Abstract
Basidiobolus ranarum is a widespread saprophyte fungus with pathogenic potential. It affects mainly the subcutaneous tissues of the trunk and limbs. Relatively recently, occasional reports of gastrointestinal basidiobolomycosis appeared in the literature. Due to the rarity of the condition and the nonspecific presenting features, the correct diagnosis is usually hard to reach. In this paper, we describe the clinical course of an otherwise healthy female, who presented with a colonic mass. She received subtotal colectomy followed by oral itraconazole, with successful outcome.
1. Introduction: Mucorales
The class Zygomycetes includes two fungal orders: Mucorales and Entomophthorales, with extremely different pathogenic potentials. Mucorales affect only the immunocompromised patient causing mortality in excess of 60% in those affected while entomophthorales, which include Basidiobolus and Conidiobolus genera, affect the immune competent individual, causing principally chronic infection of the subcutaneous tissue [1].
The fungus Basidiobolus ranarum is present in soil, decaying vegetable matter, and the intestines of amphibians, reptiles, fish, and insectivorous bats. The infection is presumably acquired through insect bites or exposure to the fungus following minor trauma to the skin [2].
2. Case Report
A 25-year-old female presented with colicky epigastric pain and nausea for three months, associated in the last month with weight loss and rectal bleeding.
On examination, she looked relatively well; her blood pressure was 104/60 mmHg, pulse 68/minute, respiration rate 20/minute, and temperature 37°C. Abdominal examination revealed a 5 × 8 cm firm, ill-defined mass in the left side of the epigastrium.
Her laboratory works showed leucocytosis (12.8 × 109/μL, reference range 4–11 × 109) and apart from low albumin (21 gm/dL, reference range 34–48), her liver functions, renal values, and electrolytes were normal.
Ultrasound/computerized axial tomography scan showed a large mass in the left half of the transverse colon with mural thickening and irregular narrowing of the lumen. Multiple enlarged mesenteric lymph nodes were also seen. Barium enema showed a long irregular stricture of the distal transverse colon (Figure 1).
Figure 1.
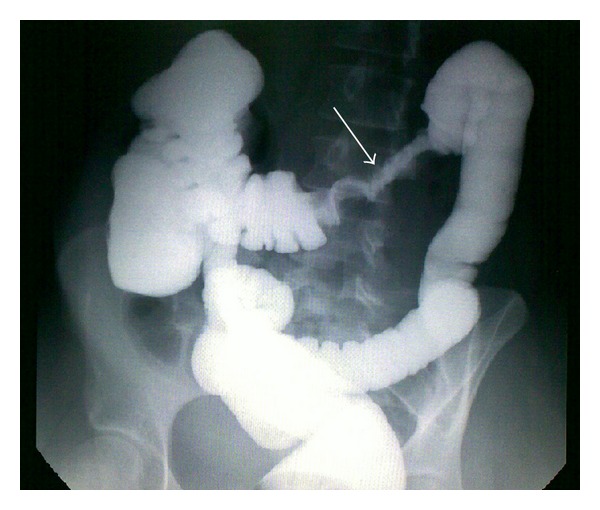
Barium enema showing apple core appearance and shouldering (white arrow), suggestive of colon cancer.
Colonoscopy revealed an incomplete stricture of the middle and distal transverse colon with mucosal ulceration. Biopsies were taken and histopathology showed chronic active colitis with extensive ulcerations.
As the clinical picture was so much suggestive of colon cancer, the patient was subjected to laparotomy where a firm mass was found in the left half of the transverse colon, to which a jejunal loop was adherent. Multiple enlarged lymph nodes were also found in the root of the mesentery. Subtotal colectomy with excision of the adherent 45 cm jejunal loop was performed and bowel continuity restored with ileosigmoid colostomy (Figure 2).
Figure 2.
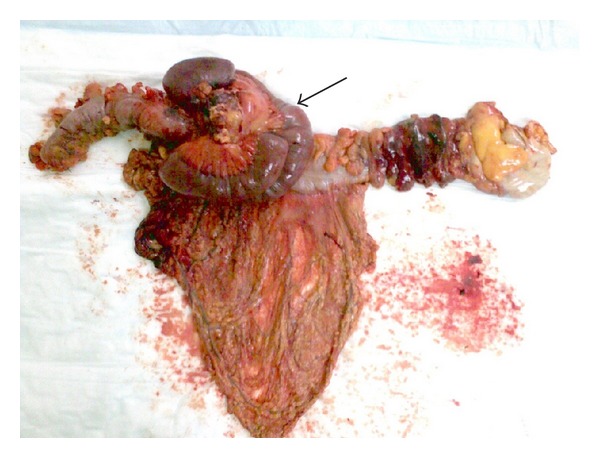
Resected colon with adherent small bowel loop (black arrow).
Histopathology of the resected specimen showed granulomatous reaction with areas of necrosis and acute suppurative inflammation. Broad, thin-walled, occasionally septated hyphae, surrounded by dense eosinophilic reaction (Splendore-Hoeppli phenomenon) were seen, which suggested the diagnosis of basidiobolomycosis (Figure 3). Oral itraconazole, in a daily dose of 200 mg, was started. In her follow-up outpatient visits, the patient remained well, her investigations, including liver and renal function tests, were normal, and she is still under itraconazole treatment.
