer or meditation, attending church, espousing belief in a transcendent being, and proselytizing spiritual ideals (Newlin, Knafl, & Melkus, 2002; Oman & Thoresen, 2005). Moreover, spirituality and its expressive behaviors have been shown to influence health and well-being among adolescents (Cotton, Zebracki, Rosenthal, Tsevat, & Drotar, 2006; Dew et al., 2008; Rew & Wong, 2006). Only a few researchers, however, have examined the impact of spirituality on SRH among youth. In one such study conducted with a U.S. cohort of suburban college students, a significant association between perceived spirituality and perceived health status was found (Zullig, Ward, & Horn, 2006). Results obtained from the few studies with young people corroborate, closely, although not exactly, conclusions generated with adults, suggesting that lifestyle behaviors may vary by age. More research is needed to definitively establish whether these behaviors influence SRH status among adolescents.
In addition to the anthropometric, psychological, and lifestyle behavior variables hypothesized to influence SRH, structural variables such as household income, an indicator of socioeconomic level (SEL), may also exaggerate reporting differences in SRH (Alexopoulos & Geitona, 2009; Subramanian, Kim, & Kawachi, 2005). According to the theory of differential vulnerability, the effect of perceived health may vary by socioeconomic groups and subsequently to reduced access to materials and/or conditions that promote physical and mental prosperity (Kessler, 1979; Kessler & Cleary, 1980). It is generally acknowledged by the scientific community that individuals within the lower SEL strata often have reduced access to materials and/or conditions that promote health and well-being. In the U.S., substantial ethnic variation exists with respect to SEL stratification.
One of the most significant challenges within the African American community is poverty. Currently, the unemployment rate for African Americans is double that of European Americans (Office of Minority Health, 2011). African American children are three times more likely to live in poverty than European American children (Costello, Keeler, & Angold, 2001). Consequently, the likelihood of reporting a compromised health status increases as SEL vulnerability increases (Goodman, Huang, Schafer-Kalkhoff, & Adler, 2007; Prus, 2011). This is particularly significant for female African American adolescents, for whom, well-documented disparities in health status persist throughout their lifespan (Eaton et al., 2010; Mayer-Davis et al., 2009; Ogden & Carroll, 2010).
Despite the ubiquitous application of SRH as a useful epidemiological measure, research supporting the relationships among anthropometric, psychological, lifestyle behavioral, and structural variables with SRH has been mostly limited to international nonclinical populations of adults. As such, findings from these studies may not generalize well to other age groups such as adolescents. The conceptualization of SRH is likely established during the early and late adolescent school years (Fosse & Haas, 2009; Wade & Vingilis, 1999). Therefore, one might expect that environmental variation, common during this period of growth and maturation, could influence how adolescents perceive their overall health status. Unfortunately, empirical data regarding the determinants of SRH with this age group are rare, with the vast majority of the existing adolescent literature devoted to predictors of SRH among international youth.
In addition to the paucity of relevant data, another important area of concern in adolescent health research on this topic is the underrepresentation of individuals from ethnically and culturally diverse backgrounds. Given the potential importance of SRH as a predictor of future morbidity and mortality, as an indicator for improving health outcomes, and as a measure of overall population health, sufficient information on factors that influence SRH across ethnicity, gender and age groups is needed.
The purpose of the current investigation was to evaluate several selected anthropometric, psychological, lifestyle behavioral, and structural variables of SRH with a sample of urban-dwelling self-identified female African American adolescents. It was hypothesized that high BMI, low global self-esteem competence, lower frequencies of physical activity, and less frequent participation in activities that promote spiritual well-being would demonstrate significant predictive capacities for poor SRH.
Method
Participants and Procedure
Cross-sectional sub-analyses were performed using data obtained as part of a larger descriptive study of weight status and health promoting behaviors among female African American adolescents from the New Orleans, Louisiana metropolitan statistical area (MSA). Using a combination of probability/non-probability sampling strategy a convenience sample of N = 310 healthy self-identified African American females between 14 and 18 years of age were recruited to participate in the study. Data collection occurred from June, 2005 through June, 2006. Using a government supported municipal list-serve of secondary institutions, pre- Hurricane Katrina sampling included the random selection of public high schools located within the two largest MSA parishes (Orleans and Jefferson). Prospective participants were recruited from these schools using traditional advertising techniques (e.g., flyers). Post Hurricane Katrina, the remaining sample were non-randomly recruited using shelter and school enrollment directories for three parishes (East-West Baton Rouge and Rapides). Due to their proximity to New Orleans, these parishes housed significant numbers of relocated MSA residents. Approximately 90% of the sample was enrolled and data collected prior to Hurricane Katrina. Inclusion and exclusion criteria are reported in detail elsewhere (Powell-Young, 2012). Briefly, teens were included if they could read and speak English, were enrolled in public high school, between the ages of 14 through 18 years, and self-identified as African American. Exclusion criteria included reported conditions or medication use with the potential to affect body weight or physical activity level. This included pregnancy within the past 6 months and/or current breastfeeding. On the day of testing, a standardized introduction to the study was presented. Demographic and study questionnaires were administered by trained research assistants. Subsequently, weight and height were measured with minimum clothing in stocking feet. All data collection activities were conducted in areas suitable for testing and measurement. Participants were compensated for their time according to approved procedures.
