Abstract
Objective
To examine the effects of an integrated, multi-component, school-based intervention program on cardiovascular disease (CVD) risk factors among a multi-ethnic cohort of middle school students.
Methods
HEALTHY was a cluster randomized, controlled, primary prevention trial. Middle school was the unit of randomization and intervention. Half the schools were assigned to an intervention program consisting of changes to the total school food environment and physical education classes, enhanced by educational outreach and behavior change activities and promoted by a social marketing campaign consisting of reinforcing messages and images. Outcome data reported (anthropometrics, blood pressure, and fasting lipid levels) were collected on a cohort of students enrolled at the start of 6th grade (~11-12 years old) and followed to end of 8th grade (~13-14 years old).
Results
42 middle schools were enrolled at 7 field centers; 4363 students provided both informed consent and CVD data at baseline and end of study. The sample was 52.7% female, 54.5% Hispanic, 17.6% non-Hispanic Black, 19.4% non-Hispanic White, and 8.5% other racial/ethnic combinations, and 49.6% were categorized as overweight or obese (BMI ≥ 85th percentile) at baseline. A significant intervention effect was detected in the prevalence of hypertension in non-Hispanic Black and White males. The intervention produced no significant changes in lipid levels.
Conclusions
The prevalence of some CVD risk factors is high in minority middle school youth and particularly males. A multi-component, school-based program achieved only modest reductions in these risk factors; however, promising findings occurred in non-Hispanic Black and White males with hypertension.
Keywords: cardiovascular disease risk, obesity, multi-ethnic, middle school, cluster design
Introduction
Cardiovascular disease (CVD) generally presents during adulthood, but the antecedents of this adult disease may be detectable in childhood. Elevated lipid and blood pressure levels have been associated with an increased risk of cardiovascular disease, and these risk factors track from childhood into adulthood1,2. Poor nutrition, a sedentary lifestyle, and genetic factors predispose to multiple CVD risk factors, including obesity, hyperlipidemia, and hypertension3.
CVD is the leading cause of mortality in the United States and is associated with the recent increase in obesity rates, which have tripled in youth since 19804. The cumulative nature of risk factors for CVD has motivated researchers to identify clinical or lifestyle interventions that can be implemented at the earliest preclinical stages. A number of these efforts have been tested in the school setting because schools can reach large, diverse populations at a developmentally-relevant time to impact the child's dietary intake and level of physical activity5,6. Previous school-based programs have increased knowledge and healthy behaviors for the purpose of improving cardiovascular health5-8.
The present paper reports findings from the recently concluded HEALTHY primary prevention trial, designed to determine if an integrated, multidisciplinary, middle school-based intervention program could lower risk factors for type 2 diabetes among students from high-risk minorities. HEALTHY was designed to compare the primary outcome, percent of students with body mass index (BMI) ≥85th percentile (combined categories for overweight and obese), in intervention versus control schools, and examine secondary risk factors including other measures of obesity as well as fasting glucose and insulin levels. The primary study results9 showed ~4% decrease in percent overweight and obese in both intervention and control schools, but no significant difference between intervention versus control. In a high-risk subgroup of those who were overweight or obese (BMI ≥ 85th percentile) at baseline, the intervention significantly decreased the proportion with BMI ≥ 95th percentile (obese). In the overall sample, intervention schools also had significantly greater reductions in BMI z-score, waist circumference > 90th percentile, and mean insulin level than control schools.
Secondary outcomes included CVD risk factors, which are the focus of this paper. We examine the effect of the HEALTHY intervention program on CVD risk factors, specifically lipid and blood pressure (BP) abnormalities, from baseline (start of students’ 6th grade in fall 2006, average age 11.8 years) to end of study (end of students’ 8th grade in spring 2009, average age 14.1 years). These data contribute to our understanding of CVD risk in multi-ethnic middle school-aged youth in the US.
Methods
Design of the HEALTHY Study
The HEALTHY study was a cluster randomized, controlled, primary prevention trial. Details of the HEALTHY study design and intervention have been described10-14. Briefly, 42 middle schools with at least 50% of students eligible for free or reduced-price lunch or belonging to a minority group were recruited by 7 participating centers (see study group listed in on-line appendix). All 6th grade students were recruited to participate in a “health screening” (height, weight, blood pressure, fasting blood draw) at baseline (start of 6th grade, fall 2006) and end of study (end of 8th grade, spring 2009). Students were given a $50 and a $60 incentive for participating in the baseline and end of study screenings, respectively. The study was approved by the Institutional Review Boards at each center, and informed consent from parents and assent from students were obtained prior to data collection.
Half of the schools were randomly assigned to receive a 2.5-year intervention program consisting of changes to the total school food environment and physical education classes. These modifications were enhanced by educational outreach and behavior change activities and promoted by a social marketing campaign consisting of reinforcing messages and images. Activities in the control schools were limited to recruitment and data collection only.
Participants and Methods
Methods for data collection have been described10. Students entering the 6th grade in fall 2006 who did not already have diabetes, were able to participate in physical education (PE) class, and provided parental consent and minor child assent were enrolled. Participating students arrived at school for a health screening data collection having fasted since midnight. Participants were asked at the beginning of the health screening when they last ate to confirm fasting status. Participants who reported eating after midnight were considered non-fasting and scheduled to return another day of the testing period. Blood was drawn and processed on-site and shipped to the HEALTHY central blood laboratory (Northwest Lipid Research Laboratories, University of Washington, Seattle).
