Abstract
Acute ankle injuries are among the most common injuries in emergency departments. However, there are still no standardized examination procedures or evidence-based treatment. Therefore, the aim of this study was to systematically search the current literature, classify the evidence, and develop an algorithm for the diagnosis and treatment of acute ankle injuries. We systematically searched PubMed and the Cochrane Database for randomized controlled trials, meta-analyses, systematic reviews or, if applicable, observational studies and classified them according to their level of evidence. According to the currently available literature, the following recommendations have been formulated: i) the Ottawa Ankle/Foot Rule should be applied in order to rule out fractures; ii) physical examination is sufficient for diagnosing injuries to the lateral ligament complex; iii) classification into stable and unstable injuries is applicable and of clinical importance; iv) the squeeze-, crossed leg- and external rotation test are indicative for injuries of the syndesmosis; v) magnetic resonance imaging is recommended to verify injuries of the syndesmosis; vi) stable ankle sprains have a good prognosis while for unstable ankle sprains, conservative treatment is at least as effective as operative treatment without the related possible complications; vii) early functional treatment leads to the fastest recovery and the least rate of reinjury; viii) supervised rehabilitation reduces residual symptoms and re-injuries. Taken these recommendations into account, we present an applicable and evidence-based, step by step, decision pathway for the diagnosis and treatment of acute ankle injuries, which can be implemented in any emergency department or doctor's practice. It provides quality assurance for the patient and promotes confidence in the attending physician.
Key words: ankle injury, ankle sprain, evidence based algorithm, diagnosis, treatment.
Introduction
Acute injuries of the ankle are among the most common injuries of the musculo-skeletal system.1 It has been estimated that about one ankle sprain occurs per 10,000 people each day in Western countries.2–4 In sport, the incidence is even higher.5–7 Sixteen to 21% of all sports related injuries are sprained ankles.4,8 In 77–99% X-rays are taken,9,10 although in only 9–15% a fracture of the ankle or foot is present.10–12 Consequently, soft tissue injuries are the most common and the majority of X-rays are not essential. Approximately 85% of sprained ankles involve the lateral ligament complex.5,13,14 In about 65% it is an isolated injury of the anterior talofibulare ligament (ATFL), in 20% both the ATFL and the calcaneofibular ligament (CFL) are involved.15–17 Injuries of the posterior talofibular ligament (PTFL) are rare, and are only caused by severe dislocation of the ankle joint.18,19 Sprains of the deltoid ligament are usually associated with a fibular fracture and a tear of the tibiofibular syndesmosis.20–23 Isolated injuries of the talofibular syndesmotic complex are very uncommon.23–25 Because the injuries of the lateral ligament complex are by far the most common, and the number of patients with residual symptoms is 10–30%,5,26,27 we focus on their treatment. While it is widely agreed that a slight injury to the lateral ligament complex recovers quickly with non-operative management and have an excellent prognosis,4,28–30 there is still controversy about the best treatment for severe ankle sprains. Although many studies are available, their quality is often flawed and comparability is poor. Diagnostic tools to verify the severity of the injury are inconsistent, some authors use stress radiography or arthroscopy while others use clinical examination. Between studies, different grades of injuries are included and varying systems of classifications are used. Times for follow up and endpoints differ, i.e. time to return to sport/work, recurrence rate, persistent pain, range of motion or subjective/functional instability. The duration and character of treatment that will follow surgery differ. This inconsistency makes comparability difficult. Since ankle injuries are common, and there are numerous residual symptoms after ankle sprains, it is crucial to institute a standardized and evidence-based approach to diagnosis and treatment, based on the current literature, in order to provide the best treatment available.
Consequently, the aim of the present study was to systematically search the current literature, classify the evidence, and develop an algorithm for diagnosis and treatment of acute ankle injuries based on these findings. The questions addressed were the following: i) which diagnostic tools are required to identify fractures of the ankle, and ligament injuries? ii) how should injuries of the lateral complex be classified? iii) should injuries of the lateral ligament complex be treated surgically, by immobilization or with functional treatment? iv) which functional treatment is the most beneficial? v) what other treatments can positively influence the course of acute ankle ligament injuries?
This study presents a transparent algorithm with clear decision rules for the diagnosis and treatment of acute ankle injuries based on the currently available trials.
Materials and Methods
We conducted an extensive search in PubMed from its inception to March 2010 for the keywords ankle sprain, and a Mesh search for ankle injuries, AND diagnosis, OR therapy, OR classification, OR therapy, OR rehabilitation. Limits were validation studies, guidelines, comparative studies, reviews, randomized controlled trial, practise guidelines, meta-analyses, clinical trials, humans, English, German. Biomechanical and cadaver studies were excluded. The Cochrane Database was then searched for ankle sprain. First, possibly eligible publications were identified by title. Selected abstracts of articles written in English or German were reviewed by 2 independent reviewers. The selected articles were retrieved and further analyzed. The reference lists of all retrieved papers were then searched manually for unidentified publications according to the initial search strategy. Randomized controlled trials (RCT), meta-analyses (MA) and systematic reviews (SR) of such trials were selected. If the issue was not suitable for testing in a randomized format, such as comparison of different diagnostic procedures, observational studies (OS) were included. Inclusion criteria required that the manuscript addressed at least one of the questions stated above (Figure 1). All studies were evaluated by 2 reviewers, one senior consultant and one senior resident, and graded according to the Eastern Association for the Surgery of Trauma (EAST, http://www.east.org) (Table 1). Class I evidence was considered to be that from prospective randomized controlled trials while class II evidence was derived from prospective clinical studies and retrospective analyses based on clearly reliable data, all other evidence was considered class III. Following the predefined questions stated above one at a time, only the studies with the highest class of scientific evidence available were selected. Thereafter, a synthesis of the results was made answering each individual question. According to the results of the trials available, a level I recommendation was given if consistent class I evidence was available, or based on class II evidence if the issue was not suitable for testing in a randomized format. Level II recommendation was given based on class II evidence. No recommendation was given if no class I or II evidence was available. Based on the level of evidence, we developed an algorithm for the diagnostic procedures required and the treatment of acute ankle injuries.
Figure 1.
Flow chart for selecting articles to be included in the study.
Table 1. Grade of scientific evidence and level of evidence according to the Eastern Association for the Surgery of Trauma (EAST) (2001).
| Grade of scientific evidence | |
|---|---|
| Class I | Prospective randomized controlled trials - may be poorly designed, have inadequate numbers, or suffer from other methodological inadequacies |
| Class II | Prospective clinical studies and retrospective analyses based on clearly reliable data (observational studies, cohort studies, prevalence studies and case control studies) |
| Class III | Retrospective studies (clinical series, database or registry review, large series of case reviews, expert opinion) |
| Level of recommendation | |
|---|---|
| Level 1 | Convincingly justifiable based on the available scientific information, usualli Class I data or strong Class II evidence, especially if the issue does not lend itself to testing in a randomized format. Conversely, low quality or contradictory Class I data may not be able to support a level 1 recommendation. |
| Level 2 | Reasonably justifiable by available scientific evidence and strongly supported by experts opinion. Usually supported by Class II data or a preponderance of Class III evidence. |
| Level 3 | Supported by available data but adequate scientific evidence is lacking, generally Class III data. Useful for educational purposes and in guiding future clinical research. |
Results
Which diagnostic tools are required to identify fractures of the ankle and ligament injuries?
Medical history
Questioning should identify the exact mechanism of injury, previous injuries or operative intervention, as well as congenital or acquired instability of the ankle joint.
X-rays
Before extended physical examination, fractures must be excluded. Therefore, it is important to decide whether X-rays are required. The Ottawa Ankle Rule (OAR) and Ottawa Foot Rule (OFR) were developed by Stiell et al. to avoid unnecessary X-rays.31–35 The exact areas that must be examined for bone tenderness are shown in Figure 2. Plain X-rays of the ankle should be taken if there is pain in the malleolar zone and any one of the following: i) bone tenderness along the distal 6 cm of the posterior edge of the tibia or tip of the lateral malleolus; ii) bone tenderness along the distal 6 cm of the posterior edge of fibula or tip of the lateral malleolus; iii) inability to bear weight both immediately and in the emergency department for four steps.
Figure 2.
Ottawa foot and ankle rule. Anatomy of the right foot and ankle. The regions that must be examined for bone tenderness are labeled in black. (A–B) Ottawa Ankle Rule. (C–D) Ottawa Foot Rule.
Plain X-rays of the foot should be taken if there is pain in the midfoot zone and any one of the following: i) bone tenderness at the base of the fifth metatarsal; ii) bone tenderness at the navicular bone; iii) inability to bear weight both immediately and in the emergency department for four steps.
If X-rays of the ankle are indicated, the antero-posterior view should be taken with 10–20° internal rotation, in order to evaluate abnormalities of the joint space.36 A meta-analysis of 15,581 patients investigating these decision rules, showed an overall sensitivity of 98% and a specificity of 32%. When applied during the first 48 h after trauma, sensitivity could be increased to 99.6% and specificity reduced to 27.9%. Although developed for application in adults, this meta-analysis found a sensitivity of 99.3% and a specificity of 26.7% in children.37 A meta-analysis evaluating the use of the OAR/OFR specifically in children also found a sensitivity of 98.5% and a reduction of X-rays by 24.8%.38 If no x-rays are indicated the patient must be informed and must aggree with the proceeding. Implementation of these decision rules can lead to tremendous cost savings.39 Many authors consider stress X-rays for diagnosis of sprained ankle to be obsolete.40–43 The procedure is painful and requires at least local anesthesia, otherwise the result is inconclusive. Frost et al. systematically reviewed 7 trials that used open exploration as the gold standard and concluded that the use of stress views for evaluating ankle instability cannot be supported.42 There was an appreciable degree of variability in values defined as normal for the different views (5–30°), and manual or mechanical techniques were used to acquire stress views.42–46 It could not be guaranteed that the injury was worsened by the acquisition of the stress views.47,48
Recommendation: when applied within 48 h after trauma the Ottawa Ankle/Foot Rule proofed to have a sensitivity of 99.6%. These rules can be applied with a similar sensitivity to children older than one year (level I) (Figure 3). Due to the unreliability and the disadvantages associated with obtaining stress views, X-rays are not recommended.