Human Subjects Protection
Before protocol implementation, written approvals to conduct the study and recruit volunteers were obtained from the relevant university institutional review board (IRB) and appropriate school administrators. Written informed consent was obtained from participants ≥ 18 years of age and from a parent or guardian of those < 18 years old. Written assent was also obtained from minor participants prior to study inclusion. Participants were compensated for their participation according to the IRB protocol.
Description of Variables and Measures
SRH
The main outcome variable for this study was SRH status captured using a single-item measure based on the CDC Behavioral Risk Factor Surveillance System (BRFSS) scale. The question asked, “How would you rate your current overall health status?” The possible response options were: excellent, good, and poor. Data have demonstrated support for the utility and reliability of single-item measures to characterize current perception of SRH among multi-ethnic groups of adolescents (Boardman, 2006; Haddock et al., 2006).
BMI
Anthropometric measures (height and weight) were assessed following standardized procedures. Height was measured to the nearest one-half inch using a portable stadiometer (Seca, Hanover, MD). Weight was measured to the nearest one-half pound using a professional dial floor scale (Health-O-Meter, Bedford Heights, OH). After appropriate conversions, BMI was calculated (BMI = weight [kg]/height [m2]). Using recommended nomenclature (Krebs et al., 2007) and 2000 CDC growth chart reference standards and percentiles (CDC, 2009), subjects were categorized as non-overweight (N-OW), ≥ 5th percentile but < 85th percentile or overweight (OW), ≥ 85th percentile.
Global self esteem
Harter’s Self-Perception Profile for Adolescents (SPPA, Harter, 1988) was used to evaluate the domain of global self-esteem with five items. The SPPA is among the most widely used self-report multi-domain measures of self-concept among youth in research settings. Items are answered on a 4-point Likert-type response scale ranging from strongly agree to strongly disagree. Domain scoring is based on derived means with values correlating from low to high with the amount of perceived self-esteem competence. Based on referenced norms of the original sample, and with each question scored on a 1–4 continuum, scores that fall between the subscale midpoint (i.e., 2.5) ± the sample standard deviation (i.e., 0.48) denote an average level of global self-esteem. Scores of 1 through 1.9 indicate below average esteem, 2 through 2.9 suggest average global esteem, and 3 through 4 reflect above average self-esteem. Normative data on the reliability and validity of the SPPA with non-clinical samples is available in the users’ manual (Harter, 1988). Cronbach’s alpha (α) reliability estimates reported for the global self-esteem domain from several diverse non-clinical samples range from .68 to .85 (Powell-Young & Spruill, In Press; Rose, Hands, & Larkin, 2011; Rudasill & Callahan, 2008). The α estimate for this sample was .67. Michaels, Barr, Roosa, and Knight (2007) suggested that measures of global self-esteem are not strong in reliability for African American adolescents. This phenomenon has been partially attributed to the Eurocentric model often guiding the development and construction of self-esteem measures. Notwithstanding the former issue, comparative evaluations of internal consistency results with African American adolescents have been essentially equal across studies and ranged from .68 through .72 for the global self-esteem subscale (Thomson & Zand, 2002). Moreover, the data indicated measurement equivalence for this concept across ethnically diverse groups.
Physical activity
The variable was measured with the Adolescent Lifestyle Profile-R2 (ALP-R2; Hendricks, Pender, Murdaugh, Tavakoli, & Hendricks, 2001). The ALP-R2 is a 44-item multidimensional instrument designed to provide participation frequency estimates for seven health promoting behaviors. The subscale, Physical Activity, has 6 items. Response options are numeric values (1 = never, 2 = sometimes, 3 = often, 4 = always). Interpretation of the physical activity score is based on the calculated average of subscale items. For example, the greater the score, the higher the respondents’ level of physical activity and vice versa. The ALP-R2 subscales have been validated with normative samples that included healthy African American adolescents (Hendricks et al., 2001; Hendricks, Murdaugh, & Pender, 2006). Reliability estimates with the validation cohorts was .77 for physical activity. The α coefficient for this sample was .73. There are no discrete cut-off points to differentiate active from sedentary participants with this measure. Estimations of percentiles (P) were calculated to categorize activity levels for this sample as follows: sedentary (≤ 10th P; score: ≤ 1.8); moderately active (> 10th P but < 90th P, score: 1.9–3.4), and active (≥ 90th P, score: 3.5–4.0).
Spiritual health
The ALP-R2 (Hendricks et al., 2001) Spiritual Health 6-item subscale was used for this measure. The subscale was developed to measure how often adolescents participated in activities hypothesized to promote spirituality. The subscale was comprised of items that related to the intrinsic and extrinsic domains of spirituality. Scoring and interpretation were based on the same metric as the Physical Activity subscale. Frequency estimations for participation in spiritual health promoting behaviors were defined by the 10th and 90th percentile as: infrequent (≤ 10th P; score: ≤ 2.0); moderately frequent (> 10th P but < 90th P, score: 2.0–3.6) and frequent participation (≥ 90th P, score: 3.7–4.0). Validation studies of the ALP-R2 and its subscales have included African American youth from 11 through 22 years of age (Hendricks et al., 2001, 2006). The average reliability estimate for the norm cohorts was .82. The α estimate for this study cohort was .74.
Household income
Enrollment in the national school lunch program served as a proxy measurement for household income and thus socioeconomic level (SEL). Eligibility for participation in the program is determined by a family income below 130% of the poverty guidelines issued by The U.S. Department of Health and Human Services (Lindsey, 2009). These guidelines are based on the poverty thresholds determined annually by the U.S. Census Bureau, which are rounded and adjusted for family size. SEL was categorized as either low (L-SEL, ≤ 130% poverty) or not low (NL-SEL). Eligibility data from the national school lunch program are widely used indicators of socioeconomic status.
