Abstract
Objectives
This longitudinal study examined the associations between older adults’ goal adjustment capacities (i.e., goal disengagement and goal reengagement capacities), functional disability, and depressive symptoms. It was expected that goal disengagement capacities would prevent an adverse effect of heightened functional disability on increases in depressive symptoms.
Methods
Multivariate regression analyses were conducted, using four waves of data from a 6-yr longitudinal study of 135 community-dwelling older adults (> 60 years old).
Results
Depressive symptoms and functionality disability increased over time. Moreover, poor goal disengagement capacities and high levels of functional disability forecasted six-year increases in depressive symptoms. Finally, goal disengagement buffered the association of functional disability with increases in depressive symptoms. No associations were found for goal reengagement capacities.
Conclusion
The findings suggest an adaptive role for goal disengagement capacities in older adulthood. When confronted with increases in functional disability, the capacity to withdraw effort and commitment from unattainable goals can help protect older adults from experiencing long-term increases in depressive symptoms.
Keywords: goal adjustment, functional disability, depressive symptoms, successful aging
It has been well-established that the experience of functional disability can contribute to depressive symptomatology in older adults (Bruce, 2001; Williamson & Schulz, 1995). This effect is partly due to the adverse consequences that functional disability can have on individuals’ activity or goal constraints, which can lead to failure experiences and loss of control (Lenze et al., 2001). Theory and research also suggest that individuals may be able cope with functional disability. In particular, there are cross-sectional data to suggest that depressive symptoms can be ameliorated if older adults can disengage from goals that have become unattainable in such circumstances (Boerner, 2004; Brandtstädter, Wentura, & Greve, 1993; Schmitz, Saile, & Nilges, 1996). However, longitudinal studies that test this hypothesis explicitly have yet to be performed. To address this gap in the literature, we analyzed four waves of data from a six-year longitudinal study of older adults. We expected that heightened functional disability would forecast increases in depressive symptoms, but only among older adults who had difficulty disengaging from unattainable goals. We did not expect this connection to become established in participants who were capable of disengaging from unattainable goals, because goal disengagement could protect them from repeated failure experiences that typically give rise to depressive symptomatology in old age.
Goal Adjustment and Depressive Symptoms in the Context of Functional Disability
Functional disability is a common and severe challenge in old age (Hébert, Brayne, & Spiegelhalter, 1997; Manton, Gu, & Lamb, 2006). These disabilities relate to problems with carrying out activities of daily living (e.g., bathing, dressing, preparing meals, or shopping) and are often perceived as uncontrollable and irreversible consequences of aging (Beckett et al., 1996). Further, functional disability has been associated with older adults’ depressive symptoms and its consequences for biological dysregulation, chronic disease, and mortality (e.g., Lenze et al., 2001; Williamson & Schulz, 1995; Zeiss, Lewinsohn, Rohde, & Seeley, 1996). Theoretical models suggest that such effects may be mediated by failure experiences, loss of control, and restrictions of (social) activities and interpersonal goals (Lenze et al., 2001). This implies that functional disability can make it difficult for an older person to pursue valued goals (e.g., visiting a relative, continuing leisure activities, or living independently at home), which in turn might increase subsequent levels of depressive symptoms (cf. Higgins, 1987).
The capacity to adjust to unattainable goals may play an important role in helping individuals avoid such adverse emotional consequences of functional disability. This notion is consistent with different theories of self-regulation that point to the emotional benefits of goal adjustment processes among individuals who can no longer attain important goals (Brandtstädter & Renner, 1990; Carver & Scheier, 1998; Heckhausen, Wrosch, & Schulz, 2010; Wrosch, 2011). Further, goal adjustment capacities have been addressed in personality theory and conceptualized as relatively stable differences in individuals’ general tendencies to disengage from unattainable goals across circumstances (i.e., goal disengagement) and to engage in other and attainable goals (i.e., goal reengagement). Goal disengagement capacities reflect a person’s tendencies to reduce effort and commitment from unattainable goals, while goal reengagement capacities involve the tendency to identify, commit to, and pursue other new goals when unattainable goals are encountered (Wrosch, Amir, & Miller, 2011; Wrosch & Miller, 2009; Wrosch, Miller, Scheier, & Brun de Pontet, 2007a; Wrosch, Scheier, Miller, Schulz, & Carver, 2003).
Cross-sectional and longitudinal research has shown that general goal disengagement capacities can forecast less negative affect, fewer depressive symptoms, lower cortisol output, less systemic inflammation, and better physical health (Miller & Wrosch, 2007; Wrosch et al., 2003, 2007a, 2011). These beneficial effects are likely to occur because goal disengagement can reduce negative mood and the associated health problems by protecting individuals from the experience of repeated failure. Goal reengagement capacities are thought to provide new meaningful goals and have been associated with purpose in life and positive affect. Research suggests that goal reengagement capacities are seldom directly related to negative mood states and physical health problems (O’Connor & Forgan, 2007; Wrosch et al., 2003, 2007a). However, there are two exceptions to this trend. First, research has also shown that goal reengagement may relate to lower distress, and that this effect is likely to take place if goal reengagement ameliorates thoughts about the inability to continue pursuing a valued goal (Wrosch et al., 2003). Second, research suggests that in some cases goal reengagement may relate to greater distress, particularly if it triggers maladaptive coping strategies (e.g., venting or self-distraction) that interfere with people’s ability to manage key life stressors (e.g., caregiving for a sick family member, Wrosch et al., 2011).
