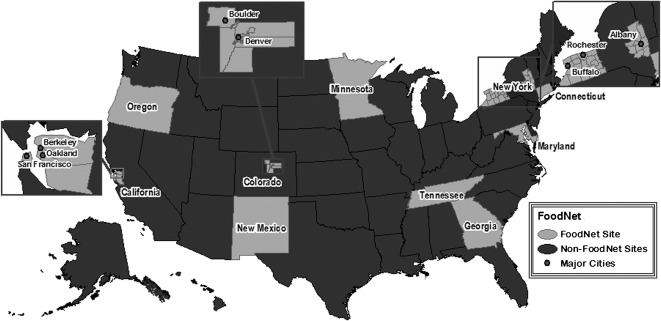
Foodborne disease is an important public health problem in the United States, with an estimated 9.4 million domestically acquired illnesses and 1351 deaths from known pathogens each year [1]. The Foodborne Diseases Active Surveillance Network (FoodNet) tracks important foodborne illnesses, generating information that provides a foundation for food safety policy and prevention efforts. FoodNet has provided information that contributes to food safety efforts by estimating numbers of foodborne illnesses, monitoring trends in incidence of specific foodborne illnesses over time, attributing illnesses to specific foods and settings, and disseminating information [2, 3]. Since it started in 1996, FoodNet has been an excellent example of partnership among federal and state agencies (Figure 1). This Clinical Infectious Diseases supplement contains a variety of articles that provide new information on current issues; together, they highlight FoodNet’s central role in US surveillance and investigation of foodborne disease.
Figure 1.
Foodborne Disease Active Surveillance Network (FoodNet) sites in 2011, including Connecticut, Georgia, Maryland, Minnesota, New Mexico, Oregon, Tennessee, and selected counties in California, Colorado, and New York. FoodNet is a collaborative program among the Centers for Disease Control and Prevention, 10 participating state health departments, the US Department of Agriculture’s Food Safety and Inspection Service, and the Food and Drug Administration.
FoodNet’s core work is ongoing active, population-based surveillance for laboratory-confirmed infections caused by 9 pathogens transmitted commonly through food, as well as for hemolytic uremic syndrome. Several articles in this supplement report on these core data, examining trends and providing regulatory and public health agencies, industry, and consumer groups with data needed to prioritize and evaluate food safety interventions and monitor progress toward national health objectives. For example, Ong et al [4] report the dramatic decline in Yersinia enterocolitica infections since 1996, particularly among young black children. Not all the news is good, however; Newton et al [5] analyze data from FoodNet and the Cholera and Other Vibrio Illness Surveillance System (COVIS), showing that Vibrio infections have increased nationally. Two articles in this supplement examine FoodNet surveillance data on invasive listeriosis. The article by Silk et al [6] summarizes trends in surveillance data from 2004 to 2009, whereas Pouillot et al [7] use FoodNet surveillance data to estimate the relative risk of listeriosis by age, pregnancy, and ethnicity, providing new insights into variations in risk across the population. Together, these articles emphasize that to substantially decrease the incidence of listeriosis, prevention measures should target higher-risk groups, particularly pregnant women, especially Hispanics, and older adults. Hall et al [8] examine trends in Cyclospora infection, showing that outbreaks and international travel play an unusually large role in the epidemiology of these infections and suggesting that prevention efforts would most effectively focus on foods from and travel to endemic areas.
FoodNet continuously works to improve the quality of its surveillance data and methods for analysis. In this supplement, Henao et al [9] describe the methods and rationale surrounding the introduction, in 2011, of a measure of overall change in the incidence of infection over time using surveillance data on infections caused by 6 bacterial pathogens. This measure, which provides a comprehensive picture of changes in incidence of foodborne infections, documents a 23% decline overall in incidence for these pathogens in 2010 compared with the first 3 years of surveillance (1996–1998). Although it does not replace pathogen-specific trend data, this summary measure can help inform the development and assessment of policies and interventions to prevent foodborne illness. Another article, by Manikonda et al [10], reports on a study to validate the reporting of deaths in FoodNet surveillance, an important issue because deaths, although rare, are disproportionately responsible for the economic and human costs of foodborne disease. Finally, Ong et al [11] examine the impact of case ascertainment strategies and case definitions on surveillance for pediatric hemolytic uremic syndrome in FoodNet.