Students provided sex, date of birth, and race/ethnicity by self report. Ethnicity (Hispanic yes/no) and race (check all that apply) were asked as two separate questions with laminated cards showing and defining choices. In general, once students had identified themselves as Hispanic they did not respond to the follow-up question of race.
Physical measures and vital signs were collected by research assistants who had been trained and certified according to study-wide standard criteria. Height and weight were measured without shoes using the Prospective Enterprises PE-AIM-101 stadiometer and the SECA Corporation Alpha 882 electronic scale, respectively. Body mass index (kg/m2) was calculated. BMI percentile by age and gender was determined using Centers for Disease Control and Prevention 2000 criteria with BMI ≥ 85th but < 95th percentile classified as overweight and BMI ≥ 95th percentile classified as obese. Blood pressure (BP) was measured using an automatic inflatable digital blood pressure monitor (Omron HEM-907 or HEM-907XL) three times, the first taken after the subject had been sitting quietly for at least 5 minutes and the second and third taken at 1 minute intervals. Appropriate cuff size was selected according to manufacturer's specifications based on a single measurement of student's upper arm circumference. Blood pressure was computed as the average of the second and third measurements. Information about medications that could have affected blood pressure was not collected. BP percentiles were determined using the National Heart Lung and Blood Institute guidelines, adjusting for age, sex, and height percentile15, and classified according to the following ranges: normal (< 90th percentile), prehypertension (90th-94th percentile), hypertension (HTN) stage 1 (95th-99th percentile), and hypertension stage 2 (> 99th percentile).
Abnormal lipid levels were defined using the following National Cholesterol Education Program (NCEP) guidelines16: total cholesterol borderline 4.4-5.1 mmol/L (170–199 mg/dL) , elevated ≥ 5.2 mmol/L (200 mg/dL); LDL cholesterol borderline 2.8-3.3 mmol/L (110–129 mg/dL), elevated ≥ 3.4 mmol/L (130 mg/dL); and HDL cholesterol low < 0.9 mmol/L (35 mg/dL). Because the NCEP criteria do not include a definition for elevated triglycerides, a cut-off ≥ 1.2 mmol/L (110 mg/dL) was used17.
Statistical Methods
Descriptive statistics including means, standard deviations, and percents were calculated for all variables. Separate generalized linear mixed models (GLMM) that took into account sources of variability both within and between schools were applied to test for effects. Change from baseline to end of study was tested in models with the end of study value as the dependent variable and the baseline value as a covariate. A series of models tested for treatment effect, for sex-by-treatment interaction, and for race-by-treatment interaction in the total sample and in the subgroup with BMI ≥ 85th percentile at baseline. Tests of race/ethnicity were limited to Hispanic, non-Hispanic Black, and non-Hispanic White, due to the diminished numbers of other groups. Models testing the interaction of BMI percentile category by treatment were also run in the total sample. Each variable in the interaction was included in the model as a main effect. If the interaction was significant, pair-wise comparisons of intervention versus control were performed for all levels of the other main effect variable. P-values represent exploratory findings; < 0.05 is considered statistically significant without adjustment for multiple comparisons. SAS 9.2 statistical software (SAS Institute Inc, Cary, NC) was used for all statistical analyses.
Results
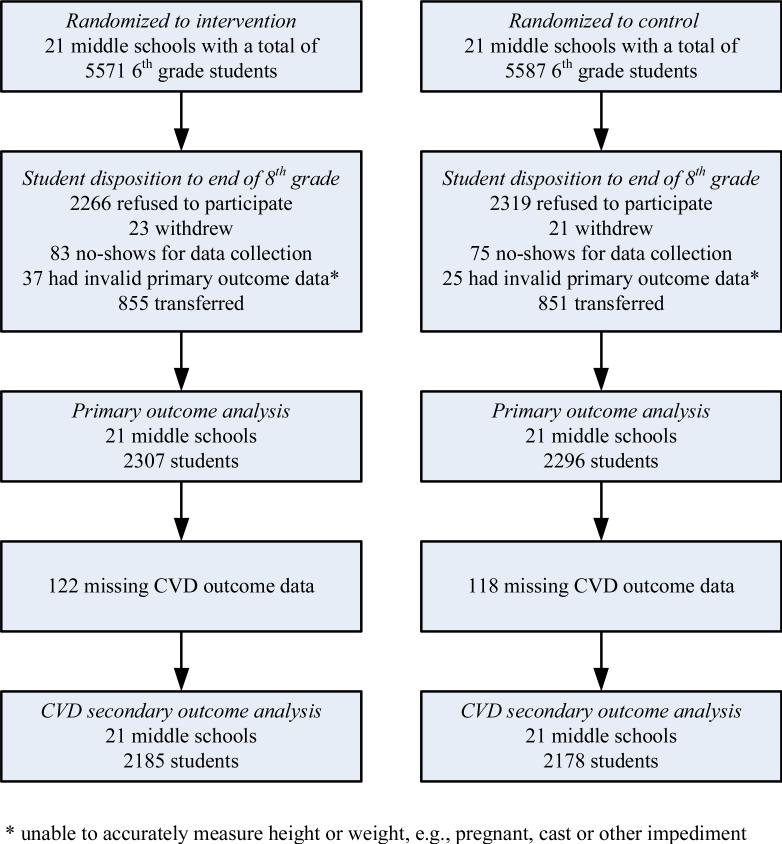
Figure 1 is a consort diagram tracking participation. All 42 schools randomized remained in the study. All 6th grade students were recruited unless they were already diagnosed with diabetes or could not take part in regular physical education classes. The figure shows that, of the 4603 students in the HEALTHY cohort, 4363 (95%) completed the assessment for cardiovascular risk factors at both baseline and end of study. Comparison of this sample versus cases with missing data showed no difference in distribution across intervention and control groups, sex, race/ethnicity, and baseline BMI percentile. The analysis sample was 52.7% female, 54.5% Hispanic, 17.6% non-Hispanic Black, 19.4% non-Hispanic White, and 8.5% other racial/ethnic combinations, and 49.6% were overweight or obese (BMI ≥ 85th percentile) at baseline.
