Active expert peer-to-peer consultation with prescribing oncologists can promote adherence to guidelines and lead to cost reductions without risk of neutropenic fever, with or without hospitalization, for patients with cancer.
Abstract
Purpose:
Practice guidelines do not recommend the routine use of colony-stimulating factors when there is a low risk (< 10%) of febrile neutropenia (FN). We prospectively determined whether expert peer-to-peer consultation with prescribing oncologists would improve adherence to guidelines and whether there would be any adverse events associated with that adherence.
Methods:
Commencing in March 2010, we reviewed requests for pegfilgrastim from 22 community oncology practices comprising 78 physicians providing service to approximately 97,000 Medicare members. Paid claims data on all chemotherapy and supportive care medications were reviewed from fourth quarter (Q4) 2009 through third quarter (Q3) 2010. In total, 82 patients received pegfilgrastim. If the prescribed chemotherapy was associated with a low risk (< 10%) for FN, then a peer review was initiated. The treating physician made the final decision to use, or not use, pegfilgrastim, and no denials were issued.
Results:
A total of 245 units (1 unit = 6 mg) of pegfilgrastim were administered during the four quarters analyzed. Use in the low-risk category decreased from 52 units in Q4 2009 to 15 units in Q3 2010. The per-member per-month (PMPM) cost of pegfilgrastim decreased across quarters, with an average cost of $1.07 PMPM for Q4 2009 and $0.57 PMPM for Q3 2010. No studied patient was admitted for neutropenic fever.
Conclusion:
Active expert peer-to-peer consultation with prescribing oncologists can promote adherence to guidelines and potentially lead to significant cost reductions without significant risk of neutropenic fever, with or without hospitalization, for patients with cancer.
Introduction
Febrile neutropenia (FN) is a medical emergency that must be treated with antibiotics covering both Gram-positive as well as Gram-negative pathogens.1 Although the definition of neutropenia varies across institutions, most agree that an absolute neutrophil count (ANC) < 500 cells/μL, or a neutrophil count < 1,000 cells/μL with a predicted nadir < 500 cells/μL, are criteria likely to be clinically significant. The treatment of FN has improved greatly, and there has been a progressive decline in mortality rates since the prompt initiation of empiric antibiotic coverage became standard.2 Despite improvements in the management of FN, minimizing the development of FN remains the primary strategy for avoidance of morbidity and mortality. Granulocyte colony-stimulating factors (G-CSFs), such as filgrastim, sargramostim, and pegfilgrastim, when used properly, minimize the incidence of neutropenic complications. The pivotal trial leading to filgrastim approval for the prevention of FN showed a reduction in the rate of FN from 76% in placebo-treated patients to 40% in filgrastim-treated patients.3 The hospitalization rate in the first cycle decreased from 69% among placebo-treated patients to 52% among filgrastim-treated patients. Clearly, the regimens studied for initial filgrastim approval were associated with extremely high rates of neutropenic events.
Although filgrastim must be administered daily for several days after cytotoxic treatment, the development of a long-acting growth factor allows a single postchemotherapy injection. The randomized study that led to the approval of pegfilgrastim used filgrastim in the control arm.4 Both the pegfilgrastim and filgrastim arms in the pivotal trials showed FN rates in the range of 10% to 20%, with a similar incidence, depth, and duration of severe neutropenia.
