Abstract
Insulin-like growth factor 1 (IGF-1) is an endocrine and autocrine/paracrine growth factor that circulates at high levels in the plasma and is expressed in most cell types. IGF-1 has major effects on development, cell growth and differentiation, and tissue repair. Recent evidence indicates that IGF-1 reduces atherosclerosis burden and improves features of atherosclerotic plaque stability in animal models. Potential mechanisms for this atheroprotective effect include IGF-1–induced reduction in oxidative stress, cell apoptosis, proinflammatory signaling, and endothelial dysfunction. Aging is associated with increased vascular oxidative stress and vascular disease, suggesting that IGF-1 may exert salutary effects on vascular aging processes. In this review, we will provide a comprehensive update on IGF-1's ability to modulate vascular oxidative stress and to limit atherogenesis and the vascular complications of aging.
Keywords: IGF-1, Oxidant stress, Aging, Atherosclerosis, Inflammation
IT is widely accepted that aging is an important risk factor for the development of atherosclerosis and its vascular complications. The underlying mechanism whereby aging elevates the probability of disease onset remains obscure; however, it is likely closely related to underlying mechanisms of atherogenesis, the most accepted being the oxidation hypothesis (1). In brief, oxidatively modified lipoproteins cause lipid-laden macrophage, or foam cell, accumulation in the fatty streak, leading to the initiation of atherosclerotic lesion formation. Subsequent recruitment of immune cells establishes a proinflammatory status, further causing elevated oxidative stress, which in turn triggers a series of events including apoptotic or necrotic death of vascular and nonvascular cells. Endothelial dysfunction, commonly represented by dysregulation of the normal contractile response of the vasculature, contributes to the recruitment of immune cells and the proinflammatory status. Oxidative stress induced lesion formation and endothelial dysfunction are interrelated, that is, an elevation in oxidative stress promotes endothelial dysfunction, and vice versa, endothelial dysfunction promotes atherosclerosis leading to elevated oxidative stress. Intriguingly, increased oxidative stress is also considered to be a key factor in mechanisms of aging-associated changes in tissue integrity and function (2). Thus, prooxidant stimuli induce apoptotic and nonapoptotic cell death and premature cell senescence in multiple cell types and tissues, which is highly relevant to both the aging process and to the pathogenesis of atherosclerosis.
GROWTH FACTORS AND ATHEROSCLEROSIS; PERMISSIVE OR PREVENTATIVE?
Traditionally, the role of growth factors in atherosclerosis has been thought to be permissive, in particular, by stimulating vascular smooth muscle cell (VSMC) migration and proliferation, thereby promoting neointima formation (3–5). However, recent findings from our group (6) and others (7,8) suggest that some growth factors might have unexpected antiatherogenic effects. Tang and colleagues (8) showed that the absence of platelet-derived growth factor (PDGF)-B in circulating cells, which are a major source of PDGF in atherosclerotic lesions, led to a phenotypic change in lesion composition, namely enhanced inflammatory cell infiltration. Intriguingly, data from the same group indicated that elimination of PDGF-B in circulating cells or blockade of PDGF receptors delayed but did not inhibit smooth muscle accumulation in lesions (9). Their data suggest a modest contribution of PDGF to atheroprogression but a major inhibitory effect of PDGF on inflammatory responses and on monocyte accumulation, potentially limiting lesion expansion. Recently, cardiac-specific overexpression of transforming growth factor-beta, a growth factor that promotes VSMC proliferation and matrix protein production (reviewed in (10)), was reported to limit atherosclerotic plaque burden (7). These plaques were characterized by fewer T-lymphocytes, more collagen, less lipid, and lower expression of inflammatory cytokines (7). In our recent study, insulin-like growth factor (IGF)-1 demonstrated antiatherogenic effects via anti-inflammatory and prorepair mechanisms, both of which are mechanisms coupled to changes in vascular oxidative stress (6). Since prorepair mechanisms and alterations in oxidative stress are also closely related to the physiology of aging, these effects of IGF-1 are relevant to understanding the role of IGF-1 in the aging process. In this review, we will provide a comprehensive update on IGF-1’s ability to modulate vascular oxidative stress and to limit atherogenesis and the vascular complications of aging.
THE IGF-1 SYSTEM AND THE VASCULATURE
IGF-1 has a fundamental role in both prenatal and postnatal development and exerts all of its known physiologic effects by binding to the IGF-1 receptor (IGF-1R) (11). Its effects are modulated by multiple IGF binding proteins (IGFBPs) (12). Circulating IGF-1 is generated by the liver under the control of growth hormone (GH). The binding of GH with its hepatic receptor stimulates expression and release of IGF-1 peptide in the circulation, which has high affinity for IGFBPs, and represents the endocrine form of IGF-1 (12,13). In addition to the liver, many other organs produce IGF-1, representing autocrine and paracrine forms of IGF-1 (12,13).
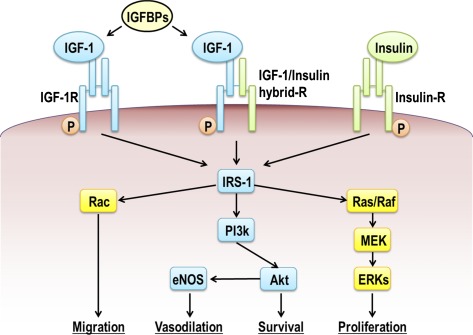
The IGF-1R is a tetramer consisting of two extracellular α-chains and two intracellular β-chains (14). The β-chains include an intracellular tyrosine kinase domain that is thought to be essential for most of the receptor’s biologic effects (13). IGF-1R signaling involves autophosphorylation and subsequent tyrosine phosphorylation of Shc and insulin receptor substrate-1, -2, -3, and -4 (15). Insulin receptor substrate serves as a docking protein and can activate multiple signaling pathways, including phosphoinositide 3-kinase (PI3K), Akt, and mitogen-activated protein kinase (11,16). The activation of these signaling pathways induces differential biologic actions of IGF-1, including cell growth, migration, and survival (17) (Figure 1). The IGF-1R can form hybrid receptors with the insulin receptor. These hybrid receptors consist of a half (alpha- and beta-subunits) of the insulin receptor and a half (alpha- and beta- subunits) of the IGF-1R. In VSMCs, both IGF-1 and insulin receptor subunits are expressed, but expression of the former is higher than the latter, resulting in dominant expression of IGF-1R and insulin/IGF-1 hybrid receptors (18–20), making VSMCs insensitive to insulin, because the hybrid receptor predominantly mediates IGF-1 signaling (21).
Figure 1.
Insulin-like growth factor (IGF)-1 signal transduction. IGF-1 binds to IGF-1R and IGF-1/Insulin hybrid receptor, whereas insulin binds only to the insulin receptor (Insulin-R), and triggers several signaling pathways. IGF binding proteins modulate IGF-1 signaling by altering IGF-1 binding to the receptors. The IGF-1R is a tyrosine kinase that undergoes autophosphorylation and catalyzes the phosphorylation of multiple cellular proteins, including members of the insulin receptor substrate (IRS) family. On phosphorylation, IRSs interact with signaling molecules, including Akt, Ras/Raf, and Rac. Activation of the phosphoinositide 3-kinase and Akt pathway supports cell survival and enhances endothelial nitric oxide synthase activity, thereby inducing vasodilation. The Ras/Raf pathway is critical for proliferative responses, whereas activation of Rac is important for cell migration.
In vascular endothelial cells (ECs), both IGF-1R and insulin receptor subunits are expressed, and IGF-1R is more abundant than the insulin receptor (22). Thus, ECs express IGF-1R, insulin/IGF-1 hybrid receptor, and insulin receptor. However, ECs appear more sensitive than VSMCs to insulin; in fact, insulin at physiological concentrations activates insulin but not IGF-1 or hybrid receptors (23).
IGF-1 binding to these receptors is modulated by six different IGFBPs. The expression of IGFBPs are tissue- and developmental stage–specific, and the concentrations of IGFBPs in different body compartments are different (24). The functions of IGFBPs are regulated by phosphorylation, proteolysis, polymerization, and cell or matrix association of the IGFBP (25). All six IGFBPs have been shown to inhibit IGF-1 action, but IGFBP-1, -3, and -5 are also shown to stimulate IGF-1 action (12). Some of IGFBPs’ effects might be IGF-1 independent (24,26).
In addition to this already complicated system, a variety of hormones and growth factors regulate IGF-1, IGF-1R, and IGFBP expression in most tissues. Moreover, there is crosstalk between IGF-1 signaling pathways and those of other growth factors and hormones (27,28). Thus, the physiological consequences of IGF-1 action are potentially altered by several mechanisms. It is outside the scope of this review to discuss all physiological functions of IGF-1 and its related peptides in the vasculature, and readers are referred to recent reviews (29–31).
IGF-1 is a potent mitogen and antiapoptotic factor for VSMC and ECs and is also promigratory (32). Thus, there is reason to speculate that IGF-1 could be proatherogenic, via its ability to stimulate VSMC migration and proliferation (3–5), enhance chemotactic macrophage migration (33), and promote cell adherent molecule expression (34,35). Potential reductions in IGF-1 effects could thus be beneficial in certain pathologic conditions in the vasculature, such as the early stages of atherosclerotic plaque formation characterized by hypertrophy/hyperplasia of VSMCs. However, it has also been postulated that reduced IGF-1 prosurvival effects could be detrimental in other conditions in which loss of VSMCs contributes to the disease process, such as destabilization of atherosclerotic plaques (36).
CLINICAL STUDIES SHOWING A LINK BETWEEN IGF-1 AND CARDIOVASCULAR DISEASE
Current studies on the association of IGF-1 levels with cardiovascular disease as an independent cardiovascular risk factor remain inconclusive but suggest an inverse relationship between the prevalence of vascular disease and the bioavailability of IGF-1. Some cross-sectional and prospective studies (37–43) suggest a positive association between IGF-1 (and in some cases IGFBP-3) and atherosclerosis. Others (44–54) found that low IGF-1 is a predictor of ischemic heart disease and mortality, consistent with the potential antiapoptotic, antioxidant, and plaque stabilization actions of IGF-1. Several large prospective cohort studies failed to systematically confirm these findings (55–60). Several methodological constraints can explain this variance. So far, most studies have used total extractable IGF-1 as an estimate for IGF-1 activity in vivo. However, this provides only a crude estimate of the active hormone, as less than 1% is in its free form, and only free IGF-1 is believed to readily cross the endothelium and interact with its receptor. Of note, IGFBPs, in addition to their potential IGF-1 independent actions, might modulate IGF-1 bioactivity without any changes in the extractable concentrations of total IGF-1. Furthermore, the activity of IGFBPs is modulated by several IGFBP proteases, complicating the analysis of IGF-1 bioactivity. Brugts and colleagues (61) recently introduced a new method to assess IGF-1 bioactivity. Instead of measuring immunoreactive IGF-1, this kinase receptor assay measures IGF-1 bioactivity of serum by its ability to activate IGF-1R autophosphorylation. Thus this assay accounts for IGFBP and IGFBP protease modulation of ligand and receptor interactions. Using this technique, IGF-1 bioactivity was evaluated in relation to survival in a population of elderly men in the Netherlands. Individuals in the highest IGF-bioactivity quartile survived significantly longer than those in the lowest quartile, both in the total population and in subgroups with a high inflammatory risk profile or a medical history of cardiovascular disease. Taken together with results from two other studies (61,62) that demonstrated an association between low free IGF-1 and risk of carotid and coronary artery disease, these findings suggest that an increase in bioactive IGF-1 is associated with lower atherosclerosis risk and cardiovascular mortality. Further support for this concept comes from studies investigating a polymorphism of the IGF-1 gene promoter, namely a variable length of a cytosine–adenosine repeat sequence, shown to influence circulating IGF-1 levels. In the population-based Rotterdam study (63), individuals without the wild-type 192 bp allele had 18% lower circulating IGF-1 and were at increased risk for type 2 diabetes, myocardial infarction, and presence of left ventricular hypertrophy (64). In the presence of hypertension, these individuals also had higher carotid intima-media thickness and higher aortic pulse wave velocity (65). Additional analyses from this study demonstrated that subjects heterozygous for the 192 bp or 194 bp alleles or noncarriers of these two alleles had lower IGF-1 and higher myocardial infarction-related mortality, particularly in cases of coexisting diabetes (66,67). However, others have not replicated these studies (68) and in a study in the United Kingdom, the opposite association was found between the 192 bp allele and IGF-1 levels (69). It is also relevant to point out that loss-of-function mutations in genes encoding components of the insulin/IGF-1 pathway are associated with extension of life in mice (70,71). Recently, mutations in the IGF-1R gene that result in reduced IGF-1 signaling have been identified in centenarians (72). Additional studies are required to determine whether genetically determined low IGF-1 levels or low bioactivity of IGF-1 is an important risk factor for atherosclerotic burden and a negative determinant of survival.