Figure 3.
Algorithm for diagnosis and treatment of acute ankle injuries.
Ligament testing
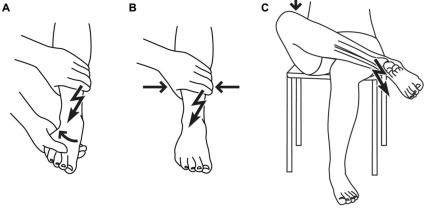
After a fracture has been ruled out, a careful physical examination should be carried out starting with observation of swelling, deformity and ecchymosis, as they are indicative of acute injury. To assess stability of the lateral ankle ligaments, two provocative maneuvers are essential. They must both be performed in comparison with the uninjured leg. If there is increased laxity, the tests are considered positive. The anterior drawer test assesses the integrity of the anterior talofibulare ligament (ATFL).49–51 It is described in detail in Figure 4A. If the ATFL is ruptured, in 50% of cases a dimple sign can be seen in the anterior aspect of the joint.52,53 The talar tilt test for the ATFL and the calcaneofibular ligament (CFL) are shown in Figure 4B.30,50,51 If physical examination is limited due to pain and swelling the patient should be treated with protection, rest, ice, compression, and elevation (PRICE) and physical examination should be performed again after 3–5 days. In two studies, van Dijk et al. compared physical examination and delayed physical examination after 3–5 days of treatment with PRICE with findings indicating the need for surgery in 282 patients. In comparison to stress radiography, arthrography, and sonography, the delayed physical examination produced the best results with a sensitivity of 96% and a specificity of 84%.49,54 In summary, if in doubt after initial physical examination, further examination should be repeated after 3–5 days. A positive stress test, in addition to pain on palpation at the site of ligament, and sign of hematoma have been shown to have a sensitivity of 96% for diagnosing a ruptured ligament. Injury of the syndesmosis requires a longer recovery time and shows more disabling symptoms than a lateral sprain of the ankle.55,56 Patients who have an acute syndesmotic injury present with pain in the anterolateral aspect of the ankle joint that is aggravated by forced dorsal flexion. The anterolateral aspect of the ankle is tender to palpation. Several clinical tests can be used to examine the syndesmosis. The external rotation test according to Frick,57–61 the squeeze test57,62 and the crossed leg test63 are shown in detail in Figure 5. They all have in common that they are considered positive if pain is triggered in the area of the syndesmosis after stress is applied. It must be noted that these tests have been validated only in small numbers of patients, since isolated injuries of the syndesmosis are rare.64 Consequently, no sensitivity has been calculated. Therefore, whenever there is a hint of such an injury, further imaging should be performed, as described below.
Figure 4.
Clinical tests of the lateral ligament complex. (A) The anterior drawer test for the anterior talofibulare ligament (ATFL) is performed with the knee joint flexed. The ankle joint is held in 10–15° plantar flexion, and the clinician presses the heel forward while holding back the tibia. (B) The talar tilt test for the ATFL and calcaneofibular ligament (CFL) is carried out with the ankle in the neutral position. The heel is held stable while inverting the talus and calcaneus on the tibia.
Figure 5.
Clinical tests for injury of the syndesmosis. The tests are considered positive if pain is triggered in the area of the syndesmosis. (A) The external rotation test is performed with the tibia fixed and an external rotation is applied. (B) For the squeeze test, the tibia and fibula are compressed above the midpoint of the calf. (C) For the crossed leg test, the patient places the leg to be tested across the kneecap of the other leg. The pivot point is at the junction of the middle and distal thirds of the tibia and a gentle force is applied on the medial side of the knee by the patient.
Recommendation: in 282 patients, physical examination, and especially delayed examination, demonstrated a sensitivity of 96% when compared to operative findings (Figure 3) (level I). Clinical tests for injuries of the syndesmosis have been validated only in small numbers of patients, since isolated injuries of the syndesmosis are rare (Figure 3) (level II). If in doubt, early MRI should be performed.
Sonography
Sonography is a valuable tool for examining the tendons of the ankle joint such as the Achilles or the peroneal tendons for rupture or displacement.20,44,45 Only a few studies have evaluated the capacity of sonography to diagnose injuries of the lateral ligaments of the ankle. Milz et al. performed sonographic evaluation in 20 patients using MRI as the gold standard with a sensitivity of 92% and a specificity of 83% for injury and rupture of ATFL.65 In 34 patients, sonography was confirmed at arthroscopy with a sensitivity of 100% and a specificity of 33%.66 However, sonographic evaluation is strongly dependent on the expertise of the technician.67 Furthermore, state of the art equipment and examination techniques are the prerequisite to assess ligament integrity.68
Recommendation: the expertise of the technician is of extreme importance for sonographic examination. Furthermore, there is a considerable difference in sensitivity according to the different ligaments and the number of patients in the observational study is low (level III). It is not, therefore, included in the standard protocol.
Arthrography
Rupture of the ATFL can be diagnosed with a sensitivity of 96–100% using arthrography.69–71 For the PTFL, sensitivity decreases to 75% for anatomical reasons.44,70 Further arthrography is invasive and is not able to provide images of the ligament itself, but it is an indirect tool for the diagnosis of rupture. Therefore, it should not be considered a standard tool for diagnosis of ligament rupture in the ankle.
Recommendation: arthrography shows a similar sensitivity only in diagnosing injuries of the ATLF compared to delayed physical examination. It is, however, an invasive procedure and should not, therefore, be recommended for routine practice.
Magnetic resonance imaging
Ruptures of lateral ligaments of the ankle can be diagnosed on MRI with a sensitivity of 75–100%.72–78 However, the clinical course of the injury in terms of osteoarthrosis or chronic instability cannot be estimated.44,79,80 In a prospective series of 95 patients with sprained ankle, there was an incidence of bone bruises in 27%. The presence of a bone bruise on MRI did not influence the clinical course and, therefore, does not require treatment.81 MRI showed a sensitivity of 100% and a specificity of 70–100% for anterior and posterior syndesmosis compared with arthrography.75 Despite the ability of MRI to depict ligamenteous injuries of the ankle, it has limited indications because of the high costs, the high incidence of sprained ankle and the poor availability. It is a particularly powerful tool for patients with chronic instability of the ankle, osteochondral lesions, occult fractures or injuries of the tibiofibular syndesmosis.50,75,82–85 In a prospective trial, arthrography, physical examination, helical CT and MRI were compared in 103 patients for the diagnosis of osteochondral lesions of the talus. Arthroscopy, MRI, and helical CT proved to be equally effective in diagnosing these injuries.86
Recommendation: MRI shows a high sensitivity for diagnosing ligament injuries of the ankle. Due to the high incidence of ankle injuries, the poor availability and high costs it should be limited to chronic instability of the ankle or reasonable suspicion of osteochondral lesions, occult fractures or injuries of the tibiofibular syndesmosis (Figure 3) (level I).
How should injuries of the lateral complex be classified?
There is much confusion in the classification systems for injuries to the ligaments of the lateral ankle. Older texts described a purely anatomical classification, whereas more recent papers have described a more functional system.30,50,87,88 Grade I injuries involve stretched ligaments without macroscopic tearing, little swelling or tenderness, minimal or no functional loss, and no mechanical instability of the joint. A grade II injury is a partial macroscopic tear in the ligament with moderate pain, swelling, and tenderness over the involved structures. There is some loss of joint movement in the joint and mild to moderate instability. A grade III injury is a complete rupture of the ligament with marked swelling, hemorrhage, and tenderness. There is loss of function, and abnormal motion and instability of the joint. We think that these two classification systems are of little value in the emergency department. A more useful approach divides the injuries into stable and unstable injuries5,51,89,90 (Table 2) based on the findings of the anterior drawer test and talar tilt test. A stable injury (grade I) demonstrates no increased laxity in the upper ankle joint, there is no complete tear of any ligament of the lateral complex. Unstable injuries (grades II and III) show increased laxity in the joint under provocative maneuvers. The anterior talofibulare ligament (grade II) and the calcaneofibular ligament (grade III) are ruptured. This classification can be used in the emergency department. Injuries are classified by clinical examination and from our point of view it is most important to decide whether they are stable or unstable.
Table 2. Classification of lateral sprains of the ankle according to the stability of the joint. Swelling and signs of hematoma should be present over the site of the ligament. ATFL, Anterior talofibulare ligament; CFL, calcaneofibulare ligament [5;47;81;82].
| Grade | Hematoma/swelling/pain on palpitation | Anterior drawer test | Talar tilit test | Anatomic lesion | |
|---|---|---|---|---|---|
| I | Positive | Negative | Negative | Incomplete tear of ATFL | Stable |
| II | Positive | Positive | Negative | Complete tear of ATFL | Unstable |
| Incomplete tear of CFL | |||||
| III | Positive | Positive | Positive | Complete tear of ATFL | Unstable |
| Complete tear of CFL |
Recommendation: a classification should allow reproducible and easy grading of the injury without elaborate techniques and also provide relevant information for treatment. Consequently, classification criteria for stable and unstable injuries, based on clinical findings, is the most suitable approach for use in an emergency department or doctor's practice (Figure 3).
Should injuries to the lateral ligament complex be treated by surgery, immobilization or functional treatment?
Because injuries of the lateral ligament complex are by far the most common, we will focus on their treatment. For treatment of injuries to the syndesmosis, systematic reviews and evidence-based guidelines are available.25,36,91 For treatment of fractures, evidence-based approaches are available on http://www.aofoundation.org.