Several articles in the supplement elucidate aspects of the “surveillance steps” that are necessary for a case of infection to be ascertained by FoodNet surveillance. FoodNet and many other surveillance systems for bacterial enteric infections are based on culture-confirmed infections, so FoodNet surveillance data must be interpreted in the context of the “surveillance steps” that lead to culture confirmation: the ill person must seek medical care, a stool specimen must be submitted, and the clinical laboratory must test for and identify the pathogen. In particular, the recent and ongoing shift among clinical laboratories toward culture-independent methods for detecting enteric pathogens is of great importance. Three articles in this supplement explore this issue. Cronquist et al [12] summarize the challenges and opportunities that culture-independent tests present for surveillance. To ensure that surveillance remains robust, the authors emphasize the need for public health practitioners to clearly explain the value of surveillance for enteric pathogens, its crucial role in outbreak detection and tracking trends, the role of outbreak detection and robust trend data in protecting public health, and the need to collaborate with all stakeholders to develop solutions. Campylobacter is one of the pathogens for which culture-independent testing methods have been introduced. In their article, Hurd et al [13] provide baseline information for understanding changing laboratory practices by documenting the procedures used by clinical diagnostic laboratories for Campylobacter detection in FoodNet in 2005, including the use of culture-independent methods and adherence to guidelines for culture-based tests. The increased availability and use of tests that detect Shiga toxin in stool specimens is one reason why the number of reported non-O157 Shiga toxin–producing Escherichia coli infections in FoodNet is increasing, although Clogher et al [14] report that physician ordering and interpretation of Shiga toxin test results remain suboptimal.
FoodNet also monitors the “surveillance steps” related to medical care by collecting information from the general population through periodic FoodNet population surveys. These surveys provide essential information for estimating the numbers of persons with diarrheal illness, the severity of illness, and the frequency with which persons seek medical care and submit a stool sample for that illness. These surveys also collect information on consumption of foods, including “risky” foods that are frequently linked to foodborne illnesses. Shiferaw et al [15] use data from the most recent FoodNet population survey, conducted in 2006–2007, to explore sex differences in food consumption, showing intriguing patterns of similarity and difference that may be useful not only in educational efforts but also in generating hypotheses about possible food sources for outbreaks.
FoodNet surveillance data can be compared with data from other surveillance systems, from surveys, and from special studies to enhance our understanding of disease burden and trends. Linking data between surveillance systems can increase FoodNet’s utility, as exemplified by the article by Shiferaw et al [16], who combined FoodNet data on Shigella infections with data from the Centers for Disease Control and Prevention (CDC) National Antimicrobial Resistance Monitoring System (NARMS). Ailes et al [17] also use data from FoodNet population surveys, along with data from FoodNet case-control studies, to explore the roles of medical care seeking, medical practices, and risk factors in geographic variation in the rates of culture-confirmed Campylobacter infection. These differences did not fully explain the geographic variation in campylobacteriosis, suggesting that real and substantial differences in risk may exist within the United States.
The attribution of enteric infections to exposure sources starts with understanding the roles of various transmission routes. Not all enteric infections are transmitted through food, and not all that are transmitted through food are acquired domestically. In this supplement, Hale et al [18] adapt the methods developed in FoodNet to estimate the total US numbers of illnesses [1] to estimate the annual numbers of illnesses caused by 7 enteric pathogens that can be attributed to contact with animals and their environments. They estimate that this transmission route is responsible for about 13% of these illnesses. FoodNet has collected information on international travel history since 2004. Kendall et al [19] describe these data, reporting that about 13% of FoodNet cases are associated with international travel, primarily in travelers returning from Latin America and the Caribbean, although travel to Africa carries the greatest risk. For those infections that are transmitted through food, sound information on food source attribution is essential to develop and prioritize food safety interventions. In an analysis that not only explores trends in Salmonella serotype Enteritidis infection in FoodNet data but also considers these trends in light of data on processed broiler chickens, Chai et al [20] bring our attention to a recent increase in human serotype Enteritidis infections, highlighting the importance of eating chicken as a risk factor. FoodNet has been able to make a unique contribution to food source attribution by using its surveillance platform to conduct case-control studies to assess risk factors for sporadic (ie, not outbreak-associated) infections. However, many approaches to food source attribution rely on data from outbreak investigations in which the etiologic agent and the food vehicle are identified. Successful investigation—that is, identification of the agent and vehicle—of a high proportion of foodborne outbreaks is essential to this work. Murphree et al [21] demonstrate the importance of collecting fecal specimens and conducting analytic epidemiologic studies as important determinants of success in outbreak investigations.