No longitudinal research to date has examined how goal disengagement and goal reengagement capacities play out in the context of older adults confronted with functional disabilities. However, the literature reviewed above suggests that those older adults who confront functional disability and are generally able to disengage from unattainable goals may avoid the experience of repeated failure (e.g., problems with maintaining independent living), which could prevent a spillover effect of functional disability on depressive symptomatology. By contrast, older adults who cannot disengage from unattainable goals are likely to experience accumulated failure in such circumstances and the resultant increase in depressive symptoms.
With respect to goal reengagement, however, the reported findings indicate that these capacities may be less likely to ameliorate depressive symptoms among older adults who confront functional disability. First, goal reengagement is mainly targeted at improving positive aspects of subjective well-being and has not been shown in previous research to reduce levels of depressive symptoms over time (Wrosch et al., 2007a, Wrosch & Miller, 2009). Second, goal reengagement has not only beneficial effects, but can also be associated with maladaptive coping and stress-specific burden (Wrosch et al., 2011). This may happen if individuals become stretched too thin, and implies that only some new goals may improve emotional well-being in the context of functional disability (e. g., focusing on positive relationships or recruiting help to maintain levels of functioning), while other new goals (e.g., new travel plans or restructuring the garden) could deplete a person’s resources, thereby increasing the person’s burden and associated depressive symptoms. These patterns illustrate how goal reengagement capacities can have both positive and negative consequences for individuals’ emotional well-being (Wrosch et al., 2011). As a result of these dual consequences, we did not expect to find a general buffering effect of goal reengagement capacities on distress.
Empirical evidence lends preliminary support to these propositions by demonstrating that replacing activities that were lost due to illness was associated with higher positive affect, but unrelated to negative mood (Duke, Leventhal, Brownlee, & Leventhal, 2002). In addition, cross-sectional research has shown that older adults who encountered age-related challenges, including functional disability, experienced comparatively low levels of depressive symptoms if they were able to flexibly adjust to unattainable goals (Boerner, 2004; Brandtstädter et al., 1993; Schmitz et al., 1996). However, given that emotional experiences can also influence goal disengagement processes (Thompson, Woodward, & Stanton, 2011; Wrosch & Miller, 2009), results from cross-sectional research remain inconclusive. To overcome this limitation, our study was conducted to examine in longitudinal research whether goal disengagement capacities can buffer the adverse effects of functional disability on increases in older adults’ depressive symptoms.
The Present Study
This research examined the associations between older adults’ goal adjustment capacities, functional disability, and depressive symptoms. We hypothesized that functional disability would predict increases in depressive symptomatology, but only among older adults who had difficulty disengaging from unattainable goals. By contrast, we expected high goal disengagement capacities to ameliorate the adverse effect of functional disability on depressive symptoms. We did not expect goal reengagement capacities to influence depressive symptomatology. To test these hypotheses, we analyzed four waves of data from a 6-yr longitudinal study of older adults. We first explored whether functional disability and depressive symptoms would change over time. Second, our main analysis investigated whether baseline levels of goal adjustment capacities would interact with functional disability in predicting 6-yr changes in depressive symptoms. To this end, we tested interactions between goal adjustment capacities and baseline, 2-yr, 4-yr, and 6-yr levels of functional disability to clarify whether goal adjustment capacities would protect participants’ mood against baseline levels or increases in functional disability.
Method
Participants
This study included a heterogeneous, community-based sample of older adults who participated in the longitudinal Montreal Aging and Health Study Study (MAHS; Wrosch, Schulz, Miller, Lupien, & Dunne, 2007b). Participants were recruited through advertisements in local Montreal newspapers, and were required to be 60 years or older in order to participate. Two-hundred-fifteen participants were recruited in 2004. They were contacted and invited for an initial appointment to the laboratory and instructed to respond to a questionnaire. If participants were unable to come to the laboratory, they were visited in their homes. Participants received $50 for their participation.
The second, third, and fourth waves of the MAHS were collected approximately two years (M = 1.89, SD = .08, range = 1.72 to 2.13 years), four years (M = 3.78, SD = .24, range = 3.28 to 4.77 years), and six years (M = 6.05, SD = .20, range = 5.52 to 6.40 years) after baseline. T2 included 184 participants (85.6%), while T3 included 164 participants (76.3%) and T4 included 137 participants (63.7%). Attrition from T1 to T4 was due to being deceased (n = 23), refusing to participate further (n = 9), being unable to locate participants (n = 19), or having other personal problems that precluded participation (n = 27). Study attrition was not significantly associated with baseline measures of the main study variables, sex, or socioeconomic status. However, participants who dropped out of the study were significantly older at baseline (M = 73.82, SD = 6.78, range = 63 to 94 years) than those who remained in the study, t(129.14) = 2.49, p = .01. A further three participants were excluded from the analyses because of multiple missing data points. Single missing data were replaced with the sample mean (goal reengagement = 1 participant; functional disability = 5 participants). Thus, the final sample consisted of 135 older adults. At baseline, these participants were 71.65 years old (SD = 5.23, range = 64 to 90 years), 53 percent were female, 38 percent had attained an undergraduate degree or higher, and the majority was retired from work (84%).
Materials
The main study variables included measures of participants’ depressive symptomatology, goal adjustment capacities, and levels of functional disabilities (i.e., difficulties with activities of daily living; see Table 1 for zero-order correlations). In addition, sociodemographic variables (age, sex, and socioeconomic status) were assessed.
Table 1.