Stable injuries (grade I) of the lateral complex recover quickly with non-surgical management and have an excellent prognosis.4,28–30,40,87,88,92 Here we will focus on the treatment of unstable injuries (grades II and III). Three treatment options are available: surgery, immobilization, and functional treatment. The main goal is to prevent residual symptoms and to provide fast recovery without harm to the patient.
Recommendation: stable injuries of the lateral ligaments of the ankle should be treated using an elastic bandage and protection, rest, ice, compression and elevation (PRICE), since these provide a good prognosis (Figure 3) (level I).
Surgery compared with conservative treatment
Kerhoffs et al. compared conservative treatment with surgery in a meta-analysis and stated that the data available failed to show which treatment was superior.93,94 While surgery seemed better for objective stability, there were no differences in subjective instability, range of motion was reduced compared with conservative treatment, and no significant differences were observable in the other outcome measurements. Most trials reported a shorter time to return to normal activities after conservative treatment.4,29,41,93–95 High costs and the significantly higher rate of complications for surgery led the authors to favor conservative treatment. This is in line with the findings of Tiling et al. who systematically reviewed 24 eligible trials and found no significant difference between conservative and surgery. They concluded that there was no need for initial surgical treatment.29 Kannus et al. reported a shorter time to return to sport and work, and a better range of motion in early follow up for conservative treatment.4 Almost all complications in their systematic review occurred in patients who had undergone surgery. This was stated in all reviews and trials analyzed. None of the studies reviewed favored surgery. Shrier et al. identified eight trials in favor of functional treatment and three trials in favor of surgery concerning residual symptoms. All the trials that supported surgery had methodical weaknesses as stated by Shrier. They concluded that primary repair and immobilization in a cast increase short-term disability compared with functional treatment, while comparable results were found during long-term follow up.41 Ogilvie-Harris et al. found significant differences in favor of conservative treatment only for time to return to sport and/or work, otherwise there were no significant differences.96 They concluded, that as no significant benefits were found in favor of surgery, …one could not recommend operative intervention. Pijneburg et al. performed a meta-analysis and included seven trials that compared surgery and conservative treatment.95 They found that surgery was superior only as far as subjective stability was concerned. But they still did not recommend surgery as the treatment of choice due to possible complications, higher costs, and because secondary reconstruction is equally effective to primary reconstruction of the ligaments.95 It must also be noted that the study by Prins et al. was included in their meta-analysis.97 This trial was strongly in favor of surgery and was excluded by many other authors due to methodical shortcomings and the heterogeneous results.4,93,94 Reviews and meta-analyses including this trial should be interpreted with caution. In an RCT, also by Pijneburg et al., objective stability and residual pain were significantly better after surgery. Again, the authors conclude that surgery should not be the treatment of choice due to higher costs, possible complications and since secondary reconstruction produces results comparable to primary reconstruction.98–108 There is no evidence to support the suggestion from some authors to adopt a surgical treatment approach for athletes.109–112 There are no randomized controlled trials that compare surgery and functional treatment in elite athletes. However, as time to return to sports has been reported to be shorter for functional treatment, this is favored by most authors also for competitive athletes.4,29,30,41,113–115 All authors agree that complications such as scar tenderness, sensory loss or disturbance, infection, and Sudeck's atrophy, apart from deep vein thrombosis that also develops in immobilized patients, only occur in those patients who underwent surgery.4,29,41,93–95 Follow-up times in the present studies and reviews are too short to draw any conclusions about the development of osteoarthrosis in the ankle joint.
Recommendation: conservative treatment should be favored over surgery due to comparable results with fewer complications after conservative treatment and significantly lower costs. Surgery should, therefore, be reserved for patients with persistent symptoms, particularly since secondary reconstruction of the ruptured ligaments is possible even years after the injury with results equal to those of primary repair (level I).
Functional treatment compared with immobilization
The two approaches to conservative treatment are: i) immobilization, usually using a cast, and ii) functional treatment, with a short period of protection using tape, a bandage, or a brace, followed by early weight-bearing, including exercises and neuromuscular training of the ankle.4 Kerkhoff et al. published a meta-analysis that compared immobilization and functional treatment.19,116 Twenty-one trials met the inclusion criteria and standards. They found no findings concerning outcome in favor of immobilization. However, seven measurements of outcome produced significantly better results in favor of functional treatment. These were: number of patients who returned to sport and work, time to return to sport and work, objective instability, persistent swelling, and patient satisfaction. They concluded that immobilization should no longer be the conservative treatment of choice for patients with acutely sprained ankles. These findings are in line with reviews by Kannus et al.,4 Jones et al.,117 and Tiling et al.,29 who found that the time to return to sport/work was significantly shorter for functional treatment. Kannus et al. stated …it is not difficult to select functional treatment as the treatment of choice for acute complete tears of the lateral ligaments of the ankle.4 Shrier et al. showed that functional treatment resulted in a shorter period of disability, whereas no studies were found supporting immobilization41. Pijneburg et al. found significantly less residual pain, better subjective stability and less time before return to work (15 compared with 38 days) for functional treatment.95 Ogilvie-Harris et al. included fourteen RCT for their review, eight of which showed significant differences in favor of functional treatment.96 This is supported by the results of the RCT by Ardevol et al. with results favoring functional treatment.118 One recent RCT by Lamb et al., promoted the use of a cast for treatment of acutely sprained ankles.119 But this trial suffers from various shortcomings and failed to compare the different methods of immobilization with the current gold standard, i.e. functional treatment. Therefore, this trial does not contribute to the ongoing debate about the best treatment for acutely sprained ankles.120–122 A further disadvantage of immobilization is that prophylaxis of thrombosis is mandatory while this is not mandatory in functional treatment.123 Further, immobilization causes atrophy of musculature which is of special concern for a return to sporting activity,30 and direct and indirect costs of functional treatment are lower than those of immobilization.124
Recommendation: there is consistent evidence that functional treatment should be considered the treatment of choice. It leads to a faster recovery with greater patient satisfaction at lower costs (Figure 3) (level I).
Which functional treatment is most beneficial?
Functional treatment includes a short period of protection with tape, bandage, or an ankle brace, and allows early weight-bearing. Exercises for range of motion, and neuromuscular training of the ankle, should begin as early as possible.4 Initial management involves control of pain, swelling, and maintenance of range of motion. Consequently PRICE (protection, rest, ice, compression, and elevation) is appropriate in the acute stage to achieve these goals.125 This should be followed by early range of motion exercises, which should, at least partly, be supervised, and proprioceptive treatment (e.g. using a balance board). In a meta-analysis by Kerkhoff et al. taping caused skin irritations, mainly itching and eczema. A semi-rigid ankle brace, compared with an elastic bandage, is associated with less time before return to work/sport and less subjective instability in short-term follow up. Lace-up ankle supports reduced persistent swelling better than a semi-rigid ankle brace. However, there are not sufficient data available to allow definitive conclusions to be drawn.126,127 Boyce et al. supported the use of a semi-rigid ankle brace instead of an elastic bandage.128 The findings of Beynnon et al. propose, that the use of an elastic bandage, combined with a semi-rigid ankle brace, could further reduce the time needed to return to sport/work.129 Wearing external ankle support could significantly reduce the number of ankle sprains, especially among subjects with a previous history of such an injury.130,131 Proprioceptive training seems to be effective in reducing residual symptoms and further injuries.132–136 In a systematic review, Zoch et al. concluded that specialized training is the most effective method for restoring range of motion and proprioception. Further isokinetic training increased the strength of the injured leg.64 Karlsson et al. showed that early functional treatment could significantly reduce the time to return to sport/work.137 A systematic review by Van Os et al. found evidence, although limited, that functional treatment combined with supervised rehabilitation training is superior to functional treatment alone as far as persistent swelling and time to return to work are concerned.138 Mohammadi et al.,139 Hupperets et al.,140 Handoll et al.,130 McKeon et al.141 and Holme et al.142 reported a significant reduction in further injuries as a result of proprioceptive rehabilitation training. The study by van Rijn et al. could not identify significant differences between supervised rehabilitation compared to home rehabilitation alone, but conclude …there is a slight possibility that usual care combined with supervised exercises is the preferred treatment option for this population.143 This is in line with the findings of Bassett et al.144 Overall, there is a consensus about the importance of ankle support, rehabilitation and proprioceptive training to improve short-term symptoms and to reduce reoccurrence of ankle sprains.64,125,130,135–137,140,141,145–149 Initial treatment of a sprained ankle using a semi-rigid ankle brace is more expensive than that using an elastic bandage. However, reduced time to return to work means that socioeconomic savings may be high.150 Leandersson et al. found the use of a semi-rigid ankle brace could lead to potential economic savings in Sweden as high as 8 million US dollars per year.151
Recommendation: ankle braces are more convenient and cost effective than tape or elastic bandage. Furthermore, supervised rehabilitation was also shown to reduce time to return to sport and/or work. Consequently, unstable ankle sprains should be treated by early functional treatment using a semi-rigid ankle brace and supervised rehabilitation (Figure 3) (level II).
What other treatments can positively influence the course of acute ankle ligament injuries?
Cryotherapy
Cryotherapy has been proved to be effective in the treatment of soft tissue injuries.96,152–155 The quality of studies of sprained ankles is poor, as cryotherapy has usually been combined with other treatments. However, it seems to reduce swelling and the need for pain killers, particularly when used soon after the injury, and it should, therefore, be part of the initial standard regimes.96,154–156 Furthermore, it improves reliability of the clinical examination.49,54 The duration, frequencies and the technique of ice application remains controversial.154,157,158
Recommendation: cryotherapy is effective in reducing pain and swelling in acute injuries of the soft tissues, especially when applied soon after the injury for 3–5 days (Figure 3) (level I).