LIFE SPAN, ATHEROSCLEROSIS, AND IGF-1 IN EXPERIMENTAL ANIMAL MODELS
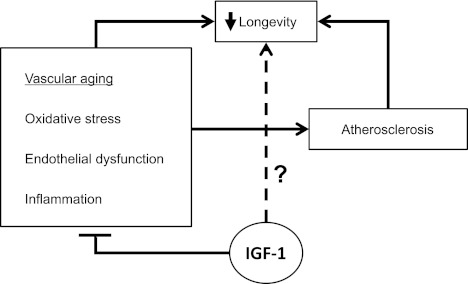
As discussed above, there is evidence that reduced bioavailability of IGF-1 predisposes to development of atherosclerosis, whereas low bioactivity of IGF-1 appears to promote longevity. Considering that atherosclerotic heart disease remains the leading cause of death in the United States, these observations may appear contradictory (Figure 2). However, interpretation of data from cross-sectional studies establishes associations and not causality, and similarly, case-control studies can be confounded by unanticipated factors, for example, identifying appropriate control subjects can be complicated when making a comparison to a group of interest with extreme conditions such as centenarians. Experimental animal models have been useful to study links between aging, IGF-1, and atherosclerosis. Caloric restriction has provided insights into the relation between aging and IGF-1 action. In every reported organism, including yeast, nematode, drosophila, mouse, and rhesus monkey, a reduction in food intake without malnutrition extends life span or delays biological aging and age-related disease onset substantially (for review, see (73)). Because a reduction in food intake decreases signaling activity and/or bioavailability of insulin and IGF-1 (or corresponding orthologs), it has been speculated that diminished insulin and IGF-1 signaling can contribute to longevity. This hypothesis is supported by the reported association between a centenarian age and mutations in the IGF-1R gene, which result in reduced IGF-1 signaling (72). The premise is also supported by experiments performed in genetically altered models in yeast, nematode, drosophila, and mouse, in which targeting of corresponding orthologs of insulin/IGF-1 effectively elongates life span. For instance, it has been shown that mice with inactivated IGF-1R live on average 26% longer than their wild-type littermates, and these IGF-1R-deficient mice display greater resistance to oxidative stress, a known determinant of ageing (74). However, the causal role of decreased IGF-1 signaling in caloric restriction-induced extension of murine life span is uncertain. A recent case control study in individuals with a GH receptor deficiency (thus a severe IGF-1 deficiency) did not confirm the life extending effect of low IGF-1 availability (75). And in an animal model of GH deficiency, caloric restriction and GH/IGF-1 deficiency has been shown to additively increase life span, suggesting their independent effects (76,77).
Figure 2.
Paradoxical effects of insulin-like growth factor (IGF)-1 on atherogenesis and the aging process. IGF-1 blunts multiple processes (in box, left) that are relevant to atherosclerosis development and to vascular aging. However, whereas evidence suggests that reduced IGF-1 promotes atherosclerosis and an increase in IGF-1 is antiatherogenic, paradoxically, IGF-1 deficiency has been linked to increased longevity (dotted line), although a final proof is still awaited.
Unfortunately, the above animal models are not relevant to study vascular complications of atherosclerosis; in fact, in none of these organisms is atherosclerotic disease a major cause of termination of life. In the rhesus monkey, valvular endocardiosis, cardiomyopathy, and myocardial fibrosis have been observed at necropsy; however, there is little evidence of atherothrombotic vascular disease (78).
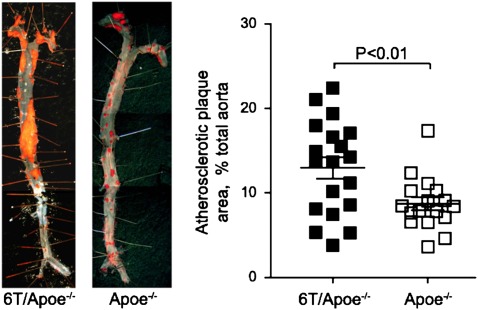
Several animal models have been exploited to investigate the pathophysiology of atherosclerosis. Localized arterial injury models have been primarily used to study the restenotic process. These models attempt to mimic the vascular repair responses to angioplasty, but several important differences must be recognized; for instance, the injury is in general to nondiseased vessels with no preexisting neointimal cell populations, and thus, responses derive predominantly from proliferating VSMCs. Because IGF-1 is a potent VSMC mitogen, the majority of studies exploring mechanical injury models and direct (79,80) or indirect (81–84) mechanisms to alter vascular IGF-1 signaling reported that increased IGF-1 or IGF-1 signaling correlates with increased neointimal burden, suggesting that IGF-1 promotes vascular hyperplasia. In particular, targeted overexpression of IGF-1 in VSMCs increases neointimal area size (80). Leukocyte antigen related protein-tyrosine phosphatase (LAR) physically associates with IGF-1R and diminishes its signaling activity by dephosphorylating IGF-1R. Deletion of the leukocyte antigen related protein-tyrosine phosphatase gene increased neointima size in a mechanical injury model, consistent with a positive effect of IGF-1 on VSMC migration and proliferation (85). Other animal models used to investigate atherosclerosis include genetic hyperlipidemia models such as apolipoprotein E deficient (Apoe−/−) and low density lipoprotein (LDL) receptor (Ldlr)-deficient mice. A high fat diet, commonly called a Western diet, is often supplied to these animals to produce even more pronounced hyperlipidemia, thus accelerating atherogenesis. These hyperlipidemic animals develop atherosclerotic lesions that parallel those of human subjects, characterized by lesion development at vascular branch points and progression from a foam cell stage to a fibroproliferative stage with well-defined fibrous caps and necrotic lipid cores (86). However, there are significant differences between human and mouse lesions at advanced stages, and caution should be taken when extrapolating observations in these animal models to humans, particularly with respect to acute events associated with plaque vulnerability (interested readers are referred to recent reviews discussing the usefulness and limitations of various mouse atherosclerosis models (87,88)). Notwithstanding these limitations, their reproducibility and extensively characterized phenotype make these genetically modified animal models an important tool to study mechanisms of atherosclerosis. It is noteworthy that Apoe−/− mice have reduced life span likely because of advanced coronary atherosclerotic disease (89). To date, few studies have evaluated IGF-1 effects on atherosclerosis using Apoe−/− mice. Harrington and colleagues (81) created double-knockout mice deficient in Apoe and pregnancy-associated plasma protein-A (Pappa), a metalloproteinase that degrades IGFBP-4. Pappa−/−/Apoe−/− mice fed a Western diet had decreased lesion size, and this correlated with reduced expression of IGFBP-5, which is positively regulated by IGF-1 (90–92). Because Pappa deficiency increases IGFBP-4 levels, thereby reducing IGF-1 bioavailability, these data suggest potential proatherogenic effects of PAPPA mediated by IGF-1. However, direct effects of PAPPA on atherosclerosis cannot be excluded. Our group investigated the effect of IGF-1 in atherosclerosis by infusing human recombinant IGF-1 into Apoe−/− mice fed a Western diet. Our study protocol provided an approximately twofold increase in total serum IGF-1 levels, which was associated with enhanced IGF-1 signaling activity, confirmed by elevation in tissue Akt phosphorylation (6). We did not measure free IGF-1, thought to be the fraction of serum IGF-1 immediately available for binding to its receptor (reviewed in (93)). Therefore, the increase of free IGF-1 in this model might be higher than the twofold increase in total IGF-1 measured. IGF-1 infusion for 12 weeks was associated with reduced atherosclerotic lesion size. This effect was accompanied by a significant reduction in urinary excretion of 8-isoprostane, a systemic index of oxidative stress. Other potential beneficial effects included a decrease in lesion macrophage infiltration, reduced aortic expression of proinflammatory cytokines and increased levels of circulating endothelial progenitor cells. IGF-1-infused animals had decreased vascular superoxide levels, upregulated expression of vascular endothelial nitric oxide synthase (eNOS) and increased nitric oxide (NO) bioavailability. IGF-1–infused animals also had reduced oxidative stress localized specifically in atherosclerotic plaque (94). Interestingly, the IGF-1–induced antioxidant effect was significantly reduced by administration of Nω-Nitro-L-arginine methyl ester, a pan-nitric oxide synthase inhibitor, indicating that this effect was dependent on NO bioavailability. However, infusion of Apoe−/− mice with GH releasing peptide-2, a synthetic peptide that increases circulating GH and IGF-I levels, did not reduce atherosclerotic burden despite a significant increase in serum IGF-1 levels associated with decreased reactive oxygen species (ROS) in the vasculature (95). The increased GH levels present in response to GH releasing peptide-2 might explain the discrepancy between the apparent beneficial effect observed in the IGF-1 infusion model and the lack of effectiveness in the GH releasing peptide-2 infusion model (96). Our findings suggest that the potential antiatherogenic effect of IGF-1 is closely associated with reduced oxidative stress in the vasculature, although it is important to note that Nω-Nitro-L-arginine methyl ester did not block the anti-atherosclerotic effect of IGF-1 (94). It has been suggested that an imbalance in redox regulation is associated with aging, leading to elevated vascular oxidative stress which predisposes to atherogenesis (97–99); thus, the antioxidant effect of IGF-1 could represent an antiaging mechanism that contributes to prevention of atherosclerosis. Additionally, we recently found that an ∼20% reduction in circulating IGF-1 levels was accompanied by a significant increase in aortic lesion size in Apoe−/− mice (Figure 3; (100)). It is well known that levels of circulating IGF-1 decline with aging (101–104). Therefore, our model of reduced bioavailabiity of IGF-1 in Apoe−/− mice mimics the loss of IGF-1 bioavailability that occurs with aging and supports the notion that low IGF-1 bioavailability exacerbates atherosclerosis. Although these observations in Apoe−/− mice with enhanced and diminished IGF-1 bioavailability are consistent with atheroprotective effects of IGF-1, further investigation is required to characterize the underlying mechanisms.
Figure 3.
Low circulating insulin-like growth factor (IGF)-1 increases atherosclerosis in Apoe-/- mice. We generated atherosclerosis-prone apolipoprotein E-deficient (Apoe-/-) mice with 6T alleles (6T/Apoe-/-) with a 20% decline in circulating IGF-I. After 12 weeks of high-fat diet feeding, 6T/Apoe-/- mice developed significantly more atherosclerosis. Left: Representative images of en face Oil Red O staining of aorta. Right: Atheroma covered area on en face aorta was expressed as % total luminal surface area. This figure is modified from; Shai S et al. Am J Physiol Heart Circ Physiol 2011; 300:H1898–H1906.
The vascular effects of alterations in circulating IGF-1 represent endocrine effects. To address effects of locally produced IGF-1 on atherosclerosis, transgenic mice which overexpress IGF-1 in smooth muscle were created on an Apoe−/− background (Apoe−/−-Tg(SMP8-Igf1)) (105). When compared with Apoe−/− mice, the Apoe−/−-Tg(SMP8-Igf1) mice developed a comparable plaque burden after 12 weeks on a Western diet, suggesting that the ability of increased circulating IGF-1 to reduce plaque burden (6) was mediated in large part via non-VSMC target cells. However, advanced plaques in Apoe−/−-Tg(SMP8-Igf1) mice displayed several features of increased plaque stability, including elevated α-smooth muscle actin positive VSMC content, increased fibrous cap area, increased collagen levels, and reduced necrotic cores (105). It is unclear if local production of IGF-1 in the vasculature declines with aging, as has been described for circulating IGF-1; furthermore, it is unknown if aging impairs IGF-1R activation in VSMCs as it does in skeletal muscle (106,107) and osteoblasts (108). If this were the case, loss of responsiveness to IGF-1 in VSMCs could contribute to the increased prevalence of atherothrombotic diseases in aged subjects.
MECHANISMS FOR ATHEROPROTECTIVE EFFECTS OF IGF-1
IGF-1 AND INFLAMMATION
An increase in inflammation is associated with aging in general and with vascular aging (109) and contributes to the development of several aging-associated syndromes such as sarcopenia (reduction in skeletal muscle mass and development of muscle weakness (110,111)). Furthermore, sarcopenia progression correlates with suppression of IGF-1 signaling in skeletal muscle (112). Inflammatory cells have a predominant role in the pathogenesis of atherosclerosis (113). At an early stage of atherogenesis, phagocytic cells such as monocytes/macrophages are recruited and infiltrate into a fatty streak, scavenging accumulated LDLs which have been denatured or modified (eg, aggregated or oxidized) locally in the tissue. Modified LDL binding to cell surface receptors and subsequent internalization induces a variety of proinflammatory responses in these cells, triggering feed-forward reactions to promote atherosclerosis (113). Inflammatory responses and oxidative stress are closely related; for instance, in monocytes/macrophages it has been shown that reactive oxygen species enhance proinflammatory cytokine production through modulating Nuclear factor-κB activity (114). At the tissue level, activated inflammatory cells express high-level of oxidant-generating enzymes, such as myeloperoxidase, NADPH oxidase, and 12/15-lipoxygenase (LOX), causing oxidative damage to surrounding tissue, further inducing inflammatory responses. Several reports suggest that IGF-1 is antiinflammatory. For instance, there is an inverse relation between serum interleukin-6 and IGF-1 levels (115), and IGF-1/IGFBP-3 administration to patients with severe burn injury induced an anti-inflammatory effect and reduced interleukin -6 and tumor necrosis factor (TNF)-α (116,117). Furthermore, low IGF-1 and high interleukin -6 and TNF-α levels are associated with higher mortality in elderly patients (51,118). Consistent with these clinical observations, data from our group show that IGF-1 modulates macrophage function. This could represent a key mechanism mediating the anti-inflammatory and antiatherogenic effects of IGF-1 in the vasculature. Indeed, human recombinant IGF-1 infusion into Apoe−/− mice markedly suppressed macrophage infiltration into atherosclerotic lesions by a mechanism that is not yet elucidated but is associated with downregulation of TNF-α expression (6). In human subjects with GH deficiency, low serum IGF-1 levels are associated with increased lipoprotein lipase and TNF-α expression in macrophages (119). Intriguingly, macrophages from these subjects are more susceptible to foam cell formation in vitro; in fact, uptake of oxidized LDL (OxLDL) was enhanced in these cells (119), consistent with the known ability of lipoprotein lipase to facilitate binding and uptake of modified LDL. IGF-1 reduces aortic lipoprotein lipase mRNA levels in Apoe−/− mice and also in cultured macrophages (94). These observations in animal models and human subjects support an anti-inflammatory and thus potentially antioxidant effect of IGF-1, which could contribute to atheroprotection. However, other reports suggest that IGF-1 has proinflammatory effects. For instance, in monocytes/macrophages, IGF-1 enhanced chemotactic macrophage migration (33), stimulated TNF-α expression (33), and enhanced LDL uptake and cholesterol esterification (120). Moreover, proatherogenic factors such as advanced glycosylation end products (121) and TNF-α (122) increase IGF-1 synthesis. Some of these effects of IGF-1 on macrophages might not necessarily be proatherogenic; for instance, IGF-1-mediated stimulation of cellular uptake of LDL could contribute to reducing plasma LDL cholesterol levels (120). Additional studies are required to clarify the action of IGF-1 on inflammatory processes in atherosclerosis.
