Abstract
Objective:
Utilization of postacute care is associated with improved poststroke outcomes. However, more than 20% of American adults under age 65 are uninsured. We sought to determine whether insurance status is associated with utilization and intensity of institutional postacute care among working age stroke survivors.
Methods:
A retrospective cross-sectional study of ischemic stroke survivors under age 65 from the 2004–2006 Nationwide Inpatient Sample was conducted. Hierarchical logistic regression models controlling for patient and hospital-level factors were used. The primary outcome was utilization of any institutional postacute care (inpatient rehabilitation or skilled nursing facilities) following hospital admission for ischemic stroke. Intensity of rehabilitation was explored by comparing utilization of inpatient rehabilitation facilities and skilled nursing facilities.
Results:
Of the 33,917 working age stroke survivors, 19.3% were uninsured, 19.8% were Medicaid enrollees, and 22.8% were discharged to institutional postacute care. Compared to those privately insured, uninsured stroke survivors were less likely (adjusted odds ratio [AOR] 0.53, 95% confidence interval [CI] 0.47–0.59) while stroke survivors with Medicaid were more likely to utilize any institutional postacute care (AOR = 1.40, 95% CI 1.27–1.54). Among stroke survivors who utilized institutional postacute care, uninsured (AOR = 0.48, 95% CI 0.36–0.64) and Medicaid stroke survivors (AOR = 0.27, 95% CI 0.23–0.33) were less likely to utilize an inpatient rehabilitation facility than a skilled nursing facility compared to privately insured stroke survivors.
Conclusions:
Insurance status among working age acute stroke survivors is independently associated with utilization and intensity of institutional postacute care. This may explain differences in poststroke outcomes among uninsured and Medicaid stroke survivors compared to the privately insured.
Stroke is a leading cause of long-term disability.1 An estimated 7 million Americans have had a stroke.2 Approximately 20% of strokes occur among people younger than 65 years (working age).3 Largely due to lost wages and institutionalization, working age stroke patients account for around half of the estimated $2.2 trillion in US stroke-related cumulative expenditures projected over the next 4 decades.4
Poststroke rehabilitation or postacute care (PAC) is associated with improved functional outcomes.5–7 PAC services occur in a range of settings, from private residences and outpatient facilities to institutional PAC services which include both inpatient rehabilitation facilities (IRFs) and skilled nursing facilities (SNFs). The intensity of institutional PAC varies from at least 3 hours of rehabilitation per day in an IRF to variable amounts of less frequent and intense rehabilitation in an SNF.8
One out of 5 working age Americans is uninsured, which may affect their probability of undergoing high-cost or high-discretion care.9–11 Because there are no broadly accepted clinical standards to guide utilization of institutional PAC (high-discretion) coupled with variation in costs, insurance status may be associated with utilization of institutional PAC among working age stroke survivors.12,13 Therefore, we explored the association between insurance status and utilization and intensity of institutional PAC accounting for patient and hospital-level confounders among working age stroke survivors. We hypothesized that privately insured stroke survivors would be more likely to receive institutional PAC and to receive more intense institutional PAC than stroke survivors with Medicaid or uninsured.
METHODS
Data source and patients.
Data from the 2004–2006 Nationwide Inpatient Sample (NIS), a nationally representative database of hospital inpatient stays and the largest all-payer inpatient care database, were used. NIS is maintained by the Agency for Healthcare Research and Quality (AHRQ) and was developed as part of the Healthcare Cost and Utilization Project (HCUP). NIS contains both individual and hospital-level information. Survey weights were not used in the primary analysis.
All patients over the age of 18 and admitted from the Emergency Department (ED) with a primary hospital discharge diagnosis of ischemic stroke and discharged to home, SNF, or IRF were included. Ischemic stroke was identified using International Classification of Diseases (ICD)-9-CM codes 433.x1, 434.x1, and 436.14 This approach has been previously validated and found to have a positive predictive value of 88% and sensitivity of 74%.15 To further improve the specificity of this algorithm, we excluded patients who were not admitted from the ED to minimize the impact of the most common misdiagnoses coded as stroke.14 Stroke patients 65 years of age and above were excluded due to the availability of Medicare. Individuals under the age of 65 are eligible for Medicare after 24 months of Social Security disability insurance.16 These patients were excluded from our study as their prestroke disability is likely correlated with their utilization of institutional PAC. Patients with insurance such as worker's compensation, CHAMPUS, or missing payer information (n = 150) were also excluded, resulting in a study population that included only privately insured, uninsured, or Medicaid stroke survivors.