Drug treatment
Ogilvie-Harris et al. reviewed 18 RCTs, and concluded that the use of non-steroidal anti-inflammatory drugs (NSAID) leads to a significant reduction in pain at short-term follow up. No particular NSAID (diclofenac, ibuprofen, piroxicam, diflunisal, or celecoxib) was superior to any of the others. Their review provided reasonable evidence that patients recovered faster and with less pain when treated with NSAID.96 Most other RCTs and systematic reviews found significant differences in favor of NSAIDs for short-term follow ups concerning pain relief.158–162 A few studies could not find any significant differences between NSAID and placebo during short-term follow up.3,163–165 During long-term follow up, no significant differences could be observed for the different treatment groups in any of the studies. So far there is some evidence that comfrey root ointment also can improve short-term symptoms.158,166 Hydrolytic enzymes treatment did not show to be superior to placebo treatment.167
Recommendation: NSAIDs reduce pain during short-term follow up. In addition to cryotherapy, they should be applied when treating acute ankle injuries for 3–7 days (Figure 3) (level I).
Other treatments
Laser therapy,158,168 ultrasound,158,169–172 electrotherapy,158 homeopathic therapy, hyperbaric oxygen therapy,173 prolotherapy, platelet rich plasma, hyaluronic acid174 or topical nitroglycerin injection175 were not effective, or available data were insufficient to prove their benefit in the treatment of acute ankle injuries. In order too prove their benefit, new treatment options must be superior to placebo and to the current gold standarrd, i.e. functional treatment. Consequently, they should not be part of a standard protocol for treatment of acute ankle sprains.19,125
Recommendation: so far, none of these treatments have been shown to enhance recovery from acute ankle injuries. Therefore, they should not be considered as part of the standard regime in treating acute ankle injuries.
Conclusions
Although current literature concerning acute ankle sprains is partly inconclusive and difficult to compare we extracted distinct trends in diagnosing and treatment of such injuries, and evaluated the level of evidence of the current literature. Based on these findings, we developed a comprehensive algorithm (Figure 3) with simple step by step decision rules. Using this algorithm helps to ensure quality of treatment. It can be easily implemented in any emergency department or doctor's practice. By application of the Ottawa Foot and Ankle Rule, the number of X-rays can be significantly reduced. Physical examination is sufficient for the diagnosis of soft tissue damage. Classification into stable and unstable injuries seems to be the most practical and important approach. MRI should be performed if symptoms persist or if there is evidence of injury to the syndesmosis. To treat injury to the lateral ligaments of the ankle, functional treatment is currently the treatment of choice, this should consist of PRICE, NSAID, early weight-bearing, and exercises for range of motion. For unstable injuries (grades II and III), a semi-rigid ankle brace and supervised rehabilitation should be provided. Operative treatment is recommended in cases of chronic instability only. Based on the currently available studies, this algorithm is safe and effective for diagnosing and treating acute ankle injuries. The algorithm is currently being validated in our department. Development of the algorithm is transparent and, therefore, helps in the decision process when choosing the most appropriate diagnostic procedure and treatment.
Acknowledgments:
thanks to Hella Maren Thun and Maximilian Saller; who designed all figures. Thanks also to Birgit Lansherr for acquisition of all eligible articles from various libraries.
References
- 1.Boruta PM, Bishop JO, Braly WG, Tullos HS. Acute lateral ankle ligament injuries: a literature review. Foot Ankle. 1990;11:107–13. doi: 10.1177/107110079001100210. [DOI] [PubMed] [Google Scholar]
- 2.Brooks SC, Potter BT, Rainey JB. Treatment for partial tears of the lateral ligament of the ankle: a prospective trial. Br Med J. 1981;282:606–7. doi: 10.1136/bmj.282.6264.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCulloch PG, Holden P, Robson DJ, et al. The value of mobilisation and non-steroidal anti-inflammatory analgesia in the management of inversion injuries of the ankle. Br J Clin Pract. 1985;39:69–72. [PubMed] [Google Scholar]
- 4.Kannus P, Renstrom P. Treatment for acute tears of the lateral ligaments of the ankle. Operation, cast, or early controlled mobilization. J Bone Joint Surg Am. 1991;73:305–12. [PubMed] [Google Scholar]
- 5.Ferran NA, Maffulli N. Epidemiology of sprains of the lateral ankle ligament complex. Foot Ankle Clin. 2006;11:659–62. doi: 10.1016/j.fcl.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Valderrabano V, Leumann A, Pagenstert G, et al. Chronic ankle instability in sports - a review for sports physicians. Sportverletz Sportschaden. 2006;20:177–83. doi: 10.1055/s-2006-927330. [DOI] [PubMed] [Google Scholar]
- 7.Fong DT, Hong Y, Chan LK, et al. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37:73–94. doi: 10.2165/00007256-200737010-00006. [DOI] [PubMed] [Google Scholar]
- 8.Maehlum S, Daljord OA. Acute sports injuries in Oslo: a one-year study. Br J Sports Med. 1984;18:181–85. doi: 10.1136/bjsm.18.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cameron C, Naylor CD. No impact from active dissemination of the Ottawa Ankle Rules: further evidence of the need for local implementation of practice guidelines. CMAJ. 1999;160:1165–8. [PMC free article] [PubMed] [Google Scholar]
- 10.Auleley GR, Kerboull L, Durieux P, et al. Validation of the Ottawa ankle rules in France: a study in the surgical emergency department of a teaching hospital. Ann Emerg Med. 1998;32:14–8. doi: 10.1016/s0196-0644(98)70093-9. [DOI] [PubMed] [Google Scholar]
- 11.Dunlop MG, Beattie TF, White GK, et al. Guidelines for selective radiological assessment of inversion ankle injuries. Br Med J. 1986;293:603–5. doi: 10.1136/bmj.293.6547.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Keogh SP, Shafi A, Wijetunge DB. Comparison of Ottawa ankle rules and current local guidelines for use of radiography in acute ankle injuries. J R Coll Surg Edinb. 1998;43:341–3. [PubMed] [Google Scholar]
- 13.Orthopädie Debrunner A.M., Orthopädische Chirurgie. Bern, Göttingen. Toronto, Seattle: Verlag Hans Huber; 2002. pp. 1113–21. [Google Scholar]
- 14.Garrick JG. The frequency of injury, mechanism of injury, and epidemiology of ankle sprains. Am J Sports Med. 1977;5:241–2. doi: 10.1177/036354657700500606. [DOI] [PubMed] [Google Scholar]
- 15.Brostrom L. Sprained ankles. I. Anatomic lesions in recent sprains. Acta Chir Scand. 1964;128:483–95. [PubMed] [Google Scholar]
- 16.Brostrom L. Sprained ankles. V. Treatment and prognosis in recent ligament ruptures. Acta Chir Scand. 1966;132:537–50. [PubMed] [Google Scholar]
- 17.Brostrom L. Sprained ankles. VI. Surgical treatment of “chronic” ligament ruptures. Acta Chir Scand. 1966;132:551–65. [PubMed] [Google Scholar]
- 18.Brostrom L. Sprained ankles. III. Clinical observations in recent ligament ruptures. Acta Chir Scand. 1965;130:560–9. [PubMed] [Google Scholar]
- 19.Kerkhoffs GM, Rowe BH, Assendelft WJ, et al. Immobilisation and functional treatment for acute lateral ankle ligament injuries in adults. Cochrane Database Syst Rev. 2002 doi: 10.1002/14651858.CD003762.CD003762 [DOI] [PubMed] [Google Scholar]
- 20.Sofka CM, Pavlov H. Sports injury update: imaging features. Curr Probl Diagn Radiol. 2001;30:174–87. doi: 10.1067/mdr.2001.115293. [DOI] [PubMed] [Google Scholar]
- 21.Seiler H. The upper ankle joint. Biomechanics and functional anatomy. Orthopade. 1999;28:460–8. doi: 10.1007/s001320050372. [DOI] [PubMed] [Google Scholar]
- 22.Linklater J. Ligamentous, chondral, and osteochondral ankle injuries in athletes. Semin Musculoskelet Radiol. 2004;8:81–98. doi: 10.1055/s-2004-823016. [DOI] [PubMed] [Google Scholar]
- 23.Tintinalli JE. Emergency Medicine. In: Kelen GD, Stapczynski JS, editors. A Com-prehensive Study Guide. 6th ed. McGraw-Hill; 2003. pp. 1736–142. [Google Scholar]