Statistical Analysis
Data analyses were performed using the Statistical Package for the Social Sciences (SPSS). Prior to analyses, all variables were assessed for accuracy, completion, and credible values. Frequencies, central tendency measures, and measures of variability were used to generate descriptive summarization of the study variables. Chi square (X2) analyses were conducted to determine the associations between SRH status and each of the predictor variables. Fisher’s exact test was used when expected frequencies were below 1 in any cell or < 5 in more than 20% of the cells. Power calculation (Faul, Erdfelder, Buchner, & Lang, 2009; Faul, Erdfelder, Lang, & Buchner, 2007) determined that 220 participants were needed to achieve power of .95 with a medium effect size (w=.30). Variables were further analyzed using ordinal logistic regression analyses to identify predictors of poor SRH. Models for each predictor were run separately with each effect adjusted for age. All main effects and interactions to be estimated had at least 20 cases in the sample data to produce stable estimates. Adjusted odds ratio (OR) and 95% confidence interval (95% CI) were estimated. Significance was set at an alpha level of .05 for tests, and by upper and lower 95% CI not containing the value of 1.0 for odds ratios. Referent groups for calculating OR were: N-OW, average self-esteem competence, active physical activity level, frequent participation in spiritual health activities, and NL-SEL.
Results
Sample Characteristics
A significant proportion (78%) of the participants resided in L-SEL homes. Data from this sample describe urban youth from low socioeconomic households with a Mage of 15.8 ± 1.2 years and MBMI of 25.5 ± 4.9 kg/m2. Overweight prevalence for this group was slightly higher than the national average for non-Hispanic Black females (Flegal et al., 2010; Ogden et al., 2010). Most considered themselves to be in either excellent or good health. More than three-quarters of the sample participants reported above average levels of self-esteem competence, Mscore = 3.5, which is not unusual finding among African American females (Robins, Trzesniewski, Tracy, Gosling, & Potter, 2002; Twenge & Crocker, 2002). Interestingly, none of the participants in this study reported scores that were consistent with below average levels of competence. Contrary to the general consensus regarding low frequencies of physical activity among ancestrally diverse populations in urban America, only a small proportion of the sample was inactive. Not unexpectedly, a significant fraction of the study participants were frequently involved in activities that promote spiritual well-being. Major study variables for this sample are characterized in Table 1.
Table 1.
Sample demographics (N = 310)
| Characteristic | Frequency (%) |
|---|---|
| Socioeconomic Level (SEL) | |
| Not low SEL | 68 (22) |
| Low SEL | 242 (78) |
| Body Mass Index | |
| Non-Overweight | 200 (65) |
| Overweight | 110 (36) |
| Self-Esteem Competence | |
| Average | 46 (15) |
| Above Average | 264 (85) |
| Physical Activity Level | |
| Sedentary | 54 (17) |
| Moderately Active | 153 (49) |
| Active | 103 (33) |
| Participation in Activities that Promote Spiritual Well-Being | |
| Infrequent | 57 (18) |
| Moderately Frequent | 190 (61) |
| Frequent | 63 (20) |
| Sample demographics (N = 310) | |
| Self-Rated Health Status | |
| Poor | 20 (6) |
| Good | 211 (68) |
| Excellent | 79 (26) |
Note: As a result of rounding percentages may not total 100.
Determinants of subjective health
No significant correlations were found between SRH and BMI (p = .23), global self-esteem (p = .17), or physical activity (p = .10). In contrast, however, frequency of participation in spiritual health activities and SEL demonstrated significant associations with SRH among this cohort. Results from logistic regression models expand the association findings. The adjusted odds of self-reporting poor health were 2.5 times as large (95% CI: 1.17, 5.31) among individuals who infrequently participated in spiritual health activities and 2.9 times as large (95% CI: 1.63, 5.33) for those who moderately engaged in spiritual activities as compared to those who frequently participate in spiritual activities. These data also suggest that the odds of adolescent African American females from L-SEL households reporting poor health were almost twice as large (OR: 1.8; 95% CI: 1.03, 3.14) as the odds of a teen residing in a NL-SEL household reporting poorer health (Figure 1).
Figure 1.
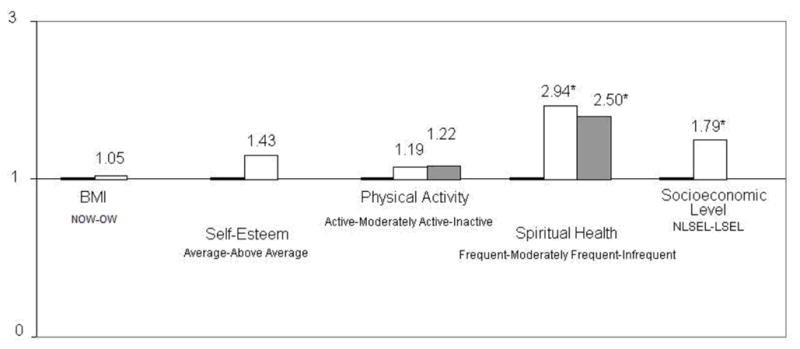
Odds ratio of reporting poor health by predictor variables among female African American adolescents. Referents are healthy weight (HW), average self-esteem, active physical activity estimate, frequent spiritual behaviors, and NLSEL. (*) 95% confidence intervals do not include 1.