Outcome.
Utilization and intensity of institutional PAC services were our outcomes of interest. These outcome variables were based on discharge destination derived from UB-92 claims form. The discharge destination field was divided into 3 mutually exclusive categories: 1) home (DISPUB92 1, 6, 8), 2) SNF (DISPUB92 3, 61), and 3) IRF (DISPUB92 62). For the primary outcome, utilization of institutional PAC services, the SNF and IRF categories were combined to form a variable representing any institutional PAC use vs discharge to home. For the secondary outcome, intensity of institutional PAC services, a series of variables representing IRF vs SNF, IRF vs discharge to home, and SNF vs discharge to home were created. Discharge destination was assumed to approximate intensity of institutional PAC based on the estimated number of hours of rehabilitation per day in each setting.
Primary predictor variable.
Insurance status was divided into 3 mutually exclusive categories: 1) private insurance, which included commercial carriers, private health maintenance organizations, and preferred provider organizations; 2) Medicaid, which included both fee-for-service and managed care; and 3) uninsured, which included both self-pay and no-charge.
Covariates.
Models were adjusted for patient and hospital-level covariates hypothesized to affect the association between insurance status and institutional PAC utilization and intensity. At the patient level, this included age (18–48, 49–54, 55–59, 60–64) and gender. Patient comorbidity burden was obtained using the Quan implementation of a modified Charlson index (0–1, 2, 3).17,18 Length of stay (0–3, 4–5, 6–8, 9+) and receiving thrombolysis (yes, no) defined by ICD-9-CM 99.10 were included as proxies for stroke severity. Hospital-level variables included teaching status, hospital size (small, medium, large), hospital location (rural, urban), and geographic location (Northeast, Midwest, South, West) as defined by the American Hospital Association. We also calculated hospital-level variables for the annual hospital stroke volume, annual hospital poststroke inpatient mortality, and volume of uninsured stroke patients cared for to account for hospital-level variation in severity, resource availability, and quality of care. These hospital variables were categorized into quartiles based on our study population and thus are not representative of the US stroke population.
Statistical analysis.
Patient and hospital characteristics were calculated by insurance status using descriptive statistics. Utilization of institutional PAC was determined for each insurance group. To evaluate the association between insurance status and institutional PAC utilization and intensity, we fit binomial and hierarchical logistic regression models. In our primary model, we explored utilization of any institutional PAC vs home. We then explored the intensity of rehabilitation by fitting a series of pairwise models for 3 different outcomes based on subsets of our main analysis (IRF vs home, SNF vs home, IRF vs SNF). For each outcome, we first fit an unadjusted model with the primary predictor of insurance status modeled as a series of categorical variables representing Medicaid and no insurance compared to the referent group of private insurance using binomial logistic regression. To account for hospital-level variation, we then fit a hierarchical logistic regression model, with hospital entered as a random effect. We then sequentially added variables to the hierarchical model with insurance status in the following order: individual level variables 1) demographics: age, gender; 2) comorbid illness and stroke severity modified Charlson score, length of stay, and thrombolysis; hospital-level variables 3) hospital factors: size, teaching status, location, annual stroke discharges, and hospital mortality; 4) geographic location; 5) proportion of uninsured working age stroke patients. All covariates were specified a priori. Robust standard errors for fixed effects were estimated using the sandwich–classic method.19 Statistical analyses were performed using SAS 9.2, using the GLIMMIX procedure.
As race-ethnicity may be an important confounder in the association between insurance status and PAC utilization and intensity, we performed a sensitivity analysis limiting our study population to stroke survivors with reported race and ethnicity. In this analysis, race-ethnicity (Black, Hispanic, Asian or Pacific Islander, and Native American compared to the referent group of non-Hispanic white) was added to the group of demographics considered and the primary model of any institutional PAC compared with discharge to home was re-evaluated. Finally, we completed a secondary analysis to ensure that excluding the survey weights did not bias the estimates by performing a nonhierarchical logistic regression model using the design-based survey weights from the NIS.