IGF-1 and Vascular Smooth Muscle Cells
Moderate oxidative stress stimulates IGF-1 (123) and IGF-1R (124) expression in VSMC. In fact, IGF-1R tyrosine kinase activity mediates hydrogen peroxide activation of mitogen-activated protein kinase (125) and Akt (126). In addition, IGF-1 itself moderately elevates ROS generation in VSMC (127), suggesting that IGF-1 amplifies its activity through ROS generation. ROS can enhance insulin signaling by inhibiting protein tyrosine phosphatase activity (128). Considering the substantial similarity between IGF-1 and insulin signaling pathways, it is possible that ROS similarly enhance IGF-1 signaling. These reports support the hypothesis that moderate oxidative stress and IGF-1 coordinately promote VSMC growth and hence atherosclerosis, especially at the initial stage of lesion formation when VSMC migration and proliferation predominate. On the other hand, it is also known that elevated ROS inhibit insulin/IGF-1 signaling (129–131) and induce apoptotic cell death (132). It is likely that the balance between ROS elevation and the activity of antioxidant systems (eg, enzymes such as glutathione peroxidase), and presumably a specific location of ROS generation (eg, plasma membrane vs mitochondrion), will determine the dominant downstream vascular effects of oxidant stress. In advanced atherosclerotic plaques, a balance between cell death and survival of cells within the fibrous cap, primarily composed of VSMC and extracellular matrix, appears to correlate with plaque instability or stability (133). Moreover, VSMC apoptosis itself can accelerate atherosclerosis (134), and this mechanism is important for the transition from early to advanced plaques. VSMC apoptosis is controlled by growth factors and cytokines, including IGF-1. A key proatherogenic molecule, OxLDL, colocalizes with apoptotic VSMC in human atherosclerotic plaques, and these cells have reduced IGF-1 and IGF1-R levels (135–137). A reduced expression of IGF-1, along with downregulation of IGF-2 and IGFBP-3, -4, -5, and -6 and intriguingly upregulation of IGFBP-1, was also demonstrated in human carotid plaques (138). Consistent with these findings, OxLDL reduces IGF-1R levels (135,136) and induces apoptosis of cultured VSMC through a redox-sensitive mechanism that includes activation of two major oxidases, LOX and NADPH oxidase. Pharmacological suppression of 5-LOX and 12/15-LOX activities abolishes OxLDL-induced VSMC apoptosis (139). Interestingly, 12-hydroxyeicosatetraenoic acid, a 12/15-LOX product, upregulates TNF-α expression and inhibits Akt phosphorylation in cultured adipocytes (140), and LOX inhibitors prevent apoptosis-inducing factor mediated cell death (141). IGF-1 is a potent survival factor for VSMC, and increased IGF-1 signaling prevents OxLDL-induced VSMC apoptosis via a phosphoinositide 3 kinase (PI3K)/Akt-dependent pathway (142). IGF-1 reduced total apoptotic cell number specifically in atherosclerotic plaque in Apoe−/− mice, and interestingly, IGF-1 had no effect on plaque SMC cell apoptosis indicating that the antiapoptotic effect of IGF-1 was exerted on non-SMC plaque cells (94). In addition to its antiapoptotic effects, IGF-1 also suppresses autophagic cell death of plaque-derived VSMC via Akt-dependent inhibition of microtubule-associated 1 light chain-3 expression (143).
It has recently been reported that smooth muscle specific IGF-1 overexpression in Apoe−/− mice (Apoe−/−-Tg(SMP8-Igf1)) (105) changes atherosclerotic lesion phenotype, resulting in elevated α-smooth muscle actin positive VSMC content, increased fibrous cap area and collagen levels, and reduced necrotic cores (105). Whereas a reduction in apoptotic cell death of VSMC was not confirmed, apparently locally produced IGF-1 promoted VSMC differentiation and matrix deposition, which has also been suggested in studies of cultured VSMCs (105,144,145). These autocrine/paracrine effects of IGF-1 could potentially stabilize plaques, thereby reducing the prevalence of atherothrombotic vascular disease.
IGF-1 AND ENDOTHELIAL DYSFUNCTION, VASCULAR TONE REGULATION
NO Availability, Oxidative Stress and IGF-1
Endothelial dysfunction is implicated in the pathogenesis of cardiovascular diseases including atherosclerosis (146). Aging is associated with endothelial dysfunction (147–150) and increased oxidative stress (148,150), implying a potential causal link between aging, oxidative stress, and endothelial dysfunction. NO plays a crucial role in endothelial function because of its potent vasodilator effect and sensitivity to the redox status of the endothelium. In the setting of high oxidative stress NO reacts with ROS, particularly superoxides, forming peroxynitrite, which is highly reactive and thus potentially highly deleterious. The ability of peroxynitrite to nitrate protein tyrosine residues can alter several cellular pathways that involve tyrosine phosphorylation, such as protein kinase C, Akt, the MAP kinases, nuclear factor kB, as well as signaling in response to IGF-1/insulin and the sympathoadrenergic system. Thus, increasing ROS production causes not only perturbations in vasodilation by decomposing NO but also potentially inhibits several signaling pathways that are crucial for maintaining normal endothelial function. Oxidative stress also lowers NO bioavailability by blocking its production. eNOS is the main enzymatic source that produces NO constitutively and in response to vasodilators such as acetylcholine. eNOS catalyzes L-arginine oxidation to produce L-citrulline and NO by transferring electrons provided from NADPH and tetrahydrobiopterin (BH4). BH4, an essential cofactor of eNOS activity, is susceptible to oxidative modification by ROS such as peroxynitrite, which results in conversion of BH4 to biologically inactive BH2. An additional mechanism for BH4 depletion caused by oxidative stress was described by Zheng and colleagues (151), who found that an increase in ROS leads to downregulation of guanosine 5′-triphosphate cyclohydrolase I, which is a rate-limiting enzyme catalyzing the initial step of BH4 biosynthesis. Insufficient availability of BH4 causes “uncoupling” of eNOS activity, resulting in superoxide and hydrogen peroxide formation instead of NO. Thus there is probably a feed-forward system for lowering NO bioavailability, once enhanced oxidative stress occurs.
There is increasing evidence that IGF-1 can preserve endothelial function. GH deficiency impairs flow-mediated arterial dilation, and thus endothelial NO-dependent vasodilation (152), and increases cardiovascular morbidity and mortality (153). Because GH is a primary regulator of circulating IGF-1 and GH deficiency leads to low IGF-1, it is reasonable to speculate that IGF-1 plays a major role in vasodilatory responses by regulating NO production in the endothelium. This hypothesis is supported by a recent publication showing that low plasma IGF-1 levels are associated with impaired endothelium dependent vasodilation (154). In patients with diabetes, vascular tone regulation is impaired, and IGF-1 supplementation improves vascular responses to vasodilators, potentially by enhancing eNOS activity (155,156). These observations in humans are supported by animal and cell culture studies. For example, in mice fed a high-fat diet (an animal model of type 2 diabetes), IGF-1 resistance exists at the endothelial level, which in turn blunts eNOS dependent vasorelaxation (157). This finding is consistent with a positive effect of IGF-1 on endothelium function. However, this model was characterized by increased serum IGF-1 levels (157), whereas patients with poorly controlled diabetes generally have low serum IGF-1 levels (158). In EC culture systems, IGF-1 acutely enhances eNOS-dependent NO production by increasing phosphorylation at Ser1177 via a PI3K and Akt pathway (159). In addition to acute effects of IGF-1 on eNOS activity, a link has been suggested between BH4 biosynthesis and IGF-1. One of the key enzymes involved in BH4 biosynthesis is 6-pyruvoyltetrahydropterin synthase; its deficiency in mice causes dwarfism with markedly reduced serum IGF-1 levels (160), suggesting that a functional BH4 biosynthetic pathway is essential for maintenance of IGF-1 levels and normal growth. By contrast, in pheochromocytoma-12 (PC12) cells, IGF-1 elevates BH4 levels, potentially by enhancing its biosynthesis through a PI3K-dependent mechanism (161). It would be interesting to determine if the potential IGF-1 effect on BH4 biosynthesis can be generalized to other tissues with NO synthase activity. In Apoe−/− mice fed a high-fat diet, we observed that IGF-1 infusion enhanced eNOS gene expression in the aorta (6). Recently, we demonstrated that IGF-1–induced atheroprotection does not depend on NO bioavailability (94). It is important to note that IGF-1–induced increase in plaque smooth muscle cells, suppression of cell apoptosis, and downregulation of lipoprotein lipase were also NO independent, suggesting a potential important role of these mechanisms in IGF-1–induced suppression of atherosclerosis. In GH-deficient rodent models (Ames dwarf mice and Lewis dwarf rats), GH and IGF-1 deficiency was accompanied by high oxidative stress in the vasculature, potentially leading to endothelial dysfunction (162,163). The high oxidative stress could be explained by reduced eNOS gene and protein expression in the aortas of Ames dwarf mice, in which acetylcholine-induced vasorelaxation was impaired. Their observation is consistent with a stimulatory role of GH/IGF-1 on eNOS expression and function; moreover, GH and IGF-1 enhanced expression of antioxidant enzymes such as Mn-superoxide dismutase, Cu/Zn-superoxide dismutase, and glutathione peroxidase-1 in aortae of the Ames dwarf mice and in explants of mouse aorta and human coronary arterial ECs (162,163), suggesting that GH and/or IGF-1 have antioxidant effects that are independent of eNOS. The role of IGF-1 in regulating endothelial function is supported by recent reports that deficiency of GH and IGF-1 exacerbates high-fat diet–induced endothelial impairment (164) and that systemic IGF-1 deficiency in mice decreases vascular oxidative stress resistance by impairing the Nuclear factor erythroid 2-like 2–dependent antioxidant response (165). Nuclear factor erythroid 2-like 2 is a transcription activator that binds to antioxidant response elements in the promoter regions of target genes; hence, it is important for the coordinated upregulation of genes in response to oxidative stress. Therefore, Nuclear factor erythroid 2-like 2 could be a key molecule linking IGF-1 signaling to its antioxidant effects and prevention of endothelial dysfunction. Intriguingly, increased incidence of intracranial hemorrhage was reported in the Lewis dwarf rats (166), implying a pivotal role of GH/IGF-1 in maintaining vascular integrity potentially mediated by antioxidant effects. Abbas and colleagues (167) took a different approach to investigate IGF-1 effects on endothelial function by creating mice with whole-body haploinsufficiency of IGF-1R and endothelium specific holo- and haploinsufficiency of IGF-1R. They found that haploinsufficiency of IGF-1R both at the whole-body level and in endothelium led to enhanced endothelial function, as assessed by reduced vasoconstriction to phenylephrine, increased basal NO production, and increased EC insulin sensitivity leading to augmented insulin-mediated NO generation. They conclude that IGF-1R, via its ability to form hybrids with the insulin receptor, is a negative regulator of insulin signaling in endothelium. In fact, they demonstrated that in an insulin-resistance mice model (whole-body insulin receptor haploinsufficiency model), the introduction of IGF-1R haploinsufficiency restored insulin-mediated NO production, basically by changing IGF-1R: insulin receptor stoichiometry. Therefore, whether IGF-1 (or IGF-1R) augments or diminishes endothelial function might be substantially affected by physiological settings (eg, presence of insulin resistance). Further clarification of IGF-1 effects on the endothelium is necessary.
IGF-1 and Hypertension
Hypertension is a major risk factor for atherosclerosis, and aging influences the prevalence of hypertension, whereas aging by itself appears insufficient to induce hypertension (168,169). As described above, IGF-1 increases endothelial NO production; hence, a major part of IGF-1 effects on vascular tone regulation can be attributed to eNOS–NO dependent mechanisms. In addition, insulin/IGF-1 reduces [Ca2+]i and Ca2+-MLC sensitivity in VSMC (170,171), thereby inducing vascular relaxation. In human subjects, it has been shown that there is an inverse association between free IGF-1 and isovolumic relaxation in arterial systemic hypertension (172), and IGF-1 levels in the low normal range are associated with hypertension in subjects without pituitary and cardiovascular diseases (173). Moreover peripheral resistance and systolic blood pressure were increased in liver-specific IGF-1 knockout mice (174), and IGF-1–induced vasorelaxant effects were impaired before the onset of hypertension in spontaneously hypertensive rats (175,176). Collectively, these observations point to a pathophysiological role of IGF-1 in the development of hypertension. The powerful vasoconstrictor, endothelin-1, has also been suggested as a potential link between IGF-1 and vascular tone regulation. IGF-1 attenuates endothelin-1–induced contractile responses in porcine aorta, potentially by altering endothelin-1/endothelin receptor type A signaling activity in smooth muscle cells (177). IGF-1 might directly or indirectly regulate endothelin-1 gene expression; for example, in liver specific IGF-1-deficient mice, endothelin-1 gene expression was upregulated in the aorta, and this was associated with elevated systolic blood pressure and impaired vasorelaxation (174). IGF-1 enhancement of NO bioavailability could explain the ability of IGF-1 to antagonize endothelin-1 contractile responses; endothelin-1 increases vascular superoxide by enhancing NADPH-oxidase activity and thus lowers NO bioavailability (178–180), suggesting that endothelin-1–induced endothelial dysfunction is at least partly mediated by increased oxidative stress. Interestingly, insulin and IGF-1 upregulate endothelin-1/endothelin receptor type A levels in VSMCs (181,182), indicating a complex interaction between insulin/IGF-1 and endothelin effects.
