Abstract
Craniomaxillofacial (CMF) trauma occurs in isolation or in combination with other serious injuries, including intracranial, spinal, and upper- and lower-body injuries. It is a major cause of expensive treatment and rehabilitation requirements, temporary or lifelong morbidity, and loss of human productivity. The aim of this study was to evaluate patterns of CMF trauma in a large patient sample within a 15-year time frame. Between 1991 and 2005, CMF trauma data were collected from 14,654 patients with 35,129 injuries at the Department of Cranio-Maxillofacial and Oral Surgery in Innsbruck, assessing a plethora of parameters such as injury type and mechanism as well as age and gender distribution over time. Three main groups of CMF trauma were evaluated: facial bone fractures, dentoalveolar trauma, and soft tissue injuries. Statistical comparisons were carried out using a chi-square test. This was followed by a logistic regression analysis to determine the impact of the five main causes for CMF injury. Older people were more prone to soft tissue lesions with a rising risk of 2.1% per year older, showing no significant difference between male and female patients. Younger patients were at higher risk of suffering from dentoalveolar trauma with an increase of 4.4% per year younger. This number was even higher (by 19.6%) for female patients. The risk of sustaining facial bone fractures increased each year by 4.6%. Male patients had a 66.4% times higher risk of suffering from this type of injury. In addition, 2550 patients (17.4%) suffered from 3834 concomitant injuries of other body parts. In summary, we observed changing patterns of CMF trauma over the last 15 years, paralleled by advances in refined treatment and management options for rehabilitation and reconstruction of patients suffering from CMF trauma.
Keywords: craniomaxillofacial trauma, injury causes, injury types, epidemiology
Craniomaxillofacial (CMF) trauma affects a significant proportion of injured patients.1,2,3,4,5,6,7,8 Over 15 years of documentation of individual cases accounts for the accumulation of large amounts of patient data on facial bone fractures, dentoalveolar trauma, and soft tissue injuries, as well as associated injuries, mainly of the head and neck. The epidemiology of CMF trauma varies in type, severity, and cause depending on the population studied.1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20
In the past 40 to 50 years, high-income countries have seen a reduction in injury rates, mortality, and morbidity resulting from injury.1 However, there are still more than five million deaths resulting from injury every year.1 Injury may also lead to disability and economic loss. Less-developed countries have not yet profited from the scientific methods of injury prevention. Thus, rates of injury-related deaths are highest in these countries. There are often no speed limit controls, seatbelt, or helmet laws, and many drivers are impaired by alcohol.7,8