Standard protocol approvals, registrations, and patient consents.
This study was approved by the University of Michigan Institutional Review Board.
RESULTS
From 2004 to 2006, the NIS contained 73,077 ischemic stroke hospitalizations with age at admission less than 65 years. Of these hospitalizations, 56,577 were uninsured, privately insured, or Medicaid enrollees, and 41,805 were discharged to home or institutional PAC. From these, 33,917 were admitted from the ED and comprised the final study population. Of these patients, 19.3% were uninsured and 19.8% had Medicaid. Patients were most commonly discharged to home (77.3%), while 14.8% and 8.0% were discharged to an IRF or an SNF, respectively.
Characteristics of the study population by insurance status are presented in table 1. Medicaid enrollees were more likely to be female and had more comorbidities as measured by the modified Charlson score than privately insured stroke survivors. Forty-nine percent of working age stroke survivors were admitted to hospitals in the South. Medicaid and uninsured stroke survivors were more likely to be admitted to urban hospitals than privately insured stroke survivors.
Table 1.
Patient and hospital-level factors and discharge destination by insurance status among 33,917 working-age ischemic stroke survivors from the Nationwide Inpatient Sample 2004–2006
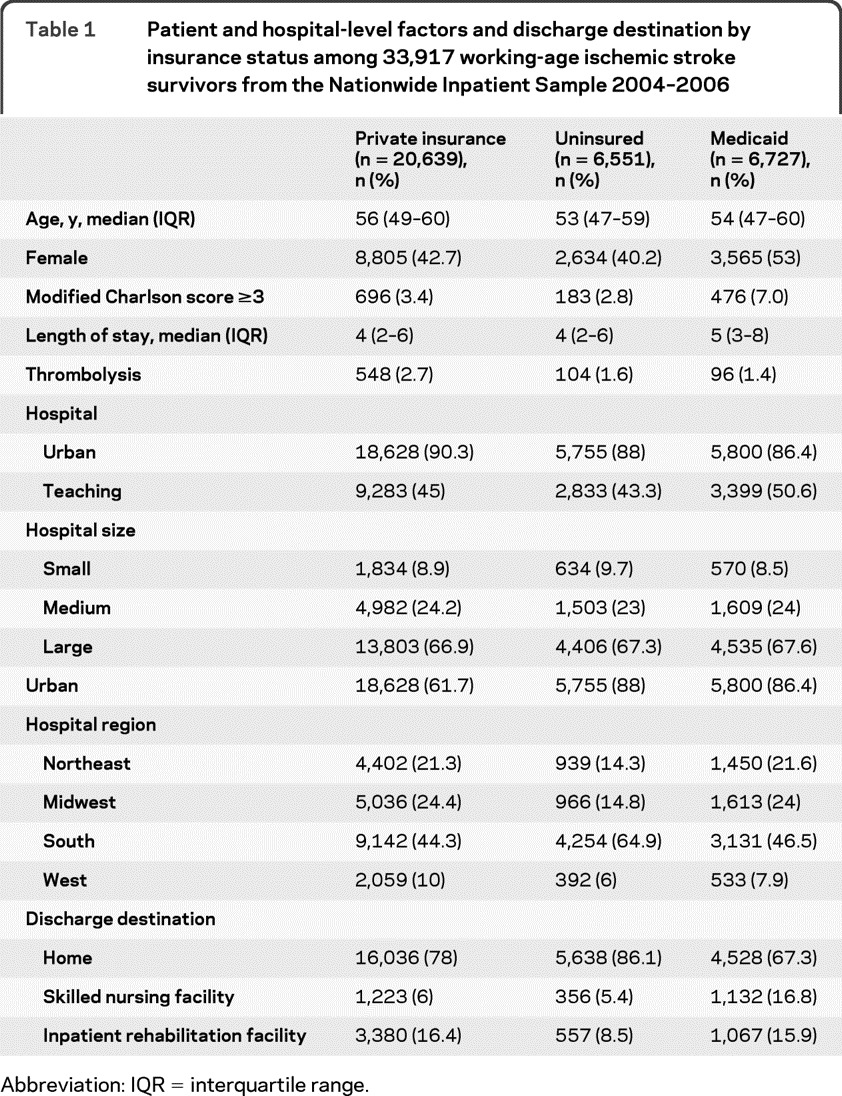
Abbreviation: IQR = interquartile range.