As a result of the collection and inclusion of post-Katrina data into the current statistical profile, additional analyses were performed in order to refine and augment the results. The findings indicate that associations between SRH and the predictor variables for the current sample with (n = 310) and without (n = 284) post-Katrina data were not significantly different (Table 2). Moreover, the logistic regression was rerun excluding the post-Katrina participants with no substantial changes in the model.
Table 2.
Summary of chi square results comparing pre- and post-Katrina data sets
| Variable | n | X2 | P |
|---|---|---|---|
| Body mass index | 310 | 2.9 | .23 |
| 284 | 1.8 | .39 | |
| Global self-esteem | 310 | 3.6 | .17 |
| 284 | 3.5 | .17 | |
| Physical activity | 310 | 7.7 | .10 |
| 284 | 8.5 | .07 | |
| Spiritual health | 310 | 18.7 | <.01 |
| 284 | 18.5 | <.01 | |
| Socioeconomic level | 310 | 51.7 | <.01 |
| 284 | 56.9 | <.01 |
Note: Pre-Katrina data set (N = 284) consists of data collected from participants prior to Hurricane Katrina. Post-Katrina data set (N = 310) consists of data collected from all study participants, both pre- and post-Hurricane Katrina.
Discussion
I found that the odds of reporting poor health did not differ significantly by BMI, global self-esteem, or physical activity level among female African American teens. The major predictors of poor subjective health were household income and spiritual well-being. My data indicate that the odds of reporting poor health increased substantially among individuals from L-SEL homes and for those who participated less frequently in lifestyle activities that contribute positively to spiritual well-being.
Most researchers suggest that higher BMI functions as a significant determinant for poor subjective health among adolescents (Galan et al., 2010; Tremblay, Dahinten, & Kohen, 2003; Vingilis et al., 2002). Yet, the results generated with my sample differ from previously published findings. One explanation for the differing observations may be the effect of culture on the identification and internalization of what constitutes a viable health threat for this segment of the population. Consequently, factors demonstrating predictive power for poor health among non-African populations, from which the vast majority of prior research findings are generated, may not be applicable with African Americans. For example, African American males and females, regardless of age, tend to hold a less negative attitude toward a more abundant female body size (Freedman, Carter, Sbrocco, & Gray, 2004; Gluck & Geliebter, 2002; Thomas, Moseley, Stallings, Nichols-English, & Wagner, 2008). In fact, African American adolescents as young as 10.5 years of age have demonstrated preferences for a larger ideal female figure (Cohn et al., 1987; Jones, Fries, & Danish, 2007). At the community level, this dynamic of acceptance and partiality may lessen the negative health implications associated with high BMI. The result, as shown in my group, is that overweight does not manifest as an independent, viable health risk.
Research results regarding the relationship between physical activity frequency and poor SRH have been inconsistent (Biddle & Asare, 2011; Galan et al., 2010; Tremblay et al., 2003). Although some researchers have found significant associations between physical activity regularity and SRH status, results from other researchers suggested no physical activity frequency effect on SRH. My research has shown that although physical activity was not a significant predictor of poor health, less frequent participation in leisure time physical activity slightly increased the odds of reporting a less than optimal health status. Although a heightened sense of global self-esteem is generally thought to be important to sense of well-being, this is often thought to be more relevant to mental health (Rosenberg, Schooler, Schoenbach, & Rosenberg, 1995). There is very little information regarding the predictive capacity of global self-esteem on general well-being. My study provides novel evidence on the effect of global self-esteem on perceived health status for urban-dwelling African American youth.
Socioeconomic inequality had an obvious and measureable effect on perceived health status among individuals in this sample. I compared my data with recent meta-analyses and found similar results. Kondo and colleagues (2009) reported that the odds of poor SRH were significantly larger (OR = 1.04) for adolescents from less affluent backgrounds. Richter and others (2009) also reported an increased risk (OR = 1.80) for poor SRH among adolescent females from low socioeconomic households. My data provide support for the theory of poverty and lower-class susceptibility for compromised health and health outcomes previously described by others (Ram, 2005).
Historically, spirituality in African American culture has been an essential aspect of holistic health. However, empirical literature that focuses on adolescent spirituality is sparse. Even less abundant is information on the influence of spiritual well-being on adolescent perceived health. Nevertheless, there is some evidence, generated from mostly adult populations, supporting the protective influences of engaging in activities that promote spirituality on health, health practices and health outcomes among this segment of the population (Chester, Himburg, & Weatherspoon, 2006; Figueroa, Davis, Baker, & Bunch, 2006; Underwood & Powell, 2006). From my data, it appears that spiritual well-being is the most salient attributable risk factor for poor subjective health. These findings imply that evaluation of and consideration for spiritual health may provide the greatest benefit when informing prevention and intervention strategies to improve health.
Limitations
This was a non-random, homogeneous sample with respect to ancestry, geography and socioeconomic status. Therefore, generalizability beyond this sample is unknown. Due to the cross-sectional nature of the data, causality and age effect of the relationship found between SEL and spiritual health with poor SRH cannot be definitively established. Misreporting bias may diminish the reliability of enrollment in the national school lunch program as a parent-proxy index for household SEL. However, because of the concentrated poverty level in New Orleans among African Americans, I do not believe that use of this measure would compromise the results generated with this study cohort. With respect to internal validity and Hurricane Katrina data, it would not be unexpected to intuit a negative impact on mental health and/or health status. However, because (a) the greater part of the data (90%) was collected prior to the disaster; (b) the income level for this target population did not noticeably change post-Katrina; (c) the greater proportion of the pre- and post-Katrina data indicate satisfactory levels of global self-esteem and well-being; and (d) no significant difference in the results when data are separated and compared, the impact of the disaster on the outcomes of this study’s results are negligible.
