Abstract
Misuse of prescription opioid medications has continued as a major public health problem in the United States. Review of major epidemiologic data bases shows that the prevalence of opioid misuse rose markedly through the 1990’s and the early part of the current decade. In this same period of time the number of prescriptions for chronic non-cancer pain increased markedly, and the intersection of these two public health problems remains a concern. Further, despite some leveling off of the overall rate of prescription opioid misuse in the past several years, surveillance data show high and increasing mortality associated with these drugs. Analysis of the 2006 National Survey of Drug Use and Health indicates the increasing prevalence of prescription opioid misuse is associated more with an increase in the general availability of these medications than misuse of the medications by those who were directly prescribed them. National Institute on Drug Abuse initiatives to address the prescription opioid problem include programs to stimulate research in the basic and clinical sciences, and education of physicians and other health personnel.
Keywords: prescription opioid misuse, drug addiction, chronic pain, prevalence of opioid abuse, NIDA National Institute on Drug Abuse
I. INTRODUCTION
Misuse of opioids in the United States is well described in anecdotal reports dating back to the 19th century (Musto 1999; Katz 2007). The misuse of prescription medications of all types was documented in the first American epidemiologic survey, which was completed in New York State in 1970. Since that time, survey data indicate different drugs cycled in and out of favor until the late 1990’s. At that time, all the major epidemiologic surveys documented a high prevalence rate of prescription opioid misuse (Colliver JD, 2006; Compton & Volkow, 2006a, 2006b; Zacny et al., 2003). Since the 1990’s, the rates of prescription opioid misuse have remained high, and many initiatives have recently emerged to better understand and address the problem. (Cicero & Inciardi, 2005; Cicero, Inciardi, et al., 2005; Cicero, Inciardi, & Munoz, 2005; Cicero, Inciardi, & Surratt, 2007; Colliver JD, 2006; Compton & Volkow, 2006b; Huang et al., 2006; Zacny et al., 2003).
This paper for the Special Edition “Perspectives on Prescription Drug Abuse and Relief of Pain for 2008” is a follow-up to an article by Compton and Volkow (2006b) concerning the major increase in opioid analgesic misuse and abuse in the United States and addresses some of the questions posed in that paper. This article updates the field on the current state of prescription opioid misuse by merging findings from various large-scale clinical and epidemiological databases. The strengths, weaknesses, and different methodological frameworks used to collect this data are examined. In addition, increases in the treatment of non-cancer pain are suggested as the most significant contributor to the increased availability of opioid medications and may be the main factor responsible for the prescription opioid misuse problem.
II. Epidemiology of Prescription Opioid Misuse
A. Terminology and Prevalence
Current literature regarding prescription opioid misuse is hampered by the lack of standardized definitions for the terms “misuse” and “abuse” and the idiosyncratic ways in which these terms are used (Compton & Volkow, 2006b), rendering it difficult to statistically combine and compare epidemiologic studies. For our purposes, we will use the definitions published in the NIDA “Research Report Series-Prescription Drugs: Abuse and Addiction” which defines prescription drug misuse as “taking a medication in a manner other than that prescribed or for a different condition than that for which the medication is prescribed” and prescription drug abuse as “the intentional misuse of a medication outside of the normally accepted standards of its use”. Other definitions of these terms were developed by an expert panel consisting of members from the American Society of Addiction Medicine, the American Academy of Pain Medicine, and the American Pain Society. The definitions they developed for misuse is “Use of a medication (for a medical purpose) other than as directed or indicated, whether willful or unintentional, and whether harm results or not” and for prescription opioid abuse: “Any use of an illegal drug, and the intentional self-administration of a medication for a nonmedical purpose such as altering one’s state of consciousness, e.g. getting high” (Katz, Adams, & Chilcoat 2007). Abuse and dependence are also defined by the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) (American Psychiatric Association, 1994). The DSM-IV definition of substance abuse is a “maladaptive pattern of substance use, leading to clinically significant impairment or distress, as manifested by one or more of the following, occurring within a 12-month period: 1) recurrent substance use resulting in a failure to fulfill major obligations at work, school, or home; 2) recurrent substance use in situations in which it is physically hazardous; 3) recurrent substance-related legal problems; or 4) continued substance use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of the substance.” The DSM-IV defines substance dependence as a cluster of three or more of the following symptoms clustering during a 12-month period: 1) tolerance to the effects of a substance; 2) withdrawal upon abrupt cessation; 3) using larger amounts than intended; 4) efforts to control or cut down use; 5) spending a great deal of time on the substance; 6) limiting social, occupational or recreational activities because of substance use; 7) use despite psychological or physical problems from the substance.
Additional difficulties arise when defining misuse, abuse and dependence in patients with pain conditions. For example, a person taking prescription opioid medication as directed already meets two of the DSM-IV criteria for an opioid dependence disorder due solely to the development of tolerance and physical dependence (withdrawal). On the other hand, a person developing addiction might be overlooked because the legal, social, and occupational criteria for dependence would manifest themselves less frequently in a person receiving their opioids by way of a legal and socially sanctioned mechanism (i.e., a prescription). To address this problem, three of the leading organizations in pain and addiction medicine have developed a consensus statement regarding the presenting symptoms of addiction in patients prescribed long-term opioids for chronic pain (American Pain Society, 2001). Addictive symptoms include one or more of the following: 1) impaired control regarding the use of the drug; 2) compulsive drug use; 3) continued drug use despite consequences; 4) unmanageable drug craving.
The term used most in this paper is “misuse”. This term encompasses prescription opioid use ranging from one time use of a prescription opioid not sanctioned by a physician, to extreme cases of abuse and addiction. We realize that misuse, abuse and addiction are conceptually and diagnostically separate and distinct (Grant et al., 2007), so we will use misuse as our “umbrella” term because it is not possible to have abuse or addiction without it. It is important to note that the studies and research articles referenced refer to all of these terms, thus making comparisons difficult. For that reason, when referring to other publications, the terms used by those authors are sometimes used to maintain consistency with the original.
Overall, following a period of apparent increases in the 1990’s, the epidemiologic data over the last three to four years shows a steady, high prevalence of prescription opioid misuse in the United States (Substance Abuse and Mental Health Services Administration, 2007; Johnston, et al., 2008). International prevalence data detailed below are now increasingly available, and show similar trends and concerning levels of misuse (International Narcotics Control Board, 2007). The epidemiologic data have been gathered using different methodologies compounding the problems of comparability between studies; however, an advantage is that trends are broadly consistent across surveys despite different methods, providing cross-validation of the findings.
1. National Survey on Drug Use and Health (NSDUH) (Substance Abuse and Mental Health Services Administration, 2007a)
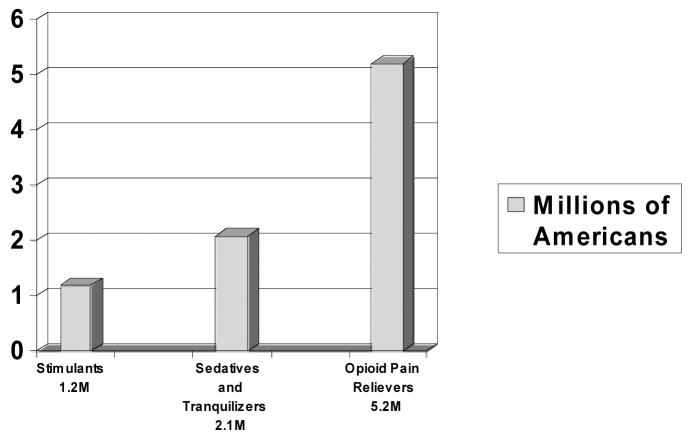
The NSDUH ascertains drug use patterns of a nationally representative sample of over 67,000, non-institutionalized individuals ages twelve and older. The section of NSDUH on “pain relievers” states that “over the counter” medications should not be included by the respondent, and that the questions pertain to the use “of any form of prescription pain relievers that were not prescribed for you or that you took only for the experience or feeling they caused.” According to the NSDUH, an estimated 5.2 million persons age 12 and over were current nonmedical users of prescription pain relievers in 2006, which is 2.1 percent of the population. This rate has been statistically unchanged since 2002. The numbers of individuals using all psychotherapeutics (pain relievers, sedatives, and stimulants) can be seen below (Figure 1) (Substance Abuse and Mental Health Services Administration, 2007a).