However, a study by Telfer et al in the United Kingdom showed that the incidence of maxillofacial fractures could be reduced significantly by compulsory seatbelt use and the reduction of drunk drivers.9 There has been a 30% decrease of trauma associated with road traffic accidents in the United Kingdom in the past 20 years due to various legislations concerning road safety.10 Since the reduction of maxillofacial trauma caused by traffic accidents, interpersonal violence has become the most reported cause for trauma in the United Kingdom.10 The goal is to reduce total numbers of trauma by finding reasons for trauma and preventing the causes to reduce costs and problems arising from these injuries.
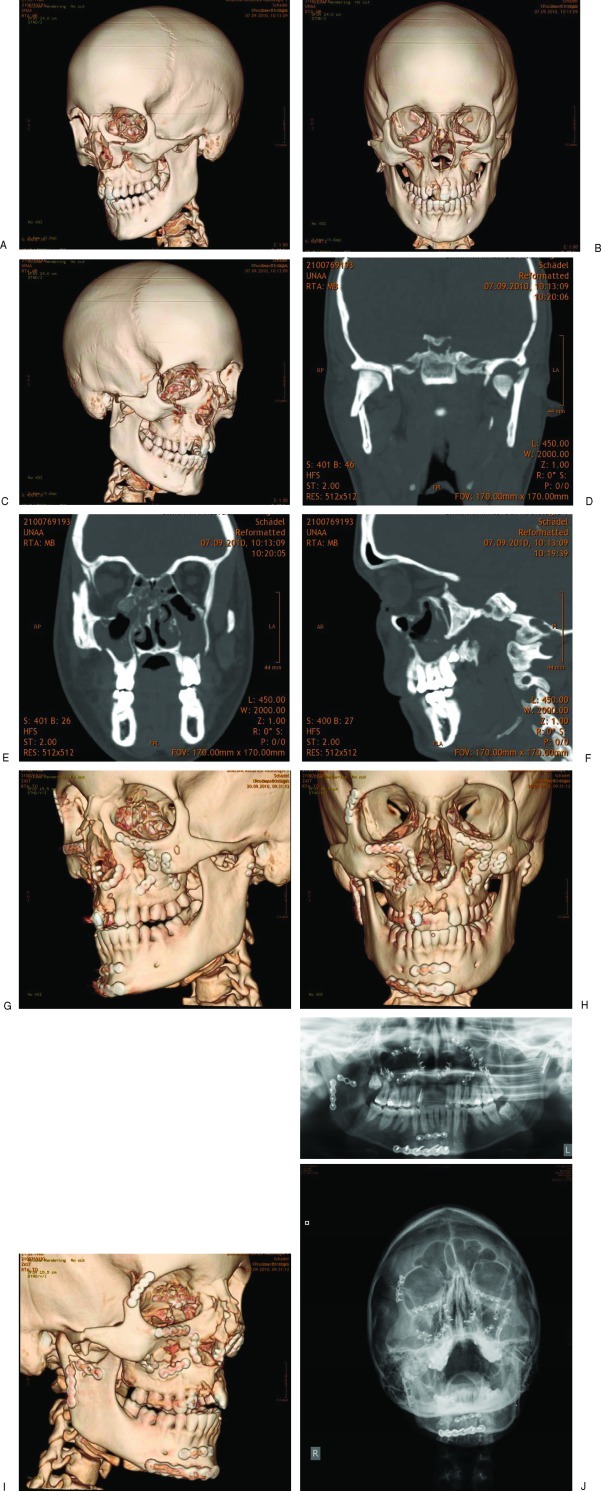
The CMF Trauma Registry at the University Hospital of Innsbruck, Austria was created in 1991 to facilitate prospective and retrospective data collection. All CMF trauma, simple and complex, is listed. Figure 1A–1J displays radiographic images of a case representative for the complexity of diagnostic assessment, categorization, and subsequent treatment allowing both excellent reconstruction and superb wound healing. Injury surveillance and research data at this center reflect the whole spectrum of CMF trauma. Its aim was to outline and thereby reveal variables responsible for high-risk conditions resulting in injury, especially CMF injury, in the Alps by identifying, describing, and quantifying trauma. Five main causes of injury exist, namely work, traffic, assaults, sports, and activities of daily life (ADL).8 The aim of this study was to assess CMF trauma by evaluating data on patients with facial bone fractures, dentoalveolar trauma, and soft tissue injuries and to investigate the impact of the five main causes of facial injury. This work also reflects statistical patterns of CMF trauma in relation to accident causes using logistic regression analyses.
Figure 1.
Selected preoperative radiographic CT images in right (A) oblique, (B) frontal, and (C) left oblique view, of a female patient 22 years of age with complex panfacial fractures of midface and mandible. Image (D) shows a coronal cut of dislocated fractures of the right mandibular condyle and left mandibular head. Image (E) depicts dislocated Le Fort I, zygoma and orbital floor fractures. Image (F) reveals the extent of the orbital floor fracture in the anterior posterior direction. Selected postoperative radiographic CT images in (G) right oblique, (H) frontal, and (I) left oblique view, and (J) conventional radiographs, show the great current options of matrix plates and screws for treating CMF Trauma.
Materials and Methods
At the Department of Cranio-Maxillofacial and Oral Surgery of the Medical University of Innsbruck, data were collected of 14,654 patients with CMF trauma from January 1, 1991, to December 31, 2005. The database that was created included medical history, symptoms, clinical signs, and radiological findings on facial bone fractures, dentoalveolar trauma, and soft tissue lesions. The following parameters were analyzed: type and frequency of injury, age and gender distribution, monthly and yearly distribution, nationality of patients, cause of accidents, and concomitant injuries.
Statistical comparisons were performed using a chi-square test. This was followed by a logistic regression analysis to determine the impact of the five main causes for CMF injury (sports, ADL, play, traffic, violence, and work accidents) on the three evaluated injury types, namely facial bone fractures, dentoalveolar trauma, and soft tissue lesions. The final regression model was used for analyzing the factors age, gender, and type of facial trauma.