IGF-1 AND ENDOTHELIAL REPAIR
Endothelial progenitor cells (EPCs) derived from bone marrow and/or the vascular wall contribute to neovascularization in response to ischemia (183), and their levels are related to cardiovascular disease outcome (184). EPCs promote endothelial repair directly by differentiation and integration into a newly formed endothelial layer or indirectly by producing a variety of proangiogenic cytokines and growth factors, promoting proliferation and migration of preexisting ECs (185), thereby preventing endothelial dysfunction (186,187). Interestingly, factors that positively or negatively alter endothelial function also affect EPC function. eNOS, which is crucial for maintenance of endothelial function, is also involved in mobilization of EPCs from bone marrow (188), and eNOS uncoupling impairs EPC mobilization and function (189). Intrinsic high expression of antioxidant enzymes has been reported in EPCs (190,191), suggesting that they are resistant to oxidative stress. However, there are conflicting reports on the effects of ROS on EPC function in neovascularization induced by hind limb ischemia (192–194). Perhaps appropriate levels of ROS, that is, “fine tuning” of the level of oxidative stress, is essential for EPC integrity. In the context of aging, it has been shown that aging reduces EPC availability and impairs EPC function, including homing, proliferation, and migration (195). More importantly, it has been shown in human subjects that an increase in circulating IGF-1 in response to GH or IGF-1 administration corrects age-dependent impairment of endothelial progenitor cells. Thus GH or IGF-1 increased circulating EPC number and improved EPC colony forming and migratory capacity, enhanced incorporation into tube-like structures, and augmented eNOS expression (196,197). These findings provide direct evidence that IGF-1 exerts beneficial effects on aging associated impairment in endothelial repair mechanisms. Similar findings in an animal model of atherosclerosis (6) imply that IGF-1 influences EPC mobilization and function by altering NO bioavailability as it does in mature ECs. However, there are many remaining questions about potential IGF-1 effects on EPC, and these are complicated by the continuing debate about the definition of EPC (198). For instance, potential IGF-1 regulation of specific EPC niches in the bone marrow and vascular wall (199) and of EPC mobilization and homing remains to be determined.
CONCLUSION AND FUTURE DIRECTIONS
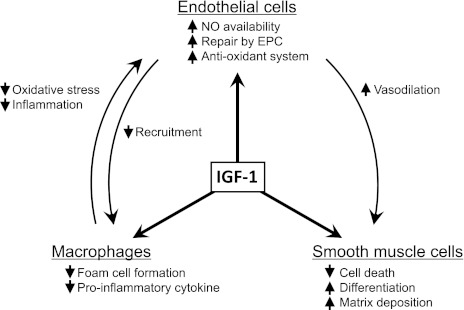
There is increasing evidence that IGF-1 exerts pleiotropic effects on the vasculature resulting in reduced vascular oxidant stress, apoptosis, and inflammatory signaling (summarized in Figure 4). Furthermore, IGF-1 reduces atherosclerotic burden and increases atherosclerotic plaque stability in animal models. These findings suggest that IGF-1 may have salutary effects on the normal vascular aging process. However, there is some evidence that reduced IGF-1 and insulin signaling may favorably impact longevity. Further studies are required to dissect the role of IGF-1 in vascular aging processes and to determine the relation between IGF-1 signaling and longevity. Defining cell–cell interactions between different cell populations (ie, EC, smooth muscle cell, and proinflammatory cells such as macrophage and T cell) will be key to dissecting the role of IGF-1 in both vascular aging and atherosclerosis. Furthermore, a better understanding of cellular–microenvironment interactions and the impact of these interactions on downstream IGF-1 signaling pathways will be critical to understand mechanisms.
Figure 4.
Effects of insulin-like growth factor (IGF)-1 on cell types involved in atherogenesis. IGF-1 exerts cell type specific effects and also alters cell–cell interactions, leading to a reduction in atherosclerosis and a more stable atherosclerotic plaque phenotype.
FUNDING
This work was supported by grants from the National Institutes of Health/National Heart, Lung, and Blood Institute R01HL070241 and R01HL080682 and National Institutes of Health/National Center for Research Resources 5 P20 RR018766-10 and National Institutes of Health/National Institute of General Medical Sciences 8 P20 GM103514-10.
Acknowledgments
None.
References
- 1.Witztum JL. The oxidation hypothesis of atherosclerosis. Lancet. 1994;344:793–795. doi: 10.1016/s0140-6736(94)92346-9. [DOI] [PubMed] [Google Scholar]
- 2.Finkel T, Holbrook NJ. Oxidants, oxidative stress and the biology of ageing. Nature. 2000;408:239–247. doi: 10.1038/35041687. [DOI] [PubMed] [Google Scholar]
- 3.Cercek B, Fishbein MC, Forrester JS, Helfant RH, Fagin JA. Induction of insulin-like growth factor I messenger RNA in rat aorta after balloon denudation. Circ Res. 1990;66:1755–1760. doi: 10.1161/01.res.66.6.1755. [DOI] [PubMed] [Google Scholar]
- 4.Hayry P, Myllarniemi M, Aavik E, et al. Stabile D-peptide analog of insulin-like growth factor-1 inhibits smooth muscle cell proliferation after carotid ballooning injury in the rat. FASEB J. 1995;9:1336–1344. doi: 10.1096/fasebj.9.13.7557024. [DOI] [PubMed] [Google Scholar]
- 5.Maile LA, Capps BE, Ling Y, Xi G, Clemmons DR. Hyperglycemia alters the responsiveness of smooth muscle cells to insulin-like growth factor-I. Endocrinology. 2007;148:2435–2443. doi: 10.1210/en.2006-1440. [DOI] [PubMed] [Google Scholar]
- 6.Sukhanov S, Higashi Y, Shai SY, Vaughn C, Mohler J, Li Y, et al. IGF-1 reduces inflammatory responses, suppresses oxidative stress, and decreases atherosclerosis progression in ApoE-deficient mice. Arterioscler Thromb Vasc Biol. 2007;27:2684–2690. doi: 10.1161/ATVBAHA.107.156257. [DOI] [PubMed] [Google Scholar]
- 7.Frutkin AD, Otsuka G, Stempien-Otero A, et al. TGF-[beta]1 limits plaque growth, stabilizes plaque structure, and prevents aortic dilation in apolipoprotein E-null mice. Arterioscler Thromb Vasc Biol. 2009;29:1251–1257. doi: 10.1161/ATVBAHA.109.186593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tang J, Kozaki K, Farr AG, et al. The absence of platelet-derived growth factor-B in circulating cells promotes immune and inflammatory responses in atherosclerosis-prone ApoE-/- mice. Am J Pathol. 2005;167:901–912. doi: 10.1016/S0002-9440(10)62061-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kozaki K, Kaminski WE, Tang J, et al. Blockade of platelet-derived growth factor or its receptors transiently delays but does not prevent fibrous cap formation in ApoE null mice. Am J Pathol. 2002;161:1395–1407. doi: 10.1016/S0002-9440(10)64415-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Raines EW, Ferri N. Thematic review series: the immune system and atherogenesis. Cytokines affecting endothelial and smooth muscle cells in vascular disease. J Lipid Res. 2005;46:1081–1092. doi: 10.1194/jlr.R500004-JLR200. [DOI] [PubMed] [Google Scholar]
- 11.LeRoith D, Werner H, Beitner-Johnson D, Roberts CT., Jr Molecular and cellular aspects of the insulin-like growth factor I receptor. Endocr Rev. 1995;16:143–163. doi: 10.1210/edrv-16-2-143. [DOI] [PubMed] [Google Scholar]
- 12.Jones JI, Clemmons DR. Insulin-like growth factors and their binding proteins: biological actions. Endocr Rev. 1995;16:3–34. doi: 10.1210/edrv-16-1-3. [DOI] [PubMed] [Google Scholar]
- 13.Delafontaine P. Insulin-like growth factor I and its binding proteins in the cardiovascular system. Cardiovasc Res. 1995;30:825–834. [PubMed] [Google Scholar]
- 14.Le Roith D. Seminars in medicine of the Beth Israel Deaconess Medical Center. Insulin-like growth factors. N Engl J Med. 1997;336:633–640. doi: 10.1056/NEJM199702273360907. [DOI] [PubMed] [Google Scholar]
- 15.Tsuruzoe K, Emkey R, Kriauciunas KM, Ueki K, Kahn CR. Insulin receptor substrate 3 (IRS-3) and IRS-4 impair IRS-1- and IRS-2-mediated signaling. Mol Cell Biol. 2001;21:26–38. doi: 10.1128/MCB.21.1.26-38.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saltiel AR, Kahn CR. Insulin signalling and the regulation of glucose and lipid metabolism. Nature. 2001;414:799–806. doi: 10.1038/414799a. [DOI] [PubMed] [Google Scholar]
- 17.Stewart CE, Rotwein P. Growth, differentiation, and survival: multiple physiological functions for insulin-like growth factors. Physiol Rev. 1996;76:1005–1026. doi: 10.1152/physrev.1996.76.4.1005. [DOI] [PubMed] [Google Scholar]
- 18.Bailyes EM, Nave BT, Soos MA, Orr SR, Hayward AC, Siddle K. Insulin receptor/IGF-I receptor hybrids are widely distributed in mammalian tissues: quantification of individual receptor species by selective immunoprecipitation and immunoblotting. Biochem J. 1997;327(Pt 1):209–215. doi: 10.1042/bj3270209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chisalita SI, Arnqvist HJ. Expression and function of receptors for insulin-like growth factor-I and insulin in human coronary artery smooth muscle cells. Diabetologia. 2005;48:2155–2161. doi: 10.1007/s00125-005-1890-4. [DOI] [PubMed] [Google Scholar]
- 20.Higashi Y, Holder K, Delafontaine P. Thiazolidinediones up-regulate insulin-like growth factor-1 receptor via a peroxisome proliferator-activated receptor gamma-independent pathway. J Biol Chem. 2010;285:36361–36368. doi: 10.1074/jbc.M110.137661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Engberding N, San Martin A, Martin-Garrido A, et al. Insulin-like growth factor-1 receptor expression masks the antiinflammatory and glucose uptake capacity of insulin in vascular smooth muscle cells. Arterioscler Thromb Vasc Biol. 2009;29:408–415. doi: 10.1161/ATVBAHA.108.181727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chisalita SI, Arnqvist HJ. Insulin-like growth factor I receptors are more abundant than insulin receptors in human micro- and macrovascular endothelial cells. Am J Physiol Endocrinol Metab. 2004;286:E896–E901. doi: 10.1152/ajpendo.00327.2003. [DOI] [PubMed] [Google Scholar]
- 23.Li G, Barrett EJ, Wang H, Chai W, Liu Z. Insulin at physiological concentrations selectively activates insulin but not insulin-like growth factor I (IGF-I) or insulin/IGF-I hybrid receptors in endothelial cells. Endocrinology. 2005;146:4690–4696. doi: 10.1210/en.2005-0505. [DOI] [PubMed] [Google Scholar]
- 24.Schneider MR, Lahm H, Wu M, Hoeflich A, Wolf E. Transgenic mouse models for studying the functions of insulin-like growth factor-binding proteins. FASEB J. 2000;14:629–640. doi: 10.1096/fasebj.14.5.629. [DOI] [PubMed] [Google Scholar]
- 25.Sakai K, Busby WH, Jr, Clarke JB, Clemmons DR. Tissue transglutaminase facilitates the polymerization of insulin-like growth factor-binding protein-1 (IGFBP-1) and leads to loss of IGFBP-1's ability to inhibit insulin-like growth factor-I-stimulated protein synthesis. J Biol Chem. 2001;276:8740–8745. doi: 10.1074/jbc.M008359200. [DOI] [PubMed] [Google Scholar]
- 26.Jones JI, Gockerman A, Busby WH, Jr, Wright G, Clemmons DR. Insulin-like growth factor binding protein 1 stimulates cell migration and binds to the alpha 5 beta 1 integrin by means of its Arg-Gly-Asp sequence. Proc Natl Acad Sci U S A. 1993;90:10553–10557. doi: 10.1073/pnas.90.22.10553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sisci D, Surmacz E. Crosstalk between IGF signaling and steroid hormone receptors in breast cancer. Curr Pharm Des. 2007;13:705–717. doi: 10.2174/138161207780249182. [DOI] [PubMed] [Google Scholar]