Figure 1. Current (last month) Number of Persons Age 12 or Older Misusing Prescription Medications in the United States in 2006.
Source: Substance Abuse and Mental Health Services Administration, 2007.
Combined data from 2002 to 2005 indicate that an annual average of 4.8 percent of persons aged 12 or older (11.4 million persons) used a prescription pain reliever nonmedically in the 12 months prior to the survey. Data from NSDUH 2002 to 2005 also indicate that an annual average of 57.7 percent of persons who first used prescription pain relievers nonmedically in the past year used hydrocodone products, and 21.7 percent used oxycodone products. Although male and female past-year initiates had similar rates of nonmedical use of oxycodone products (22.9 and 20.8 percent, respectively), male recent initiates were more likely than their female counterparts to have used hydrocodone products nonmedically (61.4 vs. 54.9 percent). Among persons who initiated nonmedical use of pain relievers in the past year, young adults aged 18 to 25 were more likely than their counterparts aged 12 to 17 or aged 35 to 49 to have used oxycodone products (27.4 vs. 20.3 and 14.9 percent) (Substance Abuse and Mental Health Services Administration, 2007b).
Of particular concern is that more persons age 12 and over initiated misuse of pain relievers (2.2 million) than any other illicit substance. By comparison, 2.1 million started using marijuana in the year prior to the interview (Figure 2) (Substance Abuse and Mental Health Services Administration, 2007c).
Figure 2. Past Year Initiates for Specific Illicit Drugs among Persons Age 12 or Older in the United States in 2006.
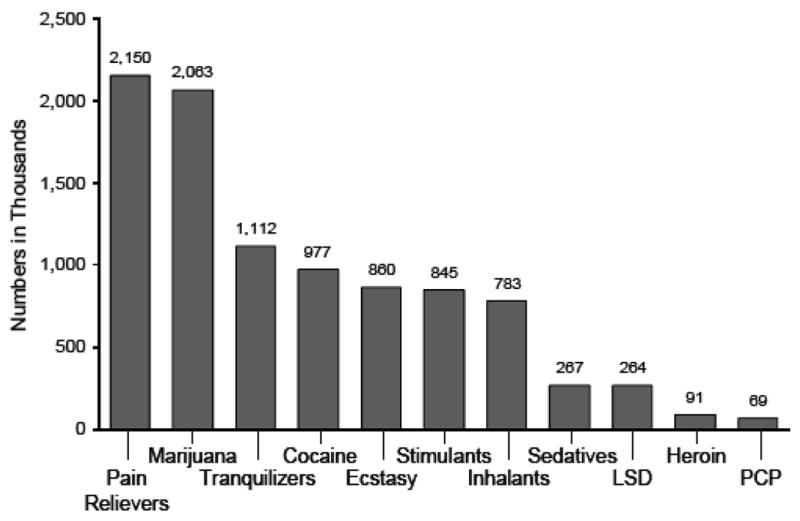
Source: Substance Abuse and Mental Health Services Administration, 2007.
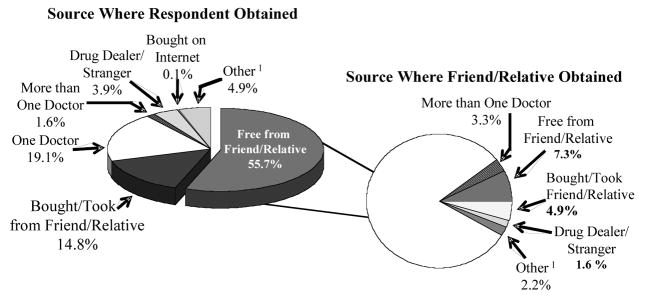
Perhaps the most interesting new fact from the recent NSDUH survey relates to the source of pain relievers that were misused. According to the 2006 NSDUH, 55.7% of those who misused pain relievers said they received their medication from friends and family and 80.7 percent of these individuals reported the friend or relative had obtained the drugs from just one doctor. Only 3.9% reported obtaining the drug from a drug dealer or stranger and only 0.1% reported buying the drug from the internet (Figure 3). A small study conducted in Miami (Inciardi; Surratt; Kurtz; & Cicero, 2007) also found a low percentage of misusers obtaining medications from the internet.
Figure 3. Source of Prescription Pain Relievers 2006 NSDUH.
Note: totals may not sum to 100% because of rounding or suppressed estimates are not shown. 1 The Other category includes the sources: “Wrote Fake Prescription Stole from Doctor’s Office/Clinic/Hospital/Pharmacy, and Some Other Way”
Source: Substance Abuse and Mental Health Services Administration, 2007.
2. Monitoring the Future (MTF), (Johnston et al., 2008)
The MTF is a series of large, annual surveys of nationally representative samples of public and private secondary school students throughout the coterminous United States. The study has been conducted with 12th graders since 1975 and 8th and 10th graders since 1991. In 2007, about 48,500 students from over 400 secondary schools participated in the survey.
MTF queries students about their use of prescription drugs while reminding them not to include medication prescribed by physicians. Among the 12th graders, annual prevalence rates for opioids increased substantially between 1990 to 2002, but have leveled off since 2003, and currently stand at about 9.0% (Figure 4) (Johnston et al., 2008). Considering one specific drug, reports of OxyContin use increased steadily among 12th graders from when it was first measured in 2002 until 2005, with annual prevalence rising from 4.0% to 5.5%, before dropping back to 4.3% in 2006 and 5.2% in 2007 (Johnston et al. 2008). The 8th and 10th grade students had a lower, but nonetheless concerning, level of past-year OxyContin use (1.8% and 3.9% past year prevalence respectively in 2007) (Johnston et al., 2008).
Figure 4. Annual Prevalence Rate of Narcotics Other than Heroin from 1975 to 2007.
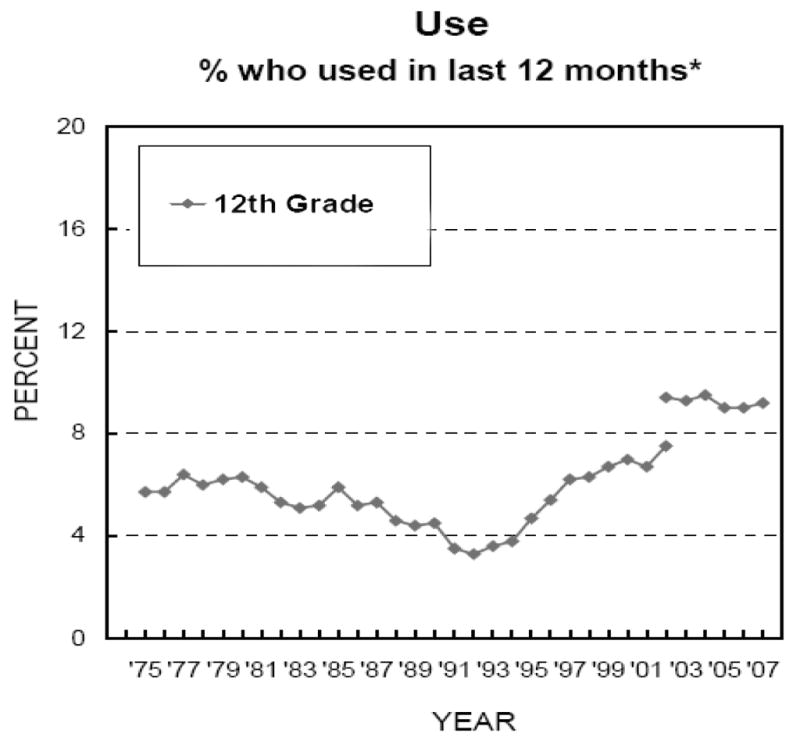
*Beginning in 2002, a revised set of questions on other narcotics use was introduced, in which Talwin, laudanum, and paregoric were replaced with Vicodin, OxyContin, and Percocet.
Only data from 12th graders is reported, because authors question validity of data from younger students for other narcotics category.
Source: Monitoring the Future study, The University of Michigan, 2008.