These limitations notwithstanding, results from this study contribute to advancing the body of subjective health research with vulnerable populations. At present, knowledge about the effects of demographic and psychosocial variables among African American adolescents is limited. Information is especially sparse for urban-dwelling adolescent African American females residing in low income households. Future researchers should aim to recruit larger, more representative samples of African Americans of both genders. Further studies are needed to investigate possible reasons for the variability in findings among African Americans adolescents.
Conclusions
To my knowledge, this is one of the first studies to evaluate the predictive capacity of several diverse determinants among a subsample of the population that is disparately affected by the health burdens. Although more research is needed, results from this study have important implications for health care. Overall, the novel findings provide clearly needed insight regarding population-specific referent and attributable risk empirics for African American youth. In addition, understanding the social and cultural context of health and illness can inform the development and implementation of prevention and intervention strategies that address health disparities.
Acknowledgments
The authors would like to thank the parents and youth for volunteering their participation.
The development of this work was supported in part by grants from the National Institute on Minority Health and Health Disparities (P20 MD00481701) and the National Institute for Nursing Research (T32 NR007110).
Thanks to Dr. Cruz Valesco-Gonzalez for statistical support.
References
- Alexopoulos EC, Geitona M. Self-rated health: Inequalities and potential determinants. International Journal of Environmental Research and Public Health. 2009;6:2456–2469. doi: 10.3390/ijerph6092456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Axelsson L, Ejlertsson G. Self-reported health, self-esteem and social support among young unemployed people: A population based study. International Journal of Social Welfare. 2002;11:111–119. doi: 10.1111/1468-2397.00205. [DOI] [Google Scholar]
- Biddle SJ, Asare M. Physical activity and mental health in children and adolescents: A review of reviews. British Journal of Sports Medicine. 2011;45:886–895. doi: 10.1136/bjsports-2011-090185. [DOI] [PubMed] [Google Scholar]
- Boardman JD. Self-rated health among U.S. adolescents. The Journal of Adolescent Health. 2006;38:401–408. doi: 10.1016/j.jadohealth.2005.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter JH. Religion/spirituality in African American culture: An essential aspect of psychiatric care. Journal of the National Medical Association. 2002;109:1184–1193. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. About BMI for children and teens. 2009 Retrieved 10/15, 2010, from http://www.cdc.gov/healthyweight/assessing/bmi/children_bmi/about_children_bmi.html.
- Centers for Disease Control and Prevention. Physical activity levels of high school students --- United States, 2010. MMWR Morbidity and Mortality Weekly Report. 2011;60:773–777. [PubMed] [Google Scholar]
- Chester DN, Himburg SP, Weatherspoon LJ. Spirituality of African-American women: Correlations to health-promoting behaviors. Journal of National Black Nurses’ Association. 2006;17(1):1–8. [PubMed] [Google Scholar]
- Cohn LD, Adler NE, Irwin CE, Jr, Millstein SG, Kegeles SM, Stone G. Body-figure preferences in male and female adolescents. Journal of Abnormal Psychology. 1987;96:276–279. doi: 10.1037//0021-843x.96.3.276. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Keeler GP, Angold A. Poverty, race/ethnicity, and psychiatric disorder: A study of rural children. American Journal of Public Health. 2001;91:1494–1498. doi: 10.2105/ajph.91.9.1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotton S, Zebracki K, Rosenthal SL, Tsevat J, Drotar D. Religion/spirituality and adolescent health outcomes: A review. The Journal of Adolescent Health. 2006;38:472–480. doi: 10.1016/j.jadohealth.2005.10.005. [DOI] [PubMed] [Google Scholar]
- Coyle J. Spirituality and health: Towards a framework for exploring the relationship between spirituality and health. Journal of Advanced Nursing. 2002;37:589–597. doi: 10.1046/j.1365-2648.2002.02133.x. [DOI] [PubMed] [Google Scholar]
- Darviri C, Artemiadis AK, Tigani X, Alexopoulos EC. Lifestyle and self-rated health: A cross-sectional study of 3,601 citizens of Athens, Greece. BMC Public Health. 2011;11:619. doi: 10.1186/1471-2458-11-619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bruin A, Picavet HS, Nossikov A. Health interview surveys. towards international harmonization of methods and instruments. WHO Regional Publications. European Series. 1996;58:i–xiii. 1–161. [PubMed] [Google Scholar]
- DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. A meta-analysis. Journal of General Internal Medicine. 2006;21:267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dessio W, Wade C, Chao M, Kronenberg F, Cushman LE, Kalmuss D. Religion, spirituality, and healthcare choices of African-American women: Results of a national survey. Ethnicity & Disease. 2004;14:189–197. [PubMed] [Google Scholar]