- 28.Tao Y, Pinzi V, Bourhis J, Deutsch E. Mechanisms of disease: signaling of the insulin-like growth factor 1 receptor pathway—therapeutic perspectives in cancer. Nat Clin Pract Oncol. 2007;4:591–602. doi: 10.1038/ncponc0934. [DOI] [PubMed] [Google Scholar]
- 29.Bayes-Genis A, Conover CA, Schwartz RS. The insulin-like growth factor axis: a review of atherosclerosis and restenosis. Circ Res. 2000;86:125–130. doi: 10.1161/01.res.86.2.125. [DOI] [PubMed] [Google Scholar]
- 30.Conti E, Carrozza C, Capoluongo E, et al. Insulin-like growth factor-1 as a vascular protective factor. Circulation. 2004;110:2260–2265. doi: 10.1161/01.CIR.0000144309.87183.FB. [DOI] [PubMed] [Google Scholar]
- 31.Delafontaine P, Song YH, Li Y. Expression, regulation, and function of IGF-1, IGF-1R, and IGF-1 binding proteins in blood vessels. Arterioscler Thromb Vasc Biol. 2004;24:435–444. doi: 10.1161/01.ATV.0000105902.89459.09. [DOI] [PubMed] [Google Scholar]
- 32.Arnqvist HJ. The role of IGF-system in vascular insulin resistance. Horm Metab Res. 2008;40:588–592. doi: 10.1055/s-0028-1082325. [DOI] [PubMed] [Google Scholar]
- 33.Renier G, Clement I, Desfaits AC, Lambert A. Direct stimulatory effect of insulin-like growth factor-I on monocyte and macrophage tumor necrosis factor-alpha production. Endocrinology. 1996;137:4611–4618. doi: 10.1210/endo.137.11.8895324. [DOI] [PubMed] [Google Scholar]
- 34.Che W, Lerner-Marmarosh N, Huang Q, et al. Insulin-like growth factor-1 enhances inflammatory responses in endothelial cells: role of Gab1 and MEKK3 in TNF-alpha-induced c-Jun and NF-kappaB activation and adhesion molecule expression. Circ Res. 2002;90:1222–1230. doi: 10.1161/01.res.0000021127.83364.7d. [DOI] [PubMed] [Google Scholar]
- 35.Li G, Barrett EJ, Ko SH, Cao W, Liu Z. Insulin and insulin-like growth factor-I receptors differentially mediate insulin-stimulated adhesion molecule production by endothelial cells. Endocrinology. 2009;150:3475–3482. doi: 10.1210/en.2009-0172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Libby P, Sasiela W. Plaque stabilization: Can we turn theory into evidence? Am J Cardiol. 2006;98:26P–33P. doi: 10.1016/j.amjcard.2006.09.017. [DOI] [PubMed] [Google Scholar]
- 37.Andreassen M, Raymond I, Kistorp C, Hildebrandt P, Faber J, Kristensen LO. IGF1 as predictor of all cause mortality and cardiovascular disease in an elderly population. Eur J Endocrinol. 2009;160:25–31. doi: 10.1530/EJE-08-0452. [DOI] [PubMed] [Google Scholar]
- 38.Boquist S, Ruotolo G, Skoglund-Andersson C, et al. Correlation of serum IGF-I and IGFBP-1 and -3 to cardiovascular risk indicators and early carotid atherosclerosis in healthy middle-aged men. Clin Endocrinol (Oxf) 2008;68:51–58. doi: 10.1111/j.1365-2265.2007.02998.x. [DOI] [PubMed] [Google Scholar]
- 39.Botker HE, Skjaerbaek C, Eriksen UH, Schmitz O, Orskov H. Insulin-like growth factor-I, insulin, and angina pectoris secondary to coronary atherosclerosis, vasospasm, and syndrome X. Am J Cardiol. 1997;79:961–963. doi: 10.1016/s0002-9149(97)00021-0. [DOI] [PubMed] [Google Scholar]
- 40.Fischer F, Schulte H, Mohan S, et al. Associations of insulin-like growth factors, insulin-like growth factor binding proteins and acid-labile subunit with coronary heart disease. Clin Endocrinol (Oxf) 2004;61:595–602. doi: 10.1111/j.1365-2265.2004.02136.x. [DOI] [PubMed] [Google Scholar]
- 41.Kawachi S, Takeda N, Sasaki A, et al. Circulating insulin-like growth factor-1 and insulin-like growth factor binding protein-3 are associated with early carotid atherosclerosis. Arterioscler Thromb Vasc Biol. 2005;25:617–621. doi: 10.1161/01.ATV.0000154486.03017.35. [DOI] [PubMed] [Google Scholar]
- 42.Ruotolo G, Bavenholm P, Brismar K, et al. Serum insulin-like growth factor-I level is independently associated with coronary artery disease progression in young male survivors of myocardial infarction: beneficial effects of bezafibrate treatment. J Am Coll Cardiol. 2000;35:647–654. doi: 10.1016/s0735-1097(99)00591-4. [DOI] [PubMed] [Google Scholar]
- 43.Schuler-Luttmann S, Monnig G, Enbergs A, et al. Insulin-like growth factor-binding protein-3 is associated with the presence and extent of coronary arteriosclerosis. Arterioscler Thromb Vasc Biol. 2000;20:E10–E15. [PubMed] [Google Scholar]
- 44.Conti E, Andreotti F, Sestito A, et al. Reduced levels of insulin-like growth factor-1 in patients with angina pectoris, positive exercise stress test, and angiographically normal epicardial coronary arteries. Am J Cardiol. 2002;89:973–975. doi: 10.1016/s0002-9149(02)02250-6. [DOI] [PubMed] [Google Scholar]
- 45.Friedrich N, Haring R, Nauck M, et al. Mortality and serum insulin-like growth factor (IGF)-I and IGF binding protein 3 concentrations. J Clin Endocrinol Metab. 2009;94:1732–1739. doi: 10.1210/jc.2008-2138. [DOI] [PubMed] [Google Scholar]
- 46.Goodman-Gruen D, Barrett-Connor E, Rosen C. IGF-1 and ischemic heart disease in older people. J Am Geriatr Soc. 2000;48:860–861. doi: 10.1111/j.1532-5415.2000.tb04774.x. [DOI] [PubMed] [Google Scholar]
- 47.Janssen JA, Stolk RP, Pols HA, Grobbee DE, de Jong FH, Lamberts SW. Serum free IGF-I, total IGF-I, IGFBP-1 and IGFBP-3 levels in an elderly population: relation to age and sex steroid levels. Clin Endocrinol (Oxf) 1998;48:471–478. doi: 10.1046/j.1365-2265.1998.00300.x. [DOI] [PubMed] [Google Scholar]
- 48.Juul A, Scheike T, Davidsen M, Gyllenborg J, Jorgensen T. Low serum insulin-like growth factor I is associated with increased risk of ischemic heart disease: a population-based case-control study. Circulation. 2002;106:939–944. doi: 10.1161/01.cir.0000027563.44593.cc. [DOI] [PubMed] [Google Scholar]
- 49.Laughlin GA, Barrett-Connor E, Criqui MH, Kritz-Silverstein D. The prospective association of serum insulin-like growth factor I (IGF-I) and IGF-binding protein-1 levels with all cause and cardiovascular disease mortality in older adults: the Rancho Bernardo Study. J Clin Endocrinol Metab. 2004;89:114–120. doi: 10.1210/jc.2003-030967. [DOI] [PubMed] [Google Scholar]
- 50.Martin RM, Gunnell D, Whitley E, et al. Associations of insulin-like growth factor (IGF)-I, IGF-II, IGF binding protein (IGFBP)-2 and IGFBP-3 with ultrasound measures of atherosclerosis and plaque stability in an older adult population. J Clin Endocrinol Metab. 2008;93:1331–1338. doi: 10.1210/jc.2007-2295. [DOI] [PubMed] [Google Scholar]
- 51.Roubenoff R, Parise H, Payette HA, et al. Cytokines, insulin-like growth factor 1, sarcopenia, and mortality in very old community-dwelling men and women: the Framingham Heart Study. Am J Med. 2003;115:429–435. doi: 10.1016/j.amjmed.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 52.Spallarossa P, Brunelli C, Minuto F, et al. Insulin-like growth factor-I and angiographically documented coronary artery disease. Am J Cardiol. 1996;77:200–202. doi: 10.1016/s0002-9149(96)90600-1. [DOI] [PubMed] [Google Scholar]
- 53.van den Beld AW, Bots ML, Janssen JA, Pols HA, Lamberts SW, Grobbee DE. Endogenous hormones and carotid atherosclerosis in elderly men. Am J Epidemiol. 2003;157:25–31. doi: 10.1093/aje/kwf160. [DOI] [PubMed] [Google Scholar]
- 54.Ruidavets JB, Luc G, Machez E, et al. Effects of insulin-like growth factor 1 in preventing acute coronary syndromes: the PRIME study. Atherosclerosis. 2011;218:464–469. doi: 10.1016/j.atherosclerosis.2011.05.034. [DOI] [PubMed] [Google Scholar]
- 55.Harrela M, Qiao Q, Koistinen R, et al. High serum insulin-like growth factor binding protein-1 is associated with increased cardiovascular mortality in elderly men. Horm Metab Res. 2002;34:144–149. doi: 10.1055/s-2002-23198. [DOI] [PubMed] [Google Scholar]
- 56.Kaplan RC, McGinn AP, Pollak MN, et al. Association of total insulin-like growth factor-I, insulin-like growth factor binding protein-1 (IGFBP-1), and IGFBP-3 levels with incident coronary events and ischemic stroke. J Clin Endocrinol Metab. 2007;92:1319–1325. doi: 10.1210/jc.2006-1631. [DOI] [PubMed] [Google Scholar]
- 57.Lawlor DA, Ebrahim S, Smith GD, Cherry L, Watt P, Sattar N. The association of insulin-like-growth factor 1 (IGF-1) with incident coronary heart disease in women: findings from the prospective British Women's Heart and Health Study. Atherosclerosis. 2008;201:198–204. doi: 10.1016/j.atherosclerosis.2007.12.061. [DOI] [PubMed] [Google Scholar]
- 58.Maggio M, Lauretani F, Ceda GP, et al. Relationship between low levels of anabolic hormones and 6-year mortality in older men: the aging in the Chianti Area (InCHIANTI) study. Arch Intern Med. 2007;167:2249–2254. doi: 10.1001/archinte.167.20.2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Saydah S, Graubard B, Ballard-Barbash R, Berrigan D. Insulin-like growth factors and subsequent risk of mortality in the United States. Am J Epidemiol. 2007;166:518–526. doi: 10.1093/aje/kwm124. [DOI] [PubMed] [Google Scholar]
- 60.Wallander M, Norhammar A, Malmberg K, Ohrvik J, Ryden L, Brismar K. IGF binding protein 1 predicts cardiovascular morbidity and mortality in patients with acute myocardial infarction and type 2 diabetes. Diabetes Care. 2007;30:2343–2348. doi: 10.2337/dc07-0825. [DOI] [PubMed] [Google Scholar]
- 61.Brugts MP, van den Beld AW, Hofland LJ, et al. Low circulating insulin-like growth factor I bioactivity in elderly men is associated with increased mortality. J Clin Endocrinol Metab. 2008;93:2515–2522. doi: 10.1210/jc.2007-1633. [DOI] [PubMed] [Google Scholar]
- 62.Janssen JA, Stolk RP, Pols HA, Grobbee DE, Lamberts SW. Serum total IGF-I, free IGF-I, and IGFB-1 levels in an elderly population: relation to cardiovascular risk factors and disease. Arterioscler Thromb Vasc Biol. 1998;18:277–282. doi: 10.1161/01.atv.18.2.277. [DOI] [PubMed] [Google Scholar]
- 63.Vaessen N, Heutink P, Janssen JA, et al. A polymorphism in the gene for IGF-I: functional properties and risk for type 2 diabetes and myocardial infarction. Diabetes. 2001;50:637–642. doi: 10.2337/diabetes.50.3.637. [DOI] [PubMed] [Google Scholar]
- 64.Bleumink GS, Schut AF, Sturkenboom MC, et al. A promoter polymorphism of the insulin-like growth factor-I gene is associated with left ventricular hypertrophy. Heart. 2005;91:239–240. doi: 10.1136/hrt.2003.019778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schut AF, Janssen JA, Deinum J, et al. Polymorphism in the promoter region of the insulin-like growth factor I gene is related to carotid intima-media thickness and aortic pulse wave velocity in subjects with hypertension. Stroke. 2003;34:1623–1627. doi: 10.1161/01.STR.0000076013.00240.B0. [DOI] [PubMed] [Google Scholar]
- 66.Yazdanpanah M, Rietveld I, Janssen JA, et al. An insulin-like growth factor-I promoter polymorphism is associated with increased mortality in subjects with myocardial infarction in an elderly Caucasian population. Am J Cardiol. 2006;97:1274–1276. doi: 10.1016/j.amjcard.2005.11.069. [DOI] [PubMed] [Google Scholar]
- 67.Yazdanpanah M, Sayed-Tabatabaei FA, Janssen JA, et al. IGF-I gene promoter polymorphism is a predictor of survival after myocardial infarction in patients with type 2 diabetes. Eur J Endocrinol. 2006;155:751–756. doi: 10.1530/eje.1.02276. [DOI] [PubMed] [Google Scholar]
- 68.Allen NE, Davey GK, Key TJ, Zhang S, Narod SA. Serum insulin-like growth factor I (IGF-I) concentration in men is not associated with the cytosine-adenosine repeat polymorphism of the IGF-I gene. Cancer Epidemiol Biomarkers Prev. 2002;11:319–320. [PubMed] [Google Scholar]