Figure 1.
Consort Diagram for Analysis of CVD Secondary Outcome Data
Table 1 presents the descriptive statistics by sex and treatment group. Overall, there were no significant differences between intervention versus control either at baseline or end of study for any of the CVD risk factors, whether measured on the original continuous scale or categorized by cut-offs. Tests of treatment group effect in males versus females and across BMI percentile categories were also not significant. Although CVD risk factors were more common among children with BMI ≥ 85th percentile in general, the intervention showed no disproportionate effect on the subgroup that was overweight or obese at baseline. While there was no sex-by-treatment interaction, sex had a significant effect in the models, indicating that these measures are inherently different for males and females. Systolic BP was higher in boys than girls at both time points, while total, LDL, and HDL cholesterol were higher in boys at baseline but were below that of girls at end of study.
Table 1.
Descriptive Statistics* for CVD Risk Factors at Baseline (6th Grade) and End of Study (8th Grade), by Sex and Treatment Group
| CVD Risk Factors | Males (n=2062) | Females (n=2301) | ||||||
|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | |||||
| 6th | 8th | 6th | 8th | 6th | 8th | 6th | 8th | |
| Systolic blood pressure (mmHg) | 107.6, 10.3 | 113.7, 10.4 | 108.4, 10.1 | 115.1, 10.4 | 106.9, 9.7 | 107.8, 9.7 | 106.6, 10.2 | 108.4, 9.5 |
| Diastolic blood pressure (mmHg) | 63.1, 8.6 | 63.6, 8.0 | 64.2, 8.9 | 64.4, 7.9 | 64.0, 8.6 | 64.9, 7.9 | 63.6, 8.6 | 65.7, 7.7 |
| Blood pressure categories | ||||||||
| <90th percentile (Normal) | 83.0% | 82.4% | 78.1% | 78.4% | 82.3% | 87.4% | 84.4% | 87.0% |
| 90th-94th percentile (Pre-HTN) | 7.8% | 7.3% | 11.2% | 9.5% | 8.8% | 6.5% | 6.0% | 6.4% |
| 95th-99th percentile (HTN stage 1) | 7.4% | 7.7% | 8.5% | 9.0% | 6.4% | 5.2% | 6.2% | 5.6% |
| >99th percentile (HTN stage 2) | 1.7% | 2.6% | 2.1% | 3.1% | 2.5% | 0.9% | 3.5% | 1.0% |
| Total cholesterol (mmol/L) | 4.1, 0.7 | 3.8, 0.7 | 4.1, 0.7 | 3.8, 0.7 | 4.0, 0.7 | 3.9, 0.7 | 4.0, 0.7 | 3.9, 0.7 |
| Total cholesterol categories | ||||||||
| <4.4 | 68.6% | 83.5% | 65.3% | 82.7% | 73.8% | 78.0% | 72.4% | 78.6% |
| 4.4-5.1 (Borderline) | 24.2% | 13.6% | 26.6% | 13.4% | 20.3% | 16.8% | 22.4% | 17.4% |
| ≥5.2 (Elevated) | 7.2% | 2.9% | 8.1% | 3.9% | 5.9% | 5.1% | 5.3% | 4.0% |
| LDL cholesterol (mmol/L) | 2.3, 0.6 | 2.0, 0.6 | 2.3, 0.6 | 2.0, 0.6 | 2.2, 0.6 | 2.1, 0.6 | 2.2, 0.6 | 2.1, 0.6 |
| LDL categories | ||||||||
| <2.8 | 83.1% | 90.7% | 82.7% | 91.2% | 85.4% | 89.8% | 88.0% | 90.3% |
| 2.8-3.3 (Borderline) | 11.7% | 7.2% | 12.3% | 6.1% | 10.1% | 7.5% | 9.3% | 7.4% |
| ≥3.4 (Elevated) | 5.2% | 2.1% | 5.0% | 2.7% | 4.5% | 2.7% | 2.8% | 2.3% |
| HDL cholesterol (mg/dL) | 1.4, 0.3 | 1.3, 0.3 | 1.4, 0.3 | 1.3, 0.3 | 1.3, 0.3 | 1.4, 0.3 | 1.4, 0.3 | 1.4, 0.3 |
| HDL categories | ||||||||
| <0.9 (Low) | 4.4% | 9.0% | 3.6% | 8.0% | 5.1% | 3.8% | 4.9% | 5.3% |
| ≥0.9 | 95.6% | 91.0% | 96.4% | 92.0% | 94.9% | 96.2% | 95.1% | 94.7% |
| Triglycerides (mg/dL) | 1.0, 0.6 | 1.0, 0.6 | 1.0, 0.6 | 1.0, 0.6 | 1.0, 0.6 | 0.9, 0.4 | 1.0, 0.7 | 0.9, 0.5 |
| Triglyceride categories | ||||||||
| <1.2 | 76.6% | 79.6% | 76.4% | 79.9% | 76.3% | 84.1% | 76.3% | 81.8% |
| ≥1.2 (Elevated) | 23.4% | 20.4% | 23.6% | 20.1% | 23.7% | 15.9% | 23.7% | 18.2% |
Descriptive statistics are expressed as mean, sd or percent.