Zero-Order Correlations Between Depressive Symptoms, Goal Disengagement, Goal Reengagement, and Functional Disability.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| (1) Baseline CES-D | |||||||
| (2) Six-year CES-D | .57** | ||||||
| (3) Baseline goal disengagement | −.11 | −.36** | |||||
| (4) Baseline goal reengagement | −.29** | −.29** | .13 | ||||
| (5) Baseline functional disability | .16 | .24** | −.06 | −.13 | |||
| (6) Two-year functional disability | .18* | .25** | −.08 | −.10 | .54** | ||
| (7) Four-year functional disability | .30** | .44** | −.18* | −.16 | .54** | .44** | |
| (8) Six-year functional disability | .29** | .34** | −.05 | −.05 | .55** | .53** | .55** |
p ≤ .05.
p ≤ .01.
Depressive symptomatology was measured across waves with the 10-item Center for Epidemiological Studies Depression Scale (CES-D10), which has been validated for use with older adults in previous research (Andresen, Malmgren, Carter, & Patrick, 1994). Participants were asked to rate how frequently they had experienced each of ten depressive symptoms during the past week on 4-point Likert-type scales (0 = less than one day, to 3 = 5–7 days). Sample items included: I felt depressed or I felt that everything I did was an effort. For each wave, a sum score of the ten depressive symptoms was computed (see Table 2). Cronbach’s alpha ranged from .71 to .83 across waves.
Table 2.
Means (Standard Deviations) and Range of Older Adults’ Levels of Functional Disability and Depressive Symptoms Across Six Years of Study.
| Baseline | Two-Year | Four-Year | Six-Year | F | |
|---|---|---|---|---|---|
| Functional disability | |||||
| Mean (SD) | 0.41 (1.09)a | 0.48 (1.05) | 0.69 (1.36)b | 0.70 (1.29)b | 4.11** |
| Range | 0–7 | 0–6 | 0–8 | 0–6 | |
| Depressive symptoms | |||||
| Mean (SD) | 5.93 (4.32)a | 6.05 (5.01)a | 6.77 (5.49) | 7.15 (5.31)b | 4.67** |
| Range | 0–18 | 0–23 | 0–28 | 0–26 | |
Note.
Means with different superscripts differ significantly from each other across time.
p ≤ .05.
p ≤ .01.
Functional disability was also assessed across waves. Participants were asked to report whether or not they had difficulty or were unable to perform each of six instrumental activities of daily living (ADLs) (heavy housework, light housework, shopping, preparing meals, managing money, and using the phone) and six basic ADLs (eating, dressing, showering, using the toilet, walking around at home, and getting in and out of a bed or chair). A count variable comprising of the total number of difficulties participants experienced with all ADLs was computed for each wave (see Table 2). At baseline, 22% of participants had difficulty with either basic or instrumental ADLs (T2 = 30%; T3 = 32%; T4 = 36%), indicating that our sample was within the normative range for older adults residing at home (National Advisory Council on Aging, 2006).
Goal adjustment capacities were measured at baseline by administering a previously validated 10-item self-report questionnaire (Miller & Wrosch, 2007; Wrosch et al., 2003, 2007a; Wrosch & Miller, 2009). Participants were asked to report how they usually react when they have to stop pursuing an important goal in their life. Four items measured goal disengagement capacities (e.g., It’s easy for me to stop thinking about the goal and let it go), and six items measured goal reengagement capacities (e.g., I start working on other new goals to pursue). Responses were measured on 5-point Likert-type scales, ranging from 1 = strongly disagree, to 5 = strongly agree. Confirmatory principal component factor analyses (using oblimin rotation) showed that the goal disengagement and goal reengagement items loaded on two separate factors (goal reengagement: eigenvalue = 3.75, loadings = .59 to .82; goal disengagement: eigenvalue = 1.93, loadings = .56 to .70). Consequently, mean scores were computed for goal disengagement (M = 3.05, SD = .72, α = .57) and goal reengagement (M = 3.69. SD = .60, α = .85) separately. The goal disengagement and goal reengagement scales were not significantly correlated with each other at baseline (see Table 1).
Sociodemographic characteristics were measured at baseline and used as covariates in the analyses to reduce the likelihood of spurious associations. In particular, we measured age, sex, and socioeconomic status (SES) because these factors have been shown to be associated with depressive symptoms in previous research (e.g., Blazer, Burchett, Service, & George, 1991). SES was measured as participants’: 1) education level (0 = no education, 1 = high school, 2 = collegial or trade school, 3 = bachelor’s degree, 4 = masters or doctorate); 2) annual family income (0 = less than $17,000, 1 = up to $34,000, 2 = up to $51,000, 3 = up to $68,000, 4 = up to $85,000, 5 = more than $85,000); and 3) perceived socioeconomic status (measured using a 10-rung SES ladder on which participants were asked to rate their socioeconomic status relative to others in their society, as described by Adler, Epel, Castellazzo, & Ickovics, 2000). These three indicators of SES were correlated in our study (rs = .40 to .53) and we therefore computed a global measure of SES by averaging the standardized scores of the single indicators.
Results
The results are described in two sections. The first section tests whether participants’ depressive symptomatology and functional disability changed over time. The second section examines the main and interaction effects of goal adjustment capacities and functional disability in predicting changes in depressive symptoms over time.