3. Drug Abuse Warning Network, 2005 (DAWN), Substance Abuse and Mental Health Services Administration (Substance Abuse and Mental Health Administration, 2007d)
The 2005 DAWN, the “New Dawn”, is a public health surveillance system that monitors drug-related hospital emergency department (ED) visits and drug-related deaths from a sample of Emergency Departments (ED) and medical examiners in select metropolitan areas. DAWN collects information by a chart-review process of patients admitted to participating hospitals for “any ED visit related to recent drug use”. The numbers of ED visits associated with drug misuse are placed in 3 categories: illicit drug use, under-age use of alcohol, and nonmedical use of pharmaceuticals. To be categorized as a DAWN case, the relationship between the ED visit and the drug use need not be causal; the drug needs only to be implicated in the visit. This approach accommodates cases where one or more drugs were involved but may or may not have directly caused the condition generating the ED visit, but at the same time avoids inclusion of current medications that are unrelated (Substance Abuse and Mental Health Administration, 2007d).
The initial DAWN surveillance system operated from 1994 to 2002, gathering data from 1995 up to and including 2002. DAWN data show that “drug-related” ED visits involving prescription opioids increased every year in this period from 42,857 to 108,320 ED visits, representing a 153% increase (Substance Abuse and Mental Health Administration, 2004). In 2002, prescription opioids represented 16% of total drug-related ED visits; with hydrocodone and oxycodone the most frequently mentioned opioids. Dependence was the most frequently mentioned motive underlying drug-related ED visits involving narcotic analgesics (47%).
The methodology for this survey changed in 2003, making comparisons before and after that date impossible. Over 1.4 million ED visits in 2005 were associated with drug misuse/abuse. Nonmedical use of pharmaceuticals was involved in nearly 600,000 of these ED visits. Of these visits, 33% involved opiates/opioids, and this was the largest single class of drugs represented. It is estimated that over 135,000 ED visits involved opiates/opioids. The most frequently listed opiates/opioids were hydrocodone products (37.8% of opiates/opioids), oxycodone products (31.6%), and methadone (30.4%) (Substance Abuse and Mental Health Administration, 2007d).
The mortality data collected by DAWN from the medical examiner system show an increase in deaths from prescription opioids over the years 1995 to 2002 in the metropolitan areas surveyed. Although these data are not representative of the United States population, they are useful for trend analysis in those areas surveyed (Substance Abuse and Mental Health Administration, 2004b).
4. Treatment Episode Data Set (TEDS), (Substance Abuse and Mental Health Services Administration, 2007e)
The (TEDS) system includes records for some 1.5 million substance abuse treatment admissions annually. While TEDS does not represent the total national demand for substance abuse treatment, it does comprise a significant proportion of all admissions for substance abuse treatment. In general, facilities reporting to TEDS receive some Federal or state funds to provide treatment services. For the United States as a whole, admissions for opiates other than heroin surged from 16,121 in 1995 to 67,887 in 2005, a 321% increase. By contrast, heroin admissions rose by only 12% during that same time period (from 227,989 to 254,345). Furthermore, the percentage of total admissions for heroin increased from 13.6% in 1995 to 13.8% in 2005, while opiates other than heroin increased from 2.0% in 1995 to 7.4% of all treatment admissions in 2005 (Substance Abuse and Mental Health Services Administration, 2007e).
5. Adverse Events Reporting System, (AERS) (United States Food and Drug Administration, 2007) and National Vital Statistics (Paulozzi, 2007)
The AERS is a computerized information database operated by the United States Food and Drug Administration (FDA) since 1998. The system is designed to support the FDA’s post-marketing safety surveillance program for all approved drug and therapeutic biologic products. The data come from two sources: the FDA receives adverse drug reaction reports from manufacturers as required by Federal regulation, and health care professionals and consumers send reports voluntarily through the Med Watch program. The reports in AERS are evaluated by clinical reviewers to detect safety signals and to monitor drug safety. This analysis forms the basis for further epidemiological studies when appropriate (United States Food and Drug Administration, 2007).
AER data from 1998 to 2005 show that 7 of the most frequent drugs suspected in death and serious nonfatal outcomes were pain medications. The overall relative increase for deaths caused by prescription medications of all types was 4 times faster than the growth in total US outpatient prescriptions, with opioid analgesics representing the largest percentage of this increase, as described in a publication by Moore, Cohen, & Furberg (2007). These findings are further confirmed by evaluation of drug –related mortality using death certificate data obtained from additional sources, which showed the largest percentage increases in prescription medication deaths between 1999 and 2003 was due to the prescription opioid methadone (275% increase), which has been increasingly prescribed for chronic pain during that time (Wysowski, 2007). A recent study by Paulozzi (2007) using data from the National Vital Statistics system, has shown that, between 1999 and 2002, the number of deaths due to prescription opioids increased 91.2%, while heroin and cocaine deaths increased 12.4% and 22.8%, respectively..
6. International
The international community has also seen an increase in reports about prescription opioid misuse. The International Narcotics Control Board (INCB) of the World Health Organization and United Nation, published in their Annual Report (International Narcotics Control Board, 2007) that prescription drug abuse is a major problem in the United States, Canada, and Mexico, and that, worldwide, prescription drug misuse was expected to exceed illicit drug use by 2007. Researchers have found that prescription opioids have replaced heroin as the most prevalent opioid in a longitudinal multi-site study of injection and non-injection drug users from around Canada (Fischer, et al. 2006). As in the United States, the Canadian researchers also reported that most individuals misusing prescription opioids stated they obtained them directly from the medical system, or indirectly from friends or relatives. A longitudinal cohort study of German youth showed similar rates of prescription opioid misuse as found in the United States, though direct United States-European comparisons are difficult because of methodological issues (Perkonigg et al., 2006). For example, single-ingredient hydrocodone (Dicodid™; Abbott, Wiesbaden, Germany) is prescribed for comparatively less common disorders in Europe, (i.e. for severe cough symptoms such as in chronic lung diseases or broncoscopy procedures) (Martindale: The Complete Drug Reference, 2007, Winkler, Mueller et al., 2007). Therefore, the high rate of misuse of this medication in the United States, where it is widely prescribed for many pain conditions, is not comparable to the misuse rates in Europe, where it is prescribed comparatively rarely. Lastly, mainland China reports a 16-fold increase of registered drug users from 1990 to 2004. Heroin remains the most common opioid used, however, polydrug use with prescription opioids was also common (Liu, Lian, & Zhao, 2006).
In summary, available data show an epidemic of prescription opioid misuse and consequences building in the United States over the decade of the 1990’s and in the current decade. Recently, prescription opioids replaced marijuana as the substance with the most new initiates (Substance Abuse and Mental Health Services Administration, 2007). Perhaps most concerning are the new data showing high and increasing rates of mortality associated with prescription opioids (United States Food and Drug Administration, 2007; Paulozzi, 2007).
B. Demographics
1. Age and gender as related to prescription opioid misuse and chronic pain
Substance misuse is generally a disease of the young. NSDUH data from 2006, report approximately 5.2 million persons in the United States ages 12 or older were current (last 30 days) nonmedical users of prescription pain relievers. Misuse of these substances was most prevalent in young adults (ages 18–25), followed by adolescents (ages 12–17) and adults (ages 26+) (Substance Abuse and Mental Health Services Administration, 2007). However, because prescription opioid use is so tied to chronic pain, when studying subgroups of individuals with chronic pain, opioid use has been reported to increase with age (Luo, Pietrobon, & Hey, 2004). Even though the use of prescription opioids increases as patients with chronic pain age, there are indications that risk of misuse may decline with increasing age in this group of chronic pain patients prescribed opioids (Webster, 2005).
Another significant difference between prescription opioid misuse and illicit drug abuse is the greater nonmedical use of opioids by adolescent females (Boyd, 2006). This study also showed the motive for use of prescription opioids was more consistent with a therapeutic indication (79%) than for other prescription medication misuse. It was also shown that those who self medicate for pain, as compared to the group that endorsed other reasons of misuse, are also more likely to have lower Drug Abuse Screening Test Scores (DAST) scores, lower marijuana use, and lower alcohol use.
In a review of 11 studies of working and community populations, Wijnhoven found women reported a higher prevalence of musculoskeletal pain than men; this was consistent with his findings showing a prevalence rate of pain for women greater than men in most anatomic pain sites studied (2006). This and other factors contribute to the significantly greater exposure to prescription opioids that women face (Simoni-Wastila, 2000) and to the higher rates of prescription opioid misuse among women in data from the 1991 National Household Survey on Drug Abuse, based on a sample of 3185 persons (Simoni-Wastila, Ritter, Strickler, 2004). However, analyses of data from more recent national studies, the National Epidemiologic Survey on Alcohol and Related Conditions 2002 (Huang, 2006), and the NSDUH 2007 (Substance Abuse and Mental Health Services Administration, 2007) show that men generally have a higher prevalence rate of prescription opioid misuse than women.