Table 2 presents descriptive statistics by treatment group within each of the three major categories of race/ethnicity. There was a significant interaction between treatment group and race/ethnicity (p=.0088) across the four BP categories. The intervention produced a significant decrease in the occurrence of hypertension and pre-hypertension in non-Hispanic Black (p=0.0073) and non-Hispanic White youth (p=0.0370). Further analysis showed that this only occurred in males.
Table 2.
Descriptive Statistics* for CVD Risk Factors at Baseline (6th Grade) and End of Study (8th Grade), by Race/Ethnicity and Treatment Group
| CVD Risk Factors | Hispanic (n=2379) | Non-Hispanic Black (n=769) | Non-Hispanic White (n=845) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Intervention | Control | |||||||
| 6th | 8th | 6th | 8th | 6th | 8th | 6th | 8th | 6th | 8th | 6th | 8th | |
| Systolic blood pressure (mmHg) | 107.0, 9.3 | 110.9, 10.5 | 107.3, 10.0 | 111.2, 10.6 | 108.6, 10.9 | 110.1, 11.0 | 109.2, 10.3 | 112.8, 11.4 | 106.5, 10.9 | 109.9, 9.8 | 107.3, 10.6 | 112.0, 9.8 |
| Diastolic blood pressure (mmHg) | 63.5, 8.2 | 64.8, 7.9 | 63.5, 8.3 | 64.8, 7.9 | 64.1, 8.7 | 63.6, 8.2 | 64.6, 8.6 | 65.7, 7.7 | 63.1, 9.6 | 63.0, 7.7 | 64.3, 9.6 | 64.9, 7.8 |
| Blood pressure categories | ||||||||||||
| <90th %ile (Normal) | 84.4% | 82.4% | 82.9% | 83.4% | 77.9% | 86.6% | 78.2% | 78.2% | 84.3% | 91.4% | 78.1% | 84.4% |
| 90th-94th %ile (Pre-HTN) | 8.6% | 8.3% | 7.9% | 7.6% | 10.3% | 6.2% | 9.7% | 8.8% | 3.8% | 3.0% | 9.3% | 7.4% |
| 95th-99th %ile (HTN stage 1) | 5.5% | 7.7% | 6.9% | 7.0% | 8.9% | 5.2% | 8.5% | 10.0% | 8.9% | 4.6% | 9.1% | 6.5% |
| >99th %ile (HTN stage 2) | 1.5% | 1.7% | 2.3% | 2.0% | 3.0% | 2.1% | 3.6% | 3.0% | 3.0% | 1.1% | 3.6% | 1.7% |
| Total cholesterol (mmol/L) | 4.0, 0.7 | 3.8, 0.7 | 4.0, 0.7 | 3.8, 0.7 | 4.2, 0.7 | 3.9, 0.7 | 4.3, 0.7 | 4.0, 0.7 | 4.1, 0.7 | 3.8, 0.7 | 4.1, 0.7 | 3.8, 0.7 |
| Total cholesterol categories | ||||||||||||
| <4.4 | 74.4% | 81.1% | 72.6% | 82.5% | 66.1% | 77.9% | 59.1% | 72.7% | 70.0% | 81.6% | 67.2% | 84.0% |
| 4.4-5.1 (Borderline) | 19.5% | 15.4% | 21.5% | 14.1% | 25.5% | 16.4% | 31.8% | 21.2% | 23.8% | 14.9% | 26.9% | 12.8% |
| ≥5.2 (Elevated) | 6.0% | 3.5% | 5.9% | 3.4% | 8.4% | 5.7% | 9.1% | 6.1% | 6.2% | 3.5% | 5.9% | 3.2% |
| LDL cholesterol (mmol/L) | 2.2, 0.6 | 2.0, 0.6 | 2.2, 0.6 | 2.0, 0.6 | 2.3, 0.6 | 2.2, 0.6 | 2.4, 0.6 | 2.3, 0.6 | 2.3, 0.6 | 2.1, 0.6 | 2.3, 0.6 | 2.1, 0.6 |
| LDL categories | ||||||||||||
| <2.8 | 86.3% | 91.7% | 88.1% | 91.9% | 80.0% | 86.8% | 77.0% | 86.7% | 84.3% | 90.5% | 84.8% | 91.6% |
| 2.8-3.3 (Borderline) | 10.0% | 6.2% | 8.8% | 6.3% | 13.0% | 10.0% | 16.7% | 8.8% | 9.7% | 7.0% | 11.2% | 5.7% |
| ≥3.4 (Elevated) | 3.7% | 2.1% | 3.1% | 1.8% | 7.1% | 3.2% | 6.4% | 4.5% | 5.9% | 2.4% | 4.0% | 2.7% |
| HDL cholesterol (mmol/L) | 1.3, 0.3 | 1.3, 0.3 | 1.3, 0.3 | 1.3, 0.3 | 1.3, 0.3 | 1.4, 0.3 | 1.5, 0.3 | 1.4, 0.3 | 1.3, 0.3 | 1.3, 0.3 | 1.4, 0.3 | 1.3, 0.3 |
| HDL categories | ||||||||||||