In 2011, the CDC released new estimates of the number of foodborne illnesses in the United States, the Food Safety Modernization Act was signed into law, and new national health objectives for foodborne illness were set as part of the Healthy People 2020 goals. All of these initiatives, as well as continued concern about food safety on the part of the public and policy makers, emphasize the need for precise and accurate information about foodborne disease. Regulators and other public health officials, consumer advocates, industry, and others need information on trends, high-risk populations, and the foods causing illness so that interventions can be targeted most efficiently and effectively. FoodNet provides the articles in this supplement as part of its efforts to disseminate the results of its surveillance and analytic work. Although FoodNet surveillance is conducted in a geographic area that covers only 15% of the US population, the data it generates are a valuable resource for the entire United States. The FoodNet program shows the impact that high-quality, nationally coordinated surveillance can have on public health and policy.
Notes
Disclaimer.
The contents of this work are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention.
Financial support.
This publication was supported in part by the Centers for Disease Control and Prevention (CDC; Cooperative Agreement U60/CD303019). FoodNet is funded by the Food Safety Office and the Emerging Infections Program of the CDC, the US Department of Agriculture Food Safety and Inspection Service, and the Food and Drug Administration.
Supplement sponsorship.
This article was published as part of a supplement entitled “Studies From the Foodborne Diseases Active Surveillance Network,” sponsored by the Division of Foodborne, Waterborne, and Environmental Diseases of the National Center for Emerging and Zoonotic Infectious Diseases from the Centers for Disease Control and Prevention, and the Association of Public Health Laboratories.
Potential conflicts of interest.
All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Scallan E, Hoekstra RM, Angulo FJ, et al. Foodborne illness acquired in the United States–major pathogens. Emerg Infect Dis. 2011;17:7–15. doi: 10.3201/eid1701.P11101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scallan E. Activities, achievements, and lessons learned during the first 10 years of the Foodborne Diseases Active Surveillance Network: 1996–2005. Clin Infect Dis. 2007;44:718–25. doi: 10.1086/511648. [DOI] [PubMed] [Google Scholar]
- 3.Jones TF, Scallan E, Angulo FJ. FoodNet: overview of a decade of achievement. Foodborne Pathog Dis. 2007;4:60–6. doi: 10.1089/fpd.2006.63. [DOI] [PubMed] [Google Scholar]
- 4. doi: 10.1093/cid/cis053. Ong KL, Gould LH, Chen DL, et al. Changing epidemiology of Yersinia enterocolitica infections: markedly decreased rates in young black children, FoodNet, 1996–2009. Clin Infect Dis 2012; 54(Suppl 5):S385–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. doi: 10.1093/cid/cis243. Newton A, Kendall M, Vugia DJ, Henao O, Mahon BE. Increasing rates of vibriosis in the United States: review of surveillance data from two systems, 1996–2010. Clin Infect Dis 2012; 54(Suppl 5):S391–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. doi: 10.1093/cid/cis268. Silk BJ, Date KA, Jackson KA, et al. Invasive listeriosis in Foodborne Diseases Active Surveillance Network, 2004–2009: further targeted prevention needed for higher-risk groups. Clin Infect Dis 2012. [DOI] [PubMed] [Google Scholar]
- 7. doi: 10.1093/cid/cis269. Pouillot R, Hoelzer K, Jackson KA, Henao OL, Silk BJ. Relative risk of listeriosis in Foodborne Diseases Active Surveillance Network (FoodNet) sites according to age, pregnancy, and ethnicity. Clin Infect Dis 2012. [DOI] [PubMed] [Google Scholar]