- 69.Frayling TM, Hattersley AT, McCarthy A, et al. A putative functional polymorphism in the IGF-I gene: association studies with type 2 diabetes, adult height, glucose tolerance, and fetal growth in U.K. populations. Diabetes. 2002;51:2313–2316. doi: 10.2337/diabetes.51.7.2313. [DOI] [PubMed] [Google Scholar]
- 70.Migliaccio E, Giorgio M, Mele S, et al. The p66shc adaptor protein controls oxidative stress response and life span in mammals. Nature. 1999;402:309–313. doi: 10.1038/46311. [DOI] [PubMed] [Google Scholar]
- 71.Selman C, Lingard S, Choudhury AI, et al. Evidence for lifespan extension and delayed age-related biomarkers in insulin receptor substrate 1 null mice. FASEB J. 2008;22:807–818. doi: 10.1096/fj.07-9261com. [DOI] [PubMed] [Google Scholar]
- 72.Suh Y, Atzmon G, Cho MO, et al. Functionally significant insulin-like growth factor I receptor mutations in centenarians. Proc Natl Acad Sci U S A. 2008;105:3438–3442. doi: 10.1073/pnas.0705467105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fontana L, Partridge L, Longo VD. Extending healthy life span—from yeast to humans. Science. 2010;328:321–326. doi: 10.1126/science.1172539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Holzenberger M, Dupont J, Ducos B, et al. IGF-1 receptor regulates lifespan and resistance to oxidative stress in mice. Nature. 2003;421:182–187. doi: 10.1038/nature01298. [DOI] [PubMed] [Google Scholar]
- 75.Guevara-Aguirre J, Balasubramanian P, Guevara-Aguirre M, et al. Growth hormone receptor deficiency is associated with a major reduction in pro-aging signaling, cancer, and diabetes in humans. Sci Transl Med. 2011;3:70ra13. doi: 10.1126/scitranslmed.3001845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bartke A, Wright JC, Mattison JA, Ingram DK, Miller RA, Roth GS. Extending the lifespan of long-lived mice. Nature. 2001;414:412. doi: 10.1038/35106646. [DOI] [PubMed] [Google Scholar]
- 77.Tsuchiya T, Dhahbi JM, Cui X, Mote PL, Bartke A, Spindler SR. Additive regulation of hepatic gene expression by dwarfism and caloric restriction. Physiol Genomics. 2004;17:307–315. doi: 10.1152/physiolgenomics.00039.2004. [DOI] [PubMed] [Google Scholar]
- 78.Colman RJ, Anderson RM, Johnson SC, et al. Caloric restriction delays disease onset and mortality in rhesus monkeys. Science. 2009;325:201–204. doi: 10.1126/science.1173635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Li H, Dimayuga P, Yamashita M, et al. Arterial injury in mice with severe insulin-like growth factor-1 (IGF-1) deficiency. J Cardiovasc Pharmacol Ther. 2002;7:227–233. doi: 10.1177/107424840200700405. [DOI] [PubMed] [Google Scholar]
- 80.Zhu B, Zhao G, Witte DP, Hui DY, Fagin JA. Targeted overexpression of IGF-I in smooth muscle cells of transgenic mice enhances neointimal formation through increased proliferation and cell migration after intraarterial injury. Endocrinology. 2001;142:3598–3606. doi: 10.1210/endo.142.8.8331. [DOI] [PubMed] [Google Scholar]
- 81.Harrington SC, Simari RD, Conover CA. Genetic deletion of pregnancy-associated plasma protein-A is associated with resistance to atherosclerotic lesion development in apolipoprotein E-deficient mice challenged with a high-fat diet. Circ Res. 2007;100:1696–1702. doi: 10.1161/CIRCRESAHA.106.146183. [DOI] [PubMed] [Google Scholar]
- 82.Nichols TC, Busby WH, Jr, Merricks E, et al. Protease-resistant insulin-like growth factor (IGF)-binding protein-4 inhibits IGF-I actions and neointimal expansion in a porcine model of neointimal hyperplasia. Endocrinology. 2007;148:5002–5010. doi: 10.1210/en.2007-0571. [DOI] [PubMed] [Google Scholar]
- 83.Razuvaev A, Henderson B, Girnita L, et al. The cyclolignan picropodophyllin attenuates intimal hyperplasia after rat carotid balloon injury by blocking insulin-like growth factor-1 receptor signaling. J Vasc Surg. 2007;46:108–115. doi: 10.1016/j.jvs.2007.02.066. [DOI] [PubMed] [Google Scholar]
- 84.Resch ZT, Simari RD, Conover CA. Targeted disruption of the pregnancy-associated plasma protein-A gene is associated with diminished smooth muscle cell response to insulin-like growth factor-I and resistance to neointimal hyperplasia after vascular injury. Endocrinology. 2006;147:5634–5640. doi: 10.1210/en.2006-0493. [DOI] [PubMed] [Google Scholar]
- 85.Niu XL, Li J, Hakim ZS, Rojas M, Runge MS, Madamanchi NR. Leukocyte antigen-related deficiency enhances insulin-like growth factor-1 signaling in vascular smooth muscle cells and promotes neointima formation in response to vascular injury. J Biol Chem. 2007;282:19808–19819. doi: 10.1074/jbc.M610452200. [DOI] [PubMed] [Google Scholar]
- 86.Zadelaar S, Kleemann R, Verschuren L, et al. Mouse models for atherosclerosis and pharmaceutical modifiers. Arterioscler Thromb Vasc Biol. 2007;27:1706–1721. doi: 10.1161/ATVBAHA.107.142570. [DOI] [PubMed] [Google Scholar]
- 87.Getz GS, Reardon CA. Diet and murine atherosclerosis. Arterioscler Thromb Vasc Biol. 2006;26:242–249. doi: 10.1161/01.ATV.0000201071.49029.17. [DOI] [PubMed] [Google Scholar]
- 88.Meir KS, Leitersdorf E. Atherosclerosis in the apolipoprotein-E-deficient mouse: a decade of progress. Arterioscler Thromb Vasc Biol. 2004;24:1006–1014. doi: 10.1161/01.ATV.0000128849.12617.f4. [DOI] [PubMed] [Google Scholar]
- 89.Moghadasian MH, McManus BM, Nguyen LB, et al. Pathophysiology of apolipoprotein E deficiency in mice: relevance to apo E-related disorders in humans. FASEB J. 2001;15:2623–2630. doi: 10.1096/fj.01-0463com. [DOI] [PubMed] [Google Scholar]
- 90.Adamo ML, Ma X, Ackert-Bicknell CL, Donahue LR, Beamer WG, Rosen CJ. Genetic increase in serum insulin-like growth factor-I (IGF-I) in C3H/HeJ compared with C57BL/6J mice is associated with increased transcription from the IGF-I exon 2 promoter. Endocrinology. 2006;147:2944–2955. doi: 10.1210/en.2005-0742. [DOI] [PubMed] [Google Scholar]
- 91.Nichols TC, du Laney T, Zheng B, et al. Reduction in atherosclerotic lesion size in pigs by alphaVbeta3 inhibitors is associated with inhibition of insulin-like growth factor-I-mediated signaling. Circ Res. 1999;85:1040–1045. doi: 10.1161/01.res.85.11.1040. [DOI] [PubMed] [Google Scholar]
- 92.Ye P, D’Ercole J. Insulin-like growth factor I (IGF-I) regulates IGF binding protein-5 gene expression in the brain. Endocrinology. 1998;139:65–71. doi: 10.1210/endo.139.1.5676. [DOI] [PubMed] [Google Scholar]
- 93.Frystyk J. Free insulin-like growth factors—measurements and relationships to growth hormone secretion and glucose homeostasis. Growth Horm IGF Res. 2004;14:337–375. doi: 10.1016/j.ghir.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 94.Sukhanov S, Higashi Y, Shai SY, et al. Differential requirement for nitric oxide in IGF-1-induced anti-apoptotic, anti-oxidant and anti-atherosclerotic effects. FEBS Lett. 2011;585:3065–3072. doi: 10.1016/j.febslet.2011.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Titterington JS, Sukhanov S, Higashi Y, Vaughn C, Bowers C, Delafontaine P. Growth hormone-releasing peptide-2 suppresses vascular oxidative stress in ApoE-/- mice but does not reduce atherosclerosis. Endocrinology. 2009;150:5478–5487. doi: 10.1210/en.2009-0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Andersson IJ, Ljungberg A, Svensson L, Gan LM, Oscarsson J, Bergstrom G. Increased atherosclerotic lesion area in apoE deficient mice overexpressing bovine growth hormone. Atherosclerosis. 2006;188:331–340. doi: 10.1016/j.atherosclerosis.2005.11.020. [DOI] [PubMed] [Google Scholar]
- 97.Marin J. Age-related changes in vascular responses: a review. Mech Ageing Dev. 1995;79:71–114. doi: 10.1016/0047-6374(94)01551-v. [DOI] [PubMed] [Google Scholar]
- 98.Payne JA, Reckelhoff JF, Khalil RA. Role of oxidative stress in age-related reduction of NO-cGMP-mediated vascular relaxation in SHR. Am J Physiol Regul Integr Comp Physiol. 2003;285:R542–R551. doi: 10.1152/ajpregu.00056.2003. [DOI] [PubMed] [Google Scholar]
- 99.Chung HY, Sung B, Jung KJ, Zou Y, Yu BP. The molecular inflammatory process in aging. Antioxid Redox Signal. 2006;8:572–581. doi: 10.1089/ars.2006.8.572. [DOI] [PubMed] [Google Scholar]
- 100.Shai SY, Sukhanov S, Higashi Y, Vaughn C, Rosen CJ, Delafontaine P. Low circulating insulin-like growth factor I increases atherosclerosis in ApoE-deficient mice. Am J Physiol Heart Circ Physiol. 2011;300:H1898–H1906. doi: 10.1152/ajpheart.01081.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hammerman MR. Insulin-like growth factors and aging. Endocrinol Metab Clin North Am. 1987;16:995–1011. [PubMed] [Google Scholar]
- 102.D’Costa AP, Ingram RL, Lenham JE, Sonntag WE. The regulation and mechanisms of action of growth hormone and insulin-like growth factor 1 during normal ageing. J Reprod Fertil Suppl. 1993;46:87–98. [PubMed] [Google Scholar]
- 103.Breese CR, Ingram RL, Sonntag WE. Influence of age and long-term dietary restriction on plasma insulin-like growth factor-1 (IGF-1), IGF-1 gene expression, and IGF-1 binding proteins. J Gerontol. 1991;46:B180–B187. doi: 10.1093/geronj/46.5.b180. [DOI] [PubMed] [Google Scholar]
- 104.Khan AS, Sane DC, Wannenburg T, Sonntag WE. Growth hormone, insulin-like growth factor-1 and the aging cardiovascular system. Cardiovasc Res. 2002;54:25–35. doi: 10.1016/s0008-6363(01)00533-8. [DOI] [PubMed] [Google Scholar]
- 105.Shai SY, Sukhanov S, Higashi Y, Vaughn C, Kelly J, Delafontaine P. Smooth muscle cell-specific insulin-like growth factor-1 overexpression in Apoe-/- mice does not alter atherosclerotic plaque burden but increases features of plaque stability. Arterioscler Thromb Vasc Biol. 2010;30:1916–1924. doi: 10.1161/ATVBAHA.110.210831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Dardevet D, Sornet C, Attaix D, Baracos VE, Grizard J. Insulin-like growth factor-1 and insulin resistance in skeletal muscles of adult and old rats. Endocrinology. 1994;134:1475–1484. doi: 10.1210/endo.134.3.8119189. [DOI] [PubMed] [Google Scholar]
- 107.Willis PE, Chadan SG, Baracos V, Parkhouse WS. Restoration of insulin-like growth factor I action in skeletal muscle of old mice. Am J Physiol. 1998;275:E525–E530. doi: 10.1152/ajpendo.1998.275.3.E525. [DOI] [PubMed] [Google Scholar]
- 108.Cao JJ, Kurimoto P, Boudignon B, Rosen C, Lima F, Halloran BP. Aging impairs IGF-I receptor activation and induces skeletal resistance to IGF-I. J Bone Miner Res. 2007;22:1271–1279. doi: 10.1359/jbmr.070506. [DOI] [PubMed] [Google Scholar]
- 109.Wang M, Zhang J, Jiang LQ, et al. Proinflammatory profile within the grossly normal aged human aortic wall. Hypertension. 2007;50:219–227. doi: 10.1161/HYPERTENSIONAHA.107.089409. [DOI] [PubMed] [Google Scholar]
- 110.Rieu I, Magne H, Savary-Auzeloux I, et al. Reduction of low grade inflammation restores blunting of postprandial muscle anabolism and limits sarcopenia in old rats. J Physiol. 2009;587:5483–5492. doi: 10.1113/jphysiol.2009.178319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Degens H. The role of systemic inflammation in age-related muscle weakness and wasting. Scand J Med Sci Sports. 2010;20:28–38. doi: 10.1111/j.1600-0838.2009.01018.x. [DOI] [PubMed] [Google Scholar]
- 112.Hammers DW, Matheny RW, Jr, Sell C, et al. Impairment of IGF-I expression and anabolic signaling following ischemia/reperfusion in skeletal muscle of old mice. Exp Gerontol. 2011;46:265–272. doi: 10.1016/j.exger.2010.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ross R. Atherosclerosis—an inflammatory disease. N Engl J Med. 1999;340:115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 114.Matata BM, Galinanes M. Peroxynitrite is an essential component of cytokines production mechanism in human monocytes through modulation of nuclear factor-kappa B DNA binding activity. J Biol Chem. 2002;277:2330–2335. doi: 10.1074/jbc.M106393200. [DOI] [PubMed] [Google Scholar]