| <0.9 (Low) | 6.2% | 6.4% | 5.4% | 8.3% | 2.3% | 3.4% | 1.5% | 3.3% | 3.8% | 9.7% | 4.8% | 6.1% |
| ≥0.9 | 93.8% | 93.6% | 94.6% | 91.7% | 97.7% | 96.6% | 98.5% | 96.7% | 96.2% | 90.3% | 95.2% | 93.9% |
| Triglycerides (mmol/L) | 1.1, 0.6 | 1.0, 0.5 | 1.1, 0.6 | 1.0, 0.6 | 0.8, 0.3 | 0.7, 0.3 | 0.8, 0.4 | 0.7, 0.3 | 1.0, 0.5 | 0.9, 0.5 | 1.0, 0.7 | 0.9, 0.4 |
| Triglyceride categories | ||||||||||||
| <1.2 | 70.9% | 77.0% | 70.5% | 76.6% | 91.8% | 93.6% | 91.5% | 93.0% | 74.3% | 83.2% | 79.2% | 83.2% |
| ≥1.2 (Elevated) | 29.1% | 23.0% | 29.5% | 23.4% | 8.2% | 6.4% | 8.5% | 7.0% | 25.7% | 16.8% | 20.8% | 16.8% |
Descriptive statistics are expressed as mean, sd or percent.
To further explore the race/ethnicity-by-gender differences, we examined the distribution across BP categories for males by race/ethnicity and treatment group (see Table 3). In the intervention schools, the proportion of Black males with pre-hypertension fell from 10.8% in 6th grade to 6.4% in 8th grade, while in the control schools it remained about the same (11.7% and 11.0%, respectively). Furthermore, among Black males the prevalence of hypertension (either stage 1 or 2) in intervention schools dropped from 13.8% to 8.3%, while in the control schools it increased from 10.4% to 18.6%. The major finding among White males was a reduction in the occurrence of hypertension, which dropped from 11.5% to 6.5% in intervention schools, versus 12.6% to 10.8% in control schools. There was no significant effect of intervention on change in BP in Hispanic youth.
Table 3.
Distribution of Blood Pressure Categories in Males, by Race/Ethnicity and Treatment Group
| Blood Pressure Categories | Hispanic (N=1124, p=.6640) | Non-Hispanic Black (N=348, p=.0009) | Non-Hispanic White (N=430, p=.0475) | |||
|---|---|---|---|---|---|---|
| 6th | 8th | 6th | 8th | 6th | 8th | |
| <90th percentile (Normal) | ||||||
| Intervention | 85.6% | 78.2% | 75.4% | 85.2% | 84.0% | 91.5% |
| Control | 79.3% | 78.3% | 77.9% | 70.3% | 73.9% | 82.6% |
| 90th-94th percentile (pre-HTN) | ||||||
| Intervention | 7.6% | 9.2% | 10.8% | 6.4% | 4.5% | 2.0% |
| Control | 10.0% | 10.0% | 11.7% | 11.0% | 13.5% | 6.5% |
| 95th-99th percentile (HTN stage 1) | ||||||
| Intervention | 5.5% | 9.9% | 9.9% | 4.9% | 10.0% | 5.5% |
| Control | 9.3% | 8.7% | 9.0% | 13.8% | 8.3% | 7.8% |
| >99th percentile (HTN stage 2) | ||||||
| Intervention | 1.2% | 2.7% | 3.9% | 3.4% | 1.5% | 1.0% |
| Control | 1.4% | 3.0% | 1.4% | 4.8% | 4.3% | 3.0% |
Discussion
We present data from a large cohort of multi-ethnic middle-school children enrolled in a school-based primary prevention trial of risk factors for type 2 diabetes. A multi-component integrated intervention program did not significantly reduce CVD risk factors in the overall sample. There was evidence of an intervention effect on the percentage of non-Hispanic Black and White subjects with hypertension. In particular, the percentage with hypertension was reduced among Black and White males, who bear a disproportionate burden from CVD in adulthood18.