CSFs are thus proven to reduce FN and associated hospitalizations. Peer-reviewed literature is abundant, describing the clinical efficacy and cost effectiveness of CSFs, when used in clinical situations deemed higher risk for FN.5–10 All nationally and internationally recognized guidelines use the likelihood of developing FN as the primary factor when determining if prophylactic CSFs should be used.11–14 It is universally recommended that prophylactic G-CSFs be used in patients receiving chemotherapy regimens with a high risk (> 20%) of FN. When using a chemotherapy regimen associated with an intermediate risk of FN (10% to 20%), guidelines recommend considering patient-related risk factors, such as age (≥ 65 years), baseline WBC count, treatment intent, and comorbid conditions. In situations where dose-dense or dose-intense chemotherapy strategies have survival benefits, prophylactic G-CSF support is recommended. No national guidelines recommend the use of CSFs when the likelihood of FN is < 10%, unless there are meaningful additional clinical risks.11–14
None of the current guidelines take cost into consideration, although the 2000 American Society of Clinical Oncology (ASCO) guideline commented that the routine use of CSFs for primary prophylaxis cannot be justified on the basis of cost savings, when the FN risk is < 15%.12
Although it is also recognized that CSFs might have the ability to reduce the duration of mild neutropenia, the clinical relevance of this finding is unproven, especially in noncurative or palliative settings. We were unable to find any literature demonstrating an improvement in clinical outcome with the prophylactic use of CSFs when the risk of FN was < 10%. The lack of literature in this low-risk setting is consistent with guidelines stating that primary prophylaxis with CSFs should not be routinely used if the risk of FN is < 10%.
Methods
Chemotherapy Classification Into Low Versus Higher Risk
Chemotherapy regimens deemed intermediate or high risk in the national guidelines are combined in this analysis as one group and called higher risk. The chemotherapy regimens that are classified as neither intermediate nor high risk in any of the guidelines, or are explicitly classified as low risk in the guidelines, were deemed low risk. One exception to this is the carboplatin-paclitaxel regimen, which is listed as an intermediate-risk regimen in the National Comprehensive Cancer Network (NCCN) guidelines, although numerous randomized clinical studies have shown that this regimen is associated with a low risk of FN.15–19, We identified two articles that showed the risk of FN with the carboplatin-paclitaxel regimen to be intermediate. One of these studies used a higher carboplatin dose (ie, area under the curve, 7.5), which is now seldom used in community practices.20 The other is an article from Japan showing a risk of FN of 18% in Japanese patients.21 It is now known that pharmacogenomic differences between white and Japanese populations resulted in this higher risk of FN in a Japanese population.22 In view of all this, we felt comfortable categorizing the carboplatin-paclitaxel regimen as low risk (< 10%) for FN.
Also, although there was a low risk of FN in the pivotal trial with the docetaxel-cyclophosphamide regimen,23,24 it has since been reported that the risk of FN with this regimen falls in the intermediate category.25 We have classified this regimen as low risk, however, consistent with national guidelines. Finally, we did observe use of pegfilgrastim in the absence of any chemotherapy administration, and such usage was classified as occurring in the setting of low-risk regimens for the purposes of this study.
The specific chemotherapy regimens categorized as low risk in this study are listed in Table 1. Use of pegfilgrastim with all other regimens was considered to be prophylaxis for a higher risk of FN.
Table 1.
Chemotherapy Regimens Deemed Low Risk for Febrile Neutropenia
| Regimen |
|---|
| Rituximab single agent |
| Paclitaxel single agent |
| Carboplatin plus paclitaxel |
| Doxorubicin plus cyclophosphamide |
| FU plus leucovorin |
| Bevacizumab single agent |
| Bortezomib single agent |
| FOLFIRI plus bevacizumab |
| FOLFOX |
| FOLFOX plus bevacizumab |
| Carboplatin plus pemetrexed |
| Rituximab plus bendamustine |
| Liposomal doxorubicin (Doxil)* |
| Docetaxel plus cyclophosphamide |
| No chemotherapy administration |
Abbreviations: FOLFIRI, FU, leucovorin, and irinotecan; FOLFOX, infusional FU, leucovorin, and oxaliplatin; FU, fluorouracil.
Doxil; Janssen Pharmaceuticals, Titusville, NJ.
Background Use of Pegfilgrastim
Twenty-two community oncology practices comprising 78 physicians in Broward and Palm Beach Counties in Florida agreed to participate in this project. As a baseline, paid claims data on all chemotherapy and supportive care medications for approximately 97,000 Medicare health maintenance organization (HMO) members in these two counties were reviewed from the fourth quarter (Q4) of 2009 and the first 2 months of 2010.