- 24.Xenos JS, Hopkinson WJ, Mulligan ME, et al. The tibiofibular syndesmosis. Evaluation of the ligamentous structures, methods of fixation, and radiographic assessment. J Bone Joint Surg Am. 1995;77:847–56. doi: 10.2106/00004623-199506000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Williams GN, Jones MH, Amendola A. Syndesmotic ankle sprains in athletes. Am J Sports Med. 2007;35:1197–207. doi: 10.1177/0363546507302545. [DOI] [PubMed] [Google Scholar]
- 26.Karlsson J, Lansinger O. Lateral instability of the ankle joint. Clin Orthop Relat Res. 1992:253–61. [PubMed] [Google Scholar]
- 27.Peters JW, Trevino SG, Renstrom PA. Chronic lateral ankle instability. Foot Ankle. 1991;12:182–91. doi: 10.1177/107110079101200310. [DOI] [PubMed] [Google Scholar]
- 28.Klein J, Rixen D, Albring T, Tiling T. Functional versus plaster cast treatment of acute rupture of the fibular ligament of the upper ankle joint. A randomized clinical study. Unfallchirurg. 1991;94:99–104. [PubMed] [Google Scholar]
- 29.Tiling T, Bonk A, Hoher J, Klein J. Acute injury to the lateral ligament of the ankle joint in the athlete. Chirurg. 1994;65:920–33. [PubMed] [Google Scholar]
- 30.Lynch SA, Renstrom PA. Treatment of acute lateral ankle ligament rupture in the athlete. Conservative versus surgical treatment. Sports Med. 1999;27:61–71. doi: 10.2165/00007256-199927010-00005. [DOI] [PubMed] [Google Scholar]
- 31.Stiell I, Wells G, Laupacis A, et al. Multicentre trial to introduce the Ottawa ankle rules for use of radiography in acute ankle injuries. Multicentre Ankle Rule Study Group. BMJ. 1995;311:594–7. doi: 10.1136/bmj.311.7005.594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stiell IG, Greenberg GH, McKnight RD, et al. A study to develop clinical decision rules for the use of radiography in acute ankle injuries. Ann Emerg Med. 1992;21:384–90. doi: 10.1016/s0196-0644(05)82656-3. [DOI] [PubMed] [Google Scholar]
- 33.Stiell IG, McKnight RD, Greenberg GH, et al. Interobserver agreement in the examination of acute ankle injury patients. Am J Emerg Med. 1992;10:14–7. doi: 10.1016/0735-6757(92)90117-g. [DOI] [PubMed] [Google Scholar]
- 34.Stiell IG, Greenberg GH, McKnight RD, et al. Decision rules for the use of radiography in acute ankle injuries. Refinement and prospective validation. JAMA. 1993;269:1127–32. doi: 10.1001/jama.269.9.1127. [DOI] [PubMed] [Google Scholar]
- 35.Stiell IG, McKnight RD, Greenberg GH, et al. Implementation of the Ottawa ankle rules. JAMA. 1994;271:827–32. [PubMed] [Google Scholar]
- 36.Rammelt S, Zwipp H, Grass R. Injuries to the distal tibiofibular syndesmosis: an evidence-based approach to acute and chronic lesions. Foot Ankle Clin. 2008;13:611–611. doi: 10.1016/j.fcl.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 37.Bachmann LM, Kolb E, Koller MT, et al. Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: systematic review. BMJ. 2003;326:417–417. doi: 10.1136/bmj.326.7386.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dowling S, Spooner CH, Liang Y, et al. Accuracy of Ottawa Ankle Rules to exclude fractures of the ankle and midfoot in children: a meta-analysis. Acad Emerg Med. 2009;16:277–87. doi: 10.1111/j.1553-2712.2008.00333.x. [DOI] [PubMed] [Google Scholar]
- 39.Anis AH, Stiell IG, Stewart DG, Laupacis A. Cost-effectiveness analysis of the Ottawa Ankle Rules. Ann Emerg Med. 1995;26:422–8. doi: 10.1016/s0196-0644(95)70108-7. [DOI] [PubMed] [Google Scholar]
- 40.Klenerman L. The management of sprained ankle. J Bone Joint Surg Br. 1998;80:11–2. doi: 10.1302/0301-620x.80b1.8037. [DOI] [PubMed] [Google Scholar]
- 41.Shrier I. Treatment of lateral collateral ligament sprains of the ankle: a critical appraisal of the literature. Clin J Sport Med. 1995;5:187–95. doi: 10.1097/00042752-199507000-00009. [DOI] [PubMed] [Google Scholar]
- 42.Frost SC, Amendola A. Is stress radiography necessary in the diagnosis of acute or chronic ankle instability? Clin J Sport Med. 1999;9:40–5. doi: 10.1097/00042752-199901000-00008. [DOI] [PubMed] [Google Scholar]
- 43.Senall JA, Kile TA. Stress radiography. Foot Ankle Clin. 2000;5:165–84. [PubMed] [Google Scholar]
- 44.Breitenseher MJ. Acute ankle injuries. Radiologe. 1999;39:16–24. doi: 10.1007/s001170050471. [DOI] [PubMed] [Google Scholar]
- 45.Breitenseher M, Trattnig S, Kukla C, et al. [Trauma of the ligaments and tendons. Examination technique and detection in MRI] Radiologe. 1995;35:456–62. [PubMed] [Google Scholar]
- 46.Breitenseher MJ. Injury of the ankle joint ligaments. Radiologe. 2007;47:216–23. doi: 10.1007/s00117-006-1442-z. [DOI] [PubMed] [Google Scholar]
- 47.Breitenseher MJ, Trattnig S, Kukla C, et al. Injuries to the lateral ligaments of the ankle joint: study technic and demonstration by means of MRI] Rofo. 1996;164:226–32. doi: 10.1055/s-2007-1015645. [DOI] [PubMed] [Google Scholar]
- 48.Paar O, Kasperk R, Nachtkamp J. Does performance of a stress roentgen image of the upper ankle joint in acute fibular capsule ligament lesion entail an operation? An experimental study. Sportverletz Sportschaden. 1991;5:99–102. doi: 10.1055/s-2007-993571. [DOI] [PubMed] [Google Scholar]
- 49.van Dijk CN, Lim LS, Bossuyt PM, Marti RK. Physical examination is sufficient for the diagnosis of sprained ankles. J Bone Joint Surg Br. 1996;78:958–62. doi: 10.1302/0301-620x78b6.1283. [DOI] [PubMed] [Google Scholar]
- 50.Puffer JC. The sprained ankle. Clin Cornerstone. 2001;3:38–49. doi: 10.1016/s1098-3597(01)90068-7. [DOI] [PubMed] [Google Scholar]
- 51.Chapman MW. Chapman's Orthopedic Surgery. Lippincott Williams and Wilkins (LWW) 2000:2473–83. [Google Scholar]
- 52.Aradi AJ, Wong J, Walsh M. The dimple sign of a ruptured lateral ligament of the ankle: brief report. J Bone Joint Surg Br. 1988;70:327–8. doi: 10.1302/0301-620X.70B2.3126191. [DOI] [PubMed] [Google Scholar]
- 53.van Dijk CN. Management of the sprained ankle. Br J Sports Med. 2002;36:83–4. doi: 10.1136/bjsm.36.2.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.van Dijk CN, Mol BW, Lim LS, et al. Diagnosis of ligament rupture of the ankle joint. Physical examination, arthrography, stress radiography and sonography compared in 160 patients after inversion trauma. Acta Orthop Scand. 1996;67:566–70. doi: 10.3109/17453679608997757. [DOI] [PubMed] [Google Scholar]
- 55.Taylor DC, Englehardt DL, Bassett FH., III Syndesmosis sprains of the ankle. The influence of heterotopic ossification. Am J Sports Med. 1992;20:146–50. doi: 10.1177/036354659202000209. [DOI] [PubMed] [Google Scholar]
- 56.Alonso A, Khoury L, Adams R. Clinical tests for ankle syndesmosis injury: reliability and prediction of return to function. J Orthop Sports Phys Ther. 1998;27:276–84. doi: 10.2519/jospt.1998.27.4.276. [DOI] [PubMed] [Google Scholar]
- 57.Frick H. Diagnosis, therapy and results of acute instability of the syndesmosis of the upper ankle joint (isolated anterior rupture of the syndesmosis) Orthopade. 1986;15:423–6. [PubMed] [Google Scholar]
- 58.Nussbaum ED, Hosea TM, Sieler SD, et al. Prospective evaluation of syndesmotic ankle sprains without diastasis. Am J Sports Med. 2001;29:31–5. doi: 10.1177/03635465010290011001. [DOI] [PubMed] [Google Scholar]
- 59.Beumer A, Swierstra BA, Mulder PG. Clinical diagnosis of syndesmotic ankle instability: evaluation of stress tests behind the curtains. Acta Orthop Scand. 2002;73:667–9. doi: 10.1080/000164702321039642. [DOI] [PubMed] [Google Scholar]
- 60.Boytim MJ, Fischer DA, Neumann L. Syndesmotic ankle sprains. Am J Sports Med. 1991;19:294–8. doi: 10.1177/036354659101900315. [DOI] [PubMed] [Google Scholar]
- 61.Grass R, Herzmann K, Biewener A, Zwipp H. Injuries of the inferior tibiofibular syndesmosis. Unfallchirurg. 2000;103:520–32. [PubMed] [Google Scholar]
- 62.Hopkinson WJ, St Pierre P, Ryan JB, Wheeler JH. Syndesmosis sprains of the ankle. Foot Ankle. 1990;10:325–30. doi: 10.1177/107110079001000607. [DOI] [PubMed] [Google Scholar]
- 63.Kiter E, Bozkurt M. The crossed-leg test for examination of ankle syndesmosis injuries. Foot Ankle Int. 2005;26:187–8. doi: 10.1177/107110070502600213. [DOI] [PubMed] [Google Scholar]
- 64.Zoch C, Fialka-Moser V, Quittan M. Rehabilitation of ligamentous ankle injuries: a review of recent studies. Br J Sports Med. 2003;37:291–5. doi: 10.1136/bjsm.37.4.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Milz P, Milz S, Steinborn M, et al. Lateral ankle ligaments and tibiofibular syndesmosis. 13-MHz high-frequency sonography and MRI compared in 20 patients. Acta Orthop Scand. 1998;69:51–5. doi: 10.3109/17453679809002357. [DOI] [PubMed] [Google Scholar]