Mean Level Changes in Functional Disability and Depressive Symptomatology
To examine mean level changes in depressive symptomatology and functional disability across six years of study, we conducted two separate repeated-measures analyses of variance (ANOVAs), incorporating the within-subject factor Time and using the scores of depressive symptoms and functional disability across waves as dependent variables, respectively. The results of the analyses were controlled for participants’ age, sex, and socioeconomic status. As reported in Table 2, the analyses demonstrated significant linear effects of Time for both depressive symptoms and functional disability, Fs(3, 393) > 4.10, ps < .01, indicating that functional disability and depressive symptoms increased over time. Post-hoc t-tests confirmed that participants’ functional disability, t(134) = 2.93, p < .01, and depressive symptoms, t(134) = 3.10, p < .01, increased significantly from baseline to 6-yr follow-up. In addition, depressive symptoms increased from 2-yr to 6-yr follow-up, t(134) = 2.97, p < .01, and functional disability increased from baseline to 4-yr follow-up, t(134) = 2.74, p < .01.
Predictors of Changes in Depressive Symptomatology
To test the hypothesis that goal disengagement capacities and functional disability would predict changes in depressive symptoms, we performed a hierarchical regression analysis, using 6-yr levels of depressive symptoms as the outcome variable. In order to operationalize change in depressive symptomatology, the first step controlled the analysis for baseline levels of depressive symptoms. In the second step of the analysis, we included the main effects of participants’ baseline levels of goal disengagement capacities, goal reengagement capacities, and baseline, 2-yr, 4-yr, and 6-yr levels of functional disability. In the final step of the analysis, we tested the interactions between goal disengagement and functional disability (separately for baseline, 2-yr, 4-yr, and 6-yr levels), and between goal reengagement and functional disability (separately for baseline, 2-yr, 4-yr, and 6-yr levels) for significance. The analysis was statistically controlled for age, sex, and socioeconomic status, and predictor variables were centered prior to the analysis.
The results of the main effects and interaction effects are presented in Table 3. Baseline levels of depressive symptoms were significantly and positively associated with 6-yr levels of depressive symptoms, F(1, 133) = 62.62, p < .01. None of the sociodemographic characteristics were significantly associated with 6-yr changes in depressive symptoms, Fs(1, 130) < 1.45, ps > .23. In support of our hypothesis, baseline levels of goal disengagement capacities (but not goal reengagement capacities) were significantly associated with 6-yr changes in depressive symptoms, F(1, 124) = 14.81, p < .01. Participants with poor goal disengagement capacities experienced larger increases in depressive symptoms over time than those who were able to disengage from unattainable goals. In addition, 4-yr levels of functional disability significantly predicted increases in depressive symptoms, F(1, 124) = 5.09, p = .03. The main effects of baseline, 2-yr, and 6-yr functional disability were not significant in the multivariate approach, Fs(1, 124) < 2.05, ps > .15. Of importance, the final step of the analysis demonstrated significant interaction effects between baseline levels of goal disengagement capacities and 2-yr, 4-yr, and 6-yr levels of functional disability in predicting changes in depressive symptoms, Fs(1, 123) > 4.39, ps < .04. There was no significant interaction effect between goal disengagement capacities and baseline functional disability, and goal reengagement capacities did not interact with any of the functional disability indicators in predicting changes in depressive symptoms, Fs(1, 123) < 2.14, ps > .14.
Table 3.
Hierarchical Regression Analysis Predicting Six-Year Changes in Depressive Symptoms by Baseline Levels of Goal Disengagement and Goal Reengagement Capacities, and Baseline, Two-Year, Four-Year, and Six-Year Levels of Functional Disability.
| Predictors | Six-year levels of depressive symptoms
|
|
|---|---|---|
| R2 | Beta | |
| Baseline levels of depressive symptoms | .32** | .57** |
| Main effects | .15** | |
| Baseline goal disengagement (GD) | .06** | −.26** |
| Baseline goal reengagement (GR) | .01 | −.10 |
| Baseline functional disability | .00 | −.03 |
| Two-year functional disability | .00 | .02 |
| Four-year functional disability | .02* | .20* |
| Six-year functional disability | .00 | .09 |
| Significant interactions | ||
| GD X Two-year functional disability | .02* | −.15* |
| GD X Four-year functional disability | .02* | −.16* |
| GD X Six-year functional disability | .02* | −.15* |
Note. Main effects and interactions were controlled for age, sex, and socioeconomic status.
p ≤ .05;
p ≤ .01.
Simple slope analyses (Aiken & West, 1991) of the three significant interaction effects showed a highly similar pattern of findings. In support of our hypotheses, baseline goal disengagement capacities were stronger predictors of fewer 6-yr increases in depressive symptoms among participants who experienced heightened functional disability at 2-yr, 4-yr, or 6-yr follow-up (βs = −.44 to −.49, ps < 01), as compared to participants who did not experience increased functional disability at the follow-ups (βs = −.10 to −.11, ps > .24). Because of the similarity of these interactions, and because the three interaction effects were partially correlated with each other, we repeated our analysis by using a composite score of functional disability levels across 2-yr, 4-yr, and 6-yr follow-up, which represented the averaged levels of functional disability experienced after baseline. The analysis confirmed that this functional disability composite score was also significantly associated with 6-yr changes in depressive symptoms, F(1,126) = 8.26, β = .26, R2 = .03, p < .01, and interacted with goal disengagement capacities in predicting 6-yr changes in depressive symptoms, F(1, 125) = 6.69, β = −.17, R2 = .03, p = .01.