Prior-Review System
Commencing March 2010, a prior-review system was initiated for pegfilgrastim. All chemotherapy and supportive care medication orders for these 97,000 Medicare HMO members were prereviewed by a board-certified hematologist/oncologist. If the prescribed chemotherapy protocol was deemed to have an intermediate (10% to 20%) or high risk (> 20%) for FN, then there was no intervention. If the prescribed chemotherapy was deemed to have a low risk (< 10%) for FN, then medical records were reviewed by the peer reviewer.
If the clinical situation did not seem to warrant prophylaxis with CSFs, then the treating physician was contacted by the reviewing physician and informed that the treatment plan was associated with a low risk of neutropenic complications, and the guidelines do not recommend the routine use of pegfilgrastim in low-risk clinical situations. If requested, a reference to the guidelines was provided as well as the pivotal trials showing the incidence of FN with the chemotherapy regimen in question. The decision to use pegfilgrastim, however, remained with the treating physician, and no denials were issued.
Postintervention Use of Pegfilgrastim
Paid claims data on all chemotherapy and supportive care medications from these 22 oncology practices were reviewed from March 2010 and the second (Q2) and third quarters (Q3) of 2010.
Results
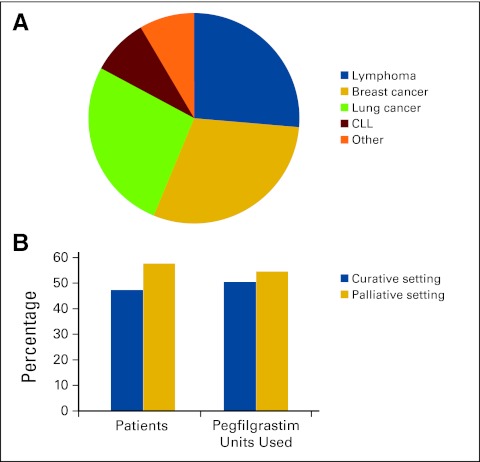
A total of 22 community oncology practices covering approximately 97,000 Medicare HMO members participated in this project. A total of 82 patients received a total of 245 units of pegfilgrastim over the four quarters from Q4 2009 through Q3 2010. Figure 1A details use by tumor type. A significant proportion of use was in lymphomas (18 patients), breast cancer (17 patients), lung cancer (16 patients), and chronic lymphocytic leukemia (six patients). Six patients received pegfilgrastim without a diagnosis of malignancy or any associated chemotherapy. These patients are classified in the others category. Figure 1B shows that the intent of therapy was deemed curative in 37 patients (45%), who received 117 units (48%) of the total pegfilgrastim used. The remaining 128 pegfilgrastim units (52%) were used in 45 patients (55%), in whom the treatment intent was palliation.
Figure 1.
(A) Use of pegfilgrastim by tumor type (N = 87). (B) Use of pegfilgrastim by treatment intent. CLL, chronic lymphocytic leukemia.
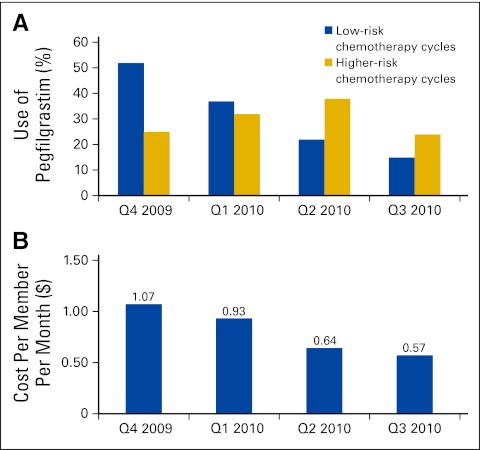
The pegfilgrastim use by quarter shows that 77 units were used in Q4 2009, 69 units in the first quarter (Q1) of 2010, 60 units in Q2 2010, and 39 units in Q3 2010 (Fig 2A). The proportional use in the low-risk category for FN was 67.5% in Q4 2009, 53.6% in Q1 2010, 36.6% in Q2 2010, and 38.4% in Q3 2010. Use in the low-risk category decreased from 52 units in Q4 2009 to 37 units in Q1 2010 to 22 units in Q2 2010 and to 15 units in Q3 2010. Use in the higher-risk category varied by quarter and did not seem to be affected by the prior-review process.