- Dew RE, Daniel SS, Armstrong TD, Goldston DB, Triplett MF, Koenig HG. Religion/Spirituality and adolescent psychiatric symptoms: A review. Child Psychiatry and Human Development. 2008;39:381–398. doi: 10.1007/s10578-007-0093-2. [DOI] [PubMed] [Google Scholar]
- DiClemente RJ, Wingood GM, Lang DL, Crosby RA, Salazar LF, Harrington K, Hertzberg VS. Adverse health consequences that co-occur with depression: A longitudinal study of Black adolescent females. Pediatrics. 2005;116:78–81. doi: 10.1542/peds.2004-1537. [DOI] [PubMed] [Google Scholar]
- Donnellan MB, Trzesniewski KH, Robins RW, Moffitt TE, Caspi A. Low self-esteem is related to aggression, antisocial behavior, and delinquency. Psychological Science. 2005;16:328–335. doi: 10.1111/j.0956-7976.2005.01535.x. [DOI] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J Centers for Disease Control and Prevention. Youth risk behavior surveillance - United States, 2009. MMWR. Surveillance Summaries : Morbidity and Mortality Weekly Report Surveillance Summaries / CDC. 2010;59:1–142. [PubMed] [Google Scholar]
- Elinder LS, Sundblom ES, Rosendahl KI. Low physical activity is a predictor of thinness and low self-rated health: Gender differences in a Swedish cohort. The Journal of Adolescent Health. 2011;48:481–486. doi: 10.1016/j.jadohealth.2010.08.005. [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods. 2009;41:1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Figueroa LR, Davis B, Baker S, Bunch JB. The influence of spirituality on health care-seeking behaviors among African Americans. ABNF Journal. 2006;17:82–88. [PubMed] [Google Scholar]
- Flegal KM, Ogden CL, Yanovski JA, Freedman DS, Shepherd JA, Graubard BI, Borrud LG. High adiposity and high body mass index-for-age in US children and adolescents overall and by race-ethnic group. The American Journal of Clinical Nutrition. 2010;91:1020–1026. doi: 10.3945/ajcn.2009.28589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fosse NE, Haas SA. Validity and stability of self-reported health among adolescents in a longitudinal, nationally representative survey. Pediatrics. 2009;123:e496–501. doi: 10.1542/peds.2008-1552. [DOI] [PubMed] [Google Scholar]
- Foti K, Eaton D. Associations of selected health risk behaviors with self-rated health status among U.S. high school students. Public Health Reports. 2010;125:771–781. doi: 10.1177/003335491012500522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman RE, Carter MM, Sbrocco T, Gray JJ. Ethnic differences in preferences for female weight and waist-to-hip ratio: A comparison of African-American and White American college and community samples. Eating Behaviors. 2004;5:191–198. doi: 10.1016/j.eatbeh.2004.01.002. [DOI] [PubMed] [Google Scholar]
- Galan I, Meseguer CM, Herruzo R, Rodriguez-Artalejo F. Self-rated health according to amount, intensity and duration of leisure time physical activity. Preventive Medicine. 2010;51:378–383. doi: 10.1016/j.ypmed.2010.09.001. [DOI] [PubMed] [Google Scholar]
- Gander J, Lee DC, Sui X, Hebert JR, Hooker SP, Blair SN. Self-rated health status and cardiorespiratory fitness as predictors of mortality in men. British Journal of Sports Medicine. 2011;45:1095–1100. doi: 10.1136/bjsm.2010.079855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gluck ME, Geliebter A. Racial/ethnic differences in body image and eating behaviors. Eating Behaviors. 2002;3:143–151. doi: 10.1016/s1471-0153(01)00052-6. [DOI] [PubMed] [Google Scholar]
- Goodman E, Huang B, Schafer-Kalkhoff T, Adler NE. Perceived socioeconomic status: A new type of identity that influences adolescents’ self-rated health. The Journal of Adolescent Health. 2007;41:479–487. doi: 10.1016/j.jadohealth.2007.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddock CK, Poston WS, Pyle SA, Klesges RC, Vander Weg MW, Peterson A, Debon M. The validity of self-rated health as a measure of health status among young military personnel: Evidence from a cross-sectional survey. Health and Quality of Life Outcomes. 2006;4:57. doi: 10.1186/1477-7525-4-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harter S. Manual for the Self-Perception Profile for Adolescents. Denver, CO: Department of Psychology, University of Denver; 1988. [Google Scholar]
- Harter S. The construction of self: A developmental perspective. New York NY: Gilford Press; 1999. [Google Scholar]
- Harter S. The development of self-representations during childhood and adolescence. In: Leary M, Tangney J, editors. Handbook of self and identity. New York, NY: Guilford Press; 2003. pp. 610–642. [Google Scholar]
- Hasson D, Arnetz BB, Theorell T, Anderberg UM. Predictors of self-rated health: A 12-month prospective study of IT and media workers. Population Health Metrics. 2006;4:8. doi: 10.1186/1478-7954-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendricks C, Murdaugh C, Pender N. The adolescent lifestyle profile: Development and psychometric characteristics. Journal of National Black Nurses’ Association. 2006;17(2):1–5. [PubMed] [Google Scholar]
- Hendricks CS, Pender N, Murdaugh C, Tavakoli A, Hendricks D. Developing an adolescent measure of health promoting lifestyles. 2001. Unpublished manuscript. [Google Scholar]