Results
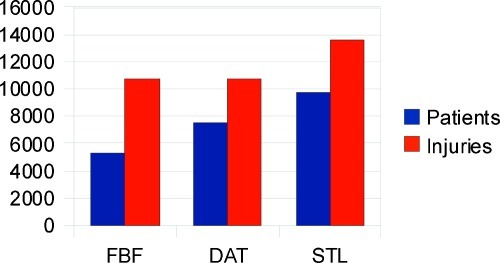
Out of the total of 14,654 patients with 35,129 injuries, 5329 patients (36.36%) suffered from 10,724 facial bone fractures, 7515 patients (51.3%) sustained 10,778 dentoalveolar traumas, and 9721 (66.34%) patients had 13,627 soft tissue lesions. The numbers reveal that patients often sustained more than one type of injury. They suffered from more than one facial bone fracture or a facial bone fracture with an accompanying dentoalveolar trauma and/or soft tissue lesion (Fig. 2).
Figure 2.
Number of patients (blue) suffering from one of the three injury types (red) facial bone fractures (FBF), dentoalveolar trauma (DAT), and soft tissue lesions (STL).
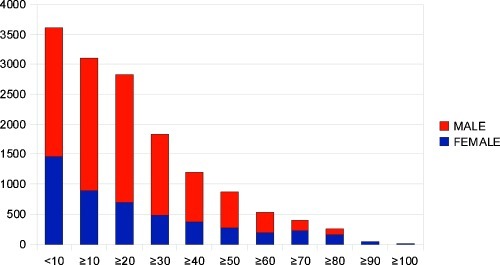
The age of the patients at the time of injury ranged from 0 to 100 years with a median age of 21 and a mean age of 26 years. Of all patients, 24.6% were between 0 and 9 years old and 65.1% were younger than 30 years of age. Almost 15% were older than 50 years (Fig. 3).
Figure 3.
Age group and gender distribution in 14,654 patients.
In the age group between 0 and 70 years, male patients sustained significantly more CMF injuries than females (p < 0.001). In the age groups of 70 and older, female patients had significantly more CMF injuries (p < 0.001).
The yearly mean of patients recorded at the institution was 977. Most injuries (7.62%) occurred in 2001, 2005 (7.13%), and 2004 (7.06%). Soft tissue lesions increased by 8.2% per year, and dentoalveolar trauma increased by 2.4% per year (both p < 0.001); however, facial bone fractures decreased in frequency by 2% per year (p < 0.001).
The monthly distribution showed that most injuries occurred in January (9.2%) and August (9.3%). February was the month with the third most injuries (8.98%), and 35.4% of maxillofacial injuries occurred in the months of December until March. November accounted for the lowest injury rates (6.9%).
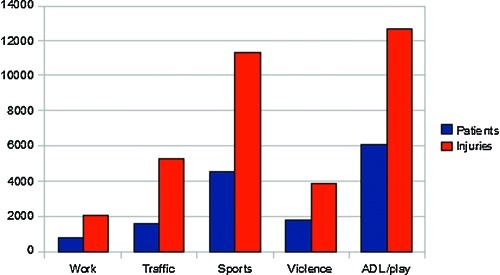
Austrians were 80.26% of patients, 8.63% of patients came from Germany, followed by 2.34% from Italy and 1.82% from Turkey (Table 1). Sports and ADL were the most frequent activities leading to injuries of the face. Sports accidents caused 30.5% of injuries, whereas ADL caused 41.2% (Fig. 4).
Table 1. Nationality of Patients, in Total Numbers.
| Nationality | Total Numbers |
|---|---|
| Austria | 11,761 |
| Germany | 1264 |
| Italy | 343 |
| Yugoslavia | 219 |
| Turkey | 266 |
| Netherlands | 234 |
| Great Britain | 110 |
| France | 54 |
| Switzerland | 72 |
| Sweden | 22 |
| Others | 309 |
Figure 4.
Number of patients and injuries in relation to different causes of injury.
Moreover, 2550 patients (17.4%) suffered from 3834 concomitant injuries of other body parts. These injuries were as follows: neurological injuries (2187), neurosurgical injuries (651), injuries of the upper and lower extremities (408), chest injuries (296), injuries of the spine (205), and abdominal injuries (87).
Facial Bone Fractures
In 5329 patients 10,724 facial bone fractures were subdivided into certain groups as shown in Table 2. There were 221 Le Fort I fractures, which was not a statistically significant difference when compared with the 195 Le Fort II fractures (p = 0.202). However, such fractures occurred significantly more often than Le Fort III fractures (p < 0.001). Almost 27% of all fractures affected the orbital bone; 23.8%, the zygoma; and 23.5%, the mandible. Maxillary injuries were less common, with 10.17%.