Figure 2.
(A) Use of pegfilgrastim across quarters (Qs), classified by chemotherapy regimen febrile neutropenia risk. (B) Per-member per-month cost of pegfilgrastim Q4 2009 through Q3 2010 (intervention began March 1, 2010).
We also analyzed whether the use of pegfilgrastim differed with the source of pegfilgrastim acquisition by oncology practices (ie, whether pegfilgrastim was acquired via buy and bill v obtained from a specialty pharmacy). When acquired by buy and bill, 60% of the usage of pegfilgrastim occurred with low-risk regimens, and when acquired from a specialty pharmacy, 45% of the usage was with low-risk regimens. A similar trend of a higher proportional use in noncurative or palliative settings was seen when pegfilgrastim was acquired via buy and bill. There was no reported episode of FN or other neutropenic events among patients in whom the practicing physician withheld pegfilgrastim in the setting of a low-risk regimen. The per-member per-month (PMPM) cost of pegfilgrastim decreased across quarters, with an average cost of $1.07 PMPM for Q4 2009, $0.93 PMPM for Q1 2010, $0.64 PMPM for Q2 2010, and $0.57 PMPM for Q3 2010 (Fig 2B).
Discussion
Our review of pegfilgrastim use in community practices in southern Florida demonstrates that a significant proportion of the drug is used with chemotherapy regimens deemed to be low risk (< 10%) for FN. In the absence of a peer-review process, more than two thirds (67.5% in Q4 2009) of pegfilgrastim use was not consistent with published literature or available guidelines. Although the ASCO, NCCN, and European Organisation for Research and Treatment of Cancer guidelines state that primary prophylaxis with CSFs be used with high-risk chemotherapy regimens (> 20% FN risk) or with intermediate-risk chemotherapy regimens (10% to 20% FN risk) associated with additional clinical risk factors for FN, none of the guidelines recommend the routine use of pegfilgrastim with low-risk chemotherapy regimens (< 10% FN risk). Clearly, the guidelines on the use of G-CSFs have not translated into some of the clinical practices.
Although our review did not go into the details of why physicians use pegfilgrastim in clinical situations generally recognized as having a low risk for FN, we speculate that physicians might be trying to prevent lower-grade neutropenia, even though there is no evidence that doing so improves clinical outcome. Direct-to-consumer advertising by the pharmaceutical industry may be an additional driver of this profound and expensive overuse. In the future, an alternate design of a randomized controlled trial of peer-review consultative process versus no consultation might be better able to define the effectiveness of the consultative process.
We conclude that a peer-review consultative process substantially decreases the inappropriate use of pegfilgrastim, even when denials are not issued. This particular peer-to-peer review system did not result in a reduction in the appropriate use of pegfilgrastim, and no neutropenic events in patients receiving low-risk regimens were reported.
Our peer-to-peer consultative review process led to significant reductions in pegfilgrastim expenses, from $1.07 PMPM in Q4 2009 to $0.57 PMPM in Q3 2010. Although we recognize the limitations of these findings would include the relatively small sample size and lack of statistical rigor, nonetheless, the savings among 97,000 covered lives could translate to more than $250 million per year in cost reduction across the entire Medicare-eligible population.
In conclusion, a large proportion of pegfilgrastim use in the 22 community practices that participated in this study was not in accordance with evidence-based literature or nationally recognized guidelines. A real-time peer-review process conducted by a board-certified hematologist and/or oncologist improved adherence to guidelines and resulted in significant cost savings.