Utilization of Institutional PAC.
Differences in utilization of institutional PAC were noted (table 1). Thirty-three percent of stroke survivors with Medicaid utilized any institutional PAC compared to 14% of uninsured and 22% of privately insured stroke survivors. In unadjusted analysis, uninsured stroke survivors were less likely to utilize any institutional PAC compared to stroke survivors with private insurance (odds ratio [OR] = 0.56, 95% confidence interval [CI] 0.52–0.61). Medicaid enrollees were more likely to utilize any institutional PAC than privately insured stroke survivors (OR = 1.69, 95% CI 1.59–1.80). The results of the multivariable models after adjustment for patient and hospital-level factors are shown in table 2 (full results of hierarchical models included as table e-1 on the Neurology® Web site at www.neurology.org). After adjustment for demographics, modified Charlson score, measures of stroke severity, hospital and regional factors, and hospital stroke payer mix, uninsured stroke survivors were less likely to utilize institutional PAC than privately insured stroke survivors (adjusted OR = 0.53, 95% CI 0.47–0.59). On the contrary, stroke survivors with Medicaid were more likely than stroke survivors with private insurance to receive any institutional PAC (adjusted OR = 1.40, 95% CI 1.27–1.54).
Table 2.
Multivariable regression models of the association between insurance status and utilization of any institutional postacute care among 33,917 working-age stroke survivors from the Nationwide Inpatient Sample 2004–2006
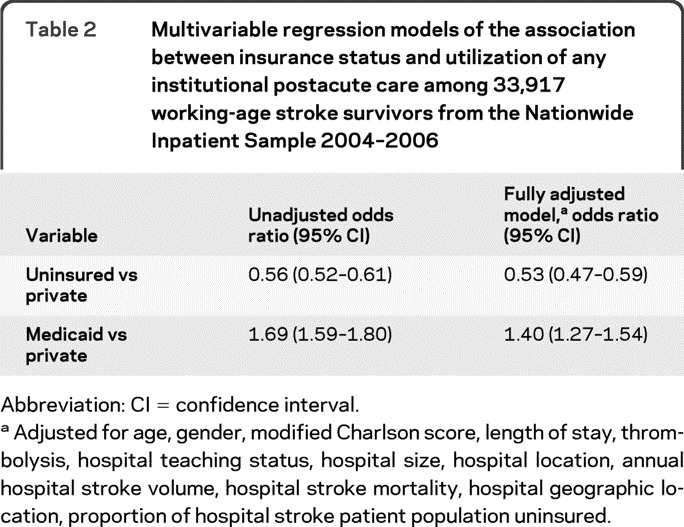
Abbreviation: CI = confidence interval.
Adjusted for age, gender, modified Charlson score, length of stay, thrombolysis, hospital teaching status, hospital size, hospital location, annual hospital stroke volume, hospital stroke mortality, hospital geographic location, proportion of hospital stroke patient population uninsured.
Intensity of PAC.
Among stroke survivors who utilized any institutional PAC, Medicaid enrollees (adjusted OR = 0.27, 95% CI 0.23–0.33) and the uninsured (adjusted OR = 0.48, 95% CI 0.36–0.64) were less likely to utilize an IRF than an SNF compared with privately insured stroke survivors after accounting for patient and hospital-level factors (table 3). Stroke survivors with Medicaid were more likely than the privately insured to utilize an SNF compared to being discharged to home (adjusted OR 2.53, 95% CI 2.23–2.87). Uninsured stroke survivors were less likely than the privately insured to utilize an IRF (adjusted OR 0.45, 95% CI 0.39–0.52) or an SNF (adjusted OR 0.73, 95% CI 0.62–0.86) compared to being discharge to home (table 3).