- 66.Oae K, Takao M, Uchio Y, Ochi M. Evaluation of anterior talofibular ligament injury with stress radiography, ultrasonography and MR imaging. Skeletal Radiol. 2010;39:41–7. doi: 10.1007/s00256-009-0767-x. [DOI] [PubMed] [Google Scholar]
- 67.Jacobson JA. Musculoskeletal sonography and MR imaging. A role for both imaging methods. Radiol Clin North Am. 1999;37:713–35. doi: 10.1016/s0033-8389(05)70125-1. [DOI] [PubMed] [Google Scholar]
- 68.Peetrons PA, Silvestre A, Cohen M, Creteur V. Ultrasonography of ankle ligaments. Can Assoc Radiol J. 2002;53:6–13. [PubMed] [Google Scholar]
- 69.van Dijk CN, Molenaar AH, Cohen RH, et al. Value of arthrography after supination trauma of the ankle. Skeletal Radiol. 1998;27:256–61. doi: 10.1007/s002560050377. [DOI] [PubMed] [Google Scholar]
- 70.Raatikainen T, Putkonen M, Puranen J. Arthrography, clinical examination, and stress radiograph in the diagnosis of acute injury to the lateral ligaments of the ankle. Am J Sports Med. 1992;20:2–6. doi: 10.1177/036354659202000102. [DOI] [PubMed] [Google Scholar]
- 71.van den Hoogenband CR, van Moppes FI, Stapert JW, Greep JM. Clinical diagnosis, arthrography, stress examination and surgical findings after inversion trauma of the ankle. Arch Orthop Trauma Surg. 1984;103:115–9. doi: 10.1007/BF00389583. [DOI] [PubMed] [Google Scholar]
- 72.Cardone BW, Erickson SJ, Den Hartog BD, Carrera GF. MRI of injury to the lateral collateral ligamentous complex of the ankle. J Comput Assist Tomogr. 1993;17:102–7. doi: 10.1097/00004728-199301000-00019. [DOI] [PubMed] [Google Scholar]
- 73.Verhaven EF, Shahabpour M, Handelberg FW, et al. The accuracy of three-dimensional magnetic resonance imaging in the diagnosis of ruptures of the lateral ligaments of the ankle. Am J Sports Med. 1991;19:583–7. doi: 10.1177/036354659101900605. [DOI] [PubMed] [Google Scholar]
- 74.Breitenseher MJ, Trattnig S, Kukla C, et al. MRI versus lateral stress radiography in acute lateral ankle ligament injuries. J Comput Assist Tomogr. 1997;21:280–5. doi: 10.1097/00004728-199703000-00022. [DOI] [PubMed] [Google Scholar]
- 75.Oae K, Takao M, Naito K, et al. Injury of the tibiofibular syndesmosis: value of MR imaging for diagnosis. Radiology. 2003;227:155–61. doi: 10.1148/radiol.2271011865. [DOI] [PubMed] [Google Scholar]
- 76.Takao M, Ochi M, Oae K, et al. Diagnosis of a tear of the tibiofibular syndesmosis. The role of arthroscopy of the ankle. J Bone Joint Surg Br. 2003;85:324–9. doi: 10.1302/0301-620x.85b3.13174. [DOI] [PubMed] [Google Scholar]
- 77.Kreitner KF, Ferber A, Grebe P, et al. Injuries of the lateral collateral ligaments of the ankle: assessment with MR imaging. Eur Radiol. 1999;9:519–24. doi: 10.1007/s003300050703. [DOI] [PubMed] [Google Scholar]
- 78.Gaebler C, Kukla C, Breitenseher MJ, et al. Diagnosis of lateral ankle ligament injuries. Comparison between talar tilt, MRI and operative findings in 112 athletes. Acta Orthop Scand. 1997;68:286–90. doi: 10.3109/17453679708996703. [DOI] [PubMed] [Google Scholar]
- 79.De Simoni C, Wetz HH, Zanetti M, et al. Clinical examination and magnetic resonance imaging in the assessment of ankle sprains treated with an orthosis. Foot Ankle Int. 1996;17:177–82. doi: 10.1177/107110079601700312. [DOI] [PubMed] [Google Scholar]
- 80.Zanetti M, De Simoni C, Wetz HH, et al. Magnetic resonance imaging of injuries to the ankle joint: can it predict clinical outcome? Skeletal Radiol. 1997;26:82–8. doi: 10.1007/s002560050198. [DOI] [PubMed] [Google Scholar]
- 81.Alanen V, Taimela S, Kinnunen J, et al. Incidence and clinical significance of bone bruises after supination injury of the ankle. A double-blind, prospective study. J Bone Joint Surg Br. 1998;80:513–5. doi: 10.1302/0301-620x.80b3.8404. [DOI] [PubMed] [Google Scholar]
- 82.Cheung Y, Rosenberg ZS. MR imaging of ligamentous abnormalities of the ankle and foot. Magn Reson Imaging Clin N Am. 2001;9:507–31. [PubMed] [Google Scholar]
- 83.Zanetti M, De Simoni C, Hodler J. Magnetic resonance tomography (MRI) of ligament injuries of the upper ankle joint. Sportverletz Sportschaden. 1996;10:58–62. doi: 10.1055/s-2007-993400. [DOI] [PubMed] [Google Scholar]
- 84.Bencardino J, Rosenberg ZS, Delfaut E. MR imaging in sports injuries of the foot and ankle. Magn Reson Imaging Clin N Am. 1999;7:131–49. [PubMed] [Google Scholar]
- 85.Campbell SE, Warner M. MR imaging of ankle inversion injuries. Magn Reson Imaging Clin N Am. 2008;16:1–18. doi: 10.1016/j.mric.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 86.Verhagen RA, Maas M, Dijkgraaf MG, et al. Prospective study on diagnostic strategies in osteochondral lesions of the talus. Is MRI superior to helical CT? J Bone Joint Surg Br. 2005;87:41–6. [PubMed] [Google Scholar]
- 87.Balduini FC, Tetzlaff J. Historical perspectives on injuries of the ligaments of the ankle. Clin Sports Med. 1982;1:3–12. [PubMed] [Google Scholar]
- 88.Balduini FC, Vegso JJ, Torg JS, Torg E. Management and rehabilitation of ligamentous injuries to the ankle. Sports Med. 1987;4:364–80. doi: 10.2165/00007256-198704050-00004. [DOI] [PubMed] [Google Scholar]
- 89.Clanton TO, Porter DA. Primary care of foot and ankle injuries in the athlete. Clin Sports Med. 1997;16:435–66. doi: 10.1016/s0278-5919(05)70034-x. [DOI] [PubMed] [Google Scholar]
- 90.Chorley JN, Hergenroeder AC. Management of ankle sprains. Pediatr Ann. 1997;26:56–64. doi: 10.3928/0090-4481-19970101-11. [DOI] [PubMed] [Google Scholar]
- 91.Amendola A, Williams G, Foster D. Evidence-based approach to treatment of acute traumatic syndesmosis (high ankle) sprains. Sports Med Arthrosc. 2006;14:232–6. doi: 10.1097/01.jsa.0000212329.32969.b8. [DOI] [PubMed] [Google Scholar]
- 92.Lassiter TE, Jr, Malone TR, Garrett WE., Jr Injury to the lateral ligaments of the ankle. Orthop Clin North Am. 1989;20:629–40. [PubMed] [Google Scholar]
- 93.Kerkhoffs GM, Handoll HH, de Bie R, et al. Surgical versus conservative treatment for acute injuries of the lateral ligament complex of the ankle in adults. Cochrane Database Syst Rev. 2007;2 doi: 10.1002/14651858.CD000380.pub2.CD000380 [DOI] [PubMed] [Google Scholar]
- 94.Kerkhoffs GM, Handoll HH, de Bie R, et al. Surgical versus conservative treatment for acute injuries of the lateral ligament complex of the ankle in adults. Cochrane Database Syst Rev. 2002;3 doi: 10.1002/14651858.CD000380.CD000380 [DOI] [PubMed] [Google Scholar]
- 95.Pijnenburg AC, van Dijk CN, Bossuyt PM, Marti RK. Treatment of ruptures of the lateral ankle ligaments: a meta-analysis. J Bone Joint Surg Am. 2000;82:761–73. doi: 10.2106/00004623-200006000-00002. [DOI] [PubMed] [Google Scholar]
- 96.Ogilvie-Harris DJ, Gilbart M. Treatment modalities for soft tissue injuries of the ankle: a critical review. Clin J Sport Med. 1995;5:175–86. doi: 10.1097/00042752-199507000-00008. [DOI] [PubMed] [Google Scholar]
- 97.Prins JG. Diagnosis and treatment of injury to the lateral ligament of the ankle. A comparative clinical study. Acta Chir Scand Suppl. 1978;486:3–149. [PubMed] [Google Scholar]
- 98.Pijnenburg AC, Bogaard K, Krips R, et al. Operative and functional treatment of rupture of the lateral ligament of the ankle. A randomised, prospective trial. J Bone Joint Surg Br. 2003;85:525–30. doi: 10.1302/0301-620x.85b4.13928. [DOI] [PubMed] [Google Scholar]
- 99.Chrisman OD, Snook GA. Reconstruction of lateral ligament tears of the ankle. An experimental study and clinical evaluation of seven patients treated by a new modification of the Elmslie procedure. J Bone Joint Surg Am. 1969;51:904–12. [PubMed] [Google Scholar]
- 100.Evans GA, Hardcastle P, Frenyo AD. Acute rupture of the lateral ligament of the ankle. To suture or not to suture? J Bone Joint Surg Br. 1984;66:209–12. doi: 10.1302/0301-620X.66B2.6368563. [DOI] [PubMed] [Google Scholar]
- 101.Karlsson J, Bergsten T, Lansinger O, Peterson L. Reconstruction of the lateral ligaments of the ankle for chronic lateral instability. J Bone Joint Surg Am. 1988;70:581–8. [PubMed] [Google Scholar]
- 102.Snook GA, Chrisman OD, Wilson TC. Long-term results of the Chrisman-Snook operation for reconstruction of the lateral ligaments of the ankle. J Bone Joint Surg Am. 1985;67:1–7. [PubMed] [Google Scholar]
- 103.St Pierre R, Allman F, Jr, Bassett FH, III, et al. A review of lateral ankle ligamentous reconstructions. Foot Ankle. 1982;3:114–23. doi: 10.1177/107110078200300211. [DOI] [PubMed] [Google Scholar]