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
Author Contributions
Conception and design: Marc L. Fishman
Financial support: Marc L. Fishman
Administrative support: Marc L. Fishman, Sharon Davis
Collection and assembly of data: Sharon Davis
Data analysis and interpretation: Akhil Kumar, Sharon Davis, William J.M. Hrushesky
Manuscript writing: All authors
Final approval of manuscript: All authors
References
- 1.Freifeld AG, Bow EJ, Sepkowitz KA, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2011;52:e56–e93. doi: 10.1093/cid/cir073. [DOI] [PubMed] [Google Scholar]
- 2.Viscoli C, Varnier O, Machetti M. Infections in patients with febrile neutropenia: Epidemiology, microbiology, and risk stratification. Clin Infect Dis. 2005;40(suppl 4):S240–S245. doi: 10.1086/427329. [DOI] [PubMed] [Google Scholar]
- 3.Neupogen patient package insert. http://www.fda.gov/downloads/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/ApprovalApplications/TherapeuticBiologicApplications/ucm094437.pdf.
- 4.Neulasta patient package insert. http://www.fda.gov/ohrms/dockets/ac/05/briefing/2005-4185B1_03_10-FDA-Tab5c.pdf.
- 5.Caggiano V, Weiss RV, Rickert TS, et al. Incidence, cost, and mortality of neutropenia hospitalization associated with chemotherapy. Cancer. 2005;103:1916–1924. doi: 10.1002/cncr.20983. [DOI] [PubMed] [Google Scholar]
- 6.Lyman GH, Michels SL, Reynolds MW, et al. Risk of mortality in patients with cancer who experience febrile neutropenia. Cancer. 2010;116:5555–5563. doi: 10.1002/cncr.25332. [DOI] [PubMed] [Google Scholar]
- 7.Timmer-Bonte JN, Adang EM, Smit HJ, et al. Cost-effectiveness of adding granulocyte colony-stimulating factor to primary prophylaxis with antibiotics in small-cell lung cancer. J Clin Oncol. 2006;24:2991–2997. doi: 10.1200/JCO.2005.04.3281. [DOI] [PubMed] [Google Scholar]
- 8.Lathia N, Mittmann N, DeAngelis C, et al. Evaluation of direct medical costs of hospitalization for febrile neutropenia. Cancer. 2010;116:742–748. doi: 10.1002/cncr.24773. [DOI] [PubMed] [Google Scholar]
- 9.Crawford J, Ozer H, Stoller R, et al. Reduction by granulocyte colony-stimulating factor of fever and neutropenia induced by chemotherapy in patients with small-cell lung cancer. N Engl J Med. 1991;325:164–170. doi: 10.1056/NEJM199107183250305. [DOI] [PubMed] [Google Scholar]
- 10.Kuderer NM, Dale DC, Crawford J, et al. Impact of primary prophylaxis with granulocyte colony-stimulating factor on febrile neutropenia and mortality in adult cancer patients receiving chemotherapy: A systematic review. J Clin Oncol. 2007;25:3158–3167. doi: 10.1200/JCO.2006.08.8823. [DOI] [PubMed] [Google Scholar]
- 11.National Comprehensive Cancer Network Guidelines Version 1.2011. hhttp://www.nccn.org/professionals/physician_gls/f_guidelines.asp.