Table 3.
Multivariable models of discharge destination among 33,917 working-age ischemic stroke survivors from the Nationwide Inpatient Sample 2004–2006
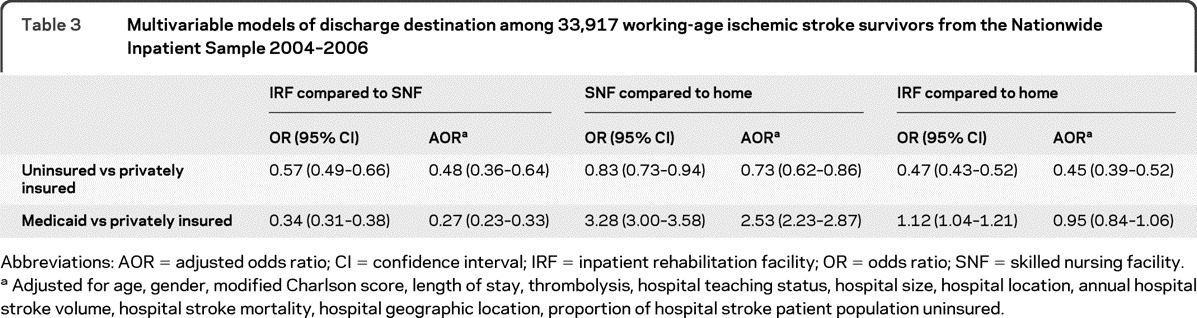
Abbreviations: AOR = adjusted odds ratio; CI = confidence interval; IRF = inpatient rehabilitation facility; OR = odds ratio; SNF = skilled nursing facility.
Adjusted for age, gender, modified Charlson score, length of stay, thrombolysis, hospital teaching status, hospital size, hospital location, annual hospital stroke volume, hospital stroke mortality, hospital geographic location, proportion of hospital stroke patient population uninsured.
Sensitivity analysis.
We obtained similar results after limiting our study population to only those stroke survivors with documented race and ethnicity (n = 23,759). After the addition of race and ethnicity to the fully adjusted model, uninsured stroke survivors remained less likely to utilize any institutional PAC (adjusted OR 0.48, 95% CI 0.43–0.55) while stroke survivors with Medicaid remained more likely to utilize any institutional PAC (adjusted OR 1.31, 95% CI 1.16–1.49) than privately insured. In addition, performing the primary analysis using the survey weights in a nonhierarchical manner did not meaningfully alter the estimates or the standard errors for the models.
DISCUSSION
In this geographically diverse sample of over 30,000 working age acute stroke survivors, insurance status was associated with both utilization and intensity of institutional PAC. Compared with privately insured, stroke survivors with Medicaid were more likely to utilize any institutional PAC. On the contrary, uninsured stroke survivors were less likely to utilize any institutional PAC than those with private insurance. If the uninsured or stroke survivors with Medicaid utilized institutional PAC, they were more likely to utilize an SNF than an IRF compared with the privately insured. These findings are particularly important today for 2 reasons. First, an estimated 7 million Americans have had a stroke and the prevalence of stroke is increasing, resulting in a growing need for PAC services.2,20 Second, as a result of the Patient Protection and Affordable Care Act, the United States is preparing to add 16 million more Medicaid beneficiaries by 2019,the vast majority of whom will be uninsured adults without dependents.21 Our results suggest a mixed outlook for these new Medicaid enrollees. On one hand, this health care reform will likely result in increased utilization of institutional PAC among stroke survivors, but on the other hand, the rehabilitation may be less intense than if they were privately insured.