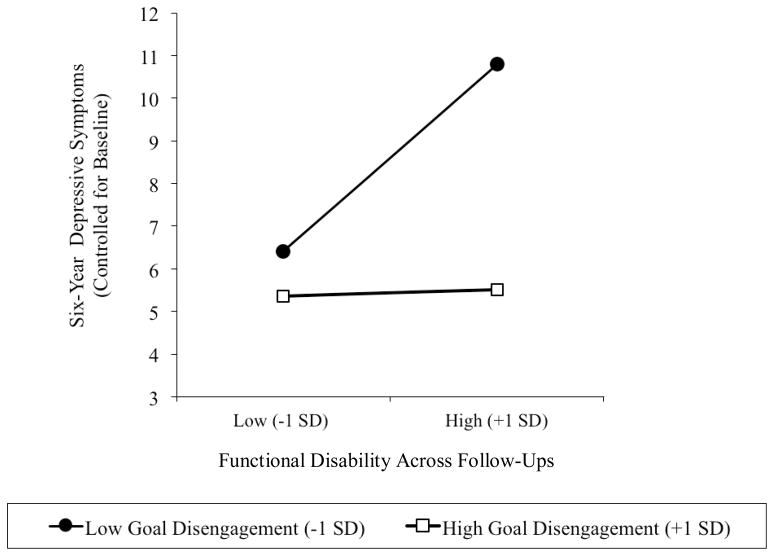
Figure 1 illustrates the latter interaction effect. We plotted the association between averaged functional disability across follow-ups (1 SD above and below the sample mean) and 6-yr changes in depressive symptoms separately for participants who had high (+1 SD) and low (−1 SD) baseline levels of goal disengagement capacities. The obtained pattern of results shows that the largest 6-yr increases in depressive symptoms were found among participants who experienced heightened functional disability across follow-ups and had poor goal disengagement capacities. By contrast, depressive symptoms were fairly stable over time among participants with less functional disability across follow-ups, and among participants who experienced heightened functional disability but were able to disengage from unattainable goals.
Figure 1.
Associations between functional disability (averaged across two-year, four-year, and six-year follow-up) and six-year changes in depressive symptoms, separately for participants who had low (−1 SD) and high (+1 SD) baseline levels of goal disengagement capacities.
Analyses of the simple slopes confirmed this interpretation of the data by documenting that heightened functional disability over follow-ups predicted 6-yr increases in depressive symptoms among participants who had poor goal disengagement capacities, β = .41, p < .01, but not among participants who were able to disengage from unattainable goals, β = .01, p = .92. By contrast, difficulty with goal disengagement was associated with 6-yr increases of depressive symptoms among participants who experienced heightened functional disability across follow-ups, β = −.50, p < .01, but not among their counterparts who experienced less functional disability, β = −.10, p = .30. Note that all analyses controlled for baseline levels of functional disability, which implies that heightened functional disability over follow-ups represented increases in functional disability. Thus, the reported pattern of findings suggests that goal disengagement capacities can protect older adults from experiencing elevated levels of depressive symptomatology when they are confronted with increases in functional disability.
Discussion
The present study examined whether goal disengagement capacities can ameliorate depressive symptomatology if older adults experience functional disability. The reported results strongly support this hypothesis. Over six years, older adults showed parallel increases in functional disability and depressive symptoms. However, an association between these constructs was observed only among older adults who had difficulty disengaging from unattainable goals, and not among their counterparts who were able to abandon unattainable goals. In particular, 6-yr increases in depressive symptoms appeared among participants who had poor goal disengagement capacities and experienced heightened levels of functional disability at 2-yr, 4-yr, or 6-yr follow-up, independent of baseline levels. This pattern of results implies that increases in functional disability contributed to subsequently elevated levels of depressive symptoms if individuals were not able to disengage from unattainable goals.
These findings are consistent with theory and research suggesting that the emergence of functional disability can constrain older adults’ valued activities and goals, which is likely to result in a loss of control and depressive symptoms (Lenze et al., 2001). In addition, the results from this study support research documenting that goal disengagement can reduce the experience of negative mood among individuals who encounter unattainable goals (Brandtstädter & Renner, 1990; Heckhausen et al., 2010; Wrosch et al., 2007a, 2011; Wrosch & Miller, 2009). Thus, when confronted with functional disability, the general ability to withdraw effort and commitment from goals that have become unattainable can help protect older adults from experiencing the adverse consequences on their emotional well-being. However, if older adults continue pursuing such goals, they may experience accumulated failure and subsequent increases in depressive symptoms. We note that although the effect sizes of goal disengagement were not particularly large (6% for the main effect and 3% for the interaction), the obtained results could be clinically meaningful in certain subgroups. Specifically, the average six-year levels of depressive symptoms observed among participants with heightened functional disability and poor goal disengagement capacities reached the recommended cut-off point for mild depression that has been established by previous research (i.e., CES-D10 > 10; Andresen et al., 1994, see also Figure 1).
This study’s findings further showed that goal reengagement capacities were generally associated with lower levels of depressive symptoms (see Table 1). However, goal reengagement capacities did not protect older adults with functional disability against increases in depressive symptomatology. These findings imply that while goal reengagement capacities can be generally associated with low depressive symptoms, they are not conducive to ameliorating the adverse emotional consequences of specific health threats. This may happen because goal reengagement facilitates the pursuit of a variety of alternative goals, and does not necessarily help an individual to cope directly with the negative emotions that derive from specific lost activities. For example, adopting certain new goals could also deplete a person’s resources and lead to failure and negative mood in the context of functional disability (e.g., starting a laborious new garden project or pursuing travel plans), while other new goals could positively influence a person’s quality of life and reduce levels of depressive symptoms (e.g., getting help from other people or improving personal relationships). This implies that there may be a trade-off that comes with the pursuit of new goals (cf. Wrosch et al., 2011), and that individuals who confront stressors and easily engage in new goals could become stretched too thin. These possibilities may explain why general goal reengagement capacities did not predict increases in depressive symptoms and is consistent with previous research that has rarely associated goal reengagement with negative mood (Wrosch et al., 2007a, Wrosch & Miller, 2009).