Childhood hypertension has been demonstrated to track into adulthood2 and to increase the risk of premature death by 57%19. Hypertension in adults is considered the most significant CVD risk factor worldwide, contributing to one-half of the coronary artery disease and approximately two-thirds of the cerebrovascular disease20. Similar to trends in adults, the prevalence of hypertension in middle school children is significantly higher in males than in females21,22. Our baseline data from the HEALTHY cohort confirm the increased prevalence of hypertension in young males22, and suggest that lifestyle-based interventions to reduce BP might effectively target the early adolescent male population.
In terms of race, national health survey data over the last two decades have shown the highest prevalence23 and steepest secular rise24 in hypertension is among Black youth (especially males). The HEALTHY intervention program had a beneficial effect on BP in the Black male subgroup. A previous school-based intervention that produced significant changes in diet, exercise, and health knowledge failed to show significant change in BP7.
Studies have shown that abnormal lipid levels in childhood may persist into adulthood, placing an individual at increased risk for CVD25. The tabled values show change in lipid levels from 6th to 8th grades by various subgroups, but we found no significant intervention effect. Lipid profiles change considerably with normal growth and maturation, with age-specific values for mean total cholesterol peaking at about 11 years of age and declining thereafter3. The lack of statistically significant difference between intervention and control groups could be attributed to modest effects of the intervention being dominated by developmental fluctuations in our middle-school sample.
Weight gain even within the normal BMI range increases risk of CVD26, whereas weight loss can substantially reduce it. It is known that crossing BMI thresholds toward obesity is associated with increases in cytokines and bioactive mediators that adversely affect cardiovascular health27. Adipose tissue is now recognized as an active endocrine and paracrine organ that dynamically affects the atherosclerotic process28. The HEALTHY intervention program was able to reduce the percentage of obese (BMI > 95th percentile) youth, as well as other traits (namely, waist circumference and fasting insulin) which co-migrate with CVD in adults.
The breadth of this study is a salient strength, as it represents a large sample of racially and ethnically diverse students from across the United States. Other school-based interventions have involved less than 1500 students within limited geographic regions5-8. Moreover, the HEALTHY intervention program is unique in scope, representing an extensive and all-encompassing attempt to change aspects of the school nutrition, physical education, promotional, and educational environments. We were able to implement this multi-faceted HEALTHY intervention in a relevant, at-risk population with high levels of fidelity9.
A number of limitations are acknowledged. About half of the student participants were in the overweight and obese categories at baseline. As a prevention strategy, it may have been more effective to focus our intervention on an at-risk, predominantly non-obese population of elementary school age children. Such an approach is supported by the concept of the period of ‘adiposity rebound’ as a critical phase in the development of obesity29. Also, students spend one-third of the day in school, which leaves them exposed to numerous other environments in the other two-thirds. The HEALTHY intervention undertook limited attempts to influence the students’ non-school milieu, including a newsletter sent to families providing information about healthy lifestyle routines and first-person testimony from peers about successes and failures. Families also received materials and education supporting maintenance of a healthy lifestyle during holiday and summer breaks. Parental involvement and compliance with healthy habits were not evaluated. Given the nature of the design as a population-based field trial with limited access to conduct detailed data collection in individual students (compared to a clinical trial environment), we were not able to collect reliable information on relevant diagnoses and treatments, such as high blood pressure and abnormal lipid values. We present the data classified by cut-off values but do not claim that these represent diagnoses.
Due to the integrated nature of the HEALTHY intervention program, with all parts targeting delivery and support of a common theme, it is not possible to determine the individual contribution of each component to the reduction in BP observed in our subjects. The physical education component targeted an increase in the time spent in moderate-to-vigorous physical activity during PE class. A reduction in systemic BP was observed in a recent study evaluating the effects of a more regimented exercise program on at-risk children30. While none of the HEALTHY nutrition goals were directly focused on decreasing sodium intake, a number of strategies (like reducing snack portion sizes and the consumption of water in place of fruit juices and sugared sodas) may have indirectly reduced sodium intake. However, we did not monitor sodium intake in our subjects, so we are unable to evaluate further.
In conclusion, while the HEALTHY intervention program did not achieve the primary objective of reducing rates of overweight/obesity9 and did not have a meaningful effect on other CVD risk factors in the total sample, the impact on blood pressure in males is notable. Given that hypertension is considered the most important CVD risk factor worldwide20, the HEALTHY study findings suggest that specific subgroups may substantially benefit from exposure to such programs in middle school years and perhaps prevent the development of risk factors that culminate in serious cardiovascular events during adulthood. The challenge for future public health research and intervention efforts like HEALTHY may be to devise strategies to target high-risk subgroups without being charged with stereotyping, discrimination, or stigmatization.
Acknowledgments
This work was completed with funding from NIDDK/NIH grant numbers U01-DK61223, U01-DK61230, U01-DK61231, and U01-DK61249, and with additional support from the American Diabetes Association. HEALTHY intervention materials and protocol are available for download at http://www.healthystudy.org/.