- 12.Ozer H, Armitage JO, Bennett CL, et al. 2000 update of recommendations for the use of hematopoietic colony-stimulating factors: Evidence-based, clinical practice guidelines—American Society of Clinical Oncology Growth Factors Expert Panel. J Clin Oncol. 2000;18:3558–3585. doi: 10.1200/JCO.2000.18.20.3558. [DOI] [PubMed] [Google Scholar]
- 13.Smith TJ, Khatcheressian, Lyman GH, et al. 2006 update of recommendations for the use of white blood cell growth factors: An evidence-based clinical practice guideline. J Clin Oncol. 2006;24:3187–3205. doi: 10.1200/JCO.2006.06.4451. [DOI] [PubMed] [Google Scholar]
- 14.Aapro MS, Bohlius J, Cameron DA, et al. 2010 update of EORTC guidelines for the use of granulocyte-colony stimulating factor to reduce the incidence of chemotherapy-induced febrile neutropenia in adult patients with lymphoproliferative disorders and solid tumours. Eur J Cancer. 2011;47:8–32. doi: 10.1016/j.ejca.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 15.Schiller JH, Harrington D, Belani CP, et al. Comparison of four chemotherapy regimens for advanced non-small cell lung cancer. N Engl J Med. 2002;346:92–98. doi: 10.1056/NEJMoa011954. [DOI] [PubMed] [Google Scholar]
- 16.Sandler A, Gray R, Perry MC, et al. Paclitaxel-carboplatin alone or with bevacizumab for non–small-cell lung cancer. N Engl J Med. 2006;355:2542–2550. doi: 10.1056/NEJMoa061884. [DOI] [PubMed] [Google Scholar]
- 17.Choi IS, Kim BS, Park SR, et al. Efficacy of modified regimen with attenuated doses of paclitaxel plus carboplatin combination chemotherapy in elderly and/or weak patients with advanced non-small cell lung cancer. Lung Cancer. 2003;39:99–101. doi: 10.1016/s0169-5002(02)00389-6. [DOI] [PubMed] [Google Scholar]
- 18.Thomas P, Castelnau O, Paillotin D, et al. Phase II trial of paclitaxel and carboplatin in metastatic small-cell lung cancer: A Groupe Français de Pneumo-Cancérologie study. J Clin Oncol. 2001;19:1320–1325. doi: 10.1200/JCO.2001.19.5.1320. [DOI] [PubMed] [Google Scholar]
- 19.Giorgio CG, Kawaquchi T, Crowley J, et al. A phase II study of carboplatin and paclitaxel as first line chemotherapy in elderly patients with advanced non-small cell lung cancer (NSCLC) Lung Cancer. 2006;51:357–362. doi: 10.1016/j.lungcan.2005.10.023. [DOI] [PubMed] [Google Scholar]
- 20.Langer C, Leighton JC, Comis RL, et al. Paclitaxel and carboplatin in combination in the treatment of advanced non–small-cell lung cancer: A phase II toxicity, response, and survival analysis. J Clin Oncol. 2005;13:1860–1870. doi: 10.1200/JCO.1995.13.8.1860. [DOI] [PubMed] [Google Scholar]
- 21.Ohe Y, Ohashi Y, Kubota K, et al. Randomized phase III study of cisplatin plus irinotecan versus carboplatin plus paclitaxel, cisplatin plus gemcitabine, and cisplatin plus vinorelbine for advanced non-small-cell lung cancer: Four-arm cooperative study in Japan. Ann Oncol. 2007;18:317–323. doi: 10.1093/annonc/mdl377. [DOI] [PubMed] [Google Scholar]
- 22.Gandara DR, Kawaguchi T, Crowley J, et al. Japanese-US common-arm analysis of paclitaxel plus carboplatin in advanced non–small-cell lung cancer: A model for assessing population-related pharmacogenomics. J Clin Oncol. 2009;27:3540–3546. doi: 10.1200/JCO.2008.20.8793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jones SE, Castelnau O, Paillotin D, et al. Phase III trial comparing doxorubicin plus cyclophosphamide with docetaxel plus cyclophosphamide as adjuvant therapy for operable breast cancer. J Clin Oncol. 2006;24:5381–5387. doi: 10.1200/JCO.2006.06.5391. [DOI] [PubMed] [Google Scholar]
- 24.Jones SE, Holmes FA, O'Shaughnessy J, et al. Docetaxel with cyclophosphamide is associated with an overall survival benefit compared with doxorubicin and cyclophosphamide: 7-year follow-up of US Oncology Research Trial 9735. J Clin Oncol. 2009;27:1177–1183. doi: 10.1200/JCO.2008.18.4028. [DOI] [PubMed] [Google Scholar]
- 25.Vandenberg T, Younus J, Al-Khayyat S. Febrile neutropenia rates with adjuvant docetaxel and cyclophosphamide chemotherapy in early breast cancer: Discrepancy between published reports and community practice—A retrospective analysis. Curr Oncol. 2010;17:2–3. doi: 10.3747/co.v17i2.498. [DOI] [PMC free article] [PubMed] [Google Scholar]