- Hennessy CH, Moriarty DG, Zack MM, Scherr PA, Brackbill R. Measuring health-related quality of life for public health surveillance. Public Health Reports. 1994;109:665–672. [PMC free article] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Institute of Medicine. State of the USA health indicators: Letter report. Washington, D.C: The National Academic Press; 2009. [Google Scholar]
- Jones LR, Fries E, Danish SJ. Gender and ethnic differences in body image and opposite sex figure preferences of rural adolescents. Body Image. 2007;4:103–108. doi: 10.1016/j.bodyim.2006.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC. A strategy for studying differential vulnerability to the psychological consequences of stress. Journal of Health and Social Behavior. 1979;20:100–108. [PubMed] [Google Scholar]
- Kessler RC, Cleary PD. Social class and psychological distress. American Sociological Review. 1980;45:463–478. [PubMed] [Google Scholar]
- Kondo N, Sembajwe G, Kawachi I, van Dam RM, Subramanian SV, Yamagata Z. Income inequality, mortality, and self rated health: Meta-analysis of multilevel studies. BMJ. 2009;339:b4471. doi: 10.1136/bmj.b4471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramers PG. The ECHI project: Health indicators for the European community. European Journal of Public Health. 2003;13(3 Suppl):101–106. doi: 10.1093/eurpub/13.suppl_1.101. [DOI] [PubMed] [Google Scholar]
- Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007;120(4 Suppl):S193–S228. doi: 10.1542/peds.2007-2329D. [DOI] [PubMed] [Google Scholar]
- Liao Y, Bang D, Cosgrove S, Dulin R, Harris Z, Taylor A Centers for Disease Control and Prevention. Surveillance of health status in minority communities - racial and ethnic approaches to community health across the U.S. (REACH U.S.) risk factor survey, United States, 2009. MMWR Surveillance Summaries : Morbidity and Mortality Weekly Report Surveillance Summaries / CDC. 2011;60:1–44. [PubMed] [Google Scholar]
- Lindsey D. Childhood poverty and inequality. New York, NY: Oxford University Press; 2009. [Google Scholar]
- Mayer-Davis EJ, Beyer J, Bell RA, Dabelea D, D’Agostino R, Jr, Imperatore G SEARCH for Diabetes in Youth Study Group. Diabetes in African American youth: Prevalence, incidence, and clinical characteristics: The SEARCH for diabetes in youth study. Diabetes Care. 2009;32(2 Suppl):S112–S122. doi: 10.2337/dc09-S203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaels ML, Barr A, Roosa MW, Knight GP. Self-esteem: Assessing measurement equivalence in a multiethnic sample of youth. Journal of Early Adolescence. 2007;27:269–295. [Google Scholar]
- Musgrave CF, Allen CE, Allen GJ. Spirituality and health for women of color. American Journal of Public Health. 2002;92:557–560. doi: 10.2105/ajph.92.4.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakata A, Takahashi M, Otsuka Y, Swanson NG. Is self-rated health associated with blood immune markers in healthy individuals? International Journal of Behavioral Medicine. 2010;17:234–242. doi: 10.1007/s12529-010-9102-0. [DOI] [PubMed] [Google Scholar]
- Newlin K, Knafl K, Melkus GD. African-American spirituality: A concept analysis. ANS Advances in Nursing Science. 2002;25:57–70. doi: 10.1097/00012272-200212000-00005. [DOI] [PubMed] [Google Scholar]
- Office of Minority Health. Data statistics: African American profile. 2011 Retrieved 01/05, 2012, from http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlid=51.
- Ogden CL, Carroll MD. Prevalence of obesity among children and adolescents: United States, trends, 1963–1965 through 2007–2008. 2010 Retrieved 11/28, 2010, from http://www.cdc.gov/nchs/data/hestat/obesity_child_07_08/obesity_child_07_08.htm.
- Okosun IS, Choi S, Matamoros T, Dever GE. Obesity is associated with reduced self-rated general health status: Evidence from a representative sample of White, Black, and Hispanic Americans. Preventive Medicine. 2001;32:429–436. doi: 10.1006/pmed.2001.0840. [DOI] [PubMed] [Google Scholar]
- Oman D, Thoresen CE. Do religion and spirituality influence health? In: Paloutzian RF, Park CL, editors. Handbook of the psychology of religion and spirituality. New York, NY: Guilford Press; 2005. pp. 435–459. [Google Scholar]
- Phillips LJ, Hammock RL, Blanton JM. Predictors of self-rated health status among Texas residents. Preventing Chronic Disease. 2005;2 Retrieved 06/14, 2011, from http://www.cdc.gov/pcd/issues/2005/oct/04_0147.htm. [PMC free article] [PubMed] [Google Scholar]
- Powell-Young YM. The validity of self-report weight and height as a surrogate method for direct measurement. Applied Nursing Research. 2012;25:25–30. doi: 10.1016/j.apnr.2010.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell-Young YM, Spruill IJ. Measuring self-concept among African Americans: Validating the factor structure of the self-perception profile for adolescents. Journal of the National Black Nurses Association. In Press. [PubMed] [Google Scholar]
- Prosper MH, Moczulski VL, Qureshi A. Obesity as a predictor of self-rated health. American Journal of Health Behavior. 2009;33:319–329. doi: 10.5993/ajhb.33.3.10. [DOI] [PubMed] [Google Scholar]
- Prus SG. Comparing social determinants of self-rated health across the United States and Canada. Social Science & Medicine. 2011;73:50–59. doi: 10.1016/j.socscimed.2011.04.010. [DOI] [PubMed] [Google Scholar]
- Ram R. Income inequality, poverty, and population health: Evidence from recent data for the United States. Social Science & Medicine. 2005;61:2568–2576. doi: 10.1016/j.socscimed.2005.04.038. [DOI] [PubMed] [Google Scholar]