- 104.Cass JR, Morrey BF, Katoh Y, Chao EY. Ankle instability: comparison of primary repair and delayed reconstruction after long-term follow-up study. Clin Orthop Relat Res. 1985;198:110–7. [PubMed] [Google Scholar]
- 105.Kitaoka HB, Lee MD, Morrey BF, Cass JR. Acute repair and delayed reconstruction for lateral ankle instability: twenty-year follow-up study. J Orthop Trauma. 1997;11:530–5. doi: 10.1097/00005131-199710000-00012. [DOI] [PubMed] [Google Scholar]
- 106.Gould N, Seligson D, Gassman J. Early and late repair of lateral ligament of the ankle. Foot Ankle. 1980;1:84–9. doi: 10.1177/107110078000100206. [DOI] [PubMed] [Google Scholar]
- 107.Sammarco GJ, DiRaimondo CV. Surgical treatment of lateral ankle instability syndrome. Am J Sports Med. 1988;16:501–11. doi: 10.1177/036354658801600513. [DOI] [PubMed] [Google Scholar]
- 108.Noyez JF, Martens MA. Secondary reconstruction of the lateral ligaments of the ankle by the Chrisman-Snook technique. Arch Orthop Trauma Surg. 1986;106:52–6. doi: 10.1007/BF00435653. [DOI] [PubMed] [Google Scholar]
- 109.Clark BL, Derby AC, Power GR. Injuries of the lateral ligament of the ankle. Conservative vs. operative repair. Can J Surg. 1965;8:358–63. [PubMed] [Google Scholar]
- 110.Eggert A, Gruber J, Darda L. Therapy of injuries of the exterior ankle joint ligaments. Randomized study of postoperative therapy and early functional treatment tactics. Unfallchirurg. 1986;89:316–20. [PubMed] [Google Scholar]
- 111.Gronmark T, Johnsen O, Kogstad O. Rupture of the lateral ligaments of the ankle: a controlled clinical trial. Injury. 1980;11:215–8. doi: 10.1016/s0020-1383(80)80046-5. [DOI] [PubMed] [Google Scholar]
- 112.Sommer CJ. The unstable upper ankle joint. Treatment of acute ligament rupture--a review of the literature. Sportverletz Sportschaden. 1996;10:76–8. doi: 10.1055/s-2007-993405. [DOI] [PubMed] [Google Scholar]
- 113.Sommer HM, Arza D. Conservative functional treatment of fibular capsule ligament rupture even in the performance athlete? Sportverletz Sportschaden. 1987;1:25–9. doi: 10.1055/s-2007-993691. [DOI] [PubMed] [Google Scholar]
- 114.Zwipp H, Hoffmann R, Wippermann B, et al. Rupture of the fibular ligament of the upper ankle joint. Orthopade. 1989;18:336–40. [PubMed] [Google Scholar]
- 115.Safran MR, Zachazewski JE, Benedetti RS, et al. Lateral ankle sprains: a comprehensive review part 2: treatment and rehabilitation with an emphasis on the athlete. Med Sci Sports Exerc. 1999;31:S438–S447. doi: 10.1097/00005768-199907001-00005. [DOI] [PubMed] [Google Scholar]
- 116.Kerkhoffs GM, Struijs PA, van Dijk CN. Acute treatment of inversion ankle sprains: immobilization versus functional treatment. Clin Orthop Relat Res. 2007;463:250–1. doi: 10.1097/BLO.0b013e318156fd3f. [DOI] [PubMed] [Google Scholar]
- 117.Jones MH, Amendola AS. Acute Treatment of Inversion Ankle Sprains: Immobilization versus Functional Treatment. Clin Orthop Relat Res. 2007;455:169–72. doi: 10.1097/BLO.0b013e31802f5468. [DOI] [PubMed] [Google Scholar]
- 118.Ardevol J, Bolibar I, Belda V, Argilaga S. Treatment of complete rupture of the lateral ligaments of the ankle: a randomized clinical trial comparing cast immobilization with functional treatment. Knee Surg Sports Traumatol Arthrosc. 2002;10:371–7. doi: 10.1007/s00167-002-0308-9. [DOI] [PubMed] [Google Scholar]
- 119.Lamb SE, Marsh JL, Hutton JL, et al. Mechanical supports for acute, severe ankle sprain: a pragmatic, multicentre, randomised controlled trial. Lancet. 2009;373:575–81. doi: 10.1016/S0140-6736(09)60206-3. [DOI] [PubMed] [Google Scholar]
- 120.Polzer H. 10-day below-knee cast for management of severe ankle sprains. Lancet. 2009;373:1602–3. doi: 10.1016/S0140-6736(09)60899-0. [DOI] [PubMed] [Google Scholar]
- 121.Kerkhoffs GM, van den Bekerom MP, Struijs PA, van Dijk CN. 10-day below-knee cast for management of severe ankle sprains. Lancet. 2009;373:1601–3. doi: 10.1016/S0140-6736(09)60898-9. [DOI] [PubMed] [Google Scholar]
- 122.van Rijn RM, van Middelkoop M. 10-day below-knee cast for management of severe ankle sprains. Lancet. 2009;373:1601–3. doi: 10.1016/S0140-6736(09)60897-7. [DOI] [PubMed] [Google Scholar]
- 123.Eisele R, Greger W, Weikert E, Kinzl L. Ambulatory prevention of thrombosis in traumatology. Unfallchirurg. 2001;104:240–5. doi: 10.1007/s001130050720. [DOI] [PubMed] [Google Scholar]
- 124.Sommer HM, Schreiber H. Early functional conservative therapy of fresh fibular capsular ligament rupture from the socioeconomic viewpoint. Sportverletz Sportschaden. 1993;7:40–6. doi: 10.1055/s-2007-993482. [DOI] [PubMed] [Google Scholar]
- 125.Barr KP, Harrast MA. Evidence-based treatment of foot and ankle injuries in runners. Phys Med Rehabil Clin N Am. 2005;16:779–99. doi: 10.1016/j.pmr.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 126.Kerkhoffs GM, Struijs PA, Marti RK, et al. Different functional treatment strategies for acute lateral ankle ligament injuries in adults. Cochrane Database Syst Rev. 2002 doi: 10.1002/14651858.CD002938.CD002938 [DOI] [PubMed] [Google Scholar]
- 127.Kerkhoffs GM, Struijs PA, Marti RK, et al. Functional treatments for acute ruptures of the lateral ankle ligament: a systematic review. Acta Orthop Scand. 2003;74:69–77. doi: 10.1080/00016470310013699. [DOI] [PubMed] [Google Scholar]
- 128.Boyce SH, Quigley MA, Campbell S. Management of ankle sprains: a randomised controlled trial of the treatment of inversion injuries using an elastic support bandage or an Aircast ankle brace. Br J Sports Med. 2005;39:91–6. doi: 10.1136/bjsm.2003.009233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Beynnon BD, Renstrom PA, Haugh L, et al. A prospective, randomized clinical investigation of the treatment of first-time ankle sprains. Am J Sports Med. 2006;34:1401–12. doi: 10.1177/0363546506288676. [DOI] [PubMed] [Google Scholar]
- 130.Handoll HH, Rowe BH, Quinn KM, de Bie R. Interventions for preventing ankle ligament injuries. Cochrane Database Syst Rev. 2001 doi: 10.1002/14651858.CD000018.CD000018 [DOI] [PubMed] [Google Scholar]
- 131.Dizon JM, Reyes JJ. A systematic review on the effectiveness of external ankle supports in the prevention of inversion ankle sprains among elite and recreational players. J Sci Med Sport. 2010;13:309–17. doi: 10.1016/j.jsams.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 132.Wester JU, Jespersen SM, Nielsen KD, Neumann L. Wobble board training after partial sprains of the lateral ligaments of the ankle: a prospective randomized study. J Orthop Sports Phys Ther. 1996;23:332–6. doi: 10.2519/jospt.1996.23.5.332. [DOI] [PubMed] [Google Scholar]
- 133.Gauffin H, Tropp H, Odenrick P. Effect of ankle disk training on postural control in patients with functional instability of the ankle joint. Int J Sports Med. 1988;9:141–4. doi: 10.1055/s-2007-1024996. [DOI] [PubMed] [Google Scholar]
- 134.Wester JU, Jespersen SM, Nielsen KD, Neumann L. Training on a wobble board following lateral ankle joint sprains. Ugeskr Laeger. 1998;160:632–4. [PubMed] [Google Scholar]
- 135.van der Wees PJ, Lenssen AF, Hendriks EJ, et al. Effectiveness of exercise therapy and manual mobilisation in ankle sprain and functional instability: a systematic review. Aust J Physiother. 2006;52:27–37. doi: 10.1016/s0004-9514(06)70059-9. [DOI] [PubMed] [Google Scholar]
- 136.Tropp H, Askling C, Gillquist J. Prevention of ankle sprains. Am J Sports Med. 1985;13:259–62. doi: 10.1177/036354658501300408. [DOI] [PubMed] [Google Scholar]
- 137.Karlsson J, Eriksson BI, Sward L. Early functional treatment for acute ligament injuries of the ankle joint. Scand J Med Sci Sports. 1996;6:341–5. doi: 10.1111/j.1600-0838.1996.tb00104.x. [DOI] [PubMed] [Google Scholar]
- 138.van Os AG, Bierma-Zeinstra SM, Verhagen AP, et al. Comparison of conventional treatment and supervised rehabilitation for treatment of acute lateral ankle sprains: a systematic review of the literature. J Orthop Sports Phys Ther. 2005;35:95–105. doi: 10.2519/jospt.2005.35.2.95. [DOI] [PubMed] [Google Scholar]
- 139.Mohammadi F. Comparison of 3 preventive methods to reduce the recurrence of ankle inversion sprains in male soccer players. Am J Sports Med. 2007;35:922–6. doi: 10.1177/0363546507299259. [DOI] [PubMed] [Google Scholar]