2. Location of Residence, urban/rural as related to prescription opioid abuse and chronic pain
Substance abuse treatment admissions data show an increasing proportion of patients reporting primary prescription opioid abuse from rural areas (Substance Abuse and Mental Health Administration, 2007). Rural areas may be more susceptible to problems associated with prescription opioids due to a number of factors including: the greater social acceptability of a “legal” product; the reduced availability of low cost heroin in rural areas; and the long history of rural prescription drug abuse of all types (Cicero, et al., 2007). The increasing prevalence in rural areas may also be associated with chronic pain and its relationship to disability claims. Depressed economic conditions in certain rural areas result in a situation of “secondary gain”; where an individuals would rather claim reduced disability payments or other forms of economic compensation, which reinforces the chronic pain state, rather than work at an unpleasant job, or risk unemployment (Fishbain, Rosomoff, Cutler, & Rosomoff, 1995; Fishbain, Rosomoff, Cutler, & Steele-Rosomoff, 1995; Rosomoff, Fishbain, Cutler, & Steele-Rosomoff, 1995). There are some indications that prescription opioid misuse is spreading to inner-city areas also (Vivian, et al., 2005).
III. ASSOCIATION OF CHRONIC NON-CANCER PAIN to PRESCRIPTION OPIOID MISUSE
A. Chronic Non-Cancer Pain
1. Definition, Background, and History
The most widely accepted definition of chronic pain is: “Pain persisting more than 90 days beyond the period of injury” (International Association for the Study of Pain, 1986). However, there is no objective measurement of pain, and psychological variables play a great role in pain perception. An unanswered question results from the lack of an objective measure of pain; that is, whether chronic pain persisting without anatomic or physiologic correlates responds differently to opioid treatment than chronic pain that is correlated to objective abnormalities. Specifically, should opioids be given to a patient with a complaint of chronic non-cancer pain, without anatomic or physiologic correlates? Research indicates abnormal drug-seeking behavior was not seen when long-term opioids were used for post-herpetic neuralgia, phantom limb pain, chronic spinal pain, and pain of mixed but well defined origin (Collett 1998). However this was not a prospective study, but a review of a number of published papers. Less is known regarding patients with somatoform disorder, somatization disorder, and pain with psychiatric comorbidity, and pain with substance abuse comorbidity.
Chronic pain and disability conditions are extremely prevalent in the United States (National Center for Health Statistics, 2007). This has lead the United States Congress to designate the years 2001 to 2010 the “Decade of Pain Research and Control” (American Pain Society, 2008) A recent Centers for Disease Control report stated that 26% of all adult Americans had pain lasting over twenty-four hours in the past month prior to the study interview. (National Center for Health Statistics, 2007) These numbers are consistent with the WHO Collaborative Study of Psychological Problems in General Health Care, which found 22% of patients had pain persisting 6 months or more in the year preceding the study interview (Gureje, et al., 1998). Similar chronic pain prevalence numbers were also found in data reported from single country studies done in the United States (25% reported one day of pain in the last 30), Australia (17% of men and 20% of women reported 3 months of pain in the last 6 months), and Denmark (19% reported pain lasting 6 months or more) (Strine et al., 2005, Blythe et al. 2001; Erickson et al., 2003). Pain is the most common symptom of people presenting for medical care (Stewart et al., 2003) and back pain in particular has been reported to be the second leading reason people seek medical care in the United States (Gureje et al., 1998). Pain is most often thought of as a symptom of disease. However, in its own right, pain is a condition which may causes injury to various organ systems, resulting in decreased quality of life, decreased longevity, and increased coronary heart disease, and for that reason requires attention and treatment (Stewart et al., 2003; Zhu et al., 2007).
The use of opioids for acute pain is a well accepted principle of medicine. However the indications for the use of opioids for chronic non-cancer pain are based on generally small clinical trials or are not uniformly accepted (Ballantyne & Mao, 2003; Martell et al., 2007). The current complex situation has evolved in the years after World War Two. At that time, there was a great hesitancy, and many prohibitions, surrounding the use of opioids. This was true even with cancer pain. The efficacy and safety of opioids for chronic cancer pain became apparent in the 1970’s and 1980’s (World Health Organization, 1986). The successful use of opioids for chronic cancer pain, led to exploring their use in chronic noncancer pain. A seminal paper by Portenoy and Foley (1986) advocated the use of opioids in cases of intractable pain in patients with no history of substance abuse. This paper of 38 cases encouraged many other similar reports; however, all have small sample sizes with short follow-up periods (Ciccone et al., 2000; Merry, Schug, Richards, & Large, 1991; Schofferman, 1993, 1999; Schug, Merry, & Acland, 1991; Zenz, Strumpf, & Tryba, 1992). Further, the use of opioids for chronic non-malignant pain proved more problematic as time progressed (Portenoy, 2004).
The problems that developed with chronic opioid use, including prescription opioid misuse, eventually resulted in an overarching concept of the need for “balance” (World Health Organization 2000). Opioids are effective and indispensable and must be available to relieve pain and suffering, but they also have a potential for misuse and must be controlled. This principle is found in The Controlled Substances Act of 1970, which provides the legal authority to the United States Attorney General to regulate opioid use, and is also clearly enumerated in the policy statements of numerous public and private organizations the world over (Zenz, 1993; Blengini, 2003) The situation of balance, where the greatest amount of suffering from chronic noncancer pain is relieved with the least amount of suffering caused by opioid abuse, is difficult to achieve. Despite widespread public and professional attention, and other efforts at control, prescription opioid abuse remains a significant problem in the United States and other countries around the world.
2. Opioid Effectiveness in Treating Chronic Non-Cancer Pain
The next point to consider is the effectiveness of the increased treatment of chronic non-cancer pain. In a recent systematic review of the literature Martell 2007 confirms earlier literature reviews (Ballantyne & Mao, 2003; Von Korff, 2004) that fail to show evidence that long term opioid administration reduces pain or improves functioning.
In fact, an increasing body of evidence is developing from both animal and human studies regarding the development of hyperalgesia as a result of chronic opioid administration (Mao, 2002, 2004, 2006). The scientific evidence base is far from complete however, chronic opioid administration results in tolerance, which in turn may be partially responsible on a cellular level for dependence and addiction. Tolerance is a well recognized side effect of opioid administration, as is heightened pain sensitivity during opioid withdrawal in both animals and humans. These changes may indicate that neural plasticity is responsible for tolerance and the development of a pro-nocioceptive mechanism in the nervous system that counters the effect of the administered opioid. Both of these processes together could not only decrease the opioid effect, but cause a hyperalgesic response (Mao, 2002, 2004, 2006), but further research is required in this area to confirm these findings and more extensively relate them to the human clinical condition. In one preliminary study in this area; patients with chronic pain who detoxified from prescription opioids, less pain was reported after detoxification than when on the opioid medication at the time of admission (Miller, Swiney, & Barkin, 2006).
Despite the numerous well known problems inherent with opioid medications, non-opioid medications also carry significant risks including gastrointestinal dysfunction and bleeding, renal impairment, and cardiovascular and central nervous system risks (Ashburn, and Staats, 1999). Therefore, opiophobia (the fear of prescribing opioid medication on the part of physicians, or the exaggerated fear that taking these medications will result in addiction on the part of patients) can cause increased suffering and increased medical risks to millions of Americans (National Institute on Drug Abuse, 2008).
3. Association of Chronic Non-Cancer Pain with Misuse
A large number of opioid prescriptions are written for the treatment of chronic non-cancer pain. In an oft-quoted study, the percentage of opioids prescribed for musculoskeletal pain doubled from 1980 to 2000 from 8% to 16% (Caudill-Slosberg, Schwartz, & Woloshin, 2004). This is consistent with a 90% increase in use of prescription opioids between 1997–2000 (ARCOS, 2007). This increase in number of opioid prescriptions parallels increases in the prevalence of the treatment of chronic noncancer pain (Gilson, et al., 2005; Gilson, et al., 2004; Joranson, et al., 2000).