Figure 3.
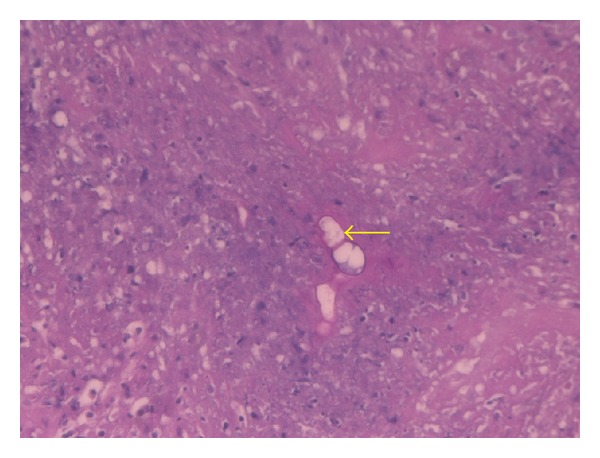
Periodic acid-Schiff stain showing fungal forms (yellow arrow) surrounded by Splendor-Hoeppli phenomenon in a background of acute suppurative inflammation and necrosis. (PASX40).
3. Discussion
Basidiobolomycosis is a rare infection caused by the fungus Basidiobolus ranarum, of the order Entomophthorales, of the class Zygomycetes [3]. Our MEDLINE search yielded 27 published cases with the largest series involving only seven cases from Arizona, USA [4].
The infection, encountered chiefly in East and West Africa, Indonesia, and India, usually affects the trunk and limbs, producing chronic subcutaneous infection [1]. Other rare sites include the gastrointestinal tract [1, 3, 4], which proved fatal in exceptional occasions [5] and the nasal sinuses [6].
How the fungus reaches the gastrointestinal tract is not clear, but ingestion of soil or animal faeces or food contaminated by either, seems to be the possible route [4].
The disease, which has been described relatively recently, has radiological features suggestive of inflammatory bowel disease or malignancy. However, contrary to these pathological entities, leucocytosis and eosinophilia are usually present [4]. In the case presented here, our patient had leukocytosis with no eosinophilia, and as previously reported [4], leukocytosis resolved after surgical resection.
Preoperatively, we diagnosed the case as a stenotic malignant lesion, or, though appeared less likely, inflammatory bowel disease, which is a common pitfall in such condition [4, 7].
The difficulty in diagnosing the condition is multifactorial. Firstly, the clinical presentation is non specific. Secondly, there is no identifiable risk factors [4]. Thirdly, as the causative agent lies deep beneath the mucosa, colonoscopic biopsies may be nonrepresentative. More often than not, the biopsy reveals non specific inflammation or granulomatous reaction. In exceptional cases, fungal hyphae may be detected. However, in suspected cases, tissue culture for fungi may provide the clue for the correct diagnosis [8]. The fourth confounding factor and contrary to expectations, victims of this infection are usually healthy immunocompetent subjects [8], in contrast to the commoner opportunistic fungal infections.
As the condition is rarely, if ever, diagnosed preoperatively, the diseased segment is usually excised [8], with impunity, as surgical resection, together with prolonged administration of azoles, are the main pillars of treatment [4].
The correct diagnosis is usually unveiled by the histopathological examination of the resected specimen or, by isolation of Basidiobolus ranarum from the cultured tissues [4]. The typical morphology of the fungus has been previously described. Histologically, there are irregularly branching thin-walled hyphae, occasionally septated and surrounded by a thick eosinophilic cuff (Splendore-Hoeppli phenomenon) [4, 8–11]. Moreover, the involved bowel segment shows marked mural thickening, fibrosis, prominent eosinophilic infiltration, and granulomatous reaction. In the case presented here, these features were present and enabled us to discover the true nature of the pathology. However, the irrefutable diagnosis needs tissue culture [8], which, due to lack of suspicion, was not carried out in our case. In the absence of culture, serodiagnosis is a useful confirmatory adjunct which could also be used to follow the response to treatment [4].
In vitro studies and clinical reports showed the effectiveness of fluconazole, itraconazole, ketoconazole, and miconazole against Basidiobolus species, [2, 12], and prolonged treatment for up to two years is usually needed [4, 8, 13]. Reports about the effectiveness of potassium iodide are conflicting [14, 15]. Follow up of the response to treatment is generally done by serial CT scan to detect regression or otherwise of the “pseudotumours” and by serological tests to detect the disappearance of specific antibodies [4].
In the case presented here, the diagnosis was unsuspected till the histopathologic examination of the resected colonic mass showed resemblance to the published features of basidiobolomycosis. Itraconazole therapy is planned to continue till the radiologic/serologic tests demonstrate complete eradication of the infection.