Overall, the study’s findings have important implications for theory and research in the area of aging and health. First, they substantiate the existing cross-sectional literature, which documents that goal disengagement can be associated with fewer depressive symptoms if older adults confront functional disability (Boerner, 2004; Brandtstädter et al., 1993; Schmitz et al., 1996). However, given that negative mood can also influence how individuals cope with stressors (Thompson et al., 2011; Wrosch & Miller, 2009), previous cross-sectional research cannot provide any conclusions about the direction of effects or the processes at work. Our research overcomes this limitation by demonstrating in longitudinal analyses that goal disengagement capacities ameliorated the impact of heightened functional disability on long-term increases in depressive symptoms.
Second, we think it is important that our study observed reliable increases in levels of depressive symptomatology over six years of study. There is much evidence from the life-span developmental literature indicating that older adults do not experience increases in negative mood (Carstensen, Isaacowitz, & Charles, 1999; Charles, Reynolds, & Gatz, 2001; Kunzmann, Little, & Smith, 2000). However, other longitudinal studies have shown that depressive mood can be elevated in older adulthood (Roberts, Lee, & Roberts, 1991; Rothermund & Brandtstädter, 2003; Wallace & O’Hara, 1992). Our findings support the latter set of studies by demonstrating that depressive symptoms increase in old age, and that this effect is associated with heightened levels of functional disability. In addition, our findings show that high levels of depressive symptoms can be avoided if older adults are able to disengage from unattainable goals. While this pattern of findings supports theory and research documenting that effective self-regulation and emotion regulation can prevent age-related declines in subjective well-being (Brandtstädter & Renner, 1990; Carstensen et al., 1999; Heckhausen et al., 2010), it also suggests that there is a particularly vulnerable group of older adults who experience age-related challenges and are unable to cope effectively with these problems. Given the goal disengagement and functional disability were largely uncorrelated in our study (see Table 1), this group of vulnerable individuals may actually be quite substantial and could consist of up to 50% of older adults suffering from functional disability. These older adults are at a high risk of experiencing depressive symptomatology and should receive more attention in future research.
Third, the identification of goal disengagement as a mechanism that can prevent the adverse effect of functional disability on older adults’ depressive symptoms could have important implications for a variety of health-related outcomes. In particular, depressive symptoms have been shown to dysregulate biological processes in the hormonal and immune systems (e.g., cortisol and systemic inflammation), and to contribute to health declines and mortality (Deuschle et al., 1997; Lenze et al., 2001; Schulz et al., 2000). Given that research has linked goal disengagement capacities to lower cortisol output, less C-reactive protein, and fewer physical health problems (Miller & Wrosch, 2007; Wrosch et al., 2007a), we argue that goal disengagement capacities could also help prevent the consequences of functional disability and depressive symptoms on older adults’ physical health.
Finally, we note that there is only little empirical evidence that can be used to assist older adults in managing functional disability (Gitlin, Hauck, Winter, Dennis, & Schulz, 2006). However, the findings from our study may inform research that is designed to help older adults cope with functional disability. In particular, we suggest that clinical interventions could target the withdrawal of goal commitment during challenging life circumstances, which could subsequently facilitate an improvement of older adults’ quality of life.
Limitations and Future Research
Although the findings of this study support our hypotheses, there are limitations that need to be addressed in future research. First, our analyses were based on self-report measures, and the associations between them could be inflated to some degree by common method variance. In addition, there may be other personality variables, such as neuroticism or optimism, which could be associated with goal disengagement capacities and explain the obtained effects. In this regard, we note that our study included measures of neuroticism and dispositional optimisms, and all reported effects remained significant if these constructs were included as covariates into the analyses. In addition, our longitudinal analyses controlled for previous levels of the outcome variable, which is likely to partial out some of the potential biases of self-reports. Nonetheless, future research should substantiate the study’s findings by examining a wider range of personality variables, and using clinician-derived measures of depressive symptomatology and physician-based measures of functional disabilities.
Second, we measured participants’ general capacities to adjust to unattainable goals and did not assess their specific goals. We focused our analysis on general goal adjustment capacities because functional disability is likely to constrain the pursuit of self-relevant goals across several different life domains. However, as discussed previously, the effects of goal reengagement capacities may depend on the specific type of new goals that they foster, which could either ameliorate or increase emotional distress in stressful life circumstances (cf. Wrosch et al., 2011). Thus, future research should extend our approach by examining both individuals’ general self-regulation capacities and how they adopt and abandon specific goals. Such research may also examine whether goal reengagement capacities can influence the effects of goal disengagement. While subsequent analyses of our data did not confirm a significant interaction between goal disengagement and goal reengagement in predicting changes in depressive symptoms, we would expect that the emotional benefits of goal disengagement could be enhanced if goal reengagement fosters the adoption of adaptive new goals. However, these benefits may be compromised if individuals cannot reengage in new goals, or if goal reengagement leads to the pursuit of new goals that increase an older adults’ burden.