The risk associated with the increased treatment of chronic non-cancer pain with prescription opioids must also be considered. It is the unfortunate fact that some patients exposed to chronic opioids will misuse them. Estimates of developing addictive behaviors around their prescription opioids vary from 4% (Adams et al., 2001) to 31% (Reid et al., 2002). The rates of misuse vary widely because of the definitions of misuse applied and differences in patient populations. Adams reported the lowest misuse rate and used opioid contracts with 41% of the patients. In one of the few prospective cohort studies of predictors of opioid misuse in chronic pain patients, 32% were found to misuse their opioid medications, and the predictors of this misuse were found to be younger age, past cocaine or alcohol abuse, and drug or DUI conviction (Ives et al., 2006).
The metric most often used to track prescription opioid medication misuse is the absolute number of cases of misuse. This treats prescription opioid medication differently than other medications where a risk-benefit assessment, rather than the sheer volume of adverse events, is used to assess the “risk” of a drug. The risk-benefit ratio, or therapeutic index, is expressed as the rate at which an adverse event occurs, which in turn is the number of adverse events divided by the number of people using the drug therapeutically. This has significant policy implications regarding assessing a medications “risk” and subsequent controlled substance scheduling. In a recent analysis of the problem of assessing an opioid medications risk (Cicero, Surratt et al., 2007), it was shown that there is an excellent correlation between the therapeutic exposure to opioid medications and the risk of abuse. This in turn suggests that a ratio is a better indicator of misuse because it will not be subject to shifts in the absolute numbers. The therapeutic index is the rate used by the pharmaceutical industry and regulatory agencies for reporting adverse events of medication, in this case misuse, and may provide the best indicator of a risk-benefit ratio. For example, the authors found that when calculated as cases of misuse per 100,000 population, hydrocodone was as highly misused as any other drug studied (e.g. extended release oxycodone) but when calculated with a ratio of cases of misuse/1000 therapeutic prescriptions, hydrocodone falls to the lower end of the risk spectrum.
B. Cancer Pain Treatment
Cancer patients are another patient group with increased use of prescription opioids (World Health Organization, 2000). Much of the enthusiasm for the long-term opioid treatment of chronic noncancer pain was based on the success of opioid treatment for cancer pain in the 1970’s and 1980’s. In the 1970’s and 1980’s, when cancer was often a fulminate disease and little attention was given to patient function. Fortunately, the prognosis for survival with many types of cancer has improved. In many cases cancer should be considered a chronic illness with periods of long remission, rather than an end-of-life event. This shift necessitates re-examination of the risk of prescription opioids. Reevaluation of the long-term high-dose administration of opioids with a cancer diagnosis should be considered relative to the survivability of the cancer (Ballantyne, 2003, 2007).
It can be seen that over the last twenty years, the two significant public health problems of chronic pain and opioid misuse have converged. This is a complex issue. The treatment of one problem, chronic non-cancer pain, is associated with the increased risk of prescription opioid misuse. By clarifying the association of prescription opioid misuse and chronic noncancer pain, possible new approaches for the treatment of these problems as well as future research directions may become more apparent.
IV. National Institute on Drug Abuse (NIDA) Initiatives and Prescription Opioid Abuse
When used properly, opioid analgesics have the potential to relieve pain and suffering, even in those with a history of substance abuse. However, as with other drugs of abuse, the use of prescription opioids can lead to misuse and addiction. The National Institute on Drug Abuse has undertaken a number of initiatives to facilitate the development of science that will inform medical professionals, policy makers, and the public health community about the proper use of prescription opioids and the treatment of opioid addiction.
A robust portfolio of research addressing prescription opioid misuse has been funded by NIDA. These studies span the range from basic science to treatment and services research. A recent initiative focused on the problem of prescription opioid use and the treatment of pain (National Institute in Drug Abuse 2008b). Funded grants include human and animal studies across different scientific disciplines including clinical neurobiology, genetics, molecular biology, prevention, treatment, and services research. This research may help us address important questions including: determining differences in addiction potential among patients being treated for chronic pain; uncovering mechanisms of hyperalgesia with sustained opioid treatment; and understanding the basic mechanisms involved in pain and how their interaction with prescription opioids influences addiction potential.
In addition, NIDA continues to encourage applications on prescription opioid misuse through an on-going funding announcement reissued in early 2008 (National Institute in Drug Abuse, 2008c) Some of the objectives of this initiative include: research to determine how the misuse of prescription drugs—particularly by pregnant women, children, and adolescents—might increase the lifetime risk of substance abuse and addiction; animal models to probe the effects of prescription opioids on neurobiological, neurochemical, and neurobehavioral processes; determining the health consequences of prescription opioid drug abuse and the underlying pathophysiology in diverse populations (for example, people with HIV/AIDS and other infectious diseases, adolescents, the elderly, and women); studies that develop and evaluate treatment approaches that maintain abstinence from prescription opioid drug misuse and prevent relapse; and research that adapts existing, or develops new and innovative treatments.
The Clinical Trials Network of NIDA is sponsoring the first large-scale multi-site national-level study on the treatment of addiction to prescription pain medication. This study tests the effectiveness of buprenorphine/naloxone tablets, along with different models of drug counseling, in patients addicted to prescription opioids (National Institute on Drug Abuse, 2008d). Participants include individuals who take prescription opioids for mild to moderate pain and have become addicted, as well as those who misuse opioids for nonmedical reasons. This study is significant because most research on treatment for opioid addiction has been done with patients addicted to heroin, not prescription drugs. In addition, this study may help determine if patients who become addicted to prescription opioids in the course of treatment for pain will respond differently to intervention than those who become addicted from recreational use.
To promote small business, the Federal government has instituted a program of awarding Small Business Innovation Research (SBIR) and Technology Transfer (STTR) grants and contracts (National Institute on Drug Abuse, 2008e). Through this mechanism, projects have been funded exploring the use of technology to manage pain in minority populations and developing screening and diagnostic tools physicians use to assess the potential for prescription opioid drug abuse in their patients.
NIDA has also sponsored activities to inform the public and medical community about the problem of prescription opioid misuse. Basic facts and research findings on prescription opioids can be found on the NIDA website. Last year, NIDA sponsored a 2-day meeting (March 4–5, 2007) held in conjunction with the American Medical Association and NIH Pain Consortium, with over 500 medical professionals, scientific researchers, and interested members of the public (National Institute on Drug Abuse, 2008f). Presenters discussed the science behind opioid addiction, adolescent misuse of opioids, benefits of opioid use when prescribed for cancer pain, development of a newer generation of pain relievers devoid of tolerance or dependence, real-time functional magnetic resonance imaging as a tool to allow patients to better manage their own pain, and other topics. This meeting provided a unique opportunity for the practice and research communities to dialogue about the problems of prescription opioid abuse and new areas of research.
Ongoing studies supported by NIDA will build knowledge addressing questions regarding the long term effect of chronic opioid administration for chronic non-cancer pain, alternative medications (such as buprenorphine) for use in patients with a history of addiction and chronic pain, and the role of tolerance and hyperalgesia with chronic opioid administration, new receptors that may play a role in pain modulation, novel delivery systems for medications to lessen abuse potential, and the development of new medications with less addiction potential.
V. CONCLUSIONS
Review of the major epidemiologic databases show that the prevalence of opioid misuse rose dramatically through the 1990’s and the early part of the current decade, stabilizing at a high level over the past few years. Many factors have probably contributed to the increased prevalence of prescription opioid misuse, including changes in medication formulations, pharmaceutical industry marketing, and the aging population (Compton & Volkow, 2006b). However, the situation that has been most associated with prescription opioid misuse is the increased treatment of chronic non-cancer pain (Ballantyne & Mao, 2003; Caudill-Slosberg et al., 2004).
The increase in numbers of prescriptions may contribute to misuse by two main mechanisms. One may be that those prescribed opioids to treat pain have developed a drug misuse problem. However, only about 20% of misusers report obtaining their prescription opioids from their own physician (Substance Abuse and Mental Health Administration, 2007). The other mechanism that could explain the way in which the increase in pain treatment (and the resultant increased prescriptions) could contribute to prescription opioid misuse is through increased environmental availability of opioid medications. This mechanism may be responsible for the increased prevalence of prescription opioid misuse. Considering that 55% of misusers obtain opioids from friends and family and 80% of the friends and family obtain the medication from a physician, it appears that the majority of the prescription opioid problem results from increased availability from prescriptions, albeit by an indirect route. Many or most of these prescriptions are likely from the treatment of acute and chronic pain. Thus, pain treatment may put some patients at risk for developing misuse themselves, but it places a larger number of persons at risk of misuse through sharing of medications with family and friends.