4. Conclusion
Gastrointestinal basidiobolomycosis is a recently recognized disease, the clinical features of which resemble those of inflammatory or neoplastic bowel disease. Whenever these diagnoses are entertained, basidiobolomycosis might be considered in the differential diagnosis.
Acknowledgments
The authors would like to thank the histopathology technicians Mr. Ghazi Bargi, Mrs. Shehnaz Khan, Mr. Saeed M. Al-Qahtani, and Ms. Leonila De Rosas.
References
- 1.Prabhu RM, Patel R. Mucormycosis and entomophthoramycosis: a review of the clinical manifestations, diagnosis and treatment. Clinical Microbiology and Infection. 2004;10(supplement 1):31–47. doi: 10.1111/j.1470-9465.2004.00843.x. [DOI] [PubMed] [Google Scholar]
- 2.Gugnani HC. A review of zygomycosis due to Basidiobolus ranarum. European Journal of Epidemiology. 1999;15(10):923–929. doi: 10.1023/a:1007656818038. [DOI] [PubMed] [Google Scholar]
- 3.Dixon DM, Fromatling RA. Taxonomy and classification of fungi. In: Murray PR, Baron EJ, Pfaller MA, Tenover RC, Yolken RH, editors. Manual of Clinical Microbiology. 6th edition. Washington, DC, USA: ASM press; 1995. pp. 699–708. [Google Scholar]
- 4.Lyon GM, Smilack JD, Komatsu KK, et al. Gastrointestinal basidiobolomycosis in Arizona: clinical and epidemiological characteristics and review of the literature. Clinical Infectious Diseases. 2001;32(10):1448–1455. doi: 10.1086/320161. [DOI] [PubMed] [Google Scholar]
- 5.Van den Berk GEL, Noorduyn LA, van Ketel RJ, van Leeuwen J, Bemelman WA, Prins JM. A fatal pseudo-tumour: disseminated basidiobolomycosis. BMC Infectious Diseases. 2006;6, article 140 doi: 10.1186/1471-2334-6-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh R, Xess I, Ramavat A, Arora R. Basidiobolomycosis: a rare case report. Indian Journal of Medical Microbiology. 2008;26(3):265–267. [PubMed] [Google Scholar]
- 7.Pasha TM, Leighton JA, Smilack JD, Heppell J, Colby TV, Kaufman L. Basidiobolomycosis: an unusual fungal infection mimicking inflammatory Bowel disease. Gastroenterology. 1997;112(1):250–254. doi: 10.1016/s0016-5085(97)70242-7. [DOI] [PubMed] [Google Scholar]
- 8.Nemenqani D, Yaqoob N, Khoja H, Al Saif O, Amra NK, Amr SS. Gastrointestinal Basidiobolomycosis: an unusual fungal infection mimicking colon cancer. Archives of Pathology and Laboratory Medicine. 2009;133(12):1938–1942. doi: 10.5858/133.12.1938. [DOI] [PubMed] [Google Scholar]
- 9.Khan ZU, Khoursheed M, Makar R, et al. Basidiobolus ranarum as an etiologic agent of gastrointestinal zygomycosis. Journal of Clinical Microbiology. 2001;39(6):2360–2363. doi: 10.1128/JCM.39.6.2360-2363.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hussein MR, Musalam AO, Assiry MH, Eid RA, El Motawa AM, Gamel AM. Histological and ultrastructural features of gastrointestinal basidiobolomycosis. Mycological Research. 2007;111(8):926–930. doi: 10.1016/j.mycres.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 11.Yousef OM, Smilack JD, Kerr DM, Ramsey R, Rosati L, Colby TV. Gastrointestinal basidiobolomycosis: morphologic findings in a cluster of six cases. American Journal of Clinical Pathology. 1999;112(5):610–616. doi: 10.1093/ajcp/112.5.610. [DOI] [PubMed] [Google Scholar]
- 12.Guarro J, Aguilar C, Pujol I. In-vitro antifungal susceptibilities of Basidiobolus and Conidiobolus spp. strains. Journal of Antimicrobial Chemotherapy. 1999;44(4):557–560. doi: 10.1093/jac/44.4.557. [DOI] [PubMed] [Google Scholar]
- 13.Saka B, Kombaté K, Mouhari-Toure A, et al. Probable basidiobolomycosis in a Togolese rural young successfully treated with ketoconazole. Bulletin de la Societe de Pathologie Exotique. 2010;103(5):293–295. doi: 10.1007/s13149-010-0090-8. [DOI] [PubMed] [Google Scholar]
- 14.Sujatha S, Sheeladevi C, Khyriem AB, Parija SC, Thappa DM. Subcutaneous zygomycosis caused by Basidiobolus ranarum—a case report. Indian Journal of Medical Microbiology. 2003;21(3):205–206. [PubMed] [Google Scholar]
- 15.Yangco BG, Okafor JI, TeStrake D. In vitro susceptibilities of human and wild-type isolates of Basidiobolus and Conidiobolus species. Antimicrobial Agents and Chemotherapy. 1984;25(4):413–416. doi: 10.1128/aac.25.4.413. [DOI] [PMC free article] [PubMed] [Google Scholar]