Among stroke survivors with Medicaid who utilized institutional PAC, 51% were discharged to an SNF compared to 27% of the privately insured. Reasons for the greater utilization of SNFs among stroke survivors with Medicaid are unknown. One possibility is that Medicaid reimbursement policies incentivize utilization of an SNF rather than the more expensive IRF. Based on Medicare payments, utilization of an IRF leads to an average of $24,219 more spending than if discharged home and an average of $10,121 more spending than if discharged to an SNF.13 In general, Medicaid reimbursement is lower than Medicare and private insurance, potentially creating a disincentive for IRFs to admit these stroke survivors.22 The association between reimbursement and intensity of institutional PAC has been shown among Medicare beneficiaries.23,24 A second potential explanation for the increased utilization of an SNF compared to an IRF among stroke survivors with Medicaid is the possibility that they have greater preexisting disability and are thus better candidates for utilization of an SNF.25 In our study population, stroke survivors with Medicaid had greater comorbidity as measured by the Charlson comorbidity index, but comorbidity and stroke severity measures were not confounders of the association between Medicaid and intensity of institutional PAC (data not shown). However, given our absence of a measurement of prestroke disability and crude measures of stroke severity and comorbidities due to the data available in the NIS, we cannot exclude that residual confounding by disability or severity may explain some of the association between Medicaid and intensity of institutional PAC.
Differences in utilization and intensity of PAC may partially explain the greater decline in quality of life and functional status experienced by uninsured and Medicaid stroke survivors compared with privately insured or Medicare recipients.26,27 Although no definitive trials address the impact of rehabilitation intensity on poststroke outcomes, the available evidence suggests that IRF utilization is associated with better outcomes than SNF utilization.13,28,29 A systematic review showed that organized and coordinated postacute inpatient rehabilitation care following an acute stroke is associated with decreased mortality and dependence compared to alternative forms of rehabilitation.7 Furthermore, another study found that among stroke survivors who were candidates for either an SNF or an IRF, survivors discharged to an SNF were more likely to be dead or institutionalized at 120 days.13 In our study, IRF utilization was assumed to be more intense rehabilitation than SNF based on the duration of daily rehabilitation.30 However, there was no information available about the length of stay, which may be longer in an SNF than IRF, or quality of rehabilitation that the stroke survivors received in SNFs or IRFs. More research is needed to understand the role of utilization and intensity of PAC on poststroke outcomes and on identified disparities in stroke outcomes by insurance status. Additionally, we did not explore variation in home health care or outpatient rehabilitation because the NIS dataset does not distinguish home rehabilitation from other types of home health care services or contain information about outpatient services. Further study is needed to explore the utilization of PAC among the over 75% of stroke survivors who are discharged home.
Several limitations of this study warrant discussion. The accuracy of NIS discharge destination field has not been determined. We expect that there is some misclassification of discharge location but we do not expect that this misclassification is related to insurance status.31 If true, the results would tend to be biased toward the null. Despite the high sensitivity and positive predicative value of the ICD-9-CM codes used to identify the stroke discharge, it is unknown if insurance status influences ICD-9-CM coding of ischemic stroke. If this is the case, the association between insurance status and PAC may be biased. Racial and ethnic information is not available for every patient in the NIS due to selective reporting by states. It is possible that race-ethnicity may confound the observed associations. However, we found no evidence of confounding in a sensitivity analysis limited to stroke survivors with reported race and ethnicity. Markers of stroke severity such as the NIH Stroke Scale that are important predictors of institutional PAC utilization were not available in the NIS dataset. Length of stay and tissue plasminogen activator administration were used as proxies for stroke severity although they likely account for only a moderate proportion of the variation in severity. The Charlson comorbidity index was used as a measure of comorbid illness and while it accounts for a large number of comorbidities, not all potentially relevant comorbidities are included and the severity of comorbidities is not accounted for. In addition to insurance status, other factors have been shown to influence utilization of PAC services, including proximity to PAC, family preferences and family support, discharge planning, and referral systems and practice pattern of providers, which were not available in our dataset.32,33 Finally, this study was limited to those younger than 65; PAC utilization may be different for Medicare recipients and requires further study.
Nearly 40% of working age stroke survivors are uninsured or have Medicaid. The results of this study suggest differences in utilization and intensity of institutional PAC for working age stroke survivors based on their insurance status. Compared to the privately insured, stroke survivors with Medicaid were more likely while uninsured stroke survivors were less likely to utilize any institutional PAC. Stroke survivors with Medicaid and without insurance who received institutional PAC received less intense PAC. In light of the impending significant increase in Medicaid enrollees, more research regarding the impact of utilization and intensity of PAC on identified poststroke outcome disparities, particularly among working age stroke survivors, is needed.
Supplementary Material
GLOSSARY
- AHRQ
Agency for Healthcare Research and Quality
- AOR
adjusted odds ratio
- CI
confidence interval
- ED
Emergency Department
- HCUP
Healthcare Cost and Utilization Project
- ICD
International Classification of Diseases
- IRF
inpatient rehabilitation facility
- NIS
Nationwide Inpatient Sample
- OR
odds ratio
- PAC
postacute care
- SNF
skilled nursing facility
Footnotes
Supplemental data at www.neurology.org
AUTHOR CONTRIBUTIONS
Dr. Skolarus: drafting the manuscript for content, including medical writing for content, study concept or design, analysis or interpretation of data, study supervision or coordination. Dr. Meurer: revising the manuscript for content, including medical writing for content, study concept or design, analysis or interpretation of data, statistical analysis. Dr. Burke: revising the manuscript for content, including medical writing for content, study concept or design, analysis or interpretation of data, statistical analysis. Dr. Prvu-Bettger: revising the manuscript for content, including medical writing for content, analysis or interpretation of data. Dr. Lisabeth: revising the manuscript for content, including medical writing for content, study concept or design, analysis or interpretation of data, study supervision or coordination.
DISCLOSURE
The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1. Differences in disability among black and white stroke survivors: United States, 2000–2001. MMWR Morb Mortal Wkly Rep 2005; 54: 3– 6 [PubMed] [Google Scholar]
- 2. Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics: 2011 update: a report from the American Heart Association. Circulation 2011; 123: e18– e209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rothwell PM, Coull AJ, Giles MF, et al. Change in stroke incidence, mortality, case-fatality, severity, and risk factors in Oxfordshire, UK from 1981 to 2004 (Oxford Vascular Study). Lancet 2004; 363: 1925– 1933 [DOI] [PubMed] [Google Scholar]
- 4. Brown DL, Boden-Albala B, Langa KM, et al. Projected costs of ischemic stroke in the United States. Neurology 2006; 67: 1390– 1395 [DOI] [PubMed] [Google Scholar]
- 5. Granger CV, Markello SJ, Graham JE, Deutsch A, Ottenbacher KJ. The uniform data system for medical rehabilitation: report of patients with stroke discharged from comprehensive medical programs in 2000–2007. Am J Phys Med Rehabil 2009; 88: 961– 972 [DOI] [PubMed] [Google Scholar]
- 6. Duncan PW, Zorowitz R, Bates B, et al. Management of adult stroke rehabilitation care: a clinical practice guideline. Stroke 2005; 36: e100– e143 [DOI] [PubMed] [Google Scholar]
- 7. Langhorne P, Duncan P. Does the organization of postacute stroke care really matter? Stroke 2001; 32: 268– 274 [DOI] [PubMed] [Google Scholar]
- 8. Coverage of Inpatient Rehabilitation Services. Available at: http://www.cms.gov/MLNMattersArticles/downloads/MM6699.pdf Accessed June 14, 2011
- 9. Schwartz KHJ, Tolbert J, Lawton E, Chen V. Uninsured: A Primer. Menlo Park, CA: Kaiser Family Foundation; 2010 [Google Scholar]
- 10. Holahan J, Cook A. The U.S. economy and changes in health insurance coverage, 2000–2006. Health Aff 2008; 27: w135– w144 [DOI] [PubMed] [Google Scholar]
- 11. Wenneker MB, Weissman JS, Epstein AM. The association of payer with utilization of cardiac procedures in Massachusetts. JAMA 1990; 264: 1255– 1260 [PubMed] [Google Scholar]
- 12. Unsworth CA, Thomas SA, Greenwood KM. Rehabilitation teams decisions on discharge housing for stroke patients. Arch Phys Med Rehabil 1995; 76: 331– 340 [DOI] [PubMed] [Google Scholar]
- 13. Buntin MB, Colla CH, Deb P, Sood N, Escarce JJ. Medicare spending and outcomes after postacute care for stroke and hip fracture. Med Care 2010; 48: 776– 784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Goldstein LB. Accuracy of ICD-9-CM coding for the identification of patients with acute ischemic stroke: effect of modifier codes. Stroke 1998; 29: 1602– 1604 [DOI] [PubMed] [Google Scholar]
- 15. Tirschwell DL, Longstreth WT., Jr Validating administrative data in stroke research. Stroke 2002; 33: 2465– 2470 [DOI] [PubMed] [Google Scholar]
- 16. Rousseau D, Clemans-Cope L, Lawton E, Langston J, Connolly J, Howard J. Dual Eligibles: Medicaid Enrollment and Spending for Medicare Beneficiaries in 2007. Available at: http://www.kff.org/medicaid/upload/7846-02.pdf Accessed June 15, 2011 [Google Scholar]
- 17. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005; 43: 1130– 1139 [DOI] [PubMed] [Google Scholar]
- 18. Goldstein LB, Samsa GP, Matchar DB, Horner RD. Charlson index comorbidity adjustment for ischemic stroke outcome studies. Stroke 2004; 35: 1941– 1945 [DOI] [PubMed] [Google Scholar]
- 19. SAS/STAT 9.2 User's Guide: The Glimmix Procedure. Cary, NC: SAS Publishing; 2008 [Google Scholar]
- 20. Muntner P, Garrett E, Klag MJ, Coresh J. Trends in stroke prevalence between 1973 and 1991 in the US population 25 to 74 years of age. Stroke 2002; 33: 1209– 1213 [DOI] [PubMed] [Google Scholar]
- 21. Medicaid Matters: Understanding Medicaid's Role in Our Health Care System. Available at: http://www.kff.org/medicaid/upload/8165.pdf Accessed June 14, 2011
- 22. Zuckerman S, Williams AF, Stockley KE. Trends in Medicaid physician fees, 2003–2008. Health Aff 2009; 28: w510– w519 [DOI] [PubMed] [Google Scholar]
- 23. Retchin SM, Brown RS, Yeh SC, Chu D, Moreno L. Outcomes of stroke patients in Medicare fee for service and managed care. JAMA 1997; 278: 119– 124 [PubMed] [Google Scholar]
- 24. Smith MA, Frytak JR, Liou JI, Finch MD. Rehospitalization and survival for stroke patients in managed care and traditional Medicare plans. Med Care 2005; 43: 902– 910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dallas MI, Rone-Adams S, Echternach JL, Brass LM, Bravata DM. Dependence in prestroke mobility predicts adverse outcomes among patients with acute ischemic stroke. Stroke 2008; 39: 2298– 2303 [DOI] [PubMed] [Google Scholar]
- 26. Dhamoon MS, Moon YP, Paik MC, et al. Quality of life declines after first ischemic stroke: The Northern Manhattan Study. Neurology 2010; 75: 328– 334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dhamoon MS, Moon YP, Paik MC, et al. Long-term functional recovery after first ischemic stroke: the Northern Manhattan Study. Stroke 2009; 40: 2805– 2811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kramer AM. Outcomes and costs after hip fracture and stroke: a comparison of rehabilitation settings. JAMA 1997; 277: 396– 404 [PubMed] [Google Scholar]
- 29. Deutsch A, Granger CV, Heinemann AW, et al. Poststroke rehabilitation: outcomes and reimbursement of inpatient rehabilitation facilities and subacute rehabilitation programs. Stroke 2006; 37: 1477– 1482 [DOI] [PubMed] [Google Scholar]
- 30. Freburger JK, Holmes GM, Ku L-JE, Cutchin MP, Heatwole-Shank K, Edwards LJ. Disparities in postacute rehabilitation care for stroke: an analysis of the state inpatient databases. Arch Phys Med Rehabil 2011; 92: 1220– 1229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kahn JM, Iwashyna TJ. Accuracy of the discharge destination field in administrative data for identifying transfer to a long-term acute care hospital. BMC Res Notes 2010; 3: 205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Buntin MB, Garten AD, Paddock S, Saliba D, Totten M, Escarce JJ. How much is postacute care use affected by its availability? Health Serv Res 2005; 40: 413– 434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ottenbacher KJ, Graham JE. The state-of-the-science: access to postacute care rehabilitation services: a review. Arch Phys Med Rehabil 2007; 88: 1513– 1521 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