In summary, the greatest factor associated with increasing prevalence of prescription opioid misuse appears to be the increased environmental exposure. This appears to be in large part due to the increased number of prescriptions of these medications in the enhanced treatment of chronic non-cancer pain. Over the last twenty years these two significant public health problems have converged, and by clarifying the association of chronic non-cancer pain and prescription opioid misuse, possible new approaches for the prevention and treatment of these problems, as well as future research directions may become more apparent.
Finally, efforts directed at reducing the problem of prescription opioid misuse should be carefully evaluated to prevent unintended consequences, specifically the under treatment of pain of all types. Availability of opioid medications should be maintained for those that have legitimate medical needs, including those with a history of a substance abuse problem, but consideration of tolerance, hyperalgesia, and misuse should be part of the prescription decision.
Footnotes
Conflict Statement: None
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institutes of Health or the United States Department of Health and Human Services.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/journals/pha.
References
- Adams NJ, Plane MB, Fleming MF, Mundt MP, Saunders LA, Stauffacher EA. Opioids and the treatment of chronic pain in a primary care sample. Journal of Pain and Symptom Management. 2001;22(3):791–796. doi: 10.1016/s0885-3924(01)00320-7. [DOI] [PubMed] [Google Scholar]
- American Pain Society. Decade of Pain Control and Research. [Accessed January 8 2008];Newsletter. 2008 January 8, 2008 web address: http://www.ampainsoc.org/decadeofpain/
- American Pain Society. Definitions related to the use of opioids for the treatment of pain: a consensus document from the American Academy of Pain Medicine, the American Pain Society, and the American Society of Addiction Medicine. 2001. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders-IV. Vol. 2000 Washington., D.C: American Psychiatric Association; 1994. [Google Scholar]
- ARCOS: Automation of Reports and Consolidated Orders System. US Department of Justice; [Accessed May 3, 2007]. Web site. http://www.deadiversion.usdoj.gov/arcos/ [Google Scholar]
- Ashburn MA, Staats PS. The management of chronic pain. Lancet. 1999;353:1865. doi: 10.1016/S0140-6736(99)04088-X. [DOI] [PubMed] [Google Scholar]
- Ballantyne JC. Chronic pain following treatment for cancer: the role of opioids. Oncologist. 2003;8(6):567–575. doi: 10.1634/theoncologist.8-6-567. [DOI] [PubMed] [Google Scholar]
- Ballantyne JC. Opioid misuse in oncology pain patients. Current Pain and Headache Reports. 2007;11(4):276–282. doi: 10.1007/s11916-007-0204-6. [DOI] [PubMed] [Google Scholar]
- Ballantyne JC, Mao J. Opioid therapy for chronic pain. New England Journal of Medicine. 2003;349(20):1943–1953. doi: 10.1056/NEJMra025411. [DOI] [PubMed] [Google Scholar]
- Blengini C, Joranson D, Ryan K. Italy reforms national policy for cancer pain relief and opioids. European Journal of Cancer Care. 2003;12(1):28–34. doi: 10.1046/j.1365-2354.2003.00325.x. [DOI] [PubMed] [Google Scholar]
- Blyth FM, March LM, Brnabic AJ, Jorm LR, Williamson M, Cousins MJ. Chronic Pain in Australia: a prevalence study. Pain. 2001;89(2–3):127–134. doi: 10.1016/s0304-3959(00)00355-9. [DOI] [PubMed] [Google Scholar]
- Boyd CJ, McCabe SE, Cranford JA, Young A. Adolescents’ Motivations to Abuse Prescription Medications. Pediatrics. 2006;118(6):2472–80. doi: 10.1542/peds.2006-1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caudill-Slosberg MA, Schwartz LM, Woloshin S. Office visits and analgesic prescriptions for musculoskeletal pain in US: 1980 vs. 2000. Pain. 2004;109(3):514–519. doi: 10.1016/j.pain.2004.03.006. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control. [accessed December 17, 2007];New Report Finds Millions in Pain. 2007 Available at: http://www.cdc.gov/nchs/pressroom/06facts/hus06.htm.
- Ciccone DS, Just N, Bandilla EB, Reimer E, Ilbeigi MS, Wu W. Psychological correlates of opioid use in patients with chronic nonmalignant pain: a preliminary test of the downhill spiral hypothesis. Journal of Pain and Symptom Management. 2000;20(3):180–192. doi: 10.1016/s0885-3924(00)00177-9. [DOI] [PubMed] [Google Scholar]
- Cicero TJ, Inciardi JA. Diversion and abuse of methadone prescribed for pain management. Journal of the American Medical Association. 2005;293(3):297–298. doi: 10.1001/jama.293.3.297. [DOI] [PubMed] [Google Scholar]
- Cicero TJ, Inciardi JA, Munoz A. Trends in abuse of Oxycontin and other opioid analgesics in the United States: 2002–2004. Journal of Pain. 2005;6(10):662–672. doi: 10.1016/j.jpain.2005.05.004. [DOI] [PubMed] [Google Scholar]
- Cicero TJ, Inciardi JA, Surratt H. Trends in the use and abuse of branded and generic extended release oxycodone and fentanyl products in the United States. Drug and Alcohol Dependence. 2007 doi: 10.1016/j.drugalcdep.2007.05.008. [DOI] [PubMed] [Google Scholar]
- Collett B-J. Opioid tolerance: the clinical perspective. The British Journal of Anaesthesia. 1998;81:58–68. doi: 10.1093/bja/81.1.58. [DOI] [PubMed] [Google Scholar]
- Colliver JD, KL, Dai L, et al. Misuse of prescription drugs: data from the 2002, 2003, and 2004 National Surveys on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2006. [Google Scholar]
- Compton WM, Volkow ND. Abuse of prescription drugs and the risk of addiction. Drug and Alcohol Dependence. 2006a;83(Suppl1):S4–7. doi: 10.1016/j.drugalcdep.2005.10.020. [DOI] [PubMed] [Google Scholar]
- Compton WM, Volkow ND. Major increases in opioid analgesic abuse in the United States: concerns and strategies. Drug and Alcohol Dependence. 2006b;81(2):103–107. doi: 10.1016/j.drugalcdep.2005.05.009. [DOI] [PubMed] [Google Scholar]
- Dominick K, Bosworth H, Dudley T, Waters S, Campbell L, Keefe F. Patterns of Opioid Analgesic Prescription Among Patients with Osteoarthritis. Journal of Pain & Palliative Care Pharmacotherapy. 2004;18(1):31–46. [PubMed] [Google Scholar]
- Edlund MJ, Steffick D, Hudson T, Harris KM, Sullivan M. Risk factors for clinically recognized opioid abuse and dependence among veterans using opioids for chronic non-cancer pain. Pain. 2007;129(3):355–362. doi: 10.1016/j.pain.2007.02.014. [DOI] [PubMed] [Google Scholar]
- Eriksen J, Jensen MK, Sjogren P, Ekholm O, Rasmusen NK. Epidemiology of chronic non-malignant pain in Denmark. Pain. 2003;106(3):221–228. doi: 10.1016/S0304-3959(03)00225-2. [DOI] [PubMed] [Google Scholar]
- Fischer B, Rehm J, Patra J, Cruz MF. Changes in illicit opioid use across Canada. Canadian Medical Association Journal. 2006;175(11):1385. doi: 10.1503/cmaj.060729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishbain DA, Rosomoff HL, Cutler RB, Rosomoff RS. Secondary gain concept: a review of the scientific evidence. Clinical Journal of Pain. 1995;11(1):6–21. [PubMed] [Google Scholar]