- 115.Succurro E, Andreozzi F, Sciaqua A, Hribal ML, Perticone F, Sesti G. Reciprocal association of plasma IGF-1 and interleukin-6 levels with cardiometabolic risk factors in nondiabetic subjects. Diabetes Care. 2008;31:1886–1888. doi: 10.2337/dc08-0553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Jeschke MG, Barrow RE, Herndon DN. Insulinlike growth factor I plus insulinlike growth factor binding protein 3 attenuates the proinflammatory acute phase response in severely burned children. Ann Surg. 2000;231:246–252. doi: 10.1097/00000658-200002000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Spies M, Wolf SE, Barrow RE, Jeschke MG, Herndon DN. Modulation of types I and II acute phase reactants with insulin-like growth factor-1/binding protein-3 complex in severely burned children. Crit Care Med. 2002;30:83–88. doi: 10.1097/00003246-200201000-00013. [DOI] [PubMed] [Google Scholar]
- 118.Cappola AR, Xue QL, Ferrucci L, Guralnik JM, Volpato S, Fried LP. Insulin-like growth factor I and interleukin-6 contribute synergistically to disability and mortality in older women. J Clin Endocrinol Metab. 2003;88:2019–2025. doi: 10.1210/jc.2002-021694. [DOI] [PubMed] [Google Scholar]
- 119.Serri O, Li L, Maingrette F, Jaffry N, Renier G. Enhanced lipoprotein lipase secretion and foam cell formation by macrophages of patients with growth hormone deficiency: possible contribution to increased risk of atherogenesis? J Clin Endocrinol Metab. 2004;89:979–985. doi: 10.1210/jc.2003-030911. [DOI] [PubMed] [Google Scholar]
- 120.Hochberg Z, Hertz P, Maor G, Oiknine J, Aviram M. Growth hormone and insulin-like growth factor-I increase macrophage uptake and degradation of low density lipoprotein. Endocrinology. 1992;131:430–435. doi: 10.1210/endo.131.1.1612024. [DOI] [PubMed] [Google Scholar]
- 121.Kirstein M, Aston C, Hintz R, Vlassara H. Receptor-specific induction of insulin-like growth factor I in human monocytes by advanced glycosylation end product-modified proteins. J Clin Invest. 1992;90:439–446. doi: 10.1172/JCI115879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Fournier T, Riches DW, Winston BW, et al. Divergence in macrophage insulin-like growth factor-I (IGF-I) synthesis induced by TNF-alpha and prostaglandin E2. J Immunol. 1995;155:2123–2133. [PubMed] [Google Scholar]
- 123.Delafontaine P, Ku L. Reactive oxygen species stimulate insulin-like growth factor I synthesis in vascular smooth muscle cells. Cardiovasc Res. 1997;33:216–222. doi: 10.1016/s0008-6363(96)00179-4. [DOI] [PubMed] [Google Scholar]
- 124.Du J, Peng T, Scheidegger KJ, Delafontaine P. Angiotensin II activation of insulin-like growth factor 1 receptor transcription is mediated by a tyrosine kinase-dependent redox-sensitive mechanism. Arterioscler Thromb Vasc Biol. 1999;19:2119–2126. doi: 10.1161/01.atv.19.9.2119. [DOI] [PubMed] [Google Scholar]
- 125.Tabet F, Schiffrin EL, Touyz RM. Mitogen-activated protein kinase activation by hydrogen peroxide is mediated through tyrosine kinase-dependent, protein kinase C-independent pathways in vascular smooth muscle cells: upregulation in spontaneously hypertensive rats. J Hypertens. 2005;23:2005–2012. doi: 10.1097/01.hjh.0000185715.60788.1b. [DOI] [PubMed] [Google Scholar]
- 126.Azar ZM, Mehdi MZ, Srivastava AK. Activation of insulin-like growth factor type-1 receptor is required for H2O2-induced PKB phosphorylation in vascular smooth muscle cells. Can J Physiol Pharmacol. 2006;84:777–786. doi: 10.1139/y06-024. [DOI] [PubMed] [Google Scholar]
- 127.Gorlach A, Brandes RP, Bassus S, et al. Oxidative stress and expression of p22phox are involved in the up-regulation of tissue factor in vascular smooth muscle cells in response to activated platelets. FASEB J. 2000;14:1518–1528. [PubMed] [Google Scholar]
- 128.Loh K, Deng H, Fukushima A, et al. Reactive oxygen species enhance insulin sensitivity. Cell Metab. 2009;10:260–272. doi: 10.1016/j.cmet.2009.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Wu DC, Re DB, Nagai M, Ischiropoulos H, Przedborski S. The inflammatory NADPH oxidase enzyme modulates motor neuron degeneration in amyotrophic lateral sclerosis mice. Proc Natl Acad Sci U S A. 2006;103:12132–12137. doi: 10.1073/pnas.0603670103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Gardner CD, Eguchi S, Reynolds CM, Eguchi K, Frank GD, Motley ED. Hydrogen peroxide inhibits insulin signaling in vascular smooth muscle cells. Exp Biol Med (Maywood) 2003;228:836–842. doi: 10.1177/15353702-0322807-09. [DOI] [PubMed] [Google Scholar]
- 131.Zhong J, Lee WH. Hydrogen peroxide attenuates insulin-like growth factor-1 neuroprotective effect, prevented by minocycline. Neurochem Int. 2007;51:398–404. doi: 10.1016/j.neuint.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 132.Simon HU, Haj-Yehia A, Levi-Schaffer F. Role of reactive oxygen species (ROS) in apoptosis induction. Apoptosis. 2000;5:415–418. doi: 10.1023/a:1009616228304. [DOI] [PubMed] [Google Scholar]
- 133.Clarke MC, Figg N, Maguire JJ, et al. Apoptosis of vascular smooth muscle cells induces features of plaque vulnerability in atherosclerosis. Nat Med. 2006;12:1075–1080. doi: 10.1038/nm1459. [DOI] [PubMed] [Google Scholar]
- 134.Clarke MC, Littlewood TD, Figg N, et al. Chronic apoptosis of vascular smooth muscle cells accelerates atherosclerosis and promotes calcification and medial degeneration. Circ Res. 2008;102:1529–1538. doi: 10.1161/CIRCRESAHA.108.175976. [DOI] [PubMed] [Google Scholar]
- 135.Okura Y, Brink M, Itabe H, Scheidegger KJ, Kalangos A, Delafontaine P. Oxidized low-density lipoprotein is associated with apoptosis of vascular smooth muscle cells in human atherosclerotic plaques. Circulation. 2000;102:2680–2686. doi: 10.1161/01.cir.102.22.2680. [DOI] [PubMed] [Google Scholar]
- 136.Okura Y, Brink M, Zahid AA, Anwar A, Delafontaine P. Decreased expression of insulin-like growth factor-1 and apoptosis of vascular smooth muscle cells in human atherosclerotic plaque. J Mol Cell Cardiol. 2001;33:1777–1789. doi: 10.1006/jmcc.2001.1441. [DOI] [PubMed] [Google Scholar]
- 137.Patel VA, Zhang QJ, Siddle K, et al. Defect in insulin-like growth factor-1 survival mechanism in atherosclerotic plaque-derived vascular smooth muscle cells is mediated by reduced surface binding and signaling. Circ Res. 2001;88:895–902. doi: 10.1161/hh0901.090305. [DOI] [PubMed] [Google Scholar]
- 138.Wang J, Razuvaev A, Folkersen L, et al. The expression of IGFs and IGF binding proteins in human carotid atherosclerosis, and the possible role of IGF binding protein-1 in the regulation of smooth muscle cell proliferation. Atherosclerosis. 2012;220:102–109. doi: 10.1016/j.atherosclerosis.2011.10.032. [DOI] [PubMed] [Google Scholar]
- 139.Higashi Y, Peng T, Du J, et al. A redox-sensitive pathway mediates oxidized LDL-induced downregulation of insulin-like growth factor-1 receptor. J Lipid Res. 2005;46:1266–1277. doi: 10.1194/jlr.M400478-JLR200. [DOI] [PubMed] [Google Scholar]
- 140.Chakrabarti SK, Cole BK, Wen Y, Keller SR, Nadler JL. 12/15-lipoxygenase products induce inflammation and impair insulin signaling in 3T3-L1 adipocytes. Obesity (Silver Spring) 2009;17:1657–1663. doi: 10.1038/oby.2009.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Seiler A, Schneider M, Forster H, et al. Glutathione peroxidase 4 senses and translates oxidative stress into 12/15-lipoxygenase dependent- and AIF-mediated cell death. Cell Metab. 2008;8:237–248. doi: 10.1016/j.cmet.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 142.Li Y, Higashi Y, Itabe H, Song YH, Du J, Delafontaine P. Insulin-like growth factor-1 receptor activation inhibits oxidized LDL-induced cytochrome C release and apoptosis via the phosphatidylinositol 3 kinase/Akt signaling pathway. Arterioscler Thromb Vasc Biol. 2003;23:2178–2184. doi: 10.1161/01.ATV.0000099788.31333.DB. [DOI] [PubMed] [Google Scholar]
- 143.Jia G, Cheng G, Gangahar DM, Agrawal DK. Insulin-like growth factor-1 and TNF-alpha regulate autophagy through c-jun N-terminal kinase and Akt pathways in human atherosclerotic vascular smooth cells. Immunol Cell Biol. 2006;84:448–454. doi: 10.1111/j.1440-1711.2006.01454.x. [DOI] [PubMed] [Google Scholar]
- 144.Hayashi K, Saga H, Chimori Y, Kimura K, Yamanaka Y, Sobue K. Differentiated phenotype of smooth muscle cells depends on signaling pathways through insulin-like growth factors and phosphatidylinositol 3-kinase. J Biol Chem. 1998;273:28860–28867. doi: 10.1074/jbc.273.44.28860. [DOI] [PubMed] [Google Scholar]
- 145.Ruiz-Torres A, Melon J, Munoz FJ. Insulin stimulates collagen synthesis in vascular smooth muscle cells from elderly patients. Gerontology. 1998;44:144–148. doi: 10.1159/000021998. [DOI] [PubMed] [Google Scholar]
- 146.Verma S, Anderson TJ. Fundamentals of endothelial function for the clinical cardiologist. Circulation. 2002;105:546–549. doi: 10.1161/hc0502.104540. [DOI] [PubMed] [Google Scholar]
- 147.Celermajer DS, Sorensen KE, Spiegelhalter DJ, Georgakopoulos D, Robinson J, Deanfield JE. Aging is associated with endothelial dysfunction in healthy men years before the age-related decline in women. J Am Coll Cardiol. 1994;24:471–476. doi: 10.1016/0735-1097(94)90305-0. [DOI] [PubMed] [Google Scholar]
- 148.Hamilton CA, Brosnan MJ, McIntyre M, Graham D, Dominiczak AF. Superoxide excess in hypertension and aging: a common cause of endothelial dysfunction. Hypertension. 2001;37:529–534. doi: 10.1161/01.hyp.37.2.529. [DOI] [PubMed] [Google Scholar]
- 149.Kung CF, Luscher TF. Different mechanisms of endothelial dysfunction with aging and hypertension in rat aorta. Hypertension. 1995;25:194–200. doi: 10.1161/01.hyp.25.2.194. [DOI] [PubMed] [Google Scholar]
- 150.Csiszar A, Wang M, Lakatta EG, Ungvari Z. Inflammation and endothelial dysfunction during aging: role of NF-kappaB. J Appl Physiol. 2008;105:1333–1341. doi: 10.1152/japplphysiol.90470.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Zheng JS, Yang XQ, Lookingland KJ, et al. Gene transfer of human guanosine 5′-triphosphate cyclohydrolase I restores vascular tetrahydrobiopterin level and endothelial function in low renin hypertension. Circulation. 2003;108:1238–1245. doi: 10.1161/01.CIR.0000089082.40285.C3. [DOI] [PubMed] [Google Scholar]
- 152.Elhadd TA, Abdu TA, Oxtoby J, et al. Biochemical and biophysical markers of endothelial dysfunction in adults with hypopituitarism and severe GH deficiency. J Clin Endocrinol Metab. 2001;86:4223–4232. doi: 10.1210/jcem.86.9.7813. [DOI] [PubMed] [Google Scholar]
- 153.Colao A, di Somma C, Pivonello R, et al. The cardiovascular risk of adult GH deficiency (GHD) improved after GH replacement and worsened in untreated GHD: a 12-month prospective study. J Clin Endocrinol Metab. 2002;87:1088–1093. doi: 10.1210/jcem.87.3.8336. [DOI] [PubMed] [Google Scholar]
- 154.Perticone F, Sciacqua A, Perticone M, et al. Low-plasma insulin-like growth factor-I levels are associated with impaired endothelium-dependent vasodilatation in a cohort of untreated, hypertensive Caucasian subjects. J Clin Endocrinol Metab. 2008;93:2806–2810. doi: 10.1210/jc.2008-0646. [DOI] [PubMed] [Google Scholar]