On-line Appendix
The following individuals and institutions constitute the HEALTHY Study Group (* indicates principal investigator or director): Study Chair Children's Hospital Los Angeles: F.R. Kaufman Field Centers Baylor College of Medicine: T. Baranowski*, L. Adams, J. Baranowski, A. Canada, K.T. Carter, K.W. Cullen, M.H. Dobbins, R. Jago, A. Oceguera, A.X. Rodriguez, C. Speich, L.T. Tatum, D. Thompson, M.A. White, C.G. Williams Oregon Health & Science University: L. Goldberg*, D. Cusimano, L. DeBar, D. Elliot, H.M. Grund, S. McCormick, E. Moe, J.B. Roullet, D. Stadler Temple University: G. Foster* (Steering Committee Chair), J. Brown, B. Creighton, M. Faith, E.G. Ford, H. Glick, S. Kumanyika, J. Nachmani, L. Rosen, S. Sherman, S. Solomon, A. Virus, S. Volpe, S. Willi University of California at Irvine: D. Cooper*, S. Bassin, S. Bruecker, D. Ford, P. Galassetti, S. Greenfield, J. Hartstein, M. Krause, N. Opgrand, Y. Rodriguez, M. Schneider University of North Carolina at Chapel Hill: J. Harrell*, A. Anderson, T. Blackshear, J. Buse, J. Caveness, A. Gerstel, C. Giles, A. Jessup, P. Kennel, R. McMurray, A-M. Siega-Riz, M. Smith, A. Steckler, A. Zeveloff University of Pittsburgh: M.D. Marcus*, M. Carter, S. Clayton, B. Gillis, K. Hindes, J. Jakicic, R. Meehan, R. Noll, J. Vanucci, E. Venditti University of Texas Health Science Center at San Antonio: R. Treviño*, A. Garcia, D. Hale, A. Hernandez, I. Hernandez, C. Mobley, T. Murray, J. Stavinoha, K. Surapiboonchai, Z. Yin Coordinating Center George Washington University: K. Hirst*, K. Drews, S. Edelstein, L. El ghormli, S. Firrell, M. Huang, P. Kolinjivadi, S. Mazzuto, T. Pham, A. Wheeler Project Office National Institute of Diabetes and Digestive and Kidney Diseases: B. Linder*, C. Hunter, M. Staten Central Biochemistry Laboratory University of Washington Northwest Lipid Metabolism and Diabetes Research Laboratories: S.M. Marcovina*
Footnotes
SM Willi was a consultant to Temple University during the study and is employed at the Children's Hospital of Philadelphia. R Jago was affiliated with Baylor College of Medicine during the study and is currently at the University of Bristol.
Clinical Trials Registration: http://clinicaltrials.gov/, number NCT00458029.
Author Contribution Statement: The writing group (Steven M. Willi, chair, Kathryn Hirst, Russell Jago, John Buse, Francine Kaufman, Laure El ghormli, Stanley Bassin, Diane Elliot, and Daniel E. Hale) takes responsibility for the content of this article. All authors confirm that they contributed to the intellectual content of the manuscript conception and design, or analysis and interpretation of data. All authors approve the final version of the published manuscript.
Conflict of Interest Statement: Dr. Kaufman stepped down as Study Chair when she took a position with Medtronic; she retains an appointment at Children's Hospital Los Angeles, University of Southern California Center for Diabetes, Endocrinology & Metabolism. The other authors have no conflicts to disclose.
References
- 1.Webber LS, Srinivasan SR, Wattingney WA, Berenson GS. Tracking of serum lipids and lipoproteins from childhood to adulthood: the Bogalusa Heart Study. Am J Epidemiol. 1991;133:884–849. doi: 10.1093/oxfordjournals.aje.a115968. [DOI] [PubMed] [Google Scholar]
- 2.Fuentes RM, Notkola IL, Shemeikka S, Tuomilehto J, Nissinen A. Tracking of systolic blood pressure during childhood: a 15 year follow-up population-based family study in eastern Finland. J Hypertens. 2002;20:195–202. doi: 10.1097/00004872-200202000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Daniels SR, Greer FR, the Committee on Nutrition Lipid screening and cardiovascular health in childhood. Pediatrics. 2008;122:198–208. doi: 10.1542/peds.2008-1349. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007-2008. JAMA. 2010;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 5.Harrell JS, McMurray RG, Bangdiwala SI, Frauman AC, Gansky SA, Bradley CB. Effects of a school-based intervention to reduce cardiovascular disease risk factors in elementary-school children: the Cardiovascular Health in Children (CHIC) Study. J Pediatr. 1996;128:797–805. doi: 10.1016/s0022-3476(96)70332-3. [DOI] [PubMed] [Google Scholar]
- 6.Hollar D, Messiah SE, Lopez-Mitnik G, Hollar TL, Almon M, Agatston AS. Healthier options for public schoolchildren program improves weight and blood pressure in 6- to 13-year-olds. J Amer Dietetic Assoc. 2010;110:261–267. doi: 10.1016/j.jada.2009.10.029. [DOI] [PubMed] [Google Scholar]
- 7.Covelli MM. Efficacy of a school-based cardiac healthy promotion intervention program for African-American adolescents. Applied Nursing Research. 2008;21:173–180. doi: 10.1016/j.apnr.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 8.McMurray RG, Harrell JS, Bangdiwala SI, Bradley CB, Deng S, Levine A. A school-based intervention can reduce body fat and blood pressure in young adolescents. Journal of Adolescent Health. 2002;31:125–132. doi: 10.1016/s1054-139x(02)00348-8. [DOI] [PubMed] [Google Scholar]