- Fishbain DA, Rosomoff HL, Cutler RB, Steele-Rosomoff R. I. Do chronic pain patients’ perceptions about their preinjury jobs determine their intent to return to the same type of job post-pain facility treatment? Clinical Journal of Pain. 1995;11(4):267–278. doi: 10.1097/00002508-199512000-00004. [DOI] [PubMed] [Google Scholar]
- Foreman RF, Marlowe DB, McLellan AT. The Internet as a Source of Drugs of Abuse. Current Psychiatry Reports. 2006;8(5):377–82. doi: 10.1007/s11920-006-0039-6. [DOI] [PubMed] [Google Scholar]
- Gilson AM, Joranson DE, Maurer MA, Ryan KM, Garthwaite JP. Progress to achieve balanced state policy relevant to pain management and palliative care: 2000–2003. Journal of Pain and Palliative Care Pharmacotherapeutics. 2005;19(1):13–26. [PubMed] [Google Scholar]
- Gilson AM, Ryan KM, Joranson DE, Dahl JL. A reassessment of trends in the medical use and abuse of opioid analgesics and implications for diversion control: 1997–2002. Journal of Pain Symptom Management. 2004;28(2):176–188. doi: 10.1016/j.jpainsymman.2004.01.003. [DOI] [PubMed] [Google Scholar]
- Grant BF, Compton WM, Crowley TJ, Hasin DS, Helzer JE, Li TK, et al. Errors in assessing DSM-IV substance use disorders. Archives of General Psychiatry. 2007;64(3):379–380. doi: 10.1001/archpsyc.64.3.379. author reply 381–372. [DOI] [PubMed] [Google Scholar]
- Gureje O, Von Korff M, Simon GE, Gater R. Persistent Pain and Well-being: a World Health Organization Study in Primary Care. Journal of the American Medical Association. 1998;280(2):147–151. doi: 10.1001/jama.280.2.147. [DOI] [PubMed] [Google Scholar]
- Heins J, Heins A, Grammas M, Costello M, Huang K, Misha S. Disparities in Analgesia and Opioid Prescribing Practices for Patients With Musculoskeletal Pain in the Emergency Department. Journal of Emergency Nursing. 2006;32(3):219–224. doi: 10.1016/j.jen.2006.01.010. [DOI] [PubMed] [Google Scholar]
- Huang B, Dawson DA, Stinson FS, Hasin DS, Ruan WJ, Saha TD, et al. Prevalence, correlates, and comorbidity of nonmedical prescription drug use and drug use disorders in the United States: Results of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2006;67(7):1062–1073. doi: 10.4088/jcp.v67n0708. [DOI] [PubMed] [Google Scholar]
- Inciardi JA, Surratt HL, Kurtz SP, Cicero TJ. Mechanisms of prescription drug diversion among drug-involved club- and street-based populations. Pain Medicine. 2007;8(2):171–183. doi: 10.1111/j.1526-4637.2006.00255.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Association for the Study of Pain., C. o. c. p. Classification of chronic pain. Pain. 1986;(suppl 3):S1–S226. [PubMed] [Google Scholar]
- International Narcotics Control Board Press Release No. 4 “Abuse of Prescription Drugs to Surpass Illicit Drug Abuse”. [Accessed December 18, 2007];Drug Watch International. 2007 Mar;XII(1) http://www.drugwatch.org/Newsletters/March%202007%20Newsletterpdf. [Google Scholar]
- Ives TJ, Chelminski PR, Hammett-Stabler CA, Malone RM, Perhac JS, Potisek NM, et al. Predictors of opioid misuse in patients with chronic pain: a prospective cohort study. BMC Health Services Research. 2006;6:46. doi: 10.1186/1472-6963-6-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national results on adolescent drug use: Overview of key findings, 2007. Bethesda, MD: National Institute on Drug Abuse; 2008. [Google Scholar]
- Joranson DE, Ryan KM, Gilson AM, Dahl JL. Trends in medical use and abuse of opioid analgesics. Journal of the American Medical Association. 2000;283(13):1710–1714. doi: 10.1001/jama.283.13.1710. [DOI] [PubMed] [Google Scholar]
- Katz N. Opioids: after thousands of years, still getting to know you. Clinical Journal of Pain. 2007;23(4):303–306. doi: 10.1097/AJP.0b013e31803cb905. [DOI] [PubMed] [Google Scholar]
- Katz NP, Adams EP, Chilcoat H, et al. Challenges in the Development of Prescription Opioid Abuse-deterrent Formulations. Clin J Pain. 2007;23:648–660. doi: 10.1097/AJP.0b013e318125c5e8. [DOI] [PubMed] [Google Scholar]
- Liu Z, Lian Z, Zhao C. Drug use and HIV/AIDS in China. Drug and Alcohol Review. 2006;25(2):173–175. doi: 10.1080/09595230500538835. [DOI] [PubMed] [Google Scholar]
- Luo X, Pietrobon R, Hey L. Patterns and trends in opioid use among individuals with back pain in the United States. Spine. 2004;29(8):884–890. doi: 10.1097/00007632-200404150-00012. discussion 891. [DOI] [PubMed] [Google Scholar]
- Martindale: The Complete Drug Reference. Martindale Products-Pharmaceutical Press; 2007. [Accessed Janurary 4, 2008]. http://www.thomsonhc.com/hcs/librarian/ND_PR/Drugs/SBK/2/PFPUI/RA16hcq2etOKut/ND_PG/PRIH/CS/529E29/ND_CPR/SearchByDatabase/ND_T/HCS/ND_P/Drugs/DUPLICATIONSHIELDSYNC/ABB2E2/ND_B/HCS/PFActionId/hcs.common.RetrieveDocumentCommon/DocId/6231-p/ContentSetId/30/SearchTerm/dicodid%20/SearchOption/BeginWith. [Google Scholar]
- Mao J. Opioid-induced abnormal pain sensitivity: implications in clinical opioid therapy. Pain. 2002;100(3):213–217. doi: 10.1016/S0304-3959(02)00422-0. [DOI] [PubMed] [Google Scholar]
- Mao J. Opioid tolerance and neuroplasticity. Novartis Foundation Symposium; 2004. pp. 181–186. discussion 187–193. [PubMed] [Google Scholar]
- Mao J. Opioid-induced abnormal pain sensitivity. Current Pain and Headache Reports. 2006;10(1):67–70. doi: 10.1007/s11916-006-0011-5. [DOI] [PubMed] [Google Scholar]
- Martell BA, O’Connor PG, Kerns RD, Becker WC, Morales KH, Kosten TR, et al. Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Annalls of Internal Medicine. 2007;146(2):116–127. doi: 10.7326/0003-4819-146-2-200701160-00006. [DOI] [PubMed] [Google Scholar]
- Merry AF, Schug SA, Richards EG, Large RG. Opioids in the treatment of chronic pain of nonmalignant origin. New Zealand Medical Journal. 1991;104(925):520–521. [PubMed] [Google Scholar]
- Miller NS, Swiney T, Barkin RL. Effects of opioid prescription medication dependence and detoxification on pain perceptions and self-reports. American Journal of Therapeutics. 2006;13(5):436–444. doi: 10.1097/01.mjt.0000212894.35705.90. [DOI] [PubMed] [Google Scholar]
- Moore TJ, Cohen MR, Furberg CD. Serious adverse drug events reported to the Food and Drug Administration, 1998–2005. Archives of Internal Medicine. 2007;167(16):1752–1759. doi: 10.1001/archinte.167.16.1752. [DOI] [PubMed] [Google Scholar]
- Musto D. The mystery of addiction. Lancet. 1999;354(Suppl):SIV1. doi: 10.1016/s0140-6736(99)90344-6. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. [Accessed on 01/11/2008];NIDA Research Report Series - Prescription Drugs: Abuse and Addiction. 2008a 2008 Available at: http://www.nida.nih.gov/ResearchReports/Prescription/Prescription6a.html. [Google Scholar]
- National Institute on Drug Abuse. [Accessed: 01/11/2008];Request for Applications. 2008b Available at: http://www.nida.nih.gov/Funding/rfa06.html.
- National Institute on Drug Abuse. [Accessed: 01/11/2008];Program Announcements. 2008c Available at: http://grants.nih.gov/grants/guide/pa-files/PA-04-110.html.
- National Institute on Drug Abuse. [Accessed on 01/31/2008];Clinical Trials Network - Research. 2008d Available at: http://www.nida.nih.gov/CTN/Research.html.
- National Institute on Drug Abuse. [Accessed on 01/31/2008];Small Business Innovation Research (SBIR) and Technology Transfer (STTR) Programs. 2008e Available at: http://www.nida.nih.gov/Funding/SBIR_STTR.html.