- 155.Fryburg DA. NG-monomethyl-L-arginine inhibits the blood flow but not the insulin-like response of forearm muscle to IGF- I: possible role of nitric oxide in muscle protein synthesis. J Clin Invest. 1996;97:1319–1328. doi: 10.1172/JCI118548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Pendergrass M, Fazioni E, Collins D, DeFronzo RA. IGF-I increases forearm blood flow without increasing forearm glucose uptake. Am J Physiol. 1998;275:E345–E350. doi: 10.1152/ajpendo.1998.275.2.E345. [DOI] [PubMed] [Google Scholar]
- 157.Imrie H, Abbas A, Viswambharan H, et al. Vascular insulin-like growth factor-I resistance and diet-induced obesity. Endocrinology. 2009;150:4575–4582. doi: 10.1210/en.2008-1641. [DOI] [PubMed] [Google Scholar]
- 158.Holly JM, Amiel SA, Sandhu RR, Rees LH, Wass JA. The role of growth hormone in diabetes mellitus. J Endocrinol. 1988;118:353–364. doi: 10.1677/joe.0.1180353. [DOI] [PubMed] [Google Scholar]
- 159.Michell BJ, Griffiths JE, Mitchelhill KI, et al. The Akt kinase signals directly to endothelial nitric oxide synthase. Curr Biol. 1999;9:845–848. doi: 10.1016/s0960-9822(99)80371-6. [DOI] [PubMed] [Google Scholar]
- 160.Elzaouk L, Leimbacher W, Turri M, et al. Dwarfism and low insulin-like growth factor-1 due to dopamine depletion in Pts-/- mice rescued by feeding neurotransmitter precursors and H4-biopterin. J Biol Chem. 2003;278:28303–28311. doi: 10.1074/jbc.M303986200. [DOI] [PubMed] [Google Scholar]
- 161.Tanaka J, Koshimura K, Murakami Y, Kato Y. Possible involvement of tetrahydrobiopterin in the trophic effect of insulin-like growth factor-1 on rat pheochromocytoma-12 (PC12) cells. Neurosci Lett. 2002;328:201–203. doi: 10.1016/s0304-3940(02)00497-4. [DOI] [PubMed] [Google Scholar]
- 162.Csiszar A, Labinskyy N, Perez V, et al. Endothelial function and vascular oxidative stress in long-lived GH/IGF-deficient Ames dwarf mice. Am J Physiol Heart Circ Physiol. 2008;295:H1882–H1894. doi: 10.1152/ajpheart.412.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Ungvari Z, Gautam T, Koncz P, et al. Vasoprotective effects of life span-extending peripubertal GH replacement in Lewis dwarf rats. J Gerontol A Biol Sci Med Sci. 2010;65:1145–1156. doi: 10.1093/gerona/glq147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Bailey-Downs LC, Sosnowska D, Toth P, et al. Growth hormone and IGF-1 deficiency exacerbate high-fat diet-induced endothelial impairment in obese Lewis dwarf rats: implications for vascular aging. J Gerontol A Biol Sci Med Sci. 2011 doi: 10.1093/gerona/glr197. doi:10.1093/gerona/glr197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Bailey-Downs LC, Mitschelen M, Sosnowska D, et al. Liver-specific knockdown of IGF-1 decreases vascular oxidative stress resistance by impairing the Nrf2-dependent antioxidant response: a novel model of vascular aging. J Gerontol A Biol Sci Med Sci. 2012;67A:313–329. doi: 10.1093/gerona/glr164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Sonntag WE, Carter CS, Ikeno Y, et al. Adult-onset growth hormone and insulin-like growth factor I deficiency reduces neoplastic disease, modifies age-related pathology, and increases life span. Endocrinology. 2005;146:2920–2932. doi: 10.1210/en.2005-0058. [DOI] [PubMed] [Google Scholar]
- 167.Abbas A, Imrie H, Viswambharan H, et al. The insulin-like growth factor-1 receptor is a negative regulator of nitric oxide bioavailability and insulin sensitivity in the endothelium. Diabetes. 2011;60:2169–2178. doi: 10.2337/db11-0197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Lakatta EG. Cardiovascular regulatory mechanisms in advanced age. Physiol Rev. 1993;73:413–467. doi: 10.1152/physrev.1993.73.2.413. [DOI] [PubMed] [Google Scholar]
- 169.Kotsis V, Stabouli S, Karafillis I, Nilsson P. Early vascular aging and the role of central blood pressure. J Hypertens. 2011;29:1847–1853. doi: 10.1097/HJH.0b013e32834a4d9f. [DOI] [PubMed] [Google Scholar]
- 170.Sandu OA, Ito M, Begum N. Selected contribution: insulin utilizes NO/cGMP pathway to activate myosin phosphatase via Rho inhibition in vascular smooth muscle. J Appl Physiol. 2001;91:1475–1482. doi: 10.1152/jappl.2001.91.3.1475. [DOI] [PubMed] [Google Scholar]
- 171.Standley PR, Zhang F, Ram JL, Zemel MB, Sowers JR. Insulin attenuates vasopressin-induced calcium transients and a voltage-dependent calcium response in rat vascular smooth muscle cells. J Clin Invest. 1991;88:1230–1236. doi: 10.1172/JCI115426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Galderisi M, Vitale G, Lupoli G, et al. Inverse association between free insulin-like growth factor-1 and isovolumic relaxation in arterial systemic hypertension. Hypertension. 2001;38:840–845. doi: 10.1161/hy1001.091776. [DOI] [PubMed] [Google Scholar]
- 173.Colao A, Di Somma C, Cascella T, et al. Relationships between serum IGF1 levels, blood pressure, and glucose tolerance: an observational, exploratory study in 404 subjects. Eur J Endocrinol. 2008;159:389–397. doi: 10.1530/EJE-08-0201. [DOI] [PubMed] [Google Scholar]
- 174.Tivesten A, Bollano E, Andersson I, et al. Liver-derived insulin-like growth factor-I is involved in the regulation of blood pressure in mice. Endocrinology. 2002;143:4235–4242. doi: 10.1210/en.2002-220524. [DOI] [PubMed] [Google Scholar]
- 175.Vecchione C, Colella S, Fratta L, et al. Impaired insulin-like growth factor I vasorelaxant effects in hypertension. Hypertension. 2001;37:1480–1485. doi: 10.1161/01.hyp.37.6.1480. [DOI] [PubMed] [Google Scholar]
- 176.Hongo K, Nakagomi T, Kassell NF, et al. Effects of aging and hypertension on endothelium-dependent vascular relaxation in rat carotid artery. Stroke. 1988;19:892–897. doi: 10.1161/01.str.19.7.892. [DOI] [PubMed] [Google Scholar]
- 177.Hasdai D, Holmes DR, Jr, Richardson DM, Izhar U, Lerman A. Insulin and IGF-I attenuate the coronary vasoconstrictor effects of endothelin-1 but not of sarafotoxin 6c. Cardiovasc Res. 1998;39:644–650. doi: 10.1016/s0008-6363(98)00144-8. [DOI] [PubMed] [Google Scholar]
- 178.Duerrschmidt N, Wippich N, Goettsch W, Broemme HJ, Morawietz H. Endothelin-1 induces NAD(P)H oxidase in human endothelial cells. Biochem Biophys Res Commun. 2000;269:713–717. doi: 10.1006/bbrc.2000.2354. [DOI] [PubMed] [Google Scholar]
- 179.Li L, Fink GD, Watts SW, et al. Endothelin-1 increases vascular superoxide via endothelin(A)-NADPH oxidase pathway in low-renin hypertension. Circulation. 2003;107:1053–1058. doi: 10.1161/01.cir.0000051459.74466.46. [DOI] [PubMed] [Google Scholar]
- 180.Wedgwood S, McMullan DM, Bekker JM, Fineman JR, Black SM. Role for endothelin-1-induced superoxide and peroxynitrite production in rebound pulmonary hypertension associated with inhaled nitric oxide therapy. Circ Res. 2001;89:357–364. doi: 10.1161/hh1601.094983. [DOI] [PubMed] [Google Scholar]
- 181.Frank HJ, Levin ER, Hu RM, Pedram A. Insulin stimulates endothelin binding and action on cultured vascular smooth muscle cells. Endocrinology. 1993;133:1092–1097. doi: 10.1210/endo.133.3.8365355. [DOI] [PubMed] [Google Scholar]
- 182.Kwok CF, Juan CC, Shih KC, Hwu CM, Jap TS, Ho LT. Insulin-like growth factor-1 increases endothelin receptor A levels and action in cultured rat aortic smooth muscle cells. J Cell Biochem. 2005;94:1126–1134. doi: 10.1002/jcb.20321. [DOI] [PubMed] [Google Scholar]
- 183.Asahara T, Murohara T, Sullivan A, et al. Isolation of putative progenitor endothelial cells for angiogenesis. Science. 1997;275:964–967. doi: 10.1126/science.275.5302.964. [DOI] [PubMed] [Google Scholar]
- 184.Werner N, Kosiol S, Schiegl T, et al. Circulating endothelial progenitor cells and cardiovascular outcomes. N Engl J Med. 2005;353:999–1007. doi: 10.1056/NEJMoa043814. [DOI] [PubMed] [Google Scholar]
- 185.Alev C, Ii M, Asahara T. Endothelial progenitor cells: a novel tool for the therapy of ischemic diseases. Antioxid Redox Signal. 2011;15:949–965. doi: 10.1089/ars.2010.3872. [DOI] [PubMed] [Google Scholar]
- 186.Foteinos G, Hu Y, Xiao Q, Metzler B, Xu Q. Rapid endothelial turnover in atherosclerosis-prone areas coincides with stem cell repair in apolipoprotein E-deficient mice. Circulation. 2008;117:1856–1863. doi: 10.1161/CIRCULATIONAHA.107.746008. [DOI] [PubMed] [Google Scholar]
- 187.Walter DH, Rittig K, Bahlmann FH, et al. Statin therapy accelerates reendothelialization: a novel effect involving mobilization and incorporation of bone marrow-derived endothelial progenitor cells. Circulation. 2002;105:3017–3024. doi: 10.1161/01.cir.0000018166.84319.55. [DOI] [PubMed] [Google Scholar]
- 188.Aicher A, Heeschen C, Mildner-Rihm C, et al. Essential role of endothelial nitric oxide synthase for mobilization of stem and progenitor cells. Nat Med. 2003;9:1370–1376. doi: 10.1038/nm948. [DOI] [PubMed] [Google Scholar]
- 189.Thum T, Fraccarollo D, Schultheiss M, et al. Endothelial nitric oxide synthase uncoupling impairs endothelial progenitor cell mobilization and function in diabetes. Diabetes. 2007;56:666–674. doi: 10.2337/db06-0699. [DOI] [PubMed] [Google Scholar]
- 190.Dernbach E, Urbich C, Brandes RP, Hofmann WK, Zeiher AM, Dimmeler S. Antioxidative stress-associated genes in circulating progenitor cells: evidence for enhanced resistance against oxidative stress. Blood. 2004;104:3591–3597. doi: 10.1182/blood-2003-12-4103. [DOI] [PubMed] [Google Scholar]
- 191.He T, Peterson TE, Holmuhamedov EL, et al. Human endothelial progenitor cells tolerate oxidative stress due to intrinsically high expression of manganese superoxide dismutase. Arterioscler Thromb Vasc Biol. 2004;24:2021–2027. doi: 10.1161/01.ATV.0000142810.27849.8f. [DOI] [PubMed] [Google Scholar]
- 192.Haddad P, Dussault S, Groleau J, et al. Nox2-containing NADPH oxidase deficiency confers protection from hindlimb ischemia in conditions of increased oxidative stress. Arterioscler Thromb Vasc Biol. 2009;29:1522–1528. doi: 10.1161/ATVBAHA.109.191437. [DOI] [PubMed] [Google Scholar]
- 193.Ingram DA, Krier TR, Mead LE, et al. Clonogenic endothelial progenitor cells are sensitive to oxidative stress. Stem Cells. 2007;25:297–304. doi: 10.1634/stemcells.2006-0340. [DOI] [PubMed] [Google Scholar]
- 194.Urao N, Inomata H, Razvi M, et al. Role of nox2-based NADPH oxidase in bone marrow and progenitor cell function involved in neovascularization induced by hindlimb ischemia. Circ Res. 2008;103:212–220. doi: 10.1161/CIRCRESAHA.108.176230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Rauscher FM, Goldschmidt-Clermont PJ, Davis BH, et al. Aging, progenitor cell exhaustion, and atherosclerosis. Circulation. 2003;108:457–463. doi: 10.1161/01.CIR.0000082924.75945.48. [DOI] [PubMed] [Google Scholar]
- 196.Thum T, Fleissner F, Klink I, et al. Growth hormone treatment improves markers of systemic nitric oxide bioavailability via insulin-like growth factor-I. J Clin Endocrinol Metab. 2007;92:4172–4179. doi: 10.1210/jc.2007-0922. [DOI] [PubMed] [Google Scholar]
- 197.Thum T, Hoeber S, Froese S, et al. Age-dependent impairment of endothelial progenitor cells is corrected by growth-hormone-mediated increase of insulin-like growth-factor-1. Circ Res. 2007;100:434–443. doi: 10.1161/01.RES.0000257912.78915.af. [DOI] [PubMed] [Google Scholar]
- 198.Yoder MC. Defining human endothelial progenitor cells. J Thromb Haemost. 2009;7(suppl 1):49–52. doi: 10.1111/j.1538-7836.2009.03407.x. [DOI] [PubMed] [Google Scholar]
- 199.Tilki D, Hohn HP, Ergun B, Rafii S, Ergun S. Emerging biology of vascular wall progenitor cells in health and disease. Trends Mol Med. 2009;15:501–509. doi: 10.1016/j.molmed.2009.09.004. [DOI] [PubMed] [Google Scholar]