Question
A 70-year-old woman is referred to an orthopaedic outpatient clinic for consideration for a total hip replacement. She is a treated hypertensive and a lifelong smoker, and has a BMI of 35. How do these factors affect her ASA status and what effect does this have on her perioperative management?
The American Society of Anesthesiologists physical status (ASA PS) classification was introduced to clinical practice 70 years ago. How has it changed in that time and how does it affect perioperative management in the 21st century? Turn overleaf to find out more about the ASA classification.
History
In 1941 the american Society of anesthetists (later the american Society of anesthesiologists, aSa) published a booklet for its members containing the first version of a ‘physical status’ classification for patients about to undergo surgery.
In May 1941, Meyer Saklad in Anesthesiology described the new ‘six degree’ ASA PS grading of a patient's physical state as just one of the components of the operative risk.1
He listed the other components as:
the planned surgical procedure;
the ability and skill of the surgeon in the particular procedure contemplated;
the attention to postoperative care; and
the past experience of the anaesthetist in similar circumstances.
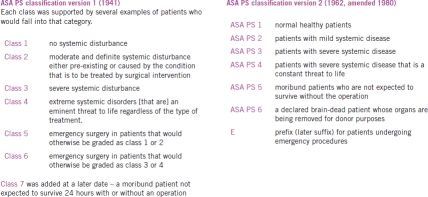
The classification of physical state was, in Saklad's opinion, a useful statistical tool and he warned: ‘No attempt should be made to prognosticate the effect of a surgical procedure upon a patient of a given Physical State.’ Saklad gave several examples of systemic illnesses for the first four classes in order to standardise the classification. There was no suggestion that patients in a poor physical state should be targeted for optimisation pre surgery. The 1941 version of the ASA classification is shown in Figure 1.
FIGURE 1.
Evolution of the ASA PS classification
The current ASA PS classification was proposed by Dripps et al in 19612 and adopted by the ASA in 1962.3 It took on the more familiar form used to the present day, with classes 1 to 4 being retained, emergency classes 5 and 6 being replaced by using the prefix ‘E’ to classes 1 to 4; the original class 7 became class 5 in the new version (Figure 1). Unlike the 1941 version, no examples of each class were given. One of the criticisms of the 1962 version is that the allocated ASA PS class is left to the judgement of the individual anaesthetist; thus there is more inter-observer variability.
In 1980, ASA PS class 6 was added to take into account the brain-stem-dead organ donor - patients that are already dead before entering theatre.
Currently the ASA PS has two functions:
To quantify the amount of physiological reserve that a patient possesses at the time at which they are assessed for a surgical procedure. This may change before the patient actually undergoes the procedure, either by optimisation and improvement of their physical state or because they deteriorate and have less reserve.
It should not be used as a sole predictor of operative risk to the patient. a patient of ASA PS 3 still has that physical status whether he or she is having a skin lesion removed under local anaesthetic or undergoing a pancreatectomy but the overall risk is much greater in the latter operation.4
As a method of adjusting healthcare billing in the US.
Other factors affecting views of ASA PS class
The current version of the ASA PS does not provide specific defining examples of ‘unwellness’ for each class. A cohort of anaesthetists may ascribe different PS classes to the same patient; this is a well-known problem when the ASA PS is part of the standardisation data for a study. Some anaesthetists will class a patient with several ‘mild’ or well-controlled systemic illnesses as ASA PS2, whereas other anaesthetists will ‘add together’ the physical effect of those illnesses and classify that patient as ASA PS3.
Additionally, anaesthetists will also take into account factors that are not medical conditions in their own right but that adversely influence how a patient will tolerate a systemic medical condition or operative procedure. The most common of these are the extremes of age (neonates and age over 80) - many anaesthetists will grade a fit 80-year-old as ASA PS3. Other influencing factors are obesity and smoking history.
ASA PS is not exhaustive of physical risk factors
The ASA classification for a particular patient is based on systemic disease. The extent of this disease is evident from the patient's past medical history and medication list, and the amount of limitation that the disease causes to his or her everyday life.
There are also some ‘card carrying’ physical problems that add to a patient's operative risk. a useful catch-all question to pick these up is: ‘Have you had any problems with previous anaesthetics?’ and ‘Has anyone in your family had any problems with anaesthetics?'
Difficult airway
Patients may have a letter written by a previous anaesthetist, a Difficult Airway Society card or a MedicAlert®-type bracelet.
Genetic problems
Malignant hyperpyrexia and suxamethonium apnoea: usually all the blood relatives of an index case are tested and the patient will know his or her status.
Jehovah's Witnesses
This subject will be covered more fully in a later article. Jehovah's Witnesses carry a higher peri-operative risk in operations with expected major blood loss and a sensitive pre-operative discussion needs to take place about what level of blood transfusion/replacement they will accept.
Making ASA PS work for surgeons
The ASA PS classification is only one component of the overall procedural risk assessment but is easily assessed at the first surgical consultation with that patient.
As a general rule of thumb, a patient who is ASA 3 or 4 (or has any other anaesthetic risk factors as described above) should have a senior anaesthetic consultation as soon as you consider them for surgery. An exception would be when patients have repeated elective procedures (such as a six-monthly cystoscopy) and their physical state has been stable since their last anaesthetic. The consultation may be with your regular anaesthetist or through an anaesthetic pre-operative clinic.
A planned consultation with the anaesthetist will allow for quantifying the risks that the patient's medical problems present in the peri-operative period and for a clear and unhurried discussion of the pre-operative management (investigation and optimisation), anaesthetic techniques and the need for post-operative critical care support.
This helps the anaesthetist but what about the surgical team? In an era in which peri-operative outcomes are scrutinised, this strategy allows for fewer cancellations on the day of surgery because the patient is ‘unfit for surgery'; better planning of the operating lists; and making sure the least-fit patients are receiving the services of the most experienced team.
SUMMARY
The ASA classification is an assessment of the patient's pre-operative physical status. On its own, the ASA classification of physical status is not a predictor of operative risk.
Operative risk is a combination of:
the physical status of the patient;
the physiological derangement that the procedure will cause;
the skill and experience of the operator;
the skill and experience of the anaesthetist (including the choice of anaesthetic); and
the physiological support service in the peri-operative period (including pre-operative optimisation and critical care).
A patient for an elective procedure with an ASA grade of 3 or 4 needs a consultation with a senior anaesthetist as far before the proposed surgery as is possible. This will enable the patient's physical condition to be optimised with better post-operative outcome and will reduce the chance of ‘on the day’ cancellation due to being medically unfit.
References
- 1.Saklad M. Grading of patients for surgical procedures. Anesthesiology. 1941;2:281–84. http://journals.lww.com/anesthesiology/toc/1941/05000. [Google Scholar]
- 2.Dripps RD, Lamont A, Eckenhoff JE. The role of anesthesia in surgical mortality. JAMA. 1961;178:261–66. doi: 10.1001/jama.1961.03040420001001. [DOI] [PubMed] [Google Scholar]
- 3.New Classification of Physical Status. Anesthesiology. 1963;24:111. http://journals.lww.com/anesthesiology/toc/1963/01000. [Google Scholar]
- 4.Owens WD. American Society of Anesthesiologists Physical Status Classification System is not a risk classification system. Anesthesiology. 2001;94:378. doi: 10.1097/00000542-200102000-00042. [DOI] [PubMed] [Google Scholar]