Table 2. Occurrence of Different Types of Facial Bone Fractures.
| Patients (n = 5329) | Injuries (n = 10,724) | Percentage |
|---|---|---|
| LeFort I | 221 | 2.06 |
| LeFort II | 195 | 1.82 |
| LeFort III | 126 | 1.17 |
| Zygoma right | 1020 | 9.51 |
| Zygoma left | 1052 | 9.81 |
| Zygomatic arch right | 358 | 3.34 |
| Zygomatic arch left | 392 | 3.66 |
| Orbital floor right | 1170 | 10.91 |
| Orbital floor left | 1125 | 10.49 |
| Orbital bone right | 421 | 3.93 |
| Orbital bone left | 409 | 3.81 |
| Maxilla right | 286 | 2.67 |
| Maxilla left | 286 | 2.67 |
| Maxillary alveolar process right | 200 | 1.86 |
| Maxillary alveolar process left | 184 | 1.72 |
| Socket right | 5 | 0.05 |
| Socket left | 5 | 0.05 |
| Condylar head right | 133 | 1.24 |
| Condylar head left | 132 | 1.23 |
| Mandibular alveolar process right | 95 | 0.89 |
| Mandibular alveolar process left | 92 | 0.86 |
| Mandibular symphysis | 173 | 1.61 |
| Mandible right | 500 | 4.66 |
| Mandible left | 544 | 5.07 |
| Condylar neck right | 392 | 3.66 |
| Condylar neck left | 442 | 4.12 |
| Nasal bone | 766 | 7.14 |
| Total | 10,724 |
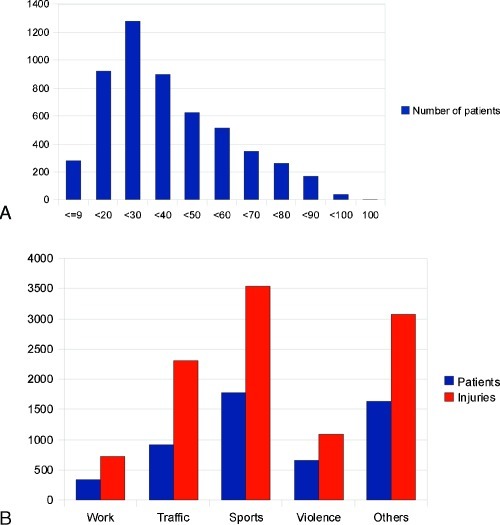
Most patients sustaining a facial bone fracture were between 20 and 40 years old (58.13%; Fig. 5A). Most facial bone fractures (32.9%) were sustained during sports activities, followed by ADL and play (28.7%). Traffic accidents led to 21.5% of all facial bone fractures, giving a total number of 1632 patients suffering from facial bone fractures during a traffic accident (Fig. 5B).
Figure 5.
(A) Age distribution of facial bone fractures. (B) Causes of facial bone fractures.
Dentoalveolar Trauma
In 7515 patients, 10,778 dentoalveolar injuries were reported, involving crown fractures, luxations, avulsions, subluxations, root fractures, intrusions, and concussions. Crown fracture was the most common injury (39%).
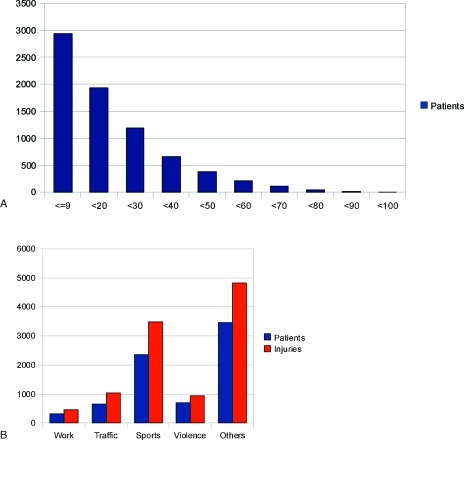
Most patients obtaining dentoalveolar trauma were younger than 10 years of age (39.1%). The most common causes for dentoalveolar trauma were ADL and play accidents (44.8%) followed by sports (32.4%; see Figs. 6A, 6B).
Figure 6.
(A) Age distribution of dentoalveolar trauma. (B) Causes of dentoalveolar trauma.