Finally, our analysis did not examine the role of chronic disease in the reported associations, or other factors that can be influenced by depressive mood. In this regard, it would be possible that underlying chronic illness could have made it more difficult for participants to disengage from unattainable goals and produced increases in functional disability and depressive symptoms. Subsequently conducted analyses suggest that this alternative possibility is unlikely to explain the observed pattern of findings, as the reported effects remained significant if we additionally controlled our analyses for prevalent chronic disease at baseline (e.g., heart problems, cancer, or arthritis). In addition, it is possible that levels of depressive symptoms could trigger a cascade of biological processes that subsequently influence risk for morbidity and mortality (Kiecolt-Glaser & Glaser, 2002; Schulz et al., 2000). We therefore suggest that future research should conduct long-term follow-ups to examine how older adults can regulate age-related challenges and protect their psychological and physical health.
Acknowledgments
The Montreal Aging and Health Study is supported by grants and awards from the Canadian Institutes of Health Research to Carsten Wrosch. Completion of this manuscript was further facilitated by a doctoral fellowship awarded to Erin Dunne, and a grant to Carsten Wrosch, from Social Sciences and Humanities Research Council of Canada, and by grants to Gregory Miller from the Canadian Institutes of Health Research (89736), the National Institute of Child Health and Human Development (058502), and the Heart and Stroke Foundation of Canada.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/hea
Contributor Information
Erin Dunne, Concordia University.
Carsten Wrosch, Concordia University.
Gregory E. Miller, University of British Columbia
References
- Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy, White women. Health Psychology. 2000;19:586–592. doi: 10.1037/0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park: Sage Publications; 1991. [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) American Journal of Preventative Medicine. 1994;10:77–84. [PubMed] [Google Scholar]
- Beckett LA, Brock DB, Lemke JH, Mendes de Leon CF, Guralnick JM, Fillenbaum GG, …Evans DA. Analysis of change in self-reported physical function among older persons in four population studies. American Journal of Epidemiology. 1996;143:766–78. doi: 10.1093/oxfordjournals.aje.a008814. [DOI] [PubMed] [Google Scholar]
- Blazer D, Burchett B, Service C, George LK. The association of age and depression among the elderly: An epidemiologic exploration. Journal of Gerontology: Medical Sciences. 1991;46:M210–M215. doi: 10.1093/geronj/46.6.m210. [DOI] [PubMed] [Google Scholar]
- Boerner K. Adaptation to disability among middle-aged and older adults: The role of assimilative and accommodative coping. The Journals of Gerontology: Series B: Psychological Sciences. 2004;59:35–42. doi: 10.1093/geronb/59.1.P35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandtstädter J, Renner G. Tenacious goal pursuit and flexible goal adjustment: Explication and age-related analysis of assimilative and accommodative strategies of coping. Psychology and Aging. 1990;5:58–67. doi: 10.1037/0882-7974.5.1.58. [DOI] [PubMed] [Google Scholar]
- Brandtstädter J, Wentura D, Greve W. Adaptive resources of the aging self: Outlines of an emergent perspective. International Journal of Behavioral Development. 1993;16:323–349. [Google Scholar]
- Bruce ML. Depression and disability in late life: Directions for future research. American Journal of Geriatric Psychiatry. 2001;9:102–112. doi: 10.1176/appi.ajgp.9.2.102. [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Isaacowitz DM, Charles ST. Taking time seriously: A theory of socioemotional selectivity. American Psychologist. 1999;54:165–181. doi: 10.1037/0003-066X.54.3.165. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF. On the self-regulation of behavior. New York: Cambridge University Press; 1998. [Google Scholar]
- Charles ST, Reynolds CA, Gatz M. Age-related differences and change in positive and negative affect over 23 years. Journal of Personality and Social Psychology. 2001;80:136–151. doi: 10.1037//0022-3514.80.1.I36. [DOI] [PubMed] [Google Scholar]
- Deuschle M, Schweiger U, Weber B, Gotthardt U, Körner A, Schmider J, Heuser I. Diurnal activity and pulsatility of the hypothalamus-pituitary-adrenal system in male depressed patients and healthy controls. The Journal of Clinical Endocrinology & Metabolism. 1997;82:234–238. doi: 10.1210/jc.82.1.234. [DOI] [PubMed] [Google Scholar]
- Duke J, Leventhal H, Brownlee S, Leventhal EA. Giving up and replacing activities in response to illness. Journal of Gerontology: Psychological Sciences. 2002;57B:367–376. doi: 10.1093/geronb/57.4.p367. [DOI] [PubMed] [Google Scholar]
- Gitlin LN, Hauck W, Winter L, Dennis MP, Schulz R. Effect of an in-home occupational and physical therapy intervention on reducing mortality in functionally vulnerable older people: Preliminary findings. Journal of the American Geriatrics Society. 2006;54:950–955. doi: 10.1111/j.1532-5415.2006.00733.x. [DOI] [PubMed] [Google Scholar]
- Hébert R, Brayne C, Spiegelhalter D. Incidence of functional decline and improvement in a community-dwelling, very elderly population. American Journal of Epidemiology. 1997;145:935–944. doi: 10.1093/oxfordjournals.aje.a009053. [DOI] [PubMed] [Google Scholar]