- National Institute on Drug Abuse. [Accessed on 01/11/2008];NIDA Special Report - Pain, Opioids, and Addiction: An Urgent Problem for Doctors and Patients - March 5–6. 2008f Available at: 2007 http://www.drugabuse.gov/whatsnew/meetings/default.html. [PubMed]
- Paulozzi LJ, Budnitz DS, Yongil Xi. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiology and Drug Safety. 15(9):618–627. doi: 10.1002/pds.1276. [DOI] [PubMed] [Google Scholar]
- Perkonigg A, Pfister H, Hofler M, Frohlich C, Zimmermann P, Lieb R, et al. Substance use and substance use disorders in a community sample of adolescents and young adults: incidence, age effects and patterns of use. European Addiction Research. 2006;12(4):187–196. doi: 10.1159/000094421. [DOI] [PubMed] [Google Scholar]
- Portenoy RK. Appropriate use of opioids for persistent non-cancer pain. Lancet. 2004;364(9436):739–740. doi: 10.1016/S0140-6736(04)16951-1. [DOI] [PubMed] [Google Scholar]
- Portenoy RK, Foley KM. Chronic use of opioid analgesics in non-malignant pain: report of 38 cases. Pain. 1986;25(2):171–186. doi: 10.1016/0304-3959(86)90091-6. [DOI] [PubMed] [Google Scholar]
- Reid MC, Engles-Horton LL, Weber MB, Kerns RD, Rogers EL, O’Connor PG. Use of opioid medications for chronic noncancer pain syndromes in primary care. Journal of General Internal Medicine. 2002;17(3):173–179. doi: 10.1046/j.1525-1497.2002.10435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosomoff HL, Fishbain DA, Cutler RB, Steele-Rosomoff R. II. Do chronic pain patients’ perceptions about their preinjury jobs differ as a function of worker compensation and non-worker compensation status? Clinical Journal of Pain. 1995;11(4):279–286. doi: 10.1097/00002508-199512000-00005. [DOI] [PubMed] [Google Scholar]
- Schofferman J. Long-term use of opioid analgesics for the treatment of chronic pain of nonmalignant origin. Journal of Pain and Symptom Management. 1993;8(5):279–288. doi: 10.1016/0885-3924(93)90156-p. [DOI] [PubMed] [Google Scholar]
- Schug SA, Merry AF, Acland RH. Treatment principles for the use of opioids in pain of nonmalignant origin. Drugs. 1991;42(2):228–239. doi: 10.2165/00003495-199142020-00005. [DOI] [PubMed] [Google Scholar]
- Simoni-Wastila L. The Use of Abusable Prescription Drugs: The Role of Gender. Journal of Women’s Health and Gender-based Medicine. 2000;9(3):289–297. doi: 10.1089/152460900318470. [DOI] [PubMed] [Google Scholar]
- Simoni-Wastila L, Ritter G, Strickler G. Gender and other factors associated with the nonmedical use of abusable prescription drugs. Substance Use and Misuse. 2004;39(1):1–23. doi: 10.1081/ja-120027764. [DOI] [PubMed] [Google Scholar]
- Stewart WF, Ricci JA, Chee E, et al. Lost productive time and cost due to common pain conditions in the U.S. workforce. Journal of the American Medical Association. 2003;290:2443–2454. doi: 10.1001/jama.290.18.2443. [DOI] [PubMed] [Google Scholar]
- Strine TW, Hootman JM, Chapman DP, Okoro CA, Balluz L. Health-related quality of life, health-risk behaviors, and disability among adults with pain related activity disability. American Journal of Public Health. 2005;95(11):2042–2048. doi: 10.2105/AJPH.2005.066225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. NSDUH Series H-32, DHHS Publication No SMA 07-4293. Office of Applied Studies; Rockville, MD: 2007a. Results from the 2006 National Survey on Drug Use and Health: National Findings. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. The NSDUH Report: Patterns and Trends in Nonmedical Prescription Pain Reliever Use: 2002 to 2005. Rockville, MD: 2007b. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. NSDUH Series H-32, DHHS Publication No SMA 07-4293. Office of Applied Studies; Rockville, MD: 2007c. Results from the 2006 National Survey on Drug Use and Health: National Findings. Appendix B and C. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. DAWN Series D-29, DHHS Publication No (SMA) 07-4256. Vol. 2007 Office of Applied Studies; Rockville, MD: 2007d. Drug Abuse Warning Network, 2005: National Estimates of Drug-Related Emergency Department Visits. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. DASIS Series: S-37, DHHS Publication No (SMA) 07-4234. Vol. 2007 Rockville, MD: 2007e. Treatment Episode Data Set (TEDS): 1995–2005. National Admissions to Substance Abuse Treatment Services. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Drug Abuse Warning Network, 2002: The DAWN Report, Oxycodone, Hydrocodone, and Polydrug Use. Vol. 2002 Office of Applied Studies; 2004a. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Mortality Data from DAWN, 2002 DAWN Series D-25, DHHS Publication No (SMA) 04-3875. Vol. 2004 Rockville, MD: 2004b. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Emergency Department Visits Involving Nonmedical Use of Selected Pharmaceuticals 2004. Office of Applied Studies; Rockville, MD: 2006. [Google Scholar]
- United States Food and Drug Administration, Center for Drug Evaluation and Research. [Accessed December 18, 2008]; Date created: August 7 2002; Updated: March 22, 2007. Web: http://www.fda.gov/cder/aers/default.htm.
- Vivian J, Saleheen H, Singer M, Navarro J, Mirhej G. Under the counter: the diffusion of narcotic analgesics to the inner city street. Journal of Ethnic Substance Abuse. 2005;4(2):97–114. doi: 10.1300/J233v04n02_05. [DOI] [PubMed] [Google Scholar]
- Von Korff M. Editorial: Potent opioids for chronic musculoskeletal pain: flying blind? Pain. 2004;109:207–209. doi: 10.1016/j.pain.2004.02.019. [DOI] [PubMed] [Google Scholar]
- Webster LRWR. Predicting aberrant behaviors in opoioid-treated patients: preliminary validation of the opioid risk tool. Pain Medicine. 2005;6(6):432–442. doi: 10.1111/j.1526-4637.2005.00072.x. [DOI] [PubMed] [Google Scholar]
- Wijnhoven A, de Vet H, Picavet S. Prevalence of Musculoskeletal Disorders is Systematically Higher in Women Than in Men. Clinical Journal of Pain. 2006;22:717–724. doi: 10.1097/01.ajp.0000210912.95664.53. [DOI] [PubMed] [Google Scholar]
- Winkler J, Mueller U, Nenoff P, Seyfarth HJ, Vogtmann M, Borte G, Ponisch W, et al. Treatment of Invasive Pulmonary Aspergillosis in Neutropenic Patients by Additional Bronchoscopic Amphotericin B Instillation. Respiration. 2007;74(6):663–673. doi: 10.1159/000105385. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Achieving Balance in National Opioids Control Policy Guidelines for Assessment. World Health Organization; Geneva: 2000. [Google Scholar]
- World Health Organization. Cancer Pain Relief. World Health Organization; Geneva: 1986. [Google Scholar]
- Wysowski DK. Surveillance of prescription drug-related mortality using death certificate data. Drug Safety. 2007;30(6):533–540. doi: 10.2165/00002018-200730060-00007. [DOI] [PubMed] [Google Scholar]
- Zacny J, Bigelow G, Compton P, Foley K, Iguchi M, Sannerud C. College on Problems of Drug Dependence taskforce on prescription opioid non-medical use and abuse: position statement. Drug and Alcohol Dependence. 2003;69(3):215–232. doi: 10.1016/s0376-8716(03)00003-6. [DOI] [PubMed] [Google Scholar]
- Zenz M, Strumpf M, Tryba M. Long-term oral opioid therapy in patients with chronic nonmalignant pain. Journal of Pain and Symptom Management. 1992;7(2):69–77. doi: 10.1016/0885-3924(92)90116-y. [DOI] [PubMed] [Google Scholar]
- Zenz M, Willweber-Strumpf A. Opiophobia and cancer pain in Europe. Lancet. 1993;341:1075–1076. doi: 10.1016/0140-6736(93)92425-s. [DOI] [PubMed] [Google Scholar]
- Zhu K, Devine A, Dick I, Prince RL. Association of Back Pain Frequency With Mortality, Coronary Heart Events, Mobility, and Quality of Life in Elderly Women. Spine. 2007;32(18):2012–2018. doi: 10.1097/BRS.0b013e318133fb82. [DOI] [PubMed] [Google Scholar]