Soft Tissue Lesions
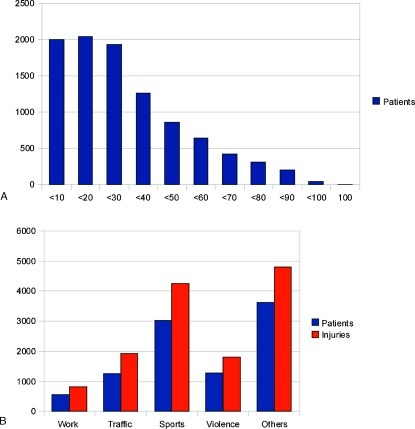
In 9721 patients, 13,627 soft tissue injuries were documented, including lacerations, hematomas, contusions, and excoriations. Lacerations were the most common injury (38%). Most soft tissue lesions occurred between the ages of 0 and 30 years (61.5%), and the most common causes for injuries were ADL, leading to 49.4% of all injuries, and sports (43.8%; Figs. 7A, 7B).
Figure 7.
(A) Age distribution of soft tissue lesions. (B) Causes of soft tissue lesions.
Regression Analyses
The risk of sustaining facial bone fractures increased each year by 4.6%. Male patients had a 66.4% times higher risk of suffering from this type of injury when compared with females. There was a 57.3% higher risk for facial bone fractures in traffic accidents (p < 0.001). However, the probability of suffering from fractures was reduced in cases of violence by 31.7% (p = 0.002), in work-related accidents by 41.9%, and in ADL by 59.8%. On the other hand, there was no statistically significant correlation of obtaining a facial bone fracture in sports accidents (p = 0.301; Table 3).
Table 3. Logistic Regression Analysis for Facial Bone Fractures—All Accidents (n = 14,654).
| Significance Adjusted (p) | Odds Ratio Adjusted | |
|---|---|---|
| Age | <0.001 | 1.046 per year |
| Sex (male) | <0.001 | 1.664 |
| Traffic | <0.001 | 1.573 |
| Work | <0.001 | 0.581 |
| Sports | 0.301 | 0.889 |
| Violence | 0.002 | 0.683 |
| Activities of daily living + play | <0.001 | 0.402 |
Younger patients were at higher risk of suffering from dentoalveolar trauma, with an increase of 4.4% per year younger and 19.6% in females compared with male patients. There was a 2.26-fold higher risk (226%) of obtaining dentoalveolar trauma in work accidents and a 2.36-fold higher risk (236%) in ADL. The probability of suffering from dentoalveolar trauma was higher in sports accidents by 87.8%.
In contrast, there was no statistically significant correlation of sustaining dentoalveolar trauma in traffic accidents and due to violence (p < 0.05; Table 4).
Table 4. Logistic Regression Analysis for Dentoalveolar Trauma—All Accidents (n = 14,654).
| Significance Adjusted (p) | Odds Ratio Adjusted | |
|---|---|---|
| Age | <0.001 | 0.956 per year |
| Sex (male) | <0.001 | 0.804 |
| Traffic | 0.017 | 1.354 |
| Work | <0.001 | 2.265 |
| Sports | <0.001 | 1.878 |
| Violence | 0.086 | 1.242 |
| Activities of daily living + play | <0.001 | 2.364 |
Older people were more prone to soft tissue lesions with a rising risk of 2.1% per year older. There was no statistically significant difference between male and female patients (p = 0.940). There was a 2.84-fold risk (284%) of obtaining a soft tissue lesion in a traffic accident and a 2.43-fold probability (243%) associated with violence. Work and sports accidents both showed a higher risk for this injury type by 98% (Table 5).
Table 5. Logistic Regression Analysis for Soft Tissue Lesions—All Accidents (n = 14,654).
| Significance Adjusted (p) | Odds Ratio Adjusted | |
|---|---|---|
| Age | <0.001 | 1.021 per year |
| Sex (male) | 0.940 | 1.003 |
| Traffic | <0.001 | 2.845 |
| Work | <0.001 | 1.98 |
| Sports | <0.001 | 1.979 |
| Violence | <0.001 | 2.425 |
| Activities of daily living + play | <0.001 | 1.471 |
Discussion
In this database, the greatest cause of injuries was ADL with 41.2% (6036), followed by sports with 30.5% (4469). Violence accounted for 11.9%, traffic accidents caused 11.1% (1750), and work accidents caused 5.3% (767) of all CMF trauma cases. Previous work with this Trauma Data Bank reviewed 9543 cases from 1991 to 2001 using regression analyses.8 Analyzing 5 additional years with this contribution, some risks regarding injuries have changed noticeably.