- 9.HEALTHY Study Group A school-based intervention for diabetes risk reduction. N Eng J Med. 2010;363(5):443–453. doi: 10.1056/NEJMoa1001933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.HEALTHY Study Group HEALTHY study rationale, design and methods: moderating risk of type 2 diabetes in multi-ethnic middle school students. International Journal of Obesity. 2009;33:S4–S20. doi: 10.1038/ijo.2009.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gillis B, Mobley C, Stadler DD, et al. for the HEALTHY Study Group Rationale, design and methods of the HEALTHY study nutrition intervention component. International Journal of Obesity. 2009;33:S29–S36. doi: 10.1038/ijo.2009.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McMurray RG, Bassin S, Jago R, et al. for the HEALTHY Study Group Rationale, design and methods of the HEALTHY study physical education intervention component. International Journal of Obesity. 2009;33:S37–S43. doi: 10.1038/ijo.2009.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Venditti EM, Elliot DL, Faith MS, et al. for the HEALTHY Study Group Rationale, design and methods of the HEALTHY study behavior intervention component. International Journal of Obesity. 2009;33:S44–S51. doi: 10.1038/ijo.2009.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DeBar LL, Schneider M, Ford EG, et al. for the HEALTHY Study Group Social marketing-based communications to integrate and support the HEALTHY study intervention. International Journal of Obesity. 2009;33:S52–S59. doi: 10.1038/ijo.2009.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–576. [PubMed] [Google Scholar]
- 16.National Cholesterol Education Program (NCEP) Highlights of the report of the expert panel on blood cholesterol in children and adolescents. Pediatrics. 1992;89:495–501. [PubMed] [Google Scholar]
- 17.Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. 2003;157:821–827. doi: 10.1001/archpedi.157.8.821. [DOI] [PubMed] [Google Scholar]
- 18.Lloyd-Jones D, Adams RJ, Brown TM, et al. members of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee Executive summary: heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation. 2010;121:948–954. doi: 10.1161/CIRCULATIONAHA.109.192666. [DOI] [PubMed] [Google Scholar]
- 19.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Eng J Med. 2010;362:485–493. doi: 10.1056/NEJMoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whitworth JA. World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;2003;21:1983–1992. doi: 10.1097/00004872-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ. Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics. 2004;113:475–482. doi: 10.1542/peds.113.3.475. [DOI] [PubMed] [Google Scholar]
- 22.Jago R, Harrell JS, McMurray RG, Edelstein S, El ghormli L, Bassin S. Prevalence of abnormal lipid and blood pressure values among an ethnically diverse population of eighth-grade adolescents and screening implications. Pediatrics. 2006;117:2065–2073. doi: 10.1542/peds.2005-1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Din-Dzietham R, Liu Y, Bielo M-V, Shamsa F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007;116:1488–1496. doi: 10.1161/CIRCULATIONAHA.106.683243. [DOI] [PubMed] [Google Scholar]
- 24.Muntner P, He J, Cutler JA, Wildman RP, Whelton PK. Trends in blood pressure among children and adolescents. JAMA. 2004;291:2107–2113. doi: 10.1001/jama.291.17.2107. [DOI] [PubMed] [Google Scholar]
- 25.Huang TT, Nansel TR, Belsheim AR, Morrison JA. Sensitivity, specificity and predictive values of pediatric metabolic syndrome components in relation to adult metabolic syndrome: the Princeton LRC follow-up study. J Pediatr. 2008;152:185–190. doi: 10.1016/j.jpeds.2007.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berenson GS, Srinivasan SR, Bao W, Newman WP, Tracy RE, Wattigney WA, for the Bogalusa Heart Study Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. N Eng J Med. 1998;338:1650–1656. doi: 10.1056/NEJM199806043382302. [DOI] [PubMed] [Google Scholar]
- 27.Van Gaal LF, Merten IL, DeBlock CE. Mechanisms linking obesity with cardiovascular disease. Nature. 2006;444:875–880. doi: 10.1038/nature05487. [DOI] [PubMed] [Google Scholar]
- 28.Lau DCW, Dhillon B, Yan H, Szmitko PE, Verma S. Adipokines: molecular links between obesity and atheroslcerosis. Am J Physiol Heart Circ Physiol. 2005;288:H2031–H2041. doi: 10.1152/ajpheart.01058.2004. [DOI] [PubMed] [Google Scholar]
- 29.Rolland-Cachera MF, Deheeger M, Maillot M, Bellisle F. Early adiposity rebound: causes and consequences for obesity in children and adults. Int J Obes. 2006;30:11–17. doi: 10.1038/sj.ijo.0803514. [DOI] [PubMed] [Google Scholar]
- 30.Farpour-Lambert NJ, Aggoun Y, Marchand LM, Martin XE, Herrmann FR, Beghetti M. Physical activity reduces systemic blood pressure and improves early markers of atherosclerosis in pre-pubertal obese children. J Am Coll Cardiol. 2009;54:2396–2406. doi: 10.1016/j.jacc.2009.08.030. [DOI] [PubMed] [Google Scholar]