- Rew L, Wong YJ. A systematic review of associations among religiosity/spirituality and adolescent health attitudes and behaviors. The Journal of Adolescent Health. 2006;38:433–442. doi: 10.1016/j.jadohealth.2005.02.004. [DOI] [PubMed] [Google Scholar]
- Richter M, Erhart M, Vereecken CA, Zambon A, Boyce W, Nic Gabhainn S. The role of behavioural factors in explaining socio-economic differences in adolescent health: A multilevel study in 33 countries. Social Science & Medicine. 2009;69:396–403. doi: 10.1016/j.socscimed.2009.05.023. [DOI] [PubMed] [Google Scholar]
- Robins RW, Trzesniewski KH, Tracy JL, Gosling SD, Potter J. Global self-esteem across the life span. Psychology and Aging. 2002;17:423–434. [PubMed] [Google Scholar]
- Rohrer JE, Young R. Self-esteem, stress and self-rated health in family planning clinic patients. BMC Family Practice. 2004;5:11. doi: 10.1186/1471-2296-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose E, Hands B, Larkin D. Reliability and validity of the self-perception profile for adolescents: An Australian sample. Australian Journal of Psychology. 2011 doi: 10.1111/j.1742-9536.2011.00031.x. Advance online publication. [DOI] [Google Scholar]
- Rosenberg M, Schooler C, Schoenbach C, Rosenberg F. Global self-esteem and specific self-esteem: Different concepts, different outcomes. American Sociological Review. 1995;60:141–156. [Google Scholar]
- Rudasill KM, Callahan CM. Psychometric characteristics of the Harter Self-Perception Profiles for Adolescents and Children for use with gifted populations. Gifted Child Quarterly. 2008;52:70–86. [Google Scholar]
- Subramanian SV, Kim D, Kawachi I. Covariation in the socioeconomic determinants of self rated health and happiness: A multivariate multilevel analysis of individuals and communities in the USA. Journal of Epidemiology and Community Health. 2005;59:664–669. doi: 10.1136/jech.2004.025742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swallen KC, Reither EN, Haas SA, Meier AM. Overweight, obesity, and health-related quality of life among adolescents: The national longitudinal study of adolescent health. Pediatrics. 2005;115:340–347. doi: 10.1542/peds.2004-0678. [DOI] [PubMed] [Google Scholar]
- Thomas AM, Moseley G, Stallings R, Nichols-English G, Wagner PJ. Perceptions of obesity: Black and White differences. Journal of Cultural Diversity. 2008;15:174–180. [PubMed] [Google Scholar]
- Thompson WM, Barksdale DJ. Physical inactivity in female African-American adolescents: Consequences, costs, & care. Journal of National Black Nurses’ Association. 2010;21(1):39–45. [PubMed] [Google Scholar]
- Thomson NR, Zand DH. The Harter Self-Perception Profile for Adolescents: Psychometrics for an early adolescent, African American sample. International Journal of Testing. 2002;2:297–310. [Google Scholar]
- Tomten SE, Hostmark AT. Self-rated health showed a consistent association with serum HDL-cholesterol in the cross-sectional Oslo health study. International Journal of Medical Sciences. 2007;4:278–287. doi: 10.7150/ijms.4.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremblay S, Dahinten S, Kohen D. Factors related to adolescents’ self-perceived health. Health Reports. 2003;14 (Suppl):7–16. [PubMed] [Google Scholar]
- Turner-Musa J, Lipscomb L. Spirituality and social support on health behaviors of African American undergraduates. American Journal of Health Behavior. 2007;31:495–501. doi: 10.5555/ajhb.2007.31.5.495. [DOI] [PubMed] [Google Scholar]
- Twenge JM, Crocker J. Race and self-esteem: Meta-analyses comparing Whites, Blacks, Hispanics, Asians, and American Indians and comment on Gray-Little and Hafdahl (2000) Psychological Bulletin. 2002;128:371–408. doi: 10.1037/0033-2909.128.3.371. discussion 409–20. [DOI] [PubMed] [Google Scholar]
- Underwood SM, Powell RL. Religion and spirituality: Influence on health/risk behavior and cancer screening behavior of African Americans. ABNF Journal. 2006;17(1):20–31. [PubMed] [Google Scholar]
- Vingilis ER, Wade TJ, Seeley JS. Predictors of adolescent self-rated health. analysis of the national population health survey. Canadian Journal of Public Health. 2002;93:193–197. doi: 10.1007/BF03404999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade TJ, Vingilis E. The development of self-rated health during adolescence: An exploration of inter- and intra-cohort effects. Canadian Journal of Public Health. 1999;90:90–94. doi: 10.1007/BF03404108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F, Wild TC, Kipp W, Kuhle S, Veugelers PJ. The influence of childhood obesity on the development of self-esteem. Health Reports. 2009;20(2):21–27. [PubMed] [Google Scholar]
- Whitt-Glover MC, Taylor WC, Floyd MF, Yore MM, Yancey AK, Matthews CE. Disparities in physical activity and sedentary behaviors among US children and adolescents: Prevalence, correlates, and intervention implications. Journal of Public Health Policy. 2009;30(1 Suppl):S309–S334. doi: 10.1057/jphp.2008.46. [DOI] [PubMed] [Google Scholar]
- Zullig KJ, Ward RM, Horn T. The association between perceived spirituality, religiosity, and life satisfaction: The mediating role of self-rated health. Social Indicators Research. 2006;79:255–274. doi: 10.1007/s11205-005-4127-5. [DOI] [Google Scholar]