- 140.Hupperets MD, Verhagen EA, van Mechelen W. Effect of sensorimotor training on morphological, neurophysiological and functional characteristics of the ankle: a critical review. Sports Med. 2009;39:591–605. doi: 10.2165/00007256-200939070-00005. [DOI] [PubMed] [Google Scholar]
- 141.McKeon PO, Hertel J. Systematic review of postural control and lateral ankle instability, part II: is balance training clinically effective? J Athl Train. 2008;43:305–15. doi: 10.4085/1062-6050-43.3.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Holme E, Magnusson SP, Becher K, et al. The effect of supervised rehabilitation on strength, postural sway, position sense and re-injury risk after acute ankle ligament sprain. Scand J Med Sci Sports. 1999;9:104–9. doi: 10.1111/j.1600-0838.1999.tb00217.x. [DOI] [PubMed] [Google Scholar]
- 143.van Rijn RM, van Os AG, Kleinrensink GJ, et al. Supervised exercises for adults with acute lateral ankle sprain: a randomised controlled trial. Br J Gen Pract. 2007;57:793–800. [PMC free article] [PubMed] [Google Scholar]
- 144.Bassett SF, Prapavessis H. Home-based physical therapy intervention with adherence-enhancing strategies versus clinic-based management for patients with ankle sprains. Phys Ther. 2007;87:1132–43. doi: 10.2522/ptj.20060260. [DOI] [PubMed] [Google Scholar]
- 145.Verhagen EA, van Tulder M, van der Beek AJ, et al. An economic evaluation of a proprioceptive balance board training programme for the prevention of ankle sprains in volleyball. Br J Sports Med. 2005;39:111–5. doi: 10.1136/bjsm.2003.011031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Verhagen E, van der BA, Twisk J, et al. The effect of a proprioceptive balance board training program for the prevention of ankle sprains: a prospective controlled trial. Am J Sports Med. 2004;32:1385–93. doi: 10.1177/0363546503262177. [DOI] [PubMed] [Google Scholar]
- 147.Verhagen EA, van Mechelen W, de Vente W. The effect of preventive measures on the incidence of ankle sprains. Clin J Sport Med. 2000;10:291–6. doi: 10.1097/00042752-200010000-00012. [DOI] [PubMed] [Google Scholar]
- 148.Thacker SB, Stroup DF, Branche CM, et al. The prevention of ankle sprains in sports. A systematic review of the literature. Am J Sports Med. 1999;27:753–60. doi: 10.1177/03635465990270061201. [DOI] [PubMed] [Google Scholar]
- 149.Hume PA, Gerrard DF. Effectiveness of external ankle support. Bracing and taping in rugby union. Sports Med. 1998;25:285–312. doi: 10.2165/00007256-199825050-00001. [DOI] [PubMed] [Google Scholar]
- 150.Callaghan MJ. Role of ankle taping and bracing in the athlete. Br J Sports Med. 1997;31:102–8. doi: 10.1136/bjsm.31.2.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Leanderson J, Wredmark T. Treatment of acute ankle sprain. Comparison of a semi-rigid ankle brace and compression bandage in 73 patients. Acta Orthop Scand. 1995;66:529–31. doi: 10.3109/17453679509002308. [DOI] [PubMed] [Google Scholar]
- 152.Cote DJ, Prentice WE, Jr, Hooker DN, Shields EW. Comparison of three treatment procedures for minimizing ankle sprain swelling. Phys Ther. 1988;68:1072–6. doi: 10.1093/ptj/68.7.1072. [DOI] [PubMed] [Google Scholar]
- 153.Meeusen R, Lievens P. The use of cryotherapy in sports injuries. Sports Med. 1986;3(6):398–414. doi: 10.2165/00007256-198603060-00002. [DOI] [PubMed] [Google Scholar]
- 154.Bleakley C, McDonough S, MacAuley D. The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med. 2004;32:251–61. doi: 10.1177/0363546503260757. [DOI] [PubMed] [Google Scholar]
- 155.Hocutt JE, Jr, Jaffe R, Rylander CR, Beebe JK. Cryotherapy in ankle sprains. Am J Sports Med. 1982;10:316–9. doi: 10.1177/036354658201000512. [DOI] [PubMed] [Google Scholar]
- 156.Hubbard TJ, Denegar CR. Does Cryotherapy Improve Outcomes With Soft Tissue Injury? J Athl Train. 2004;39:278–9. [PMC free article] [PubMed] [Google Scholar]
- 157.Bleakley CM, McDonough SM, MacAuley DC, Bjordal J. Cryotherapy for acute ankle sprains: a randomised controlled study of two different icing protocols. Br J Sports Med. 2006;40:700–5. doi: 10.1136/bjsm.2006.025932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Bleakley CM, McDonough SM, MacAuley DC. Some conservative strategies are effective when added to controlled mobilisation with external support after acute ankle sprain: a systematic review. Aust J Physiother. 2008;54:7–20. doi: 10.1016/s0004-9514(08)70061-8. [DOI] [PubMed] [Google Scholar]
- 159.Ekman EF, Ruoff G, Kuehl K, et al. The COX-2 specific inhibitor Valdecoxib versus tramadol in acute ankle sprain: a multi-center randomized, controlled trial. Am J Sports Med. 2006;34:945–55. doi: 10.1177/0363546505283261. [DOI] [PubMed] [Google Scholar]
- 160.Ekman EF, Fiechtner JJ, Levy S, Fort JG. Efficacy of celecoxib versus ibuprofen in the treatment of acute pain: a multicenter, double-blind, randomized controlled trial in acute ankle sprain. Am J Orthop. 2002;31:445–51. [PubMed] [Google Scholar]
- 161.Slatyer MA, Hensley MJ, Lopert R. A randomized controlled trial of piroxicam in the management of acute ankle sprain in Australian Regular Army recruits. The Kapooka Ankle Sprain Study. Am J Sports Med. 1997;25:544–53. doi: 10.1177/036354659702500419. [DOI] [PubMed] [Google Scholar]
- 162.Kayali C, Agus H, Surer L, Turgut A. The efficacy of paracetamol in the treatment of ankle sprains in comparison with diclofenac sodium. Saudi Med J. 2007;28:1836–9. [PubMed] [Google Scholar]
- 163.Dupont M, Beliveau P, Theriault G. The efficacy of antiinflammatory medication in the treatment of the acutely sprained ankle. Am J Sports Med. 1987;15:41–5. doi: 10.1177/036354658701500106. [DOI] [PubMed] [Google Scholar]
- 164.Viljakka T, Rokkanen P. The treatment of ankle sprain by bandaging and antiphlogistic drugs. Ann Chir Gynaecol. 1983;72:66–70. [PubMed] [Google Scholar]
- 165.Almekinders LC. Anti-inflammatory treatment of muscular injuries in sport. An update of recent studies. Sports Med. 1999;28:383–8. doi: 10.2165/00007256-199928060-00001. [DOI] [PubMed] [Google Scholar]
- 166.Predel HG, Giannetti B, Koll R, et al. Efficacy of a comfrey root extract ointment in comparison to a diclofenac gel in the treatment of ankle distortions: results of an observer-blind, randomized, multicenter study. Phytomedicine. 2005;12:707–14. doi: 10.1016/j.phymed.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 167.Kerkhoffs GM, Struijs PA, de Wit C, et al. A double blind, randomised, parallel group study on the efficacy and safety of treating acute lateral ankle sprain with oral hydrolytic enzymes. Br J Sports Med. 2004;38:431–5. doi: 10.1136/bjsm.2002.004150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.de Bie RA, de Vet HC, Lenssen TF, et al. Low-level laser therapy in ankle sprains: a randomized clinical trial. Arch Phys Med Rehabil. 1998;79:1415–20. doi: 10.1016/s0003-9993(98)90237-4. [DOI] [PubMed] [Google Scholar]
- 169.van der Windt DA, van der Heijden GJ, van den Berg SG, et al. Ultrasound therapy for musculoskeletal disorders: a systematic review. Pain. 1999;81:257–71. doi: 10.1016/S0304-3959(99)00016-0. [DOI] [PubMed] [Google Scholar]
- 170.van der Windt DA, van der Heijden GJ, van den Berg SG, et al. Ultrasound therapy for acute ankle sprains. Cochrane Database Syst Rev. 2002;1 doi: 10.1002/14651858.CD001250.CD001250 [DOI] [PubMed] [Google Scholar]
- 171.Almekinders LC, Deol G. The effects of aging, antiinflammatory drugs, and ultrasound on the in vitro response of tendon tissue. Am J Sports Med. 1999;27:417–21. doi: 10.1177/03635465990270040301. [DOI] [PubMed] [Google Scholar]
- 172.Pennington GM, Danley DL, Sumko MH, et al. Pulsed, non-thermal, high-frequency electromagnetic energy (DIAPULSE) in the treatment of grade I and grade II ankle sprains. Mil Med. 1993;158:101–4. [PubMed] [Google Scholar]
- 173.Bennett M, Best TM, Babul S, et al. Hyperbaric oxygen therapy for delayed onset muscle soreness and closed soft tissue injury. Cochrane Database Syst Rev. 2005;4 doi: 10.1002/14651858.CD004713.pub2.CD004713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Petrella RJ, Petrella MJ, Cogliano A. Periarticular hyaluronic acid in acute ankle sprain. Clin J Sport Med. 2007;17:251–7. doi: 10.1097/JSM.0b013e3180f6169f. [DOI] [PubMed] [Google Scholar]
- 175.Rabago D, Slattengren A, Zgierska A. Prolotherapy in primary care practice. Prim Care. 2010;37:65–80. doi: 10.1016/j.pop.2009.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]