- Heckhausen J, Wrosch C, Schulz R. A motivational theory of lifespan development. Psychological Review. 2010;117:32–60. doi: 10.1037/a0017668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ET. Self-discrepancy: A theory relating self and affect. Psychological Review. 1987;94:319–340. doi: 10.1037/0033-295X.94.3.319. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Glaser R. Depression and immune function: Central pathways to morbidity and mortality. Journal of Psychosomatic Research. 2002;53:873–876. doi: 10.1016/S0022-3999(02)00309-4. [DOI] [PubMed] [Google Scholar]
- Kunzmann U, Little TD, Smith J. Is age-related stability of subjective well-being a paradox? Cross-sectional and longitudinal evidence from the Berlin Aging Study. Psychology and Aging. 2000;15:511–526. doi: 10.1037/0882-7974.15.3.511. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Rogers JC, Martire LM, Mulsant BH, Rollman BL, Dew MA, Reynolds CF. The associations of late-life depression and anxiety with physical disability: A review of the literature and prospectus for future research. American Journal of Geriatric Psychiatry. 2001;9:113–135. doi: 10.1176/appi.ajgp.9.2.113. [DOI] [PubMed] [Google Scholar]
- Manton KG, Gu X, Lamb VL. Change in chronic disability from 1982 to 2004/2005 as measured by long-term changes in function and health in the elderly population. Proceedings of the National Academy of Sciences of the United States of America. 2006;103:18734–39. doi: 10.1073/pnas.0608483103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Wrosch C. You’ve gotta know when to fold ‘em: Goal disengagement and systemic inflammation in adolescence. Psychological Science. 2007;18:773–777. doi: 10.1111/j.1467-9280.2007.01977.x. [DOI] [PubMed] [Google Scholar]
- National Advisory Council on Aging (NACA) Seniors in Canada 2006: A report card. Ottawa: NACA; 2006. [Google Scholar]
- O’Connor RC, Forgan G. Suicidal thinking and perfectionism: The role of goal adjustment and behavioral inhibition/activation systems. Journal of Rational-Emotive & Cognitive-Behavior Therapy. 2007;25:321–341. doi: 10.1007/s10942-007-0057-2. [DOI] [Google Scholar]
- Roberts RE, Lee ES, Roberts CR. Changes in prevalence of depressive symptoms in Alameda County: Age, period, and cohort trends. Journal of Aging and Health. 1991;3:66–86. doi: 10.1177/089826439100300104. [DOI] [Google Scholar]
- Rothermund K, Brandtstädter J. Depression in later life: Cross-sequential patterns and possible determinants. Psychology and Aging. 2003;18:80–90. doi: 10.1037/0882-7974.18.1.80. [DOI] [PubMed] [Google Scholar]
- Schmitz U, Saile H, Nilges P. Coping with chronic pain: Flexible goal adjustment as an interactive buffer against pain-related distress. Pain. 1996;67:41–51. doi: 10.1016/0304-3959(96)03108-9. [DOI] [PubMed] [Google Scholar]
- Schulz R, Beach SR, Ives DG, Martire LM, Kop W, Ariyo A. Association between depression and mortality in older adults: The Cardiovascular Health Study. Archives of Internal Medicine. 2000;160:1761–1768. doi: 10.1001/archinte.160.12.1761. [DOI] [PubMed] [Google Scholar]
- Thompson EH, Woodward JT, Stanton AL. Moving forward during major goal blockage: Situational goal adjustment in women facing infertility. Journal of Behavioral Medicine. 2011 doi: 10.1007/s10865-010-9309-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace J, O’Hara MW. Increases in depressive symptomatology in the rural elderly: Results from a cross-sectional and longitudinal study. Journal of Abnormal Psychology. 1992;101:398–404. doi: 10.1037/0021-843X.101.3.398. [DOI] [PubMed] [Google Scholar]
- Williamson GM, Schulz R. Activity restriction mediates the association between pain and depressed affect: A study of younger and older adult cancer patients. Psychology and Aging. 1995;10:369–379. doi: 10.1037/0882-7974.10.3.369. [DOI] [PubMed] [Google Scholar]
- Wrosch C. Self-regulation of unattainable goals and pathways to quality of life. In: Folkman S, editor. Oxford Handbook on Stress, Health, and Coping. Oxford University; 2011. pp. 319–333. [Google Scholar]
- Wrosch C, Amir E, Miller GE. Goal adjustment capacities, coping, and subjective well-being: The sample case of caregiving for a family member with mental illness. Journal of Personality and Social Psychology. 2011 doi: 10.1037/a0022873. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wrosch C, Miller GE. Depressive symptoms can be useful: Self-regulatory and emotional benefits of dysphoric mood in adolescence. Journal of Personality and Social Psychology. 2009;96:1181–1190. doi: 10.1037/a0015172. [DOI] [PubMed] [Google Scholar]
- Wrosch C, Miller GE, Scheier MF, Brun de Pontet S. Giving up on unattainable goals: Benefits for health? Personality and Social Psychology Bulletin. 2007a;33:251–265. doi: 10.1177/0146167206294905. [DOI] [PubMed] [Google Scholar]
- Wrosch C, Scheier MF, Miller GE, Schulz R, Carver CS. Adaptive self-regulation of unattainable goals: Goal disengagement, goal reengagement, and subjective well-being. Personality and Social Psychology Bulletin. 2003;29:1494–1508. doi: 10.1177/0146167203256921. [DOI] [PubMed] [Google Scholar]
- Wrosch C, Schulz R, Miller GE, Lupien S, Dunne E. Physical health problems, depressive mood, and cortisol secretion in old age: Buffer effects of health engagement control strategies. Health Psychology. 2007b;26:341–349. doi: 10.1037/0278-6133.26.3.341. [DOI] [PubMed] [Google Scholar]
- Zeiss AM, Lewinsohn PM, Rohde P, Seeley JR. The relationship of physical disease and functional impairment to depression in the elderly. Psychology and Aging. 1996;11:572–581. doi: 10.1037/0882-7974.11.4.572. [DOI] [PubMed] [Google Scholar]