- 8. doi: 10.1093/cid/cis049. Hall RL, Jones JL, Hurd S, Smith G, Mahon BE, Herwaldt BL. Population-based active surveillance for Cyclospora onfection—United States, FoodNet, 1997–2009. Clin Infect Dis 2012; 54(Suppl 5):S411–7. [DOI] [PubMed] [Google Scholar]
- 9. doi: 10.1093/cid/cis244. Henao OL, Crim SM, Hoekstra RM. Calculating a measure of overall change in the incidence of selected laboratory-confirmed infections with pathogens transmitted commonly through food, Foodborne Diseases Active Surveillance Network (FoodNet), 1996–2010. Clin Infect Dis 2012; 54(Suppl 5):S418–20. [DOI] [PubMed] [Google Scholar]
- 10. doi: 10.1093/cid/cis266. Manikonda K, Palmer A, Wymore K, et al. Validating deaths reported in the Foodborne Diseases Active Surveillance Network: are all deaths being captured? Clin Infect Dis 2012. [DOI] [PubMed] [Google Scholar]
- 11. doi: 10.1093/cid/cis208. Ong KL, Apostal M, Comstock N, et al. Strategies for surveillance of pediatric hemolytic uremic syndrome: Foodborne Diseases Active Surveillance Network, 2000–2007. Clin Infect Dis 2012; 54(Suppl 5):S424–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. doi: 10.1093/cid/cis267. Cronquist AB, Mody RK, Atkinson R, et al. Impacts of culture-independent diagnostic practices on public health surveillance for bacterial enteric pathogens. Clin Infect Dis 2012. [DOI] [PubMed] [Google Scholar]
- 13. doi: 10.1093/cid/cis245. Hurd S, Patrick M, Hatch J, et al. Clinical laboratory practices for the isolation and identification of Campylobacter in FoodNet sites: baseline information for understanding changes in surveillance data. Clin Infect Dis 2012; 54(Suppl 5):S440–5. [DOI] [PubMed] [Google Scholar]
- 14. doi: 10.1093/cid/cis246. Clogher P, Hurd S, Hoefer D, et al. Assessment of physician knowledge and practices concerning STEC infection and enteric illness, 2009, FoodNet. Clin Infect Dis 2012; 54(Suppl 5):S446–52. [DOI] [PubMed] [Google Scholar]
- 15. doi: 10.1093/cid/cis247. Shiferaw B, Verrill L, Booth H, et al. Gender differences in food consumption: FoodNet population survey, 2006–2007. Clin Infect Dis 2012; 54(Suppl 5):S453–7. [DOI] [PubMed] [Google Scholar]
- 16. doi: 10.1093/cid/cis230. Shiferaw B, Solghan S, Palmer A, et al. Antimicrobial susceptibility patterns of Shigella isolates in FoodNet sites, 2000–2010. Clin Infect Dis 2012; 54(Suppl 5):S458–63. [DOI] [PubMed] [Google Scholar]
- 17. doi: 10.1093/cid/cis050. Ailes E, Scallan E, Berkelman RL, Kleinbaum DG, Tauxe RV, Moe CL. Do differences in risk factors, medical care seeking, or medical practices explain the geographic variation in campylobacteriosis in the FoodNet sites Clin Infect Dis 2012; 54(Suppl 5):S464–71. [DOI] [PubMed] [Google Scholar]
- 18. doi: 10.1093/cid/cis051. Hale CR, Scallan E, Dunn J, et al. Estimates of enteric illness attributable to contact with animals and their environments in the United States. Clin Infect Dis 2012; 54(Suppl 5):S472–9. [DOI] [PubMed] [Google Scholar]
- 19. doi: 10.1093/cid/cis052. Kendall ME, Crim S, Fullerton K, et al. Travel-associated enteric infections diagnosed after return to the United States, Foodborne Diseases Active Surveillance Network (FoodNet), 2004–2009. Clin Infect Dis 2012; 54(Suppl 5):S480–7. [DOI] [PubMed] [Google Scholar]
- 20. doi: 10.1093/cid/cis231. Chai SJ, White PL, Lathrop SL, et al. Salmonella enterica serotype enteritidis: increasing Incidence of domestically acquired infections. Clin Infect Dis 2012; 54(Suppl 5):S488–97. [DOI] [PubMed] [Google Scholar]
- 21. doi: 10.1093/cid/cis232. Murphree R, Garman K, Phan Q, Everstine K, Gould LH, Jones TF. Characteristics of foodborne disease outbreak investigations conducted by FoodNet sites, 2003–2008. Clin Infect Dis 2012; 54(Suppl 5):S498–503. [DOI] [PubMed] [Google Scholar]