In the 10-year period of evaluation, a 2.25-fold risk of obtaining a facial bone fracture existed in case of a traffic accident.8 In the 15-year review, the risk was reduced to 1.57-fold. This was paralleled by a decrease in the number of facial bone fractures in work, sports, violence, and ADL/play accidents. But the probability to suffer from facial bone fractures increased slightly comparing the factor age within the former 10-year period to the 15-year time frame.
The risk for obtaining dentoalveolar trauma at work increased by 29%.8 In the 15-year period, this changed to a risk of 226%. ADL used to be 49%; this has now changed to 236%. The probability of obtaining a soft tissue lesion in a traffic accident used to be 1.58 and has changed to a 2.84-fold higher risk. Also, there is now a 2.43-fold risk of suffering from this type of injury when exposed to violence compared with a 1.3-fold risk in the 10-year time period.8 This could also be explained by an 2.1% increase of facial soft tissue lesions per year.
Causes of Injury
A study by Kuehne et al reviewed patients from a German trauma emergency room from May 1998 to June 2002. Patients suffering from facial bone fractures reported in 42.8% of the cases that the injury was caused by a traffic accident.11 This high percentage can be explained by the fact that the study group only reviewed patients from the trauma room, whereas many patients with a facial bone fracture reported directly to the craniomaxillofacial surgery department. Flinzberg et al reported in a general review about facial injuries that up to 62% of facial bone fractures were obtained during sporting activity.12 In this current study, 32.2% of all facial bone fractures were sustained during a sporting activity. This shows that there are various regional discrepancies concerning the cause of injury.
In the United Kingdom, Kirkpatrick stated in a general review that craniomaxillofacial trauma was caused by interpersonal violence in 52% of cases, whereas in our study 11.9% were caused by violence. In the U.K. study, traffic accidents caused 16% of trauma cases and sports injuries caused 19%.10
The U.S. study group of Imahara et al analyzed cases from the National Trauma Data Bank from 2001 to 2005.13 Only children and adolescents up to the age of 18 were included in this study. In 277,008 pediatric trauma patients, 4.6% suffered from a facial fracture. In our study, 22.6% of patients suffering from facial bone fractures were between 0 and 19 years old. The proportion of facial fractures increased with age, a result that was also highlighted by this study, with an increase of 4.6% per year.13
In the U.S. study, injury was caused in 55.1% of all patients by motor vehicle collisions and in 11.8% by violence. It should be noted that in children of age 1 and older, injury is the most common cause of death. In traffic accidents, facial fractures were more common in children who were not restrained. There was a significantly higher mortality rate (63%) in patients with facial fractures. The authors stated that the lack of appropriate restraints increased the facial fracture risk in children by 16%.13
Gassner et al examined trauma cases from 1991 to 2000 for CMF trauma in children.14 Play accidents were the most common cause, leading to 58.2% of CMF trauma, whereas traffic accidents only led to 5% of facial injuries. However, in this study, dentoalveolar injuries (76.3%) and soft tissue lesions were included along with facial bone fractures (11.5%), whereas the U.S. study specifically examined facial fractures.
Gender
In our study, 4765 patients were female (32.5%) and 9889 patients were male (67.5%). In the study by Mourouzis et al from Greece, 92.8% were male and only 7.2% female. It should be noted that they especially evaluated sports-related maxillofacial fractures.15 Kuehne et al from Germany stated that 78.4% of patients were male.11 In the Brazil study, the male-to-female ratio was 4:1.16 In Turkey, 77.5% were male and 22.5% female.17 In Iran, there was a male-to-female ratio of 3.8:1.7 Another Iranian study group reported that 89% of their patients were male and 11% female.18 In India, the study group of Subhashraj et al revealed a recorded male-to-female ratio of 3.7 to 1.19 Another Arabian study evaluated 772 patients were 90% were male and 10% female.20
Age
In our study, 24% of patients suffering from facial bone fractures were between 20 and 29 years old. Almost 60% (58.13%) were aged from 20 to 40 years. Looking at dentoalveolar trauma, 39% of the patients were 9 years and younger. In addition, 64.9% of the patients suffering from dentoalveolar trauma were younger than 20 years. These results did not differ from the 10-year study.8
Kuehne et al analyzed that patients with facial bone injuries reported to the clinic with a mean age of 39.8 years.11 Al Ahmed et al found that most (39%) maxillofacial fractures occurred to patients aged 20 to 29 years and 12.1% occurred to patients aged 12 years and younger.20 Ansari from Iran also stated that patients between 21 and 30 years obtained most facial fractures with the mean age being 24.6 years.7 The study group of Brasileiro and Passeri stated that the patients' mean age was 30.6 with a deviation of ±14.7 years.16
Conclusion
CMF trauma reconstruction developed into a highly specialized field of treatment options following advanced diagnostic modalities in the past 15 years. Therefore, it plays a prominent role in patient care in several disciplines and necessitates close collaboration of specialists such as CMF/facial surgeons, neurosurgeons, ophthalmologists, trauma surgeons, and others.21,22,23,24,25,26,27,28 And the amount of CMF trauma in developing countries continues to rise; the incidence and etiology of CMF injuries varies strongly from one country to another due to social, cultural, and environmental factors.
Assessing a plethora of parameters such as injury type and mechanism as well as age and gender distribution over time, we showed the interaction of the three main groups of CMF trauma, namely facial bone fractures, dentoalveolar trauma, and soft tissue injuries, in statistical comparisons and determined the impact of the five main causes for CMF trauma. In addition, 17.4% of all patients suffered from concomitant injuries of other body parts. Older people were more prone to soft tissue lesions, with a rising risk of 2.1% per year older, showing no statistically significant difference between male and female patients. Younger patients were at higher risk of suffering from dentoalveolar trauma, with a statistical increase of 4.4% per year younger. This number was even higher for female patients by 19.6%. The risk of sustaining facial bone fractures increased each year by 4.6%. Male patients had a 66.4% times higher risk of suffering from this type of injury. The most frequent activities leading to CMF injuries were sports (30.5%) and ADL (41.2%).
The challenges of treating complex CMF trauma, the emotional consequences of such trauma for patients with regard to possible long-term disfigurement, and the socioeconomic impact of CMF trauma on health care systems and industry (in terms of lost workdays and decreased productivity) need awareness to support widespread and manifold prevention efforts as the incidence of CMF trauma is reducible through multidirected prevention programs.
References
- 1.Mock C, Quansah R, Krishnan R, Arreola-Risa C, Rivara F. Strengthening the prevention and care of injuries worldwide. Lancet. 2004;363:2172–2179. doi: 10.1016/S0140-6736(04)16510-0. [DOI] [PubMed] [Google Scholar]
- 2.Islam S Ahmed M Walton G M Dinan T G Hoffman G R The prevalence of psychological distress in a sample of facial trauma victims. A comparative cross-sectional study between UK and Australia J Craniomaxillofac Surg 2011. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Mulligan R P, Friedman J A, Mahabir R C. A nationwide review of the associations among cervical spine injuries, head injuries, and facial fractures. J Trauma. 2010;68:587–592. doi: 10.1097/TA.0b013e3181b16bc5. [DOI] [PubMed] [Google Scholar]
- 4.Simmons O, Manson P N. Endoscopic management of orbital and frontal sinus fractures. J Craniomaxillofac Trauma. 2009;2:177–184. doi: 10.1055/s-0028-1098967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Medel N, Panchal N, Ellis E. Postoperative care of the facial laceration. J Craniomaxillofac Trauma. 2010;3:189–200. doi: 10.1055/s-0030-1268516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cornelius C P, Ehrenfeld M. The use of MMF screws: surgical technique, indications, contraindications, and common problems in review of the literature. J Craniomaxillofac Trauma. 2010;3:55–80. doi: 10.1055/s-0030-1254376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ansari M H. Maxillofacial fractures in Hamedan province, Iran: a retrospective study (1987–2001) J Craniomaxillofac Surg. 2004;32:28–34. doi: 10.1016/j.jcms.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 8.Gassner R, Tuli T, Hächl O, Rudisch A, Ulmer H. Cranio-maxillofacial trauma: a 10 year review of 9,543 cases with 21,067 injuries. J Craniomaxillofac Surg. 2003;31:51–61. doi: 10.1016/s1010-5182(02)00168-3. [DOI] [PubMed] [Google Scholar]
- 9.Telfer M R, Jones G M, Shepherd J P. Trends in the aetiology of maxillofacial fractures in the United Kingdom (1977–1987) Br J Oral Maxillofac Surg. 1991;29:250–255. doi: 10.1016/0266-4356(91)90192-8. [DOI] [PubMed] [Google Scholar]
- 10.Kirkpatrick N. Facial and orbital injuries. Surgery. 2004;22:185–190. [Google Scholar]
- 11.Kuehne C A, Krueger C, Homann M, Mohr C, Ruchholtz S. Epidemiology and management in emergency room patients with maxillofacial fractures. Mund Kiefer Gesichtschir. 2007;11:201–208. doi: 10.1007/s10006-007-0063-7. [DOI] [PubMed] [Google Scholar]
- 12.Flinzberg S, Vesper M, Schmelzle R. Zahn- und Gesichtsschädelverletzungen. Diagnostik, Therapie und Rekonstruktion. Trauma Berufskrankh. 2003;5:405–414. [Google Scholar]
- 13.Imahara S D, Hopper R A, Wang J, Rivara F P, Klein M B. Patterns and outcomes of pediatric facial fractures in the United States: a survey of the National Trauma Data Bank. J Am Coll Surg. 2008;207:710–716. doi: 10.1016/j.jamcollsurg.2008.06.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gassner R, Tuli T, Hächl O, Moreira R, Ulmer H. Craniomaxillofacial trauma in children: a review of 3,385 cases with 6,060 injuries in 10 years. J Oral Maxillofac Surg. 2004;62:399–407. doi: 10.1016/j.joms.2003.05.013. [DOI] [PubMed] [Google Scholar]
- 15.Mourouzis C, Koumoura F. Sports-related maxillofacial fractures: a retrospective study of 125 patients. Int J Oral Maxillofac Surg. 2005;34:635–638. doi: 10.1016/j.ijom.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 16.Brasileiro B F, Passeri L A. Epidemiological analysis of maxillofacial fractures in Brazil: a 5-year prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:28–34. doi: 10.1016/j.tripleo.2005.07.023. [DOI] [PubMed] [Google Scholar]
- 17.Erol B, Tanrikulu R, Görgün B. Maxillofacial fractures. Analysis of demographic distribution and treatment in 2901 patients (25-year experience) J Craniomaxillofac Surg. 2004;32:308–313. doi: 10.1016/j.jcms.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 18.Motamedi M H. An assessment of maxillofacial fractures: a 5-year study of 237 patients. J Oral Maxillofac Surg. 2003;61:61–64. doi: 10.1053/joms.2003.50049. [DOI] [PubMed] [Google Scholar]
- 19.Subhashraj K, Nandakumar N, Ravindran C. Review of maxillofacial injuries in Chennai, India: a study of 2748 cases. Br J Oral Maxillofac Surg. 2007;45:637–639. doi: 10.1016/j.bjoms.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 20.Al Ahmed H E, Jaber M A, Abu Fanas S H, Karas M. The pattern of maxillofacial fractures in Sharjah, United Arab Emirates: a review of 230 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:166–170. doi: 10.1016/j.tripleo.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 21.Pappachan B, Alexander M. Correlating facial fractures and cranial injuries. J Oral Maxillofac Surg. 2006;64:1023–1029. doi: 10.1016/j.joms.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 22.Kloss F R, Tuli T, Hächl O. et al. The impact of ageing on cranio-maxillofacial trauma-a comparative investigation. Int J Oral Maxillofac Surg. 2007;36:1158–1163. doi: 10.1016/j.ijom.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 23.Wheeler J, Phillips J. Pediatric facial fractures and potential long-term growth disturbances. J Craniomaxillofac Trauma. 2011;4:43–52. doi: 10.1055/s-0031-1272901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pereira F L, Gealh W C, Barbosa C EB, Filho L I. Different surgical approaches for multiple fractured atrophic mandibles. J Craniomaxillofac Trauma. 2011;4:19–24. doi: 10.1055/s-0031-1272898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bossert R P, Girotto J A. Blindness following facial fracture: treatment modalities and outcomes. J Craniomaxillofac Trauma. 2009;2:117–124. doi: 10.1055/s-0029-1215874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Haug R H, Serafin B L. Mandibular angle fractures: a clinical and biomechanical comparison—the works of Ellis and Haug. J Craniomaxillofac Trauma. 2008;1:31–38. doi: 10.1055/s-0028-1098961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kellman R M, Losquadro W D. Comprehensive airway management of patients with maxillofacial trauma. J Craniomaxillofac Trauma. 2008;1:39–48. doi: 10.1055/s-0028-1098962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ellis E. Treatment methods for fractures of the mandibular angle. J Craniomaxillofac Trauma. 1996;2:28–36. [PubMed] [